Abstract
Kawasaki disease (KD) arises due to the disorder of the inflammation response and faulty immune regulation. Interleukin-27 (IL-27) is a novel cytokine with both pro-inflammatory and anti-inflammatory effects. This study investigated the relationship between serum levels of IL-27, Interleukin-17A (IL-17A), Interleukin-10 (IL-10), Interleukin-6 (IL-6), Interleukin-1β (IL-1β), tumor necrosis factor-α (TNF-α) and coronary artery lesions (CALs) in patients with KD. We obtained blood samples from 81 children with KD before intravenous immunoglobulin (IVIG) therapy. Levels of IL-27, IL-17A, IL-10, IL-6, IL-1β and TNF-α were measured in 251 cases, including 4 groups: the normal control group, NC (n = 90), febrile control, FC (n = 80), KD without coronary arteries (n = 41) and KD with coronary arterial lesions (n = 40). White blood cells counts (WBC), red blood cells counts (RBC), hemoglobin, C-reactive protein (CRP), erythrocyte sedimentation rate and procalcitonin (PCT) were tested in all subjects. Levels of IL-27, IL-10, IL-17A, IL-6, IL-1β and TNF-α were significantly elevated, and RBC and hemoglobin significantly decreased in the group of KD group compared with febrile and control groups. IL-27, IL-6, IL-1β and TNF-α serum levels are even higher in KD children with CALs. There was positive relationship between serum levels of IL-27 and WBC, CRP, PCT, IL-10, IL-17A, IL-6 and TNF-α in children with KD. The up-regulation of IL-27 may be closely linked to up-regulation of systemic pro-inflammatory markers in acute KD. Morover, IL-27 may be involved in the development of CALs in acute KD.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Kawasaki disease (KD) mainly occurs in infants and young children. KD is characterized by the development of acute vasculitis and is the leading cause of acquired heart disease in the pediatric age group in developed countries [1]. Coronary arterial lesions (CALs) are critical complication of KD, leading to myocardial ischemia, infarction and sudden death [2]. The exact series of events in pathogenesis of KD remains unknown; however, there is a growing body of evidence suggests that the development of KD may be an autoimmune-like process [3]. Our laboratory has identified inflammatory cytokines (TNF-a, IL-6 and IL-10) that are thought to play an important role in the development and progression of KD [4]. There is also evidence that disturbed immunological function leading to immunoglobulin-resistant KD may be triggered by an infectious agent in concert with an imbalance of Th17/T cells [5].
Interleukin-27 (IL-27) is a novel member of the IL-6/IL-12 family [6], which exerts pleiotropic suppressive effects on naive and effector T cell populations during infection and inflammation. IL-27 is expressed by antigen-presenting cells (APCs), monocytes, endothelial cells and dendritic cells [7]. Recent evidence has demonstrated that IL-27 has both pro- and anti-inflammatory effects. Additionally, IL-27 regulates angiogenesis, hematopoiesis and osteoclastogenesis [8–10]. The observations that IL-27 has a profound effect on T cell activation and the production of IL-17A, and IL-10, strongly suggest that IL-27 may serve as a novel diagnostic biomarker for predicting bacterial infection in critically ill patients [11, 12]. However, whether IL-27 modulates the inflammation observed in KD patients is still unknown. Thus, we examined serum concentrations of IL-27, IL-17A, IL-10, IL-6, IL-1β and TNF-α in KD patients to ascertain whether these cytokines are involved in the development of KD.
Materials and methods
Subject recruitment
Patient diagnosis was in strict accordance with the criteria proposed by the Japanese Kawasaki Disease Research Committee [13]. Eighty-one patients (48 males and 33 females, 2.26 ± 1.68 years old) with KD were enrolled from the Children’s Hospital of Chongqing Medical University, Chongqing, P.R. China. As controls, 80 children with an acute febrile infectious disease and 90 healthy children were selected.
Echocardiography was obtained within 2 weeks of the onset or before intravenous immunoglobulin administration. Patients with KD were divided into 2 groups according to the presence of CAL: patients with CAL and patients without CALs. CAL was defined by an internal diameter of artery >3.0 mm (<5 years); >4.0 mm (≥5 years), or if the internal diameter of a segment was at least 1.5 times that of an adjacent coronary artery [14].
All blood samples were drawn before IVIG therapy in the KD patient group. Most of blood samples were collected in the first week of illness. Serum was frozen at −80 °C until assays were performed.
Measurement of serum levels of IL-27, IL-17A, IL-10, IL-6, IL-1β, TNF-α
Serum concentrations of IL-27, IL-17A, IL-10, IL-6, IL-1 β and TNF-α were measured using enzyme-linked immunosorbent assay (ELISA) kit (RayBiotech, USA), according to the manufacturer’s instructions. The intra- and inter-assay coefficients of variation for IL-27, IL-10, IL-6, IL-1β and TNF-α were: <10% and <12%. The intra- and inter-assay coefficients of variation for IL-17A were: <7.1 and <9.1%.
Statistical analysis
Statistical analysis was performed using SPSS version 17 software (SPSS Inc., Chicago, IL, USA). We presented the data as mean ± standard deviation (SD) or as median (25th–75th percentile) for all values. One-way analysis of variance (ANOVA) or Kruskal–Wallis ANOVA and Mann–Whitney U tests were used to compare concentrations of cytokines. A Spearman’s test was used to measure associations between sequential parameters. A p value of <0.05 was considered to be statistically significant.
Results
General laboratory findings and levels of IL-27, IL-17A, IL-10, IL-6, IL-1β, TNF-α
The clinical characteristics of children patients with Kawasaki disease, febrile infectious disease (FC) and normal children (NC) are summarized in Table 1. There were no statistically significant differences in age or gender among the three groups. There was a statistically significant decrease in RBC (NC: 4.6 ± 0.4, FC: 4.3 ± 0.4, KD: 4.0 ± 0.4 106/mm3) and HB (NC: 123.3 ± 9.5, FC: 113.3 ± 13.5, KD: 106.3 ± 11.0 g/dL) in the KD group. The levels of WBC (NC: 8.7 ± 1.9, FC: 14.2 ± 6.6, KD: 16.5 ± 7.0 103/uL), platelet (NC: 359.8 ± 144.7, FC: 376.7 ± 147.1, KD: 393.0 ± 164.3 103/uL), CRP (NC: 8.1 ± 0.4, FC: 38.8 ± 30.7, KD: 51.7 ± 36.9 mg/dL), ESR (NC: 4.8 ± 2.4, FC: 65.8 ± 34.3, KD: 76.7 ± 27.2 mm/h) and PCT [NC: 0.2 (0.0–0.2), FC: 1.6 (1.0–2.0), KD: 2.6 (0.1–1.6)] (all p<0.05) were markedly higher in the KD group than that of in NC group but similar to that of in FC group. The serum levels of IL-27 (NC: 335.3 (237.7–520.9), FC: 451.0 (299.6–554.5), KD: 1433.0 (337.7–1318.5) pg/ml), IL-17A (NC: 0.1 (0.0–1.3), FC: 2.1 (0.0–6.1), KD: 30.1 (6.1–52.7) pg/ml), IL-10 (NC: 4.2 (3.2–6.8), FC: 4.2 (3.2–6.8), KD: 13.5 (7.6–26.9) pg/ml), IL-6 (NC: 7.2 ± 2.0, FC: 110.5 ± 21.3, KD: 224.2 ± 32.4 pg/ml), IL-1β (NC: 3.2 ± 0.5, FC: 4.2 ± 1.2, KD: 9.2 ± 1.2 pg/ml) and TNF-α (NC: 17.3 ± 3.8, FC: 19 ± 9.8, KD: 67 ± 9.0 pg/ml) (all p<0.05) were markedly elevated in the KD group compared to the FC and NC groups (Table 1).
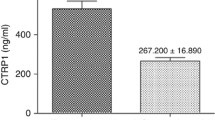
Differences in serum IL-27, IL-17A, IL-10, IL-6, IL-1β, TNF-α between KD with and without CALs
There were no significant differences between group of KD with CALs and group of KD without CALs in age, sex, WBC, platelet, RBC, HB, CRP, ESR, PCT, IL-17A and IL-10. However, the serum level of IL-27, IL-6, IL-1β and TNF-α were markedly higher in the KD patients with CALs than in patients without CALs [2157.25 (419.99–2311.62) vs. 779.5 (296.01–778.08) pg/ml] (p<0.05), (234.1 ± 133.1 vs. 110.5 ± 73.7 pg/ml) (p<0.05), (33.8 ± 18.7 vs. 3.6 ± 0.6 pg/ml) (p<0.05), (56 ± 15.4 vs. 21.6 ± 4.6 pg/ml) (p<0.05) (Table 2).
Correlations between cytokine and patient characteristics
WBC, CRP, PCT, IL-10, IL-17A, IL-6 IL-1β and TNF-α levels were positively correlated with IL-27 in patients with KD (r = 0.185, p = 0.037; r = 0.291, p = 0.000; r = 0.400, p = 0.000; r = 0.454, p = 0.000; r = 0.618, p = 0.000; r = 0.263, p = 0.044; r = −0.130, p = 0.401; r = 0.372, p = 0.013, respectively) (Table 3).
Discussion
L-27 is a heterodimeric cytokine that plays roles in the immune system and inflammation. We were motivated to study the concentrations of IL-27, IL-17A, IL-10, IL-6, IL-1β and TNF-α in children with KD, normal and febrile controls to assess its role in the pathogenesis of KD. Our study demonstrated that (1) levels of IL-27, IL-17A, IL-10, IL-6, IL-1β and TNF-α increased in patients with KD, compared with normal subjects, and (2) serum levels of IL-27 increased in KD patients with CALs, compared with normal subjects and with KD without CALs. Moreover, we found (3) WBC, CRP, PCT, IL-10, IL-17A, IL-6 and TNF-α levels were significantly correlated with IL-27 in patients with KD.
Many studies have reported that immune activation may contribute to its pathogenesis [15] due to the observations that several pro-inflammatory and anti-inflammatory cytokines are elevated during the acute phase of KD. In our previous study we demonstrated that resistin acted as an inflammatory cytokines and levels were significantly higher in patients with KD [16]. There is an ongoing debate on the nature of the T-cell response in development of KD, including the role of regulatory T cells (Tregs) and a subset of T cells known as Th17 cells. Tregs and Th17 cells produce the essential cytokine, and IL-10 and Th17 cells produce the essential cytokine IL-17A. There is a growing body of evidence that the levels of IL-10 and IL-17A increase in patients with KD [17, 18]. This data implicate imbalances in Tregs and Th17 cells in the development of the acute vasculitis syndrome of KD. Recently, some researches have demonstrated that intravenous immunoglobulin (IVIG) suppresses differentiation, amplification, and functions of human Th17 cells and in inhibiting the production of IL-17A from Th17 cells [19–22].
IL-27 plays many roles in the cell, and it was first reported in 2002. It is a heterodimeric cytokine composed of the EBV-transformed gene 3 subunit and p28 subunit. The orphan cytokine receptor WSX-1 was discovered to bind to IL-27 and was required for the effect of IL-27. Subsequent work revealed that the second subunit of the IL-27 receptor complex was gp130 [23]. IL-27 is predominantly synthesized by activated antigen-presenting cells including monocytes, endothelial cells and dendritic cells. IL-27 has been observed to be a player in a variety of inflammatory and infectious illness such as septic peritonitis, collagen-induced arthritis and has recently been evaluated as a novel diagnostic biomarker for bacterial infections [24, 25]. Recently, studies have shown that circulating levels of IL-27 are increased in patients with ischemic heart disease, IL-27 also improved cardiac contraction and coronary perfusion [26]. IL-27 can also enhance antitumor immunity by inhibiting regulatory T cell (Treg) differentiation and angiogenesis. IL-27’s role in invasion in some immunological disease such as asthma and rheumatoid arthritis has been previously described [27, 28].
Recently, IL-27 was shown to promote IL-10 secretion by human CD4+T cells in vitro. IL-27 suppresses the production of IL-17A from CD4+T cells primarily through a STAT1-dependent mechanism, but research has also demonstrated an effect on STAT3-dependent production of IL-17A by CD4+T cells [29, 30]. At the same time, there is a Th17/Treg cell imbalance in the patients with KD [31]. However, there is little data describing the role of IL-27 in acute inflammatory diseases like KD. This gap in our knowledge prompted us to examine the serum concentrations of IL-27 in children with KD and assess its association with IL-10 and IL-17A in the pathogenesis of KD.
In this study, we showed that the serum levels of IL-10 and IL-17A were increased in KD patients, which is in accordance with previous research [31, 32]. IL-10 is a potent cytokine that exerts pleiotropic effects on immunoregulation and inflammation [33]. Another report provided support for the role of IL-27 in the regulation of IL-10 production by CD4+cells. These authors also discovered that IL-27 could induce IL-10 production in Th1, Th2 and Th17 cells by acting on the transcription factors STAT1 and STAT3 [34]. In our study, we found that there was a robust positive correlation between the levels of IL-27 and IL-10. Therefore, we hypothesize that IL-27 may induce the production of IL-10 in the acute phase of KD, but further work is required to validate this hypothesis.
IL-17A is a cytokine produced by CD4+T cells. When IL-17A is produced by Th17 cells the cytokine has pro-inflammatory properties that regulate tissue inflammation by acting on a broad range of cell types to induce the expression of other cytokines (such as IL-6, TNF-a and IL-8), chemokines (such as cxcl1, cxcl10) and metalloproteinases [35, 36]. Overexpression of IL-17 has been linked to autoimmune diseases such as rheumatic arthritis and systemic lupus erythematosis [37]. Thus, we know that IL-17 may also act as a pro-inflammatory cytokine. Our study showed that serum levels of IL-17 A were positively correlated to IL-27 levels. This indicates that IL-27 may be associated with the production of IL-17A during the acute phase of KD. Nevertheless, in another autoimmune disease, progressive multiple sclerosis, plasma IL-27 levels were negatively correlated to the percentage of circulating Th17 cells and the concentration of plasma IL-17A [38]. Therefore, further studies are required to explore and clarify the relationship between IL-27 and Th17.
The increased immune response in KD affects multiple organ systems and is particularly centered in the cardiovascular system. These cardiovascular cells also release a variety of cytokines that promote inflammatory vascular injury. Is the IL-27-dependent activation of IL-10 and IL-17A via STAT1 and STAT3 a mechanism in the development of KD? Further experiments will be required to answer this intriguing question.
Previous studies have reported that CRP and PCT are associated with KD [39]. However, few studies have demonstrated a relationship between CRP, PCT and IL-27. In our study we found a positive relationship between IL-27 serum levels and CRP and PCT. These results suggest that IL-27 may be involved in inflammation during the acute phase of KD.
Finally, in this study we confirmed observations from our previous study that showed that the levels of RBC and hemoglobin were decreased in KD [16]. Another laboratory demonstrated that systemic oxidative stress together with premature aging of RBCs could play a critical role in the cardiovascular complications associated with KD [40, 41]. We are very interested in whether or not decreased levels of RBC and hemoglobin are linked to oxidative stress in KD.
Caroline Galeotti et al have shown that IVIG infusion and aspirin are the standard treatment of acute KD. However, 10–20% of patients show resistance to IVIG therapy and present higher risk of coronary vasculitis. The relative roles of second IVIG infusion, corticosteroids, calcineurin inhibitors, IL-1 antagonists and anti-TNF-α agents remain uncertain [42]. Therefore, alternative therapies are expected to provide more options for the management of resistant patients. Both coronary artery bypass surgery and percutaneous intervention have been used to treat Kawasaki disease patients who develop myocardial ischemia as a consequence of coronary artery aneurysms and stenosis [43].
Galeotti [44] also demonstrated that a number of biomarkers in Kawasaki disease have shown potential for predicting response to IVIG. This may serve to guide our future studies in this area. The potential limitations of our study should be noted. As serum levels of IL-27, IL-10 and IL-17A are regulated by many cytokines, chemokines and cells, therefore, more chemokines should be further examined such as monocyte chemoattractant protein-1 (MCP-1) and vascular endothelial growth factor (VEGF). A limitation of the present study was that the sample size of the present study was relatively small. Larger studies and the long-term management are required to confirm our observations.
In conclusion, this is the first study to show significant elevation of serum IL-27 in the KD patients with CALs. Morover, the levels of IL-10, IL-17A, IL-6 and TNF-α were linked to IL-27 serum levels in the acute phase of KD, providing further evidence about the inflammatory role of IL-27 in KD. These observations indicate that IL-27 may play an indispensable role in the immune and inflammation response in KD. Further studies are needed to elucidate the exact relationship between IL-27 and IL-17A, IL-10 and other inflammatory cytokines and the pathogenesis of KD vasculitis.
References
Kawasaki T. Acute febrile mucocutaneous syndrome with lymphoid involvement with specific desquamation of the fingers and toes in children: clinical observations of 50 cases. Jpn J Allerg. 1967;16:178–222.
Newburger JW, Takahashi M, Gerber MA, et al. Diagnosis, treatment, and long-term management of Kawasaki disease: a statement for health professionals from the Committee on Rheumatic Fever, Endocarditis, and Kawasaki Disease, Council on Cardiovascular Disease in the Young, American Heart Association. Pediatrics. 2004;114:1708–33.
Yeung RS. Kawasaki disease: update on pathogenesis. Curr Opin Rheumatol. 2010;22:551–60.
Settin A, Ismail A, El-Magd MA, et al. Gene polymorphisms of TNF-alpha-308 (G/A), IL-10 (-1082) (G/A), IL-6 (-174) (G/C) and IL-1Ra (VNTR) in Egyptian cases with type 1 diabetes mellitus. Autoimmunity. 2009;42:50–5.
Afzali B, Lombardi G, Lechler RI, et al. The role of T helper 17 (Th17) and regulatory T cells (Treg) in human organ transplantation and autoimmune disease. Clin Exp Immunol. 2007;148:32–46.
Pflanz S, Timans JC, Cheung J, et al. IL-27, a heterodi-meric cytokine composed of EBI3 and p28 protein, induces proliferation of naive CD4+ T cells. Immunity. 2002;16:779–90.
Boulay JL, O’Shea JJ, Paul WE, et al. Molecular phylogeny within type I cytokines and their cognate receptors. Immunity. 2003;19(2):159–63.
Lin TT, Lu J, Qi CY, et al. Elevated serum level of IL-27 and VEGF in patients with ankylosing spondylitis and associate with disease activity. Clin Exp Med. 2015;15(2):227–31.
Seita J, Asakawa M, Ooehara J, et al. Interleukin-27 directly induces differentiation in hematopoietic stem cells. Blood. 2008;111(4):1903–12.
Park JS, Jung YO, Oh HJ, et al. Interleukin-27 suppresses osteoclastogenesis via induction of interferon-γ. Immunology. 2012;137(4):326–35.
Hunter CA, Kastelein R. Interleukin-27: balancing protective and pathological immunity. Immunity. 2012;37:960–9.
Wong Hector R, Cvijanovich Natalie Z, Hall Mark, et al. Interleukin-27 is a novel candidate diagnostic biomarker for bacterial infection in critically ill children. Crit Care. 2012;16:R213.
JCS Joint Working Group. Guidelines for diagnosis and management of cardiovascular sequelae in Kawasaki disease (JCS 2008). Circ J. 2010;74:1989–2020.
Japan Kawasaki Disease Research Committee. Report of subcommittee on standardization of diagnostic criteria and reporting of coronary artery lesions in Kawasaki disease. Tokyo: Ministry of Health and Welfare; 1984.
Rowley AH, Shulman ST. Pathogenesis and management of Kawasaki disease. Expert Rev Anti Infect Ther. 2010;8:197–203.
Liu R, He B, Gao F, et al. Relationship between adipokines and coronary artery aneurysm in children with Kawasaki disease. Transl Res. 2012;160:131–6.
Hirao J, Hibi S, Andoh T, Ichimura T. High levels of circulating interleukin-4 and interleukin-10 in Kawasaki disease. Int Arch Allergy Immunol. 1997;112:152–6.
Guo MM-H, Tseng W-N, Ko C-H, et al. Th17- and Treg-related cytokine and mRNA expression are associated with acute and resolving Kawasaki disease. Allergy. 2015;70:310–8.
Maddur MS, Sharma M, et al. Inhibitory Effect of IVIG on IL-17 production by Th17 Cells is Independent of Anti-IL-17 antibodies in the Immunoglobulin Preparations. J Clin Immunol. 2013;33:S62–6.
Maddura Mohan S, Kaveri Srini V, Bayry Jagadeesh. Comparison of different IVIg preparations on IL-17 production by human Th17 cells. Autoimmun Rev. 2011;10:809–10.
Maddur MS, Hegde P, et al. Inhibition of differentiation, amplification, and function of human TH17 cells by intravenous immunoglobulin. J Allergy Clin Immunol. 2011;127(3):823–30.
Rasouli Manoochehr, Heidarib Behzad, Kalani Mehdi, et al. Downregulation of Th17 cells and the related cytokines with treatment in Kawasaki disease. Immunol Lett. 2014;162:269–75.
Yoshida H, Nakaya M, Miyazaki Y. Interleukin 27: a double-edged sword for offense and defense. J Leukoc Biol. 2009;86:1295–303.
Wirtz S, Tubbe I, Galle PR, et al. Protection from lethal septic peritonitis by neutralizing the biological function of interleukin 27. J Exp Med. 2006;203:1875–81.
Niedbala W, Cai B, Wei X, et al. Interleukin 27 attenuates collagen-induced arthritis. Ann Rheum Dis. 2008;67:1474–9.
Ma Ming-Chieh, Bao-Wei WangTzu-Pei Yeh, et al. Interleukin-27, a novel cytokine induced by ischemia–reperfusion injury in rat hearts, mediatescardioprotective effectsvia the gp130/STAT3 pathway. Basic Res Cardiol. 2015;110:22.
Yoshimoto T, Yoshimoto T, Yasuda K, et al. IL-27 suppresses Th2 cell development and Th2 cytokines production from polarized Th2 cells: a novel therapeutic way for Th2-mediated allergic inflammation. J Immunol. 2007;179(7):4415–23.
Lai X, Wang H, Cao J, et al. Circulating IL-27 is elevated in rheumatoid arthritis patients. Molecules. 2016;21(11):1565.
Stumhofer JS, Laurence A, Wilson EH, et al. Interleukin 27 negatively regulates the development of interleukin 17-producing T helper cells during chronic inflammation of the central nervous system. Nat Immunol. 2006;7:937–45.
Wang H, Meng R, Li Z, et al. IL-27 induces the differentiation of Tr1-like cells from human naive CD4+ T cells via the phosphorylation of STAT1 and STAT3. Immunol Lett. 2011;136:21–8.
Jia S, Li C, Wang G, et al. The T helper type 17/regulatory T cell imbalance in patients with acute Kawasaki diseasec. Clin Exp Immunol. 2010;162:131–7.
Kobayashi N, Mori M, Kobayashi Y, et al. Intravenous gamma-globulin therapy improves hypercytokinemia in the acute phase of Kawasaki disease. Mod Rheumatol. 2004;14:447–52.
Lalani I, Bhol K, Ahmed AR. Interleukin-10: biology, role in inflammation and autoimmunity. Ann Allergy Asthma Immunol. 1997;79:469–83.
CromeSQ WangAY. LevingsMK. Translationalmini-reviewseries on Th17 cells: function and regulation of human T helper 17 cells in health and disease. Clin Exp Immunol. 2010;159:109–19.
Laan M, Cui ZH, Hoshino H, et al. Neutrophil recruitment by human IL- 17 via C-X-C chemokine release in the airways. J Immunol. 1999;162:2347–52.
Afzali B, Mitchell P, Lechler RI, et al. Translational mini-review series on Th17 cells: induction of interleukin-17 production by regulatory T cells. Clin Exp Immunol. 2010;159:120–30.
Volin MV, Shahrara S. Role of TH-17 cells in rheumatic and other autoimmune diseases. Rheumatology (Sunnyvale). 2011. doi:10.4172/2161-1149.1000104.
Tang SC, Fan XH, Pan QM, et al. Decreased expression of IL-27 and its correlation with Th1 and Th17 cells in progressive multiple sclerosis. J Neurol Sci. 2015;348(1–2):174–80.
Yoshikawa H, Nomura Y, Masuda K, et al. Serum procalcitonin value is useful for predicting severity of Kawasaki disease. Pediatr Infect Dis J. 2012;31(5):523–5.
Pietraforte Donatella, Gambardella Lucrezia, Marchesi Alessandra, et al. Red blood cells as bioindicators of cardiovascular risk in Kawasaki disease: a case report. Int J Cardiol. 2015;181:311–3.
Straface E, Gambardella L, Metere A, et al. Oxidative stress and defective platelet apoptosis in naïve patient with Kawasaki disease. Biochem Biophys Res Commun. 2010;392:426–30.
Galeotti C, Kaveri SV, Cimaz R, et al. Predisposing factors, pathogenesis and therapeutic intervention of Kawasaki disease. Drug Discov Today. 2016;21(11):1850–7.
Newburger JW, et al. Kawasaki disease. J Am Coll Cardiol. 2016;67(14):1738–49.
Galeotti C, Kaveri SV, Bayry Jagadeesh. Molecular and immunological biomarkers to predict IVIg response. Trends Mol Med. 2015;21(3):145–7.
Acknowledgements
This work was supported by National Natural Science Foundation of China under Grant: No. 81270412 and National Natural Science Foundation of China under Grant: No. 81500273.
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Conflict of interest
All authors have no actual or potential conflicts of interest with other people or organizations with 3 years of initiating the work presented here.
Ethical approval
The study protocol was approved by the Ethics Committee of Children’s Hospital of Chongqing Medicine University, and written informed consent forms were obtained from the parents of all subjects.
Rights and permissions
About this article
Cite this article
Si, F., Wu, Y., Gao, F. et al. Relationship between IL-27 and coronary arterial lesions in children with Kawasaki disease. Clin Exp Med 17, 451–457 (2017). https://doi.org/10.1007/s10238-017-0451-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10238-017-0451-8