Abstract
Venous thromboembolism (VTE) occurs roughly in one out of five cancer patients and is the second cause of death in this population. When all cancer patients are considered together, a sevenfold increased risk for VTE has been calculated. Over the last 20 years, a number of risk factors have been recognized. These have been used in several risk assessment models aimed at identifying high-risk patients who are therefore candidates for thromboprophylaxis. An easily applicable and reliable risk score is based on the cancer site, hemoglobin levels, pre-chemotherapy platelet and leukocyte counts as well as body mass index. The additional measurement of two biomarkers, namely D-dimer and soluble P-selectin, may improve estimates of the cumulative VTE probability. A variable incidence of VTE has been determined in patients with specific types of malignancy, with the highest odds in those with pancreatic cancer followed by head and neck tumors. In terms of histotype, the risk of VTE is significantly higher in patients with adenocarcinoma than in those with squamous cell carcinoma and in patients with high-grade versus low-grade tumors. Cancer therapy may also be responsible for VTE; specifically, the presence of an indwelling central venous catheter, immunomodulatory drugs such as thalidomide and lenalidomide, monoclonal antibodies, such as bevacizumab, erythropoiesis-stimulating agents and hormonal therapy with tamoxifen place patients at higher risk. The pathogenesis of cancer-related VTE is poorly understood but is likely to be multifactorial. “Virchow’s triad,” comprising stasis consequent to a decreased blood flow rate, an enhanced blood clotting tendency such as accompanies inflammation and growth factor expression, and structural modifications in blood vessel walls, is thought to play a central role in the induction of VTE. The prophylaxis and treatment of VTE are based on well-established drugs such as vitamin K antagonists and unfractionated and low-molecular-weight heparins as well as on an expanding group of new oral anticoagulants, including fondaparinux, rivaroxaban, apixaban and dabigatran. Furthermore, aspirin has been shown to prevent arterial thrombosis and to reduce the rate of major vascular events. Guidelines for the general management of VTE in cancer patients and in those with an indwelling central venous catheter have been recently developed with the aim of selecting the most rational therapeutic approach for each clinical situation. The main features of VTE based on our own observations of 92 cancer patients and 159 patients with non-neoplastic disease are briefly described herein.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Historical clues and definitions
In the medical field, it is somewhat daring to ascribe the first observation of a clinical presentation or the first demonstration of a certain phenomenon to a particular author or research group for the very simple reason that, when one looks a bit more carefully and goes sufficiently far back in a retrieval of the literature, one very often comes across a paper(s) describing the same or a similar condition, or providing the same or similar observations.
This is indeed the case for cancer-related coagulopathy, commonly referred to as Trousseau’s syndrome after the French physician Armand Trousseau, who in 1865 [1] provided a detailed description of an association between cancer and venous thromboembolism (VTE). This primogeniture, however, was challenged when a careful search of the literature dating back to the first half of the nineteenth century revealed that the occurrence of deep-vein thrombosis (DVT) in cancer patients had been reported by Bouillard and Bouillaud [2] in 1823, 42 years earlier than Trousseau. However, since the eponymous term “Trousseau’s syndrome” (TS) is now used worldwide, it has been adopted in the present review.
Trousseau’s syndrome can be defined as an association of cancer with VTE or pulmonary embolism (PE). It is a cancer-related hypercoagulability and should therefore be regarded as a paraneoplastic pro-coagulant phenomenon. TS occurs with a relatively high frequency on every internal medicine ward. Since the risk for VTE varies according to the type of malignancy, and because this complication may lead to death in a sizable proportion of affected cancer patients, it is essential that all efforts be made to prevent the occurrence of TS through the use of adequate thromboprophylactic measures or, failing such efforts, that it be promptly recognized and appropriately treated.
Obviously, the diagnosis of TS implies the correct definition of DVT and PE and their occurrence evaluated as possible, probable or definite according to internationally accepted and well-defined criteria [3]. Variations in the reported disease prevalence may in fact be due, at least in part, to variability in diagnostic criteria. The present study abides by the following criteria: a definite diagnosis of DVT or PE is based on the occurrence of clinical features and a confirmation by angiography (or pulmonary angiogram in case of PE), CT scan, magnetic resonance imaging or histopathologic examination of the thrombus, either subsequent to its surgical removal or obtained during autopsy. DVT is deemed probable when diagnostic tests have not been performed or the results are considered indeterminate in the presence of positive plethysmography and/or Doppler ultrasound examination and/or radionuclide venography and/or radiolabeled fibrinogen leg scan (or a perfusion or ventilation-perfusion lung scan strongly indicative of PE). Finally, the diagnosis of possible DVT or PE implies that confirmatory tests have not been done or their results are considered indeterminate but the clinical signs and symptoms are typical of DVT or PE and/or the diagnosis has been made by a physician and/or the medical record shows that the patient has been given anticoagulation therapy or undergone a therapeutic surgical procedure, including an inferior vena cava filter in the case of PE.
Epidemiology
In the United States, over 200,000 first lifetime cases of VTE are reported each year but the actual number is likely to be remarkably higher as the condition is frequently misdiagnosed or unreported. In Western populations, the annual incidence of VTE ranges from 71 to 117 cases/100,000 persons/year, and it rises exponentially with age, from ≤5 cases/100,000 patients age ≤15 years to almost 500 cases/100,000 patients age ≥80 years [3, 4]. A similar pattern was reported in a Taiwanese nationwide population-based cohort study [5] carried out on 2,774 patients, in whom the occurrence of symptomatic VTE ranged from 4/100,000 in patients age <40 years to 108/100,000 in patients age ≥80 years.
An overwhelming body of evidence, published in the last 20 years and summarized in extensive reviews [6, 7], unequivocally points to a clinical association between VTE and cancer. In fact, the prevalence of VTE was 7 % in a group of 747 patients with solid tumors who were followed for a median of 526 days [6]. A similarly higher incidence of VTE was reported in patients with hematologic malignancies: in a meta-analysis of 29 independent cohorts comprising over 18,000 patients and almost 1,150 events, VTE occurred in 6.4 % of lymphoma patients [8]. As expected, venous thrombosis was more frequently seen than arterial thrombosis and the incidence of both vascular events was significantly higher in patients with non-Hodgkin lymphoma (and especially in those with high-grade disease) than in those with Hodgkin lymphoma.
When patients with all types of malignant tumors are considered together, cancer has been calculated to pose an approximately sevenfold higher risk for VTE, although the magnitude of the risk varies to a remarkable extent among cancer patients, with even a 28-fold higher risk associated with certain neoplastic conditions [7]. Likewise, the features of VTE in cancer patients may range extensively, from simple abnormalities in laboratory coagulation tests in the absence of specific clinical symptoms to massive thromboembolic events associated with disseminated intravascular coagulation.
Levitan et al. [9] studied the association of malignant and non-malignant diseases with an initial episode of DVT/PE, recurrent DVT/PE and mortality in a population of over 1.2 million US Medicare patients age ≥ 65 years who were admitted to the hospital with a diagnosis of malignancy. They found that the percentage of patients with DVT/PE at initial hospitalization was higher among those with malignancy than among those with non-malignant disease (0.6 vs. 0.57 %, p = 0.001). In that study, the probability of readmission within 6 months of initial hospitalization because of a recurrent thromboembolic event was 0.22 for patients with prior DVT/PE and malignancy, compared with 0.065 for patients with prior DVT/PE and no malignancy (p = 0.001). In the same group of patients with DVT/PE and malignant disease, the probability of death within 6 months of initial hospitalization was 0.94, compared with 0.29 among those with DVT/PE and no malignancy (p = 0.001). Thus, based on a very large number of patients whose data could be collected thanks to the availability of the Medicare Provider Analysis and Review Record (MEDPAR) database, it was calculated that patients with concurrent DVT/PE and malignancy have a more than threefold higher risk of recurrent thromboembolic disease and death than patients with DVT/PE without malignancy.
Risk factors
Approximately 25 % of patients with VTE will die within 1 week, and sometimes within 24–48 h, thus frustrating any attempt at effective treatment. Given this frequently dramatic outcome, an assessment of the risk factors for VTE, PE and DVT in large cohort studies, including subjects observed for prolonged periods of time, is essential. However, a reliable assessment of such factors implies that the diagnosis is based on strict clinical criteria and subsequently confirmed by venogram or pulmonary angiogram or, when appropriate, by autopsy examination.
Increased body mass index (BMI) and frank obesity, heavy smoking, the use of oral contraceptives, hormone replacement therapies and general as opposed to regional (spinal or epidural) anesthesia have long been considered significant risk factors for VTE, although uncertain and sometimes conflicting results have been reported, especially when the above-mentioned factors were assessed independently. The risks posed to cancer patients by the long-term use of central venous catheters (CVC) and the more frequent use of polychemotherapy have become increasingly clear [10]. Also, a matter of concern is the thrombogenic pathogenicity of anti-β2-glycoprotein I (β2GPI) antibodies, a feature of the antiphospholipid syndrome (APS). A large, multicentre, retrospective study showed that post-translational modification of β2GPI via thiol-exchange reactions is a highly specific indicator of APS. Thus, in addition to standard laboratory tests for APS, measurement of oxidized β2GPI increases the reliability of VTE risk predictions [11].
A further, recently emphasized consideration is the risk of VTE posed by protracted immobilization, such as during prolonged flights [12]. Almost two billion people travel by commercial aircraft annually, with over 300 million of these travelers on long-haul flights. A direct relation between the incidence of VTE and long-distance flights has been documented; specifically, the risk of DVT under these conditions is between 3 and 12 %. The pathophysiologic changes that increase the risk of in-flight VTE are prolonged sitting in a confining environment, hypoxia (as is typical in an airplane cabin) and dehydration. This added risk is particularly relevant given that cancer patients often undertake long-distance flights in order to be treated in more specialized and/or better equipped centers. In healthy subjects, individual risk factors for air-travel-related VTE are age >40 years, female gender, use of oral contraceptives, varicose veins in the lower limbs, obesity and genetic thrombophilia.
Heit et al. [13] carried out a population-based case–control study on 625 Olmsted County (Minnesota, USA) residents who experienced a first lifetime episode of DVT or PE between January 1976 and December 1990. An equivalent number of age- and sex-matched residents of the same county who had no history of VTE served as the controls. Univariate analysis identified the following risk factors: age, BMI, congestive heart failure, active malignant tumors treated by chemotherapy, previous superficial vein thrombosis and previous varicose vein procedures, chronic renal disease, neurologic disease with limb paresis or plegia, central venous catheterization or trans-venous pacemaker implantation, trauma, any type of surgery but especially orthopedic surgery and neurosurgery, any type of anesthesia, hospital or nursing home stay and recent hospital admission. In addition, among females, post-partum state and gynecologic surgery were also identified as risk factors for VTE.
In a multivariate analysis, the independent factors for VTE were (listed according to decreasing magnitude of risk: (a) patients undergoing recent surgery (22-fold higher risk); (b) patients with a history of recent trauma (12-fold); (c) patients confined to a hospital or nursing home (eightfold); (d) patients with neoplasms (fourfold based on the tumor alone, and greater than sixfold in those receiving chemotherapy); (e) patients with a CVC or a trans-venous pacemaker (fivefold higher risk for a venous thrombosis in the upper extremities); (f) patients with previous superficial vein thrombosis (fourfold) and (g) neurologic disease associated with paresis of the extremities (threefold). Varicose veins and congestive heart failure were either poorly or not significantly linked to a higher risk of VTE. The risk associated with varicose veins was more evident in young patients and decreased with age [13].
The results of this population-based case–control study thus indicate that among the vast array of potential risk factors for VTE the diagnosis of malignancy implies a mean fourfold higher risk, placing it fourth among the six risk factors identified in the multivariate analysis. However, the study provided no information as to whether the VTE event preceded discovery of the tumor or was instead a later complication of its clinical course, nor did it specify the magnitude of the risk according to the different tumor histotypes.
In light of these considerations, it is not surprising that VTE is the second most common cause of death in patients with cancer, and it can also be the presenting complaint in patients with an occult malignancy [14]. One obvious question is how many patients with unprovoked VTE do indeed harbor an occult and often asymptomatic tumor and whether the tumor incidence in these patients is higher than expected. To answer this question, White et al. [15], making use of the California Cancer Registry, examined the data collected from 528,693 adult cancer patients during a 6-year period, with the aim of identifying the occurrence of VTE in the year before the cancer was actually diagnosed. The number of patients with unprovoked VTE was slightly higher than expected, and in the large majority of the unexpected cases of VTE a diagnosis of metastatic-stage cancer was made within 4 months. In addition, a significantly elevated standardized incidence ratio (SIR) of unprovoked VTE was detected only in seven cancer types: acute myelogenous leukemia, non-Hodgkin lymphoma and renal, ovarian, pancreatic, stomach and lung cancer (SIR range, 1.8–4.2).
Based on a conventional estimate, one in five cancer patients will sooner or later develop a VTE. Consequently, every effort should be made to reliably single out high-risk patients, that is, those most likely to benefit from thromboprophylaxis, while sparing those with low or no risk from an unnecessary, relatively expensive and potentially dangerous treatment. To reduce the remarkable heterogeneity of clinical practice among different medical centers and to pursue the appropriateness of thromboprophylaxis, a number of risk score systems have been proposed in the last few years, although not all of them have been properly validated. In addition to risk factors that are common to several systems (such as hypercoagulable disorders, obesity, atrial fibrillation), there are factors which have been proposed according to specific clinical conditions (acute vs. chronic patients, surgical vs. non-surgical patients, and so on). Even so, it seems reasonable to estimate that both overuse and underuse of thromboprophylaxis are still applied to similar proportions (roughly 30 %) of the patients.
With the aim of preventing VTE among hospitalized patients, Kucher et al. [16] have developed a computer-alert program which, through a link to the patient database, was capable of identifying hospitalized patients at risk for DVT in the absence of prophylaxis (Table 1). On the other hand, a number of risk factors, listed in Table 2, have been combined to yield the so-called “Geneva risk score system” that is able to identify acutely ill medical patients with a score ≥3 who should receive thromboprophylaxis [17].
An easily available and reproducible risk assessment model has now been validated in multiple settings as well as in prospective and retrospective observational studies [16, 17]. The model is based on: (a) clinical parameters, such as the cancer site, with gastric and pancreatic cancers implying the highest risk (score 2), followed by lung cancer, lymphoma, and gynecologic, bladder and testicular tumors (score 1); (b) laboratory parameters, including pre-chemotherapy platelet count (≥350,000/mm3), hemoglobin levels (<10 g/dL or the administration of erythropoiesis-stimulating agents, ESAs) and pre-chemotherapy leukocyte count (>11,000/mm3), with a risk score of 1 assigned to each of these laboratory variables; (c) BMI ≥35 kg/m2, which is also assigned a risk score of 1. Overall, a risk score ≥3 defines high-risk patients; a score of 1–2 those at intermediate risk and a score of 0 low-risk patients.
According to the Vienna Cancer and Thrombosis Study [18], if the risk score is implemented with the additional measurement of two well-known biomarkers, namely D-dimer (a fragment of fibrin that is formed as a result of fibrin degradation) and P-selectin (a member of the selectin family of cell adhesion molecules), an even better cumulative probability of VTE in cancer patients can be established. However, the P-selectin assay is expensive and not widely available.
In another study [19], 257 cancer patients with acute VTE who had been hospitalized within the previous 30 days for acute medical illness or surgery were enrolled in the SWiss Venous ThromboEmbolism Registry (SWIVTER). Univariate analysis showed that both outpatient status at the time of VTE diagnosis and ongoing or recent chemotherapy were associated with the absence of VTE prophylaxis. Conversely, in the multivariate analysis, the only independent predictors of the need for thromboprophylaxis were intensive care unit admission within 30 days, prior DVT, surgery within 30 days, bed confinement for >3 days and outpatient status.
More recently, in a study using electronic medical record interrogation, the most reliable risk factors predictive of VTE were previous VTE, bed rest, CVC insertion and a diagnosis of cancer. Based on these elements, a risk assessment model was constructed [20] that was shown to be more accurate than the Kucher score, thus improving rates of thromboprophylaxis.
Recurrent Trousseau’s syndrome
While VTE frequently recurs within 6–12 months, recurrence is sometimes seen as late as 10 or more years after a first episode. For the sake of clarity and to avoid misdiagnoses in clinical practice, the diagnostic criteria of recurrent DVT or PE [3] are briefly summarized before we consider the risk factors contributing to such recurrences. A diagnosis of recurrence is considered definite or probable when all of the confirmatory tests already mentioned for DVT or PE are positive in a previously uninvolved or already involved but fully resolved site. The diagnosis is considered possible when confirmatory tests are not available or have not been done, or their results are indeterminate but the other criteria are present and the recurrence occurs in a previously uninvolved or fully resolved site.
In a study based on recurrent VTEs diagnosed during 10,198 person-years of follow-up [21], the overall cumulative percentages of VTE recurrence were 5.2 % at 1 month, 10.1 % at 6 months, almost 13 % at 1 year and slightly over 30 % at 10 years. Increasing age and BMI, extremity paresis, malignant tumors and neurosurgery were independent predictors of first overall VTE recurrence. Thus, the occurrence of a malignant tumor resulted in more than twofold increased risk for recurrent VTE, which rose to more than fourfold in patients receiving concomitant chemotherapy. In turn, concurrent chemotherapy interacted with the patient’s age and sex, with the risk of recurrence being higher in males and in older patients.
Arterial thromboembolism
Venous and arterial thromboses have usually been considered as separate entities with different etiologies. Arterial thrombosis usually follows the rupture of an atherosclerotic plaque and intraplaque hemorrhage. However, more recent data indicate a link between venous and arterial thromboses. Thus, age, obesity, smoking, diabetes mellitus, blood hypertension, hypertriglyceridemia and the metabolic syndrome are considered risk factors for both vascular complications. In addition, concurrent venous and arterial thromboses frequently occur in several clinical conditions, including the APS, hyperhomocysteinemia, infections and, above all, malignancies. A final possible link is the recent demonstration that, compared with matched controls, patients with VTE are more likely to suffer arterial thrombotic complications; conversely, the risk of incident venous thromboembolism is higher in patients with asymptomatic atherosclerosis or clinical manifestations of atherothrombosis [22]. Based on these observations, it has been speculated [23] that the activation of coagulation and inflammatory pathways triggered by biological stimuli in the arterial and venous systems is responsible for both types of vascular complications.
Tumor histotypes
Virtually all forms of cancer can be associated with a hypercoagulable state and hence with TS, including relatively rare tumors such as pleural mesothelioma [24] and renal Ewing’s sarcoma [25]. However, clinical observation has long shown that the relative risk of DVT/PE among patients with specific types of malignancy is highly variable, although relatively few studies have attempted to establish a reliable graded list. In the already mentioned study by Levitan et al. [9], the rate of DVT/PE was 16/10,000 for patients with head and neck cancers and 22/10,000 for those with bladder or breast cancer, but it steadily increased to 85, 96, 110, 117 and 120/10,000 patients for stomach cancer, lymphoma, and tumors of the pancreas, brain and ovaries, respectively.
In an outpatient population, Paneesha et al. [26] also found a broad-ranging risk of VTE for 17 cancer types, with the highest risk posed by pancreatic cancer [OR 9.65, 95 % confidence interval (CI) 5.51–16.91] followed by tumors of the head and neck (OR 8.24, 95 % CI 5.06–13.42). The lowest risk was determined for skin cancers (OR 0.89, 95 % CI 0.42–1.87 for melanoma; OR 0.74, 95 % CI, 0.32–1.69 for non-melanoma). Interestingly, the tumor-site-specific risk of outpatients differed from that of hospitalized patients.
In addition to the variable incidence of VTE in different types of malignancy, the highest risk of developing VTE seems to be associated with adenocarcinoma. In their study of 537 patients with lung carcinoma, Blom et al. [27] showed that the thrombotic risk in this group is 20-fold higher than in the general population and that patients with adenocarcinoma have a significantly higher risk than those with squamous cell carcinoma. The risk is even higher during chemo- and/or radiotherapy as well as in the presence of metastases.
Tumor grade likewise plays a role in identifying patients with cancer who are at high risk of VTE. In a study of 747 patients with solid tumors who were followed up for a median of 526 days, the risk of VTE was significantly higher in patients with high-grade than in those with low-grade tumors, suggesting that tumor differentiation and cancer-associated VTE are pathogenetically linked [6].
Cancer therapy and Trousseau’s syndrome
In addition to the increased risk of VTE in cancer patients with an indwelling CVC or a totally implanted medical device, a number of therapies have been linked to a higher incidence of VTE [28, 29]. This is the case for multiple myeloma patients during induction treatment with the immunomodulatory drug (IMiD) thalidomide in combination with anthracyclines and/or dexamethasone, in whom quantitative changes in coagulation factor levels often result in a prothrombotic state [30–32]. It has also been reported for thalidomide- and lenalidomide-based chemotherapeutic regimens, given the thrombogenic activities of these drugs [33, 34].
A risk of roughly 12 % of all-grade VTE has been reported in cancer patients receiving the humanized monoclonal antibody bevacizumab, which inhibits the activity of vascular endothelial growth factor (VEGF) and is used with increasing frequency to treat numerous cancers, including colorectal, lung, breast, kidney and ovarian cancer [35]. However, conflicting results have been published on the thrombogenicity of bevacizumab, in that a pooled analysis of over 6,000 patients in randomized phase II and III studies showed no statistically significant increases in the unadjusted or exposure-adjusted incidences of all-grade VTEs either for patients on bevacizumab versus controls in the overall population or as a function of tumor histotype [36].
Among hematopoietic growth factors, ESAs are frequently used in the oncological setting because of their ability to correct chemotherapy-induced bone marrow suppression and anemia. However, their administration to patients with cancer is associated with increased risks of VTE and higher mortality [37, 38], and even tumor progression [39].
In a retrospective analysis of the use of adjuvant hormonal therapy with tamoxifen in a cohort of 3,572 women with breast cancer [40], a coincidence was demonstrated between the introduction of this drug and the clustering of VTE, with the risk being specifically due to tamoxifen. Accordingly, it was suggested that patients scheduled to receive tamoxifen should be carefully assessed for their susceptibility to VTE before therapy is initiated. The risk of VTE is considered lower, although not negligible, with anastrozole [41, 42]. Since the use of combined oral contraceptives is associated with an increased risk of VTE [43], the Society of Family Planning recommends that women of childbearing age who are being treated for cancer should avoid, whenever possible, combined estrogen and progestin contraceptives because they may further increase the risk of VTE [44].
Pathogenetic mechanisms
The pathogenetic mechanism underlying cancer-related thromboembolic events is still largely unknown, but it is presumably multifactorial. Since these complications may appear even before or at the time the tumor is diagnosed, their occurrence should be considered independently of the coagulopathies arising in patients receiving cancer therapies or biological agents, as the treatment itself is likely to play a triggering role.
One of the many insights ascribed to the German pathologist Rudolf Virchow dates back over 150 years ago, when he suggested that for thrombogenesis to occur three components should be fulfilled. These pathophysiological mechanisms, now referred to as “Virchow’s triad,” have been ascribed to VTE as well and they occur independently of the underlying clinical condition, hence within and outside the oncological setting: (a) decreased rate of blood flow, resulting in stasis; (b) enhanced blood clotting tendency, triggered by inflammation and changes in growth factor levels, both of which favor hemostatic and platelet activation; (c) anatomical and structural changes in the blood vessel walls.
-
(a)
To note just a few examples, patients with cachexia-inducing neoplasias such as pancreatic cancer and those with bone-involving or bone-metastasizing tumors such as multiple myeloma or prostate cancer are often confined to bed and thus immobilized. In patients with a bulky mediastinal mass and superior vena cava syndrome, as may occur in Hodgkin lymphoma, there is venous blood engorgement in the vena cava district. Both of these clinical conditions frequently result in slower blood flow and hence in venous stasis, predisposing these patients to VTE.
-
(b)
A number of coagulation disorders have been recognized in cancer patients, ascribable to factors such as tumor growth features, neo-angiogenesis with abnormal endothelial cells, impaired myelopoiesis, hypoproteinemia or the growth of metastatic lesions with organ dysfunction secondary to metastatic invasion [45]. In this context, tissue factor, also called thrombokinase or CD142, is of particular interest. This protein is present in subendothelial tissue and leukocytes and it is the primary cellular initiator of blood coagulation. Tissue factor is in fact involved in the cancer-related hypercoagulability that characterizes TS, tumor growth, angiogenesis and metastasis [46]. The expression of mutant K-ras, epidermal growth factor receptor, phosphatase and tensin homolog or p53 results in increased levels and activity of CD142, and thus to tumor aggressiveness, neo-angiogenesis and TS. A similar up-regulation of the thrombin receptor (protease-activated receptor-1) has been described in cancer cells expressing oncogenic K-ras [46].
-
(c)
The heterogeneity of endothelial cells depending on the vascular bed has been established by microarray analyses. This finding implies that endothelial cells from the macrovascular versus microvascular web, from arteries versus veins and from different organs clearly differ in their gene expression profiles [47]. It was therefore hypothesized and eventually demonstrated that compared with the lumenal endothelium of other veins, in the valvular sinus endothelium of the great saphenous vein the anticoagulant proteins thrombomodulin and the endothelial protein C receptor are up-regulated while, conversely, the pro-coagulant protein von Willebrand factor is down-regulated [48], thus accounting for the more thromboresistant phenotype of the endothelium lining the valve pockets. Whether analogous findings can be extended to all or the large majority of vein districts remains to be ascertained.
A novel mechanism that extends our understanding of cancer-related thrombosis was recently proposed. In a murine model of chronic myelogenous leukemia, the presence of malignant and non-malignant neutrophils was shown to enhance the generation of neutrophil extracellular traps (NETs) [49]. Increased NET generation has also been detected in mammary and lung carcinoma models. Thus, predisposition to NET formation seems to be a frequent property of the peripheral blood neutrophils of cancer patients. When a minor systemic infection was simulated in tumor bearing and in control mice, large amounts of chromatin and a prothrombotic state were detected in the tumor bearing but not in the control animals. Under the experimental conditions adopted in that study, it was postulated that large quantities of extracellular DNA are released from NETs at late stages of cancer or following a minor infection, and this excess chromatin exerts procoagulant and prothrombotic effects [49].
However, it should be underscored that no coagulopathy can be predicted a priori based on abnormalities in any one of the components of Virchow’s triad. Rather, coagulopathy, especially in the oncological setting, must be understood as a multifactorial and complex process that is likely to result from a close interaction among the various components [50].
Prophylaxis and treatment
The therapeutic approach to VTE in tumor-bearing patients is basically similar to that of unprovoked symptomatic VTE occurring in patients with non-neoplastic diseases. However, the appearance of a tumor obviously imposes the need to therapeutically address both the tumor and the coagulopathy. It should also be emphasized that, as clearly shown by observational studies [26, 51] and as discussed earlier in this review, the risk is variable according to the tumor type, the natural history of each tumor and even depending on whether the cancer patient is post-surgical/hospitalized or seen as an outpatient [26].
Unfractionated heparin, vitamin K antagonists (VKA) such as warfarin and in some cases fondaparinux sodium are usually advised for the treatment of VTE. Low-molecular-weight heparins (LMWH) can be recommended for initial and continuous anticoagulant treatment as well as for the prevention of VTE in oncological patients [30]. An initial 7- to 10-day course of subcutaneous LMWH followed by secondary prophylaxis with an oral VKA is a well-established approach to significantly reducing the risk of recurrent thromboembolic events [51].
Venous thromboembolism associated with the use of immunomodulatory drugs or biological agents merits particular attention. As noted above, in addition to hematologic toxicity, the most common adverse event of the antiangiogenic and immunomodulatory drugs thalidomide and lenalidomide is in fact VTE [31, 33, 34]. These drugs are often administered in association with dexamethasone in patients with relapsed/refractory multiple myeloma; for the treatment of newly diagnosed myeloma; in association with alkylating agents such as cyclophosphamide and melphalan; or combined with novel agents, including bortezomib, carfilzomib and elotuzumab as highly active regimens. Regardless of the therapeutic intent, secondary prophylaxis with VKA is strongly warranted [34]. Also of concern is the above-mentioned higher risk of VTE in patients receiving the novel antiangiogenic agent bevacizumab [35, 36].
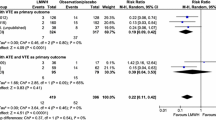
In the last few years, the introduction of novel oral anticoagulants has remarkably enlarged the therapeutic perspectives of VTE [52]. Among the newer drugs, the following have been extensively investigated: (a) fondaparinux, a synthetic and highly sulfated pentasaccharide that binds to antithrombin with high affinity, resulting in a conformational change in antithrombin that significantly increases its ability to inactivate factor Xa; (b) rivaroxaban and apixaban, which act as factor Xa inhibitors and (c) dabigatran etexilate, an oral direct thrombin inhibitor. These novel anticoagulants lack some of the limitations of VKA and do not require routine monitoring.
No reliable data are so far available regarding the use of these drugs in the oncological setting, but indirect comparison with warfarin, the current standard of care for the prevention of stroke in chronic non-valvular atrial fibrillation, indicates that either dabigatran (110 mg twice daily) or apixaban (5 mg twice daily) are similarly effective for stroke prevention compared to warfarin, although apixaban has a better safety profile than 150 mg of rivaroxaban or dabigatran twice daily in terms of a lower occurrence of major bleeding. Conversely, 150 mg dabigatran twice daily seems to be better than rivaroxaban in the prevention of stroke [53]. Despite the limited practical use of indirect comparison studies and even though the new oral anticoagulants may indeed be more efficacious than warfarin for the prevention of VTE in cancer patients (as demonstrated in those with atrial fibrillation [54]), large randomized clinical trials comparing the efficacy and safety of these three novel anticoagulants are clearly needed to determine the optimal approach to the prevention and treatment of cancer-related coagulopathy. In patients for whom there is clinical equipoise as to whether anticoagulation therapy should be continued or interrupted, extended anticoagulation with apixaban has been shown to reduce the risk of recurrent VTE without inducing a higher rate of major bleeding [55].
A crucial point in the treatment of TS is to avoid both over- and under treatment. To this end, the identification of those factors potentially involved in VTE recurrence is essential, as it would help to tailor the best anticoagulation regimen and its most suitable duration. Aspirin is conventionally regarded as an agent that prevents arterial thrombosis, an effect mediated through the inhibition of platelet cyclooxygenase-1 and resulting in the decreased synthesis of thromboxane A2 (platelet-activating eicosanoid) [56]. However, when given at a low dose of 100 mg daily for up to 4 years with the aim of preventing VTE recurrence, aspirin was shown to significantly reduce the rate of major vascular events but not the rate of VTE recurrence [57].
Recently, an international consensus working group of experts developed an excellent set of guidelines for the management of VTE in cancer patients [58]. The definition of levels of evidence according to the GRADE system (A: high; B: moderate; C: low; D: very low) and the classification of recommendations (strong: grade 1; weak: grade 2; best clinical practice: guidance) are provided in the same paper [58]. In recognition of the importance of these guidelines in clinical practice and with the aim of establishing a source of rapid consultation for the most common clinical situations, we have arbitrarily transformed their detailed descriptions into a concise table (Table 3). Also, the same group of experts elaborated international good clinical practice guidelines with the aim of overcoming the lack of consensus on the treatment of symptomatic VTE in cancer patients bearing an indwelling CVC [59]. Briefly, either LMWH or VKA should be used for at least 3 months. If the CVC is uninfected, correctly positioned and obviously functional, it can be kept in situ. Nonetheless, regardless of its permanence or removal, the duration of anticoagulation has not been established. In terms of catheter-related VTE prophylaxis, the type of catheter (open ended rather than closed ended), its position (above, below or at the same level as the junction of the superior vena cava with the right atrium), and its placement procedure may affect the occurrence of VTE. It is recommended that a CVC be inserted in the right jugular vein, with the distal end of the catheter located at the junction of the superior vena cava with the right atrium. The use of anticoagulation for the routine prophylaxis of catheter-related VTE is not recommended [59].
Personal observations
From January 1996 to December 2011, 251 patients who suffered a VTE were recruited from a single (our own) center. Within this group, 159 (63.3 %) did not have any known malignancies (group 1: Table 4) whereas in the remaining 92 (36.6 %) different types of malignancy had been diagnosed (group 2: Table 5). In group 1, the mean age of the patients was 61.2 years and the female-to-male ratio was 1.16:1; in group 2, the corresponding values were 66.4 years and 1:1.3. The prevalence and incidence rate of all types of VTE was 5.6 % and 6.3 per 1,000 person-years, respectively. In both groups, the diagnoses of the underlying diseases largely reflected the pathologies most commonly observed by ourselves based on our specific skills. This explains the higher percentages of connective tissue diseases and chronic HCV infection (including HCV-related mixed cryoglobulinemia) than would be expected based solely on the relative frequency of these clinical conditions. Conversely, VTE in patients with chronic atrial fibrillation accounted for only 6.3 % of the patients in the non-neoplastic group since very few such patients are hospitalized in our center, whereas the occurrence of this complication would have been remarkably higher in a cardiologic setting.
The same is true when one specifically considers the patients in group 2, with neoplastic disease. Multiple myeloma was the most frequent malignancy in tumor-associated VTE because the large majority of patients with myelomas who are diagnosed in Apulia and in the neighboring geographical areas are referred to our center, given our established reputation in the diagnosis and treatment of this neoplasia. An additional factor is the thrombogenic activity of the IMiDs thalidomide and lenalidomide, which are frequently prescribed for the treatment of myeloma. Regarding the chronological relationships between the diagnosis of cancer and VTE occurrence, in 58 patients (63 %), the vascular complication occurred from months to years after the tumor was first detected; in 23 patients (25 %) VTE and neoplasia were concomitantly diagnosed and in the remaining 11 patients (12 %) VTE preceded tumor detection by a few to several months.
In both groups of patients, the thromboembolic events, and consequently the corresponding spectrum of clinical features, were largely variable and obviously reflected the severity of the vascular event as well as the presence of co-morbidities. Clinical manifestations ranged from dramatic and often rapidly lethal pulmonary and cerebral embolism to VTE originating in the deep and superficial veins of the lower and upper limbs; from abdominal VTE affecting the portal, mesenteric and splenic veins to thrombi originating in the veins of the neck (Table 6). In several patients, more than one venous district and sometimes thrombosis involving both the venous and the arterial districts were diagnosed. The probability of death within 180 days from initial hospitalization was 0.87 among patients with neoplastic disease who suffered a VTE versus 0.31 among those with VTE and no malignancy (p < 0.001).
Conclusions
Trousseau’s syndrome is a relatively frequent and sometimes deadly cancer-related coagulopathy. Given the high prevalence of cancer patients hospitalized in nearly every Internal Medicine Department, it is essential that all internists: (a) be aware that a previously undiagnosed cancer may be detected in patients with unprovoked VTE; (b) become familiar with clinical situations likely to give rise to VTE; (c) develop the skills to recognize and assess the risk factors that predispose cancer patients to a first episode of VTE and to its possible recurrence; (d) keep in mind that iatrogenic VTE is not unusual when thrombogenic chemotherapeutic agents (including IMiDs, antiangiogenic drugs, ESAs, monoclonal antibodies and antiestrogen hormones) are administered; (e) learn to manage thromboprophylaxis and to appropriately treat each specific event.
Abbreviations
- APS:
-
Antiphospholipid syndrome
- CI:
-
Confidence interval
- CT:
-
Computed tomography
- CVC:
-
Central venous catheter
- DVT:
-
Deep-vein thrombosis
- ESAs:
-
Erythropoiesis-stimulating agents
- IMiD:
-
Immunomodulatory drug
- LMWH:
-
Low-molecular-weight heparins
- NETs:
-
Neutrophil extracellular traps
- PE:
-
Pulmonary embolism
- SIR:
-
Standardized incidence ratio
- β2GPI:
-
Beta-2 glycoprotein I
- TS:
-
Trousseau’s syndrome
- VEGF:
-
Vascular endothelial growth factor
- VKA:
-
Vitamin K antagonists
- VTE:
-
Venous thromboembolism
References
Trousseau A (1865) Phlegmasia alba dolens. Clinique Mèdicale de l’Hôtel-Dieu de Paris 3:654–712
Bouillard JB, Bouillaud S (1823) De l’obliteration des veines et de son influence sur la formation des hydropisies partielles: consideration sur la hydropisies passive et general. Arch Gen Med 1:188–204
Silverstein MD, Heit JA, Mohr DN, Petterson TM, O’Fallon WM, Melton LJ III (1998) Trends in the incidence of deep vein thrombosis and pulmonary embolism: a 25-year population-based study. Arch Intern Med 158:585–593
Spencer FA, Emery C, Lessard D, Anderson F, Emani S, Aragam J, Becker RC, Goldberg RJ (2006) The Worcester Venous Thromboembolism study: a population-based study of the clinical epidemiology of venous thromboembolism. J Gen Intern Med 21:722–727
Lee CH, Cheng CL, Lin LJ, Tsai LM, Yang YH (2011) Epidemiology and predictors of short-term mortality in symptomatic venous thromboembolism. Circ J 75:1998–2004
Ahlbrecht J, Dickmann B, Ay C, Dunkler D, Thaler J, Schmidinger M, Quehenberger P, Haitel A, Zielinski C, Pabinger I (2012) Tumor grade is associated with venous thromboembolism in patients with cancer: results from the Vienna Cancer and Thrombosis Study. J Clin Oncol 30:3870–3875
Noble S, Pasi J (2010) Epidemiology and pathophysiology of cancer-associated thrombosis. Br J Cancer 102(Suppl 1):S2–S9
Caruso V, Di Castelnuovo A, Meschengieser S, Lazzari MA, de Gaetano G, Storti S, Iacoviello L, Donati MB (2010) Thrombotic complications in adult patients with lymphoma: a meta-analysis of 29 independent cohorts including 18 018 patients and 1149 events. Blood 115:5322–5328
Levitan N, Dowlati A, Remick SC, Tahsildar HI, Sivinski LD, Beyth R, Rimm AA (1999) Rates of initial and recurrent thromboembolic disease among patients with malignancy versus those without malignancy. Risk analysis using Medicare claims data. Medicine (Baltimore) 78:285–291
Verso M, Agnelli G (2003) Venous thromboembolism associated with long-term use of central venous catheters in cancer patients. J Clin Oncol 21:3665–3675
Ioannou Y, Zhang JY, Qi M, Gao L, Qi JC, Yu DM, Lau H, Sturgess AD, Vlachoyiannopoulos PG, Moutsopoulos HM, Rahman A, Pericleous C, Atsumi T, Koike T, Heritier S, Giannakopoulos B, Krilis SA (2011) Novel assays of thrombogenic pathogenicity in the antiphospholipid syndrome based on the detection of molecular oxidative modification of the major autoantigen beta2-glycoprotein I. Arthritis Rheum 63:2774–2782
Gavish I, Brenner B (2011) Air travel and the risk of thromboembolism. Intern Emerg Med 6:113–116
Heit JA, Silverstein MD, Mohr DN, Petterson TM, O’Fallon WM, Melton LJ III (2000) Risk factors for deep vein thrombosis and pulmonary embolism: a population-based case-control study. Arch Intern Med 160:809–815
Young A, Chapman O, Connor C, Poole C, Rose P, Kakkar AK (2012) Thrombosis and cancer. Nat Rev Clin Oncol 9:437–449
White RH, Chew HK, Zhou H, Parikh-Patel A, Harris D, Harvey D, Wun T (2005) Incidence of venous thromboembolism in the year before the diagnosis of cancer in 528,693 adults. Arch Intern Med 165:1782–1787
Kucher N, Koo S, Quiroz R, Cooper JM, Paterno MD, Soukonnikov B, Goldhaber SZ (2005) Electronic alerts to prevent venous thromboembolism among hospitalized patients. N Engl J Med 352:969–977
Chopard P, Spirk D, Bounameaux H (2006) Identifying acutely ill medical patients requiring thromboprophylaxis. J Thromb Haemost 4:915–916
Ay C, Simanek R, Vormittag R, Dunkler D, Alguel G, Koder S, Kornek G, Marosi C, Wagner O, Zielinski C, Pabinger I (2008) High plasma levels of soluble P-selectin are predictive of venous thromboembolism in cancer patients: results from the Vienna Cancer and Thrombosis Study (CATS). Blood 112:2703–2708
Kucher N, Spirk D, Baumgartner I, Mazzolai L, Korte W, Nobel D, Banyai M, Bounameaux H (2010) Lack of prophylaxis before the onset of acute venous thromboembolism among hospitalized cancer patients: the SWIss Venous ThromboEmbolism Registry (SWIVTER). Ann Oncol 21:931–935
Woller SC, Stevens SM, Jones JP, Lloyd JF, Evans RS, Aston VT, Elliott CG (2011) Derivation and validation of a simple model to identify venous thromboembolism risk in medical patients. Am J Med 124:947–954
Heit JA, Mohr DN, Silverstein MD, Petterson TM, O’Fallon WM, Melton LJ III (2000) Predictors of recurrence after deep vein thrombosis and pulmonary embolism: a population-based cohort study. Arch Intern Med 160:761–768
Franchini M, Mannucci PM (2012) Association between venous and arterial thrombosis: clinical implications. Eur J Intern Med 23:333–337
Prandoni P, Piovella C, Pesavento R (2012) Venous thromboembolism and arterial complications. Semin Respir Crit Care Med 33:205–210
Matsui H, Nishinaka K, Oda M, Kubori T, Udaka F (2007) Trousseau syndrome due to pleural mesothelioma. Neurologist 13:205–208
Rizzo D, Barone G, Ruggiero A, Maurizi P, Furfaro IF, Castagneto M, Riccardi R (2011) Massive venous thrombosis of inferior vena cava as primary manifestation of renal Ewing’s sarcoma. Clin Nephrol 75:560–564
Paneesha S, McManus A, Arya R, Scriven N, Farren T, Nokes T, Bacon S, Nieland A, Cooper D, Smith H, O’Shaughnessy D, Rose P (2010) Frequency, demographics and risk (according to tumour type or site) of cancer-associated thrombosis among patients seen at outpatient DVT clinics. Thromb Haemost 103:338–343
Blom JW, Osanto S, Rosendaal FR (2004) The risk of a venous thrombotic event in lung cancer patients: higher risk for adenocarcinoma than squamous cell carcinoma. J Thromb Haemost 2:1760–1765
Manzoni M, Bencardino K, Piovella F, Chatzileontiadou S, Delfanti S, Riccardi A, Danova M, Corazza GR (2007) New agents in medical oncology and the risk of venous thromboembolism. J Exp Clin Cancer Res 26:185–194
Prandoni P, Falanga A, Piccioli A (2005) Cancer and venous thromboembolism. Lancet Oncol 6:401–410
Khosravi-Shahi P, Perez-Manga G (2009) International recommendations for the prevention and treatment of venous thromboembolism associated with cancer. Clin Drug Investig 29:625–633
Merchionne F, Perosa F, Dammacco F (2007) New therapies in multiple myeloma. Clin Exp Med 7:83–97
van Marion AM, Auwerda JJ, Lisman T, Sonneveld P, de Maat MP, Lokhorst HM, Leebeek FW (2008) Prospective evaluation of coagulopathy in multiple myeloma patients before, during and after various chemotherapeutic regimens. Leuk Res 32:1078–1084
Cives M, Milano A, Dammacco F, Silvestris F (2012) Lenalidomide in multiple myeloma: current experimental and clinical data. Eur J Haematol 88:279–291
Larocca A, Cavallo F, Mina R, Boccadoro M, Palumbo A (2012) Current treatment strategies with lenalidomide in multiple myeloma and future perspectives. Future Oncol 8:1223–1238
Nalluri SR, Chu D, Keresztes R, Zhu X, Wu S (2008) Risk of venous thromboembolism with the angiogenesis inhibitor bevacizumab in cancer patients: a meta-analysis. JAMA 300:2277–2285
Hurwitz HI, Saltz LB, Van CE, Cassidy J, Wiedemann J, Sirzen F, Lyman GH, Rohr UP (2011) Venous thromboembolic events with chemotherapy plus bevacizumab: a pooled analysis of patients in randomized phase II and III studies. J Clin Oncol 29:1757–1764
Bennett CL, Silver SM, Djulbegovic B, Samaras AT, Blau CA, Gleason KJ, Barnato SE, Elverman KM, Courtney DM, McKoy JM, Edwards BJ, Tigue CC, Raisch DW, Yarnold PR, Dorr DA, Kuzel TM, Tallman MS, Trifilio SM, West DP, Lai SY, Henke M (2008) Venous thromboembolism and mortality associated with recombinant erythropoietin and darbepoetin administration for the treatment of cancer-associated anemia. JAMA 299:914–924
Bohlius J, Wilson J, Seidenfeld J, Piper M, Schwarzer G, Sandercock J, Trelle S, Weingart O, Bayliss S, Djulbegovic B, Bennett CL, Langensiepen S, Hyde C, Engert A (2006) Recombinant human erythropoietins and cancer patients: updated meta-analysis of 57 studies including 9353 patients. J Natl Cancer Inst 98:708–714
Aapro M, Jelkmann W, Constantinescu SN, Leyland-Jones B (2012) Effects of erythropoietin receptors and erythropoiesis-stimulating agents on disease progression in cancer. Br J Cancer 106:1249–1258
Onitilo AA, Doi SA, Engel JM, Glurich I, Johnson J, Berg R (2012) Clustering of venous thrombosis events at the start of tamoxifen therapy in breast cancer: a population-based experience. Thromb Res 130:27–31
Deitcher SR, Gomes MP (2004) The risk of venous thromboembolic disease associated with adjuvant hormone therapy for breast carcinoma: a systematic review. Cancer 101:439–449
Howell A, Cuzick J, Baum M, Buzdar A, Dowsett M, Forbes JF, Hoctin-Boes G, Houghton J, Locker GY, Tobias JS (2005) Results of the ATAC (Arimidex, Tamoxifen, Alone or in Combination) trial after completion of 5 years’ adjuvant treatment for breast cancer. Lancet 365:60–62
Rott H (2012) Thrombotic risks of oral contraceptives. Curr Opin Obstet Gynecol 24:235–240
Patel A, Schwarz EB (2012) Cancer and contraception. Release date May 2012. SFP Guideline #20121. Contraception 86:191–198
Kvolik S, Jukic M, Matijevic M, Marjanovic K, Glavas-Obrovac L (2010) An overview of coagulation disorders in cancer patients. Surg Oncol 19:e33–e46
Rak J, Milsom C, May L, Klement P, Yu J (2006) Tissue factor in cancer and angiogenesis: the molecular link between genetic tumor progression, tumor neovascularization, and cancer coagulopathy. Semin Thromb Hemost 32:54–70
Chi JT, Chang HY, Haraldsen G, Jahnsen FL, Troyanskaya OG, Chang DS, Wang Z, Rockson SG, van de Rijn M, Botstein D, Brown PO (2003) Endothelial cell diversity revealed by global expression profiling. Proc Natl Acad Sci USA 100:10623–10628
Brooks EG, Trotman W, Wadsworth MP, Taatjes DJ, Evans MF, Ittleman FP, Callas PW, Esmon CT, Bovill EG (2009) Valves of the deep venous system: an overlooked risk factor. Blood 114:1276–1279
Demers M, Krause DS, Schatzberg D, Martinod K, Voorhees JR, Fuchs TA, Scadden DT, Wagner DD (2012) Cancers predispose neutrophils to release extracellular DNA traps that contribute to cancer-associated thrombosis. Proc Natl Acad Sci USA 109:13076–13081
Wolberg AS, Aleman MM, Leiderman K, Machlus KR (2012) Procoagulant activity in hemostasis and thrombosis: Virchow’s triad revisited. Anesth Analg 114:275–285
Buller HR, Prins MH (2003) Secondary prophylaxis with warfarin for venous thromboembolism. N Engl J Med 349:702–704
Kennedy B, Gargoum FS, Kennedy L, Khan F, Curran DR, O’Connor TM (2012) Emerging anticoagulants. Curr Med Chem 19:3388–3416
Mantha S, Ansell J (2012) An indirect comparison of dabigatran, rivaroxaban and apixaban for atrial fibrillation. Thromb Haemost 108:476–484
Miller CS, Grandi SM, Shimony A, Filion KB, Eisenberg MJ (2012) Meta-analysis of efficacy and safety of new oral anticoagulants (dabigatran, rivaroxaban, apixaban) versus warfarin in patients with atrial fibrillation. Am J Cardiol 110:453–460
Agnelli G, Buller HR, Cohen A, Curto M, Gallus AS, Johnson M, Porcari A, Raskob GE, Weitz JI (2013) Apixaban for extended treatment of venous thromboembolism. N Engl J Med 368:699–708
Warkentin TE (2012) Aspirin for dual prevention of venous and arterial thrombosis. N Engl J Med 367:2039–2041
Brighton TA, Eikelboom JW, Mann K, Mister R, Gallus A, Ockelford P, Gibbs H, Hague W, Xavier D, Diaz R, Kirby A, Simes J (2012) Low-dose aspirin for preventing recurrent venous thromboembolism. N Engl J Med 367:1979–1987
Farge D, Debourdeau P, Beckers M, Baglin C, Bauersachs RM, Brenner B, Brilhante D, Falanga A, Gerotzafias GT, Haim N, Kakkar AK, Khorana AA, Lecumberri R, Mandala M, Marty M, Monreal M, Mousa SA, Noble S, Pabinger I, Prandoni P, Prins MH, Qari MH, Streiff MB, Syrigos K, Bounameaux H, Buller HR (2012) International clinical practice guidelines for the treatment and prophylaxis of venous thromboembolism in patients with cancer. J Thromb Haemost
Debourdeau P, Farge D, Beckers M, Baglin C, Bauersachs RM, Brenner B, Brilhante D, Falanga A, Gerotzafias GT, Haim N, Kakkar AK, Khorana AA, Lecumberri R, Mandala M, Marty M, Monreal M, Mousa SA, Noble S, Pabinger I, Prandoni P, Prins MH, Qari MH, Streiff MB, Syrigos K, Buller HR, Bounameaux H (2013) International clinical practice guidelines for the treatment and prophylaxis of thrombosis associated with central venous catheters in patients with cancer. J Thromb Haemost 11:71–80
Acknowledgments
This study was supported in part by the ‘Associazione Italiana per la Ricerca sul Cancro’ (AIRC), the Italian Ministry of University and Scientific and Technologic Research and the Finalized Project of the Apulia Region “Biotecnoter.”
Conflict of interest
The authors have no conflicts of interests to declare.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Dammacco, F., Vacca, A., Procaccio, P. et al. Cancer-related coagulopathy (Trousseau’s syndrome): review of the literature and experience of a single center of internal medicine. Clin Exp Med 13, 85–97 (2013). https://doi.org/10.1007/s10238-013-0230-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10238-013-0230-0