Abstract
Metabolic syndrome is characterized by increased cardiovascular risk. Pentraxin 3 (PTX3), an acute phase protein, is involved in atherosclerosis. No information is available on PTX3 plasma concentrations in metabolic syndrome and on its associations with metabolic alterations and subclinical atherosclerosis. The aim of this study was to assess PTX3 plasma levels in metabolic syndrome patients compared to control subjects and their potential associations with anthropometric and clinical components of the syndrome as well as with carotid artery intima-media thickness (cIMT), a marker of subclinical atherosclerosis. Plasma was obtained from metabolic syndrome patients (NCEP-ATP III criteria n = 41, 20 M/21F) and by age-matched control subjects (n = 32, 16 M/16F). PTX3 was measured using sandwich ELISA and cIMT with ultrasound. Compared to those of the control subjects, plasma levels of PTX3 were higher (+~100%, P = 0.0009) in metabolic syndrome patients. In univariate analysis, plasma PTX3 was negatively (P = 0.005) associated with high-density lipoprotein (HDL) cholesterol and positively (P = 0.046) with plasma triglycerides and with cIMT (P = 0.045) in the patients (n = 41). In multivariate analysis the direct association between PTX3 and cIMT was no longer significant after correction for HDL. None of these associations were detected in the control patients. These data demonstrate that PTX3, a novel marker of vascular disease, is higher in patients with metabolic syndrome associated with subclinical atherosclerosis. In addition, PTX3 is significantly independently correlated with low HDL cholesterol, but not with cIMT, suggesting a novel association between PTX3 and atherogenic lipid profile.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Increased cardiovascular risk is a common feature of the metabolic syndrome from the early stages of the disease, prior to the development of clinical atherosclerosis [1–3]. Carotid artery intima-media thickness (cIMT), a well-established surrogate marker of subclinical atherosclerosis is higher in metabolic syndrome patients without a clinical history of overt atherosclerosis compared with the general population [3, 4]. Among the cluster of cardiovascular risk factors associated with the syndrome, atherogenic dyslipidemia, clinically presenting as low high-density lipoproteins (HDLs) and high plasma triglycerides promotes atherogenesis [5].
Pentraxin 3 (PTX3) is an inducible protein belonging to the C-reactive protein (CRP) family. PTX3, which is highly expressed by vascular cells in response to inflammatory stimuli, has recently been associated with atherosclerosis and its complications [6]. In particular, PTX3 seems to be involved in the pathogenesis and progression of atherosclerosis, as well as in acute cardiovascular events, since it has been shown to induce in vitro the expression of tissue factor in endothelial cells [7, 8]. Also consistent with this view, PTX3 production is stimulated by known cardiovascular risk factors, including oxidized LDLs and inflammation-related stimuli [9, 10]. In a clinical setting, PTX3 expression has been demonstrated in atherosclerotic plaques and in plasma of patients undergoing percutaneous coronary intervention [11, 12]. In addition, PTX3 plasma levels increase during acute myocardial infarction [13] representing an independent predictor of mortality [14] and high plasma PTX3 is reported in selected populations with a higher incidence of cardiovascular disease [15–17].
Potential changes in PTX3 plasma concentrations in metabolic syndrome and their associations with vascular and metabolic alterations of the syndrome are unknown. In this study we therefore tested the hypothesis that metabolic syndrome is associated with higher PTX3 plasma concentrations and that PTX3 is associated with cardiometabolic risk factors and/or vascular disease in this setting. To this end, we measured plasma levels of PTX3 in a population of metabolic syndrome patients without clinically overt atherosclerosis compared with a group of age- and sex-matched control subjects. We also explored the potential associations of plasma PTX3 with carotid artery IMT as a surrogate marker of subclinical atherosclerosis as well as with the anthropometric and clinical components of the syndrome.
Materials and methods
Patients
Forty-one metabolic syndrome patients (20 M/21F) were recruited for the study from the Metabolic outpatient Unit in Trieste Hospital. The inclusion criteria were diagnosis of metabolic syndrome according to the National Cholesterol Education Program-Adult Treatment Panel III (NCEP-ATP III) criteria [18]. Thirty-two age- and sex-matched healthy subjects (16 M/16F) were recruited as the control group. For all subjects, the exclusion criteria were the diagnosis or evidence of liver failure or disease, renal failure (plasma creatinine above 1.5 mg/dl), cancer, chronic autoimmune and thyroid disease, concomitant acute inflammatory diseases (as suggested by clinical history and by white blood cells > 10,000/mm3), and history of alcohol abuse or self-reported daily alcohol intake above 50 g. Six patients (3 M/3F) and four control subjects (2 M/2F) were current smokers or had quit smoking less than one year previous. Nineteen patients were taking hypolipidemic drugs at the time of the study, while all of the control subjects were free of hypolipidemic medications. Females taking hormonal estrogen therapy were excluded from the study. On a baseline screening visit each subject was admitted to the outpatient ward in the morning after overnight fasting. A blood sample and a detailed medical history were collected and a baseline examination was performed. Blood pressure was measured on both arms using a standard mercury sphygmomanometer. Weight and height were measured in duplicate and recorded to the nearest 0.1 kg and 0.5 cm, respectively. Body mass index was calculated as weight (in kilograms) divided by height (in meters) squared. Waist circumference was measured on bare skin during mid-respiration at the natural indentation between the tenth rib and the iliac crest to the nearest 0.5 cm. All variables were measured in duplicate and the average of two measurements was used for patient classification. For all samples plasma was rapidly separated and stored at −80°C until analysis. Finally, the patients underwent carotid artery ultrasound to determine cIMT as described below. The study protocol was approved by the local Ethical Committee. All patients were given detailed oral and written information on the study aims and risks and they gave written consent before entering the study.
Laboratory methods
Plasma glucose, HDL and LDL cholesterol, and plasma triglycerides were measured using standard methods. Plasma high sensitive CRP was measured using ELISA (Diagnostics Biochem Canada Inc. London, ON, Canada).
Determination of plasma PTX3
Plasma PTX3 concentrations were quantified using the sandwich ELISA detection system (Alexis Biochemical), as follows. 96 well-ELISA plates were coated with 100 μl of antibody against human PTX3, 700 ng/ml in 100 μl coating buffer (15 mM carbonate buffer pH 9.6) and incubated overnight at 4°C. After incubation, the plates were washed and 300 μl of 5% dry milk in washing buffer were then added. The plates were incubated for 2 h at room temperature and then washed three times with washing buffer. 50 μl of diluted plasma or 50 μl (in duplicate) recombinant human PTX3 standard (scalar dilution: 75 pg/ml to 2.4 ng/ml) were added and then incubated for 2 h at 37°C. The plates were washed five times with washing buffer, and 25 ng/ml of antibody to human PTX3 (Biotin) were then added in each well. 100 μl/well streptavidin-horseradish peroxidase diluted 1:4,000 were added and the plates incubated for 1 h at room temperature. After incubation the plates were washed five times and 100 μl of chromogen substrate ABTS were added. Plates were read after 15 min at 405 nm in an automatic ELISA reader. In our hands, the lowest detection limit of PTX3 in the sandwich ELISA kit was 0.12 ng/ml.
Detection of carotid atherosclerosis
Carotid artery ultrasound was performed by two experienced sonographers blinded to laboratory results with an Acuson Sequoia 512 platform (Siemens/Acuson) equipped with the 8L5 linear array transducer. Patients were placed in a supine position and images were taken from longitudinal sections of the carotid artery in a standardized fashion. The flow divider served as a landmark to define four segments of ≈ 15 mm length: the proximal internal carotid artery separated from the carotid bulb at the level of the flow divider followed by the distal and proximal common carotid artery. All scans were stored digitally on the internal hard disk of the ultrasound system for subsequent analysis. The combined IMT was calculated as the mean of 16 single measurements taken bilaterally from each segment at both the anterior and the posterior carotid artery wall.
Statistical analysis
Results are expressed as mean ± SEM. A P-value of 0.05 or less was considered statistically significant. Significance between two groups was determined by unpaired Student’s t-test. Post hoc analysis was performed, where appropriate, by using a t-test with Bonferroni’s adjustment. Univariate and multivariate regression analyses were performed using the Statview software for Windows (version 5; S.A.S. Institute Inc, Cary, NC, USA).
Results
Clinical characteristics of study subjects and plasma PTX3 levels
Table 1 shows the demographic, biochemical, and clinical characteristics of the study subjects. The metabolic syndrome patients did not differ from the control subjects in age and gender distribution but they had expected anthropometric and metabolic alterations including increased waist circumference, HOMA, plasma glucose, triglycerides, CRP, and blood pressure with lower HDL-cholesterol. Carotid artery IMT in the patients was 0.8 ± 0.04 mm, in line with previous reports in literature on populations comparable in age and clinical characteristics [4].
Plasma levels of PTX3 in the metabolic syndrome and control subjects are shown in Fig. 1. The patients were characterized by significantly (P = 0.0009) higher plasma concentrations of PTX3 than those of the control subjects.
Correlation of plasma PTX3 with clinical and anthropometric parameters of the metabolic syndrome as well as with subclinical atherosclerosis
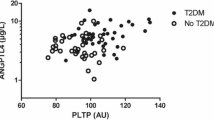
The role of PTX3 in atherosclerosis prompted us to evaluate whether a correlation occurs between plasma PTX3 and cardiometabolic risk factors in the syndrome. As shown in Table 2, in univariate analysis plasma levels of PTX3 were correlated negatively (P = 0.005) with HDL cholesterol and positively (P = 0.046) with plasma triglycerides. In contrast, PTX3 did not correlate with any of the anthropometric and clinical parameters under evaluation in the control subjects (data not shown). To further define the association between PTX3 and HDL, the whole study population was subdivided into two groups according to HDL cholesterol levels (assuming a cut-off of 40 mg/dl in males and 50 mg/dl in females). The low HDL group included more metabolic syndrome patients, while age and gender distribution were not different in the two groups. Consistently with the previous observations, PTX3 levels were lower (P = 0.01) in the high HDL compared with the low HDL group (Fig. 2).
In addition, a direct (P = 0.045) association between PTX3 and cIMT was observed in the patients (Table 2). A multiple regression analysis was then performed to adjust the relationship between PTX3 and cIMT for HDL cholesterol in the syndrome. Results show that, in the patients the inverse association between PTX3 and cIMT was no longer significant following adjustment for HDL (P = 0.21).
Discussion
This study provides the first assessment of plasma PTX3 concentrations in the metabolic syndrome with subclinical atherosclerosis. The data demonstrates higher plasma PTX3 in metabolic syndrome patients compared with matched control individuals. PTX3 is a selective marker of vascular activation associated with atherosclerosis [6]. Plasma PTX3 levels increase during acute myocardial infarction [13] and in selected populations with a higher incidence of vascular disease [15–17]. We now observe in vivo that in the metabolic syndrome, which is characterized by increased cardiovascular risk, PTX3 plasma levels are significantly and consistently higher when compared with those in the control subjects. This finding is corroborated by the observation that 19 out of 41 patients were taking either statins or fibrates, potentially blunting vascular inflammation and affecting lipid levels. Therefore, the rise in PTX3 plasma concentrations could potentially have been underestimated by current data. In addition, the significant increase in plasma PTX3 did not reach pathological levels (≥ 4 ng/ml) [17], which is in line with the observation that the patients were free of a clinical history of cardiovascular disease and were characterized by subclinical atherosclerosis, as demonstrated by their carotid artery IMT. With regard to the control subjects, the reported values of plasma PTX3 in our study are well in line with previous data in literature [19].
In this study we also assessed the potential associations between PTX3 and cardiometabolic risk factors that characterize the metabolic syndrome. The data demonstrates a novel association between PTX3 and atherogenic lipid profile. In particular, PTX3 levels were higher in subjects with low HDL (which were mostly represented by patients with the metabolic syndrome) and in this group PTX3 was inversely correlated with HDL cholesterol. Low HDL-cholesterol is a strong predictor of cardiovascular disease both in the general and metabolic syndrome population [20, 21] and it is implicated in the progression of carotid artery intima-media thickening in the syndrome [22]. Thus, the novel inverse correlation between PTX3 and HDL cholesterol underscores the impact of atherogenic lipid profile on the cardiovascular risk associated with the syndrome. The underlying mechanisms are still unclear. Although several in vitro and in vivo studies have demonstrated a direct association between PTX3 expression and atherosclerosis [13–16, 23], it should be noted that a recent study reported a HDL-stimulated dose-dependent increase in PTX3 expression and production by endothelial cells, possibly contributing to the antiatherosclerotic properties of HDLs [24]. The reasons for these discrepant results are unclear and deserve further investigation. It is possible that the relationships between PTX3, atherosclerosis, and lipids are complex and are differently regulated in healthy and pathological conditions.
Elevated triglycerides in patients directly correlated with plasma PTX3. Since levels of triglycerides vary inversely with HDL cholesterol, this relationship is expected. However, a previous study suggested that plasma triglycerides have an independent role in vascular inflammation [25]. In addition, triglyceride-rich lipoproteins have been shown to stimulate the expression of leukocyte adhesion molecules and monocyte adherence in the presence, but not in the absence of TNFα [26]. Thus, increased triglycerides may contribute to amplify vascular inflammation in the metabolic syndrome and could possibly further enhance PTX3 production. Additional in vitro studies are needed to directly test this hypothesis.
Carotid artery IMT is increasingly recognized as a significant independent predictor of adverse cardiovascular outcomes in both cross-sectional and longitudinal studies [27, 28]. The prevalence of carotid arterial thickening is higher in patients with the metabolic syndrome without a clinical history of cardiovascular disease [4] and in this population cIMT further progresses over time [22]. In this study we found a positive association between carotid artery IMT and PTX3 plasma levels, which was not however confirmed in multivariate analysis. These findings suggest that in addition to PTX3 other factors play an important role in promoting carotid artery media thickening in the syndrome.
In this study, we did not observe a statistically significant association between PTX3 and LDL-cholesterol either in the metabolic syndrome group or in the control group. This finding is in line with previous data from our group suggesting a potential link between LDL cholesterol and PTX3 in the presence but not in the absence of LDL-hypercholesterolemia [29]. Overall, the present findings introduce the novel concept that altered plasma PTX3 concentrations occur in the metabolic syndrome with subclinical atherosclerosis and are associated with atherogenic lipid profile. Lack of association in the control group suggests that potential pathological processes linking PTX3 and plasma lipids do not occur in the presence of low PTX3 plasma concentrations.
Although PTX3 is implicated in cardiovascular disease, its pathogenic or protective role is currently under investigation [6, 30]. In this regard, the finding of increased PTX3 plasma levels and their inverse association with HDL cholesterol in the syndrome deserves further attention to establish whether increased PTX3 is beneficial or deleterious in this setting.
In conclusion, our data shows that plasma PTX3 levels are higher in the metabolic syndrome associated with subclinical atherosclerosis and demonstrates a novel association with reduced HDL cholesterol. To our knowledge, this is the first report of increased plasma PTX3 in metabolic syndrome patients. Given its involvement in vascular disease and its correlation with clinical outcome, the current findings suggest a possible mechanism by which PTX3 may be involved in the increased cardiometabolic risk associated with the syndrome.
References
Koh KK, Han SH, Quon MJ (2005) Inflammatory markers and the metabolic syndrome: insights from therapeutic interventions. J Am Coll Cardiol 46:1978–1985
Malik S, Wong ND, Franklin SS et al (2004) Impact of the metabolic syndrome on mortality from coronary heart disease, cardiovascular disease, and all causes in United States adults. Circulation 110:1245–1250
Lakka HM, Laaksonen DE, Lakka TA et al (2002) The metabolic syndrome and total and cardiovascular disease mortality in middle-aged men. JAMA 288:2709–2716
McNeill AM, Rosamond WD, Girman CJ et al (2004) Prevalence of coronary heart disease and carotid arterial thickening in patients with the metabolic syndrome (The ARIC Study). Am J Cardiol 94:1249–1254
Grundy SM (2006) Atherogenic dyslipidemia associated with metabolic syndrome and insulin resistance. Clin Cornerstone 8:S21–S27
Mantovani A, Garlanda C, Bottazzi B et al (2006) The long pentraxin PTX3 in vascular pathology. Vascul Pharmacol 45:326–330
Napoleone E, di Santo A, Peri G et al (2004) The long pentraxin PTX3 up-regulates tissue factor in activated monocytes: another link between inflammation and clotting activation. J Leukoc Biol 76:203–209
Napoleone E, Di Santo A, Bastone A et al (2002) Long pentraxin PTX3 upregulates tissue factor expression in human endothelial cells: a novel link between vascular inflammation and clotting activation. Arterioscler Thromb Vasc Biol 22:782–787
Klouche M, Peri G, Knabbe C et al (2004) Modified atherogenic lipoproteins induce expression of pentraxin-3 by human vascular smooth muscle cells. Atherosclerosis 175:221–228
Breviario F, d’Aniello EM, Golay J et al (1992) Interleukin-1-inducible genes in endothelial cells. Cloning of a new gene related to C-reactive protein and serum amyloid P component. J Biol Chem 267:22190–22197
Rolph MS, Zimmer S, Bottazzi B et al (2002) Production of the long pentraxin PTX3 in advanced atherosclerotic plaques. Arterioscler Thromb Vasc Biol 22:e10–e14
Kotooka N, Inoue T, Fujimatsu D et al (2008) Pentraxin 3 is a novel marker for stent-induced inflammation and neointimal thickening. Atherosclerosis 197:368–374
Peri G, Introna M, Corradi D et al (2000) PTX3, a prototypical long pentraxin, is an early indicator of acute myocardial infarction in humans. Circulation 102:636–641
Latini R, Maggioni AP, Peri G et al (2004) Lipid Assessment Trial Italian Network (LATIN) investigators. Prognostic significance of the long pentraxin PTX3 in acute myocardial infarction. Circulation 110:2349–2354
Boehme M, Kaehne F, Kuehne A et al (2007) Pentraxin 3 is elevated in haemodialysis patients and is associated with cardiovascular disease. Nephrol Dial Transplant 22:2224–2229
Malaponte G, Libra M, Bevelacqua Y et al (2007) Inflammatory status in patients with chronic renal failure: the role of PTX3 and pro-inflammatory cytokines. Int J Mol Med 20:471–481
Suzuki S, Takeishi Y, Niizeki T et al (2008) Pentraxin 3, a new marker for vascular inflammation, predicts adverse clinical outcomes in patients with heart failure. Am Heart J 155:75–81
National Institutes of Health Third Report of the National Cholesterol Education (2001) Program expert panel on detection, evaluation, and treatment of high blood cholesterol in adults (Adult Treatment Panel III). Executive summary, Bethesda, National Institutes of Health, National Heart, Lung and Blood Institute (NIH publ. no. 01-3670)
Hampel DJ, Pratschke J, May G et al (2006) Living kidney donation: anemia and inflammation in the early postoperative period. Transplant Proc 38:661–663
Boden WE (2000) High-density lipoprotein cholesterol as an independent risk factor in cardiovascular disease: assessing the data from Framingham to the Veterans Affairs High-Density Lipoprotein Intervention Trial. Am J Cardiol 86:19L–22L
Hong Y, Jin X, Mo J et al (2007) Metabolic syndrome, its preeminent clusters, incident coronary heart disease and all-cause mortality—results of prospective analysis for the atherosclerosis risk in communities study. J Intern Med 262:113–122
Wallenfeldt K, Hulthe J, Fagerberg B (2005) The metabolic syndrome in middle-aged men according to different definitions and related changes in carotid artery intima-media thickness (IMT) during 3 years of follow up. J Intern Med 258:28–37
Alberti A, Gilardini L, Zulian A et al (2008) Expression of long pentraxin PTX3 in human adipose tissue and its relation with cardiovascular risk factors. Atherosclerosis May 15 (Epub ahead of print)
Norata GD, Marchesi P, Pirillo A et al (2008) Long pentraxin 3, a key component of innate immunity, is modulated by high-density lipoproteins in endothelial cells. Arterioscl Thromb Vasc Biol 28:925–931
Dichtl W, Nilsson L, Goncalves I et al (1999) Very low-density lipoprotein activates nuclear factor-kappaB in endothelial cells. Circ Res 84:1085–1094
Ting HJ, Stice JP, Schaff UY et al (2007) Triglyceride-rich lipoproteins prime aortic endothelium for an enhanced inflammatory response to tumor necrosis factor-alpha. Circ Res 100:381–390
Lekakis JP, Papamichael CM, Cimponeriu AT et al (2000) Atherosclerotic changes of extracoronary arteries are associated with the extent of coronary atherosclerosis. Am J Cardiol 85:949–952
Mack WJ, LaBree L, Liu C et al (2000) Correlations between measures of atherosclerosis change using carotid ultrasonography and coronary angiography. Atherosclerosis 150:371–379
Bosutti A, Grassi G, Zanetti M et al (2007) Relation between the plasma levels of LDL-cholesterol and the expression of the early marker of inflammation long pentraxin PTX3 and the stress response gene p66ShcA in pacemaker-implanted patients. Clin Exp Med 7:16–23
Camozzi M, Zacchigna S, Rusnati M et al (2005) Pentraxin 3 inhibits fibroblast growth factor 2-dependent activation of smooth muscle cells in vitro and neointima formation in vivo. Arterioscler Thromb Vasc Biol 25:1837–1842
Acknowledgment
We are grateful to Dr. Annamaria Semolic for excellent technical assistance.
Conflict of interest statement
The authors declare that they have no conflict of interest related to the publication of this manuscript.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Zanetti, M., Bosutti, A., Ferreira, C. et al. Circulating pentraxin 3 levels are higher in metabolic syndrome with subclinical atherosclerosis: evidence for association with atherogenic lipid profile. Clin Exp Med 9, 243–248 (2009). https://doi.org/10.1007/s10238-009-0039-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10238-009-0039-z