Abstract
The aim of the present work is to quantitatively assess the three-dimensional distributions of the displacements experienced during the cardiac cycle by the luminal boundary of abdominal aortic aneurysm (AAA) and to correlate them with the local bulk hemodynamics. Ten patients were acquired by means of time resolved computed tomography, and each patient-specific vascular morphology was reconstructed for all available time frames. The AAA lumen boundary motion was tracked, and the lumen boundary displacements (LBD) computed for each time frame. The intra-aneurysm hemodynamic quantities, specifically wall shear stress (WSS), were evaluated with computational fluid dynamics simulations. Co-localization of LBD and WSS distributions was evaluated by means of Pearson correlation coefficient. A clear anisotropic distribution of LBD was evidenced in both space and time; a combination of AAA lumen boundary inward- and outward-directed motions was assessed. A co-localization between largest outward LBD and high WSS was demonstrated supporting the hypothesis of a mechanistic relationship between anisotropic displacement and hemodynamic forces related to the impingement of the blood on the lumen boundary. The presence of anisotropic displacement of the AAA lumen boundary and their link to hemodynamic forces have been assessed, highlighting a new possible role for hemodynamics in the study of AAA progression.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
1 Introduction
Abdominal aortic aneurysm (AAA) is a degenerative disease of the last segment of the aorta, representing 83 % of all non-cerebral aneurysms diagnosed in the United States (Lawrence et al. 1999; Gillum 1995); untreated AAAs may rupture a severe clinical event associated with high rate of mortality and morbidity.
The pathogenesis of AAA is extremely complex and not completely understood (Dalman et al. 2006; Michel et al. 2011); most likely, aneurysms result from the interaction of multiple factors, systemic, and local, particularly hemodynamic features. In fact, presence of reverse flow, pressure wave propagation, and wall shear stress (WSS) have all been acknowledged to play a leading role in AAA development and clinical outcome (Dalman et al. 2006; Dua and Dalman 2010; Nixon et al. 2010; Hoshina et al. 2003; Boussel et al. 2008).
Since long researchers have struggled in the attempt to identify and elucidate the mechanisms leading to aneurysm initiation, progression, and wall failure (Vorp 2007). Despite many progresses, the majority of criteria proposed for risk stratification and decision making still rely on empirical measurements (Hirose and Takamiya 1998; Fillinger et al. 2003; Speelman et al. 2010; Raghavan et al. 2000; McGloughlin and Doyle 2010), with the maximum AAA diameter (Greenhalgh et al. 2004) still being the prevalent index to evaluate risk of rupture, rather than on the analysis of biomechanical properties (Hua and Mower 2001).
In this quest for elements that may help understanding the pathophysiology of the disease, an interesting phenomenon is the cyclical displacements experienced by the vessel wall during the cardiac cycle due to the blood flow pulsatile action. The presence of unequal circumferential deformation of the aorta has been documented before: Uneven aortic motions were observed at the infrarenal level (Arko et al. 2007), and significant aneurysm neck pulsatility was also reported (Van Herwaarden et al. 2006; Vos et al. 2003). On the other hand, their effects have mostly been considered and investigated in relation to the consequences on endograft motions after its positioning, less as a specific feature of AAA wall behavior throughout the cardiac cycle or in biomechanical analysis. Different concomitant causes could contribute to the occurrence of anisotropic displacements, such as complex AAA shape subjected to hydrostatic pressure change, heterogeneity of mechanical properties of vessel wall, and intraluminal thrombus. Another compelling hypothesis is that anisotropic displacements may be the result of the action of the intra-aortic bulk hemodynamics, that is, the effect of the blood jet coming from the distal abdominal aorta impinging on a limited portion of the lumen surface due to the aorta direction and the AAA sac morphology. Contiguous regions of the lumen surface are then possibly subjected to different mechanical stresses, so that their mechanical response can be dissimilar.
Thanks to advances in both biomedical imaging and computational fluid dynamic (CFD), this issue can be directly addressed. In fact, in vivo AAA displacements can be acquired noninvasively at different instants of the cardiac cycle with dynamic four-dimensional computed tomography (4D-CT), while intra-aortic hemodynamics, namely velocity and WSS distributions, can be computed by means of CFD on the same patient-specific geometry (Formaggia et al. 2009).
The aim of this work is to quantitatively assess the three-dimensional (3D) distributions of the displacements experienced by AAA luminal boundary over the cardiac cycle as reconstructed from 4D-CT acquisitions and put them in relation to the hemodynamic variables obtained by CFD simulations, specifically to WSS maps, being its maximum values commonly employed as a surrogate for the identification of blood impingement region. It is worth mentioning that depending on the complexity of the case at hand, the luminal boundary represents the interface between blood and vessel wall or between blood and intraluminal thrombus (ILT). In both situations, the availability of a mechanistic relationship between anisotropic displacements of this interface and bulk hemodynamics may shed new light on the role of hemodynamics in AAA progression studies and may influence the design of new rupture risk indices in the future, with direct implications on planning for surveillance and surgical intervention.
2 Materials and methods
2.1 Patient recruitment
Ten patients who underwent 4D-CT as preoperative evaluation of an AAA between July 2007 and December 2008 were selected at the Operative Unit of Vascular Surgery of the Ca’ Grande Ospedale Maggiore Policlinico in Milan, Italy. All the patients were initially considered for EVAR due to hostile abdomen, high risks condition, advanced age, or patient choice. Aneurysms were classified as small (\(<\)5 mm), medium (5.0–6.5 mm), or large (\(>\)6.5 mm), according to the recommendations of the Society for Vascular Surgery/International Society for Cardiovascular Surgery reporting subcommittee (Ahn et al. 1997).
Ethical review board approval and informed consent were obtained from all patients. Detailed imaging data, physiological parameters, and outcome data were collected prospectively.
2.2 Image acquisition: scanner and protocol
The acquisitions were performed with a Somatom Definition Dual Source CT (Siemens, Erlanger, Germany), before and after contrast media administration with retrospectively electrocardiographic (ECG) gated spiral acquisition. Non-ionic contrast media (Iomeron, Bracco, Milan, Italy) was used with a concentration of 400 mg/I mg, 1.5 cc pro kg, and an injection speed of 3 cc/s. The temporal resolution was 85 ms, and the total effective dose according to the applied protocol was 34 mSv per acquisition and per patient. Ten ECG gated series of axial images were reconstructed at every 10 % of the R-R interval from the aortic arch to the common femoral arteries, allowing the retrieval of dynamic imaging of the aorta during a complete systolic–diastolic cycle.
2.3 3D model reconstruction
All image processing operations, from 3D reconstruction to post processing, were performed by means of the Vascular Modeling Toolkit, VMTK (Antiga and Steinman 2012). For each dataset and for all the ten time frames, the 3D surface model of the lumen surface of the aorta from the thoracic segment to the first tract of the common iliac arteries was reconstructed using a gradient-driven level set technique: Taking advance of the presence of the contrast agent enhancing the blood in the images, this technique identifies the interface blood vessel wall at the ridges of the image intensity gradient (Antiga et al. 2008). The main side branches (celiac trunk, superior mesenteric artery, right and left renal arteries) were also included in the model. Since one of the goals of the present work is to track the movement of the lumen surface, a reference temporal position was selected among those reconstructed as the 7th time frame, corresponding to the mid-diastolic phase. This selection was justified as the position presumably closer to a resting condition and indeed more appropriate as reference. Ultimately, the ten 3D triangulated surface models describing the location of the lumen boundary throughout the cardiac cycle were obtained.
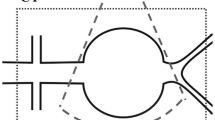
2.4 Vascular geometric characterization
For each reference time frame, a series of operations were performed to automatically identify the portion of the network hosting the AAA, that is, the segment comprised between the origin of the renal arteries and the common iliac bifurcations (Piccinelli et al. 2009) (Fig. 1a, b). Additionally, an automated separation of the lumen surface of the AAA in posterior and anterior sectors was performed by means of the bifurcation reference system (Piccinelli et al. 2009) computed at the iliac bifurcation (Fig. 1c) and tools to robustly parallel transport vectors on centerlines (Piccinelli et al. 2009). The lines robustly delineating the separation between anterior and posterior areas were hence identified on the AAA 3D surface, Fig. 1d. Given the presence of the spine posteriorly, it is acknowledged that AAAs tend to develop differently in these to regions. The rationale behind the separation of the anterior/posterior was indeed to allow a precise characterization of the lumen behavior in the two sub-regions. Moreover, in order to focus on the behavior of the lumen boundary in correspondence of the aneurysm, the most upstream location of the aneurysmatic dilatation was identified by an experienced operator by monitoring wall thickness, presence of thrombus, or aortic diameter enlargement on the source images. Subsequent analyses were applied from this position to the iliac bifurcation.
3D model of AAA and close vasculature. a, b AAA sac (opaque blue) and centerline; two different orientations of the model are shown to highlight the 3D nature of the aneurysmal sac; c definition of the bifurcation plane at the iliac bifurcation; by means of the plane normal (red) the separation of the AAA surface model in an anterior and posterior sectors can be performed; d each point on the AAA surface is associated with a circumferential angle, here plotted, from 0 to 3.14 radians (anterior sector) and from 0 to \(-\)3.14 radians (posterior sector); e flattening procedure of the AAA 3D surface into a rectangular domain; the angular metric is plotted and the line separating in the anterior and posterior sectors indicated
2.5 Lumen boundary motion tracking
To quantitatively evaluate the movement of the AAA lumen surface throughout the cardiac cycle, the displacement of each point of the current 3D surface was computed for each time frame with respect to the 7th time frame, previously identified as the reference. Reference and current surfaces were first rigidly registered by means of the ICP algorithm (Besl and McKay 1992) to disregard purely rigid motion. Successively to account for the non-rigid motion, each point on the current position was supposed to move in the direction of the local surface normal, a reasonable assumption given the small entity of the displacement considered. In practice, for each current point, the closest triangle on the reference surface was identified and the displacement calculated as its Euclidean distance to the triangle. Ultimately, nine maps of displacement, hereafter indicated as lumen boundary displacements (LBD)—displacements of each time frame with respect to the 7th—were available for each patient. Positive (negative) values of displacement indicate an outward (inward) motion of the lumen boundary with respect to the mid-diastolic time frame (Fig. 2).
2.6 Numerical simulations
Once the reference geometry of the specific patient was reconstructed, the surface model was turned into a volumetric mesh of linear tetrahedra (in the range 1.1–2.2 millions of elements) in view of unsteady CFD simulations performed using the finite element code LifeV (LifeV Library 2012). Blood was considered as a Newtonian, homogeneous, and incompressible fluid, so that the Navier-Stokes equations were used for its mathematical description (Formaggia et al. 2009). Blood viscosity was set equal to 0.035 Poise, density equal to 1.0 \((\text{ g/cm}^{3})\) (Formaggia et al. 2009), and time step equal to 0.02 s. Given the small magnitude of the observed displacements and the fact that flow impingement patterns are not expected to critically depend on perturbations of the boundary, rigid walls were adopted. Accordingly to this hypothesis, the ILT was not modeled. Therefore, the effective lumen representing the computational domain could be either the interface between blood and vessel or the interface between blood and ILT. At the inlet, the physiological flow rate \(Q(t)\), depicted in Fig. 3 and chosen as representative of the physiological inflow, was prescribed through a Lagrange multipliers approach (Formaggia et al. 2009; Veneziani and Vergara 2005). For each of the mesenteric and renal branches, we prescribed a flow rate equal to \(Q(t)\)/20 (with the assumption of flat velocity profile), so that 4/5 \(Q(t)\) is the flow rate ultimately entering the AAA. At the two iliac outlets, a zero-stress condition was prescribed, since the region of interest was far from them. The Reynolds number reaches the value of about 8,000 at systole. Transition to turbulence in AAA could occur just after the systole, during the deceleration phase see (Yip and Yu 2001).
Since in this work we analyze the effect of the jet at systole, and in our simulations, no turbulence models were adopted. In order to allow a comparison between displacement maps and hemodynamics features, WSS (used as surrogate of flow impingement) maps were computed at the ten instants over the cycle.
2.7 Relationship between lumen boundary displacements and wall shear stress
To compare vector fields defined on the AAA surface, namely LBD and WSS, computational techniques to patch and flatten 3D surfaces were applied (Antiga and Steinman 2004). First contiguous rectangular regions, here referred to as patches, were automatically defined on the 3D model, and the quantities of interest averaged over each patch. Second the surface was “opened” at the line separating the anterior-posterior sectors (Fig. 1d) and flattened onto a parametric rectangular space (Fig. 1e). The size of each patch was defined through a longitudinal and a circumferential step. The longitudinal step defines the patch “height,” while the circumferential one determines the number of patches into which the vessel circumference is split (in Fig. 1e this circumferential division is shown by means of different shades of color). Flattened maps were obtained for all patients at each time frame, and WSS and LBD were compared over these specific regions. A smoothing operation was also performed on the rectangular maps by means of a Gaussian filter. Both the averaging into rectangular domains and the smoothing procedure were performed in order to remove spurious high frequencies in LBD and WSS while retaining their global features.
Finally, Pearson’s correlation index (Development 2011) between the two rectangular maps, which are defined over the same parametric space, was calculated for each time frame and for each patient to quantify the co-localization of LBD and WSS.
3 Results
3.1 Data of the population
The median age of the population was 72 years. Eight patients were male (80 %) and 2 female (20 %). The median Height was \(173 \pm 9\) cm, body weight \(85.5 \pm 15.41\) kg, body mass index \(27.56 \pm 4.5\). Six patients had a history of smoking (60 %), 6 suffered of hypertension (60 %), 1 was diabetic (10 %), 2 suffered from peripheral arterial disease (20 %), and 2 had a myocardial infarction or aorto-coronary bypass graft surgery (20 %).
Aneurysms were classified as small in 4 cases (40 %) and medium in 6 (60 %). The mean proximal neck diameter was \(23.26 \pm 4.00\) mm (range 18.00–29.67) and length \(4.12 \pm 1.38\) cm (range 2.5–6.63). The mean maximum aortic diameter was \(50.53 \pm 7.57\) mm (range 39.37–64.09), while the mean length of AAA was \(8.46 \pm 3.49\) cm (range 5.1–16.0).
Particular care was also dedicated to assess the presence of ILT along the aneurysmal sac. ILT was not observed in 2 cases (20 %), while it was largely present in 8 (80 %). In Table 1, details about the presence, distribution, and size of the ILT for the analyzed cases are given.
3.2 Relation between lumen boundary displacement and fluid dynamics
For each patient, the 3D surfaces for all time frames were reconstructed, the AAA portion isolated, and the line separating the anterior/posterior sectors identified. The longitudinal length of the AAA segments ranged between 87 and 133 mm. The longitudinal step was set to 4 mm, while the circumferential interval was of \(24^{\circ }\) (14 intervals). The nine LBD and WSS maps were computed, and their flattened versions obtained. The final number of regular patches ranged between 304 and 465.
We observed that for all the analyzed cases, the largest displacements occurred close to the systolic peak (3rd, 4th, and 5th frame), while they globally faded away in the mid and late diastolic phases. Figure 4 depicts the LBD maps of the first patient for all the time frames, while Figs. 5, 6, 7 report only the maps for frames close to the systolic peak for the remaining cases, to represent the instants where the displacements were larger.
Flattened and smoothed maps of LBD (top) and WSS (bottom) for patients 02, 03, 04 at 3rd (systolic peak), 4th and 5th time frames; red (blue) color represents outward (inward) AAA lumen boundary motion with respect to the reference position and high (low) WSS. The reconstructed 3D model is also depicted at the seventh time frame; AAA sac (red surface) and its centerline (red line) are indicated
Flattened and smoothed maps of LBD (top) and WSS (bottom) for patients 05, 06, 07 at 3rd (systolic peak), 4th, and 5th time frames; red (blue) color represents outward (inward) AAA lumen boundary motion with respect to the reference position and high (low) WSS. The reconstructed 3D model is also depicted at the seventh time frame; AAA sac (red surface) and its centerline (red line) are indicated
Flattened and smoothed maps of LBD (top) and WSS (bottom) for patients 08, 09, 10 at 3rd (systolic peak), 4th, and 5th time frames; red (blue) color represents outward (inward) AAA lumen boundary motion with respect to the reference position and high (low) WSS. The reconstructed 3D model is also depicted at the seventh time frame; AAA sac (red surface) and its centerline (red line) are indicated
The qualitative analysis of LBD clearly highlighted the anisotropic distributions of the AAA lumen boundary displacements both in space and time for all the analyzed cases: The portions of the AAA lumen boundary experiencing outward and inward motion were concentrated in different parts of the AAA surface and abruptly separated from each other. The outward motion was preferentially observed in the anterior sectors of the AAA lumen boundary. In Fig. 2, the boundary displacements are depicted for one of the analyzed cases directly on the 3D surface for all the 9 maps, showing the appearance of the largest outward motions (in red) in the anterior sector and around the systolic peak.
Quantitatively, the percentages of AAA surface area moving in the outward or inward direction with respect to the reference time frame were evaluated at all frames. A spike in the percentage of outer directed lumen boundary area was evidenced around the systolic peak with an average value of \(67 \pm 12\) % of the total AAA lumen boundary area (range between 25 and 82 %); it decreased to \(43 \pm 11\) % (range 19–63 %) during the late diastolic phase. The average percentage of AAA boundary lumen boundary moving in the inward direction was assessed at \(35 \pm 15\) % close to the systolic peak (range 18–84 %) and increased during the diastolic phase to \(57 \pm 12\) % (range 36–81 %). Notably, in all the analyzed cases and throughout the first half of the cardiac cycle, the AAA lumen boundary exhibited a somewhat surprising combination of inward and outward motions, where the latter were however prevalent. This trend vanished for most cases in the second part of the cardiac cycle.
The analysis of the displacement values was then separately performed for areas undergoing outward and inward motion. For all the patients, the largest displacements occurred at time frames close to the systolic peak in both inward and outward directions (Table 2). At those instants, the outward motions exceeded the in-plane image spacing (\(0.48\times 0.48\) mm) in all the cases except one (patient 10), while the inward motions remained in four cases out of ten below the image resolution even at systolic peak. For patient 10, the motion actually remained always below the in-plane image spacing. In absolute terms, the outward displacement exceeded the inward one for all the analyzed cases except one (patient 6). When the 3rd, 4th and 5th frames were considered, the maximum outward LBD ranged between 0.55 and 1.40 mm (mean \(0.75 \pm 0.29\) mm), and the maximum inward LBD ranged between 0.35 and 1.87 mm (mean \(0.59 \pm 0.35\) mm). In all cases, both inward and outward displacement values at the systolic peak decidedly decreased during the mid and late diastolic phases, usually below the image resolution.
No particular trends or relations were assessed between the presence of ILT and the percentages of lumen boundary area moving inward/outward or the LBD values (Tables 1, 2). In particular, similar values of inward/outward displacements were found for rather heterogeneous situations of ILT burden and distribution along the aneurysm sac, as for case 1 and case 3 (no ILT versus concentric ILT), or case 2 and 8 (concentric versus eccentric ILT).
WSS (Figs. 4, 5, 6, 7) exhibited distribution patterns similar to LBD: During the systolic phase areas of intense stresses alternated over the AAA lumen boundary with zones of rather mild friction, though we observed a strong dependence on the specific shape of the AAA sac at hand.
The comparison of LBD and WSS allows a qualitative assessment of the correlation, in time and space, between the two distributions, directly linking the AAA lumen boundary motion to the hemodynamic forces. The co-localization of outward motion and high WSS was clear at the systolic peak in half of the analyzed cases, particularly cases 1, 3, 4, 5, 9. For the other cases, this relation was less clear, even though both the maximum LBD and WSS still occurred at the systolic phase.
A quantitative analysis of the co-localization of LBD and WSS was performed computing the Pearson’s correlation index between the maps values. Table 3 reports the index for each case at each frame. A relative increase in the correlation index is visible close to the systolic peak for all the cases except patient 6 (Fig. 6). The increase is particularly evident for cases 1, 3, 4, 5, 8, 9, while it is less abrupt for patients 2, 7, 10. Ultimately, in 4 cases, there is at least one time frame with correlation index \(>\)0.73.
Once again, since the lumen boundary represents the interface between blood and the underlying structure, the presence of ILT and its distribution along the aneurysmal sac were qualitatively evaluated for associations with the correlation results just reported. No relation was found linking the presence or thickness of ILT with WSS and LBD co-localization for the analyzed cases. High Pearson indexes were found close to the systolic peak for cases without ILT (patient 1), thick concentric ILT (patient 3), or thick eccentric ILT (patient 8), suggesting that the presence of ILT has no obvious influence on LBD anisotropy.
For a better representation of the flow patterns inside the AAA, the velocity fields are shown in Fig. 8 at the systolic peak for each case, together with the WSS map at the impingement area. These 3D representations can provide a more comprehensive picture of the complexity of flow features: The direction of the blood jet coming from the aorta—and consequently influenced by its geometry—, its impact on the lumen boundary, and their relation to LBD. For some of the cases with a relatively high correlation coefficient, these figures further evidence the correspondence between the zone impacted by the blood and the outward LBD (cases 1, 3, 4, 8, 9). Coherently, in case 6, which exhibited a low correlation coefficient, the blood jet was aligned along the axial direction of the vessel, and no pattern was detectable in the LBD map. Figure 8 also highlighted the strong influence of the aorta geometry in determining the direction of impact.
4 Discussion
The mechanisms that lead to AAA development, progression, and rupture are still unclear and most probably implicate a number of factors from family history, vascular wall biology and hemodynamic features (Dalman et al. 2006; Dua and Dalman 2010). Several indices have been proposed for the classification of aneurysms depending on their likelihood to rupture, although a comprehensive account for the phenomena occurring at the vascular wall and for the specificity of the patient is still out of reach (Vorp 2007; Hirose and Takamiya 1998; Fillinger et al. 2003; Speelman et al. 2010; Raghavan et al. 2000; McGloughlin and Doyle 2010; Hua and Mower 2001).
The focus of this work was the assessment and quantification of anisotropic displacements experienced by AAA lumen boundary throughout the cardiac cycle. 4D-CT acquisitions have been employed to evaluate aneurysmal lumen boundary motion, while specific hemodynamic features have been investigated as a potential explanation for such displacements by means of CFD simulations in the specific patient anatomy.
The importance of wall motion due to the pulsatile nature of the blood flow has been considered in some recent work (Arko et al. 2007; Van Herwaarden et al. 2006; Vos et al. 2003), and, consistently, emphasis has been placed on the necessity of performing dynamic imaging of AAA instead of traditional static acquisition in order to account for these phenomena (Laskowski et al. 2007) and to plan better treatments (Iezzi et al. 2011). In these works (Arko et al. 2007, 2006; Vos et al. 2003), the authors measured anisotropic wall motions at several locations along the infrarenal segment, mostly on 2D images, and relate their results to the role of wall pulsatility with respect to endografts positioning and possibly migration after implant. Instead, in the present study, we focused on obtaining a complete 3D description of the displacements of the AAA lumen boundary and its parent vasculature by means of 4D-CT imaging in order to provide some insights on the wall behavior throughout the cardiac cycle. To the authors’ knowledge, this is the first attempt to use this methodology to study the complete 3D lumen boundary displacement quantitatively and in vivo.
By means of this technique, we assessed the presence of anisotropic displacements of the AAA lumen boundary. In all the analyzed cases but one, and specifically at the systolic peak considerable portions of the lumen boundary, usually in the anterior sector, were found to move outward with respect to the reference position (mid-diastole), while others to move inward. Such strong anisotropy in the lumen boundary displacement progressively vanished in the remaining instants of the cycle. The presence of strongly heterogeneous LBD in space (anterior versus posterior sectors) and time (systolic versus diastolic phase) may potentially affect the biomechanics of AAA, in terms of distribution and magnitude of strains and stresses, influence biological processes such as wall remodeling, and ultimately determine the evolution of AAA toward rupture.
The concurrent presence of outward and inward displacements at systole is an interesting observation by itself. In the classical view, vascular structures are supposed to expand and relax concentrically, respectively at systole and diastole, due to the effect of hydrostatic pressure. Our results demonstrated that this is not necessarily the case, and that AAA displacement is probably caused, or at least contributed by hemodynamic forces related to the impingement of the blood on the lumen boundary. Indeed, hydrostatic pressure alone, even in combination with complex geometry, would hardly be sufficient to explain this phenomenon: During systole, the impingement of the jet on the AAA lumen boundary determines outward motion of the impacted area, while other regions not subjected to such force “accommodated” the resulting displacement with opposite inward motion. During diastole, the less energetic flow reorganizes within the AAA volume, no specific trend or correlation is noticeable, and the displacement magnitude significantly decreases.
The co-localization between large LBD and high WSS was not equally evident in all the cases. This is not surprising, since a high correlation is expected only for those cases where flow impingement occurs on the sac due to the specific morphology of the abdominal aorta, while it is expected to be absent when the blood flow is aligned with the vessel wall and the impingement occurs directly at the iliac bifurcation. This is strongly patient dependent, since it is the proximal aorta geometry and the sac morphology that eventually determine the presence of an impingement region and, according to our hypothesis, of an AAA lumen boundary anisotropic motion (Fig. 8). This makes the assessment of anisotropic boundary displacements and of high viscous forces on the sac a potentially informative tool to evaluate the status of a specific AAA, and, at the same time, it makes the specific morphology of the abdominal aorta a potential predictor of the actual biomechanical environment.
The presence in the majority of the analyzed cases of an intraluminal thrombus, whose cellular composition, biomechanical properties, and role in the progression of the disease are still under investigation, was taken into consideration in analyzing the motion of the interface between blood and its underlying structure (the vessel wall or the ILT, accordingly to the case considered) in order to establish potential ILT effects on the phenomenon we describe. No specific trend was found throughout the analyzed situations that could indicate a specific pattern of response of the lumen displacements to hemodynamic stresses due to ILT burden or distribution. While acknowledging ILT importance for a proper description of the mechanical environment, the goal of the present study was in fact to verify the impact of the bulk flow on the lumen boundary, that is, on the interface in direct contact with the blood.
The present study was not aimed at determining a cause–effect relationship between displacements and rupture, but at documenting the existence of cyclic anisotropic displacements and at suggesting a direct physical explanation for their occurrence. Future investigations are in order to determine the extent of their effects in terms of strain and stresses inside the vessel wall or the complex structure ILT-vessel wall.
Some limitations of this study should be mentioned. One possible obstacle to the application of these techniques is the high image resolution needed to appreciate the 4D lumen displacement. Depending on the cases at hand, some motions may still fall under the in-plane image spacing, which makes their computation less reliable. In the cases reported in the present study, the largest displacements were well above voxel size, while in some regions, they were comparable or lower than voxel size. However, by identifying the location of gradient magnitude ridges using sub-voxel interpolation, the segmentation technique employed in this work is capable of recovering the presence of sub-voxel displacements, which is confirmed by the identification of consistent displacements in contiguous regions of the surface.
For the CFD simulations, a rigid wall hypothesis was adopted, instead of performing a fluid-structure interaction analysis. This choice was made since we were interested in localizing the regions of the sac surface where the WSS was higher, not in determining its precise value. For this reason, we believe that the rigid wall assumption is acceptable for our aims, and it simplifies the analysis remarkably. Moreover, it is still argument for debate whether a turbulence model should be employed in simulating the intra-aneurysmal hemodynamics. The remarkable agreement between measured LBD and simulated WSS seems to suggest that no explicit treatment of turbulence is needed to reproduce the location of flow impingement in the abdominal aorta.
5 Conclusions
The assessment of AAA sac cyclical displacements and their anisotropy may represent a promising direction for patient risk stratification and prediction of AAA evolution. As new means of investigation such as 4D-CT and patient-specific CFD become widely available, these evaluations may play a role in research and clinical environments for patient management, pre-surgical evaluation, and follow-up planning.
References
Ahn SS, Rutherford RB, Johnston KW, May J, Veith FJ, Baker JD, Ernst CB, Moore WS (1997) Reporting standards for infrarenal endovascular abdominal aortic aneurysm repair. Ad Hoc Committee for Standardized Reporting Practises in Vascular Surgery of the Society of The Vascular Surgery/International Society for Cardiovascular Surgery. J Vasc Surg 25:405–410
Antiga L, Steinman DA (2004) Robust and objective decomposition and mapping of bifurcating vessels. IEEE Trans Med Imaging 23:704–713
Antiga L, Steinman DA (2012) The vascular modeling toolkit. Available at http://www.vmtk.org. Accessed August
Antiga L, Piccinelli M, Botti L, Ene-Iordache B, Remuzzi A, Steinman DA (2008) An image-based modeling framework for patient-specific hemodynamics. Med Biol Eng Comput 46:1097–1112
Arko FR, Murphy EH, Davis CM III, Johnson ED, Smith ST, Zarins CK (2007) Dynamic geometry and wall thickness of the aortic neck of abdominal aortic aneurysms with intravascular ultrasonography. J Vasc Surg 46:891–897
Besl PJ, McKay ND (1992) A method for registration of 3D shapes. IEEE Trans Pattern Anal Mach Intell 14:239–256
Boussel L, Rayz V, McCulloch C, Martin A, Acevedo-Bolton G, Lawton M et al (2008) Aneurysm growth occurs at region of low Wall Shear Stress. Patient-specific correlation of hemodynamics and growth in a longitudinal study. Stroke 39:2997–3002
Dalman RL, Tedesco MM, Myers J, Taylor CA (2006) Mechanisms, stratification and treatment. Ann NY Acad Sci 1085:92–109
Dua MM, Dalman RL (2010) Hemodynamics influences on abdominal aortic aneurysm disease: application of biomechanics to aneurysm pathophysiology. Vasc Pharmacol 53(1–2):11–21
Fillinger MF, Marra SP, Raghavan ML, Kennedy FE (2003) Prediction of rupture risk in abdominal aortic aneurysm during observation: wall stress versus diameter. J Vasc Surg 37:724–732
Formaggia L, Quarteroni A, Veneziani A (2009) Cardiovascular mathematics—modeling and simulation of the circulatory system. Springer, Berlin
Gillum RF (1995) Epidemiology of aortic aneurysm in the United States. J Clin Epidemiol 48:1289–1298
Greenhalgh R, Brown LC, Kwong GP, Powell JT, Thompson SG (2004) Comparison of endovascular aneurysm repair with open repair in patients with abdominal aortic aneurysm (EVAR trial 1), 30-day operative mortality results: randomised controlled trial. Lancet 364(9437):843–848
Hirose y, Takamiya M (1998) Growth curve of ruptured aortic aneurysm. J Cardiovasc Surg 39:9–13
Hoshina K, Sho E, Sho M, Nakahashi TK, Dalman RL (2003) Wall shear stress and strain modulate experimental aneurysm cellularity. J Vasc Surg 37:1067–1074
Hua J, Mower WR (2001) Simple geometric characteristics fail to reliably predict abdominal aortic aneurysm wall stresses. J Vasc Surg 34:308–315
Iezzi R, Di Stasi C, Dattesi R, Pirro F, Nestola M, Cina A, Codispoti FA, Snider F, Bonomo L (2011) Proximal aneurysmal neck: dynamic ECG-gated CT angiography—conformational pulsatile changes with possible consequences for endograft sizing. Radiology 260:591–598
Laskowski I, Verhagen HJM, Gagne PJ, Moll FL, Muhs BE (2007) Current state of dynamic imaging in endovascular aortic aneurysm repair. J Endovasc Therapy 14:807–812
Lawrence PF, Gazak C, Bhirangi L, Jones B, Bhirangi K, Oderich G, Treiman G (1999) The epidemiology of surgically repaired aneurysms in the United States. J Vasc Surg 30:632–640
LIFEV software. Available at http://www.lifev.org. Accessed Aug 2012
McGloughlin TM, Doyle BJ (2010) New approaches to abdominal aortic aneurysm rupture risk assessment. Engineering insights with clinical gain. Arterioscler Thromb Vasc Biol 30:1687–1694
Michel JB, Martin-Ventura JL, Egido J, Sakalihasan N, Treska V, Lindholt J, Allaire E, Thorsteinsdottir U, Cockerill G, Swedenborg J, FAD EU consortium (2011) Novel aspects of the pathogenesis of aneurysms of the abdominal aorta in humans. Cardiovasc Res 90(1):18–27
Nixon AM, Gunel M, Sumpio BE (2010) The critical role of hemodynamics in the development of cerebral vascular disease. J Neurosurg 112(6):1240–1253
Piccinelli M, Veneziani A, Steinman DA, Remuzzi A, Antiga L (2009) A framework for geometric analysis of vascular structures: applications to cerebral aneurysms. IEEE Trans Med Imaging 28:1141–1155
R Development Core Team (2011) R: a language and environment for statistical computing. Vienna, Austria. http://www.R-project.org. Accessed December
Raghavan ML, Vorp DA, Federle MP, Makaroun MS, Webster MW (2000) Wall stress distribution on three-dimensionally reconstructed models of human abdominal aortic aneurysm. J Vasc Surg 31(7):760–769
Speelman L, Schurink GWH, Bosboom EMH, Buth J, Breeuwer M, van de Vosse FN, Jocobs MH (2010) The mechanical role of thrombus on the growth rate of an abdominal aortic aneurysm. J Vasc Surg 51:19–26
Van Herwaarden JA, Bartels LW, Muhs BE, Vincken KL, Lindeboom MY, Teutelink A, Moll FL, Verhagen HJ (2006) Dynamic magnetic resonance angiography of the aneurysm neck: conformational changes during the cardiac cycle with possibile consequences for endograft and future design. J Vasc Surg 44:22–28
Veneziani A, Vergara C (2005) Flow rate defective boundary conditions in haemodynamics simulations. Int J Numer Method Fluids 47:803–816
Vorp DA (2007) Biomechanics of abdominal aortic aneurysm. J Biomech 40(9):1887–1902
Vos AWF, Wisselink W, Marcus JT, Vahl AC, Manoliu RA, Rauwerda JA (2003) Cine MRI assessment of aortic aneurysm dynamics before and after endovascular repair. J endovasc Therapy 10:433–439
Yip TH, Yu SCM (2001) Cyclic transition to turbolence in rigid abdominal aneurysm models. Fluid Dyn Res 29(81):113
Acknowledgments
The authors would like to thank Barbara Barberis and Alessandro Duci. This study has been performed with a partial funding of the Fondazione Cà Granda Ospedale Policlinico, Milan, Italy. C. Vergara has been partially supported by the ERC Advanced Grant N.227058 MATHCARD.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Piccinelli, M., Vergara, C., Antiga, L. et al. Impact of hemodynamics on lumen boundary displacements in abdominal aortic aneurysms by means of dynamic computed tomography and computational fluid dynamics. Biomech Model Mechanobiol 12, 1263–1276 (2013). https://doi.org/10.1007/s10237-013-0480-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10237-013-0480-5