Abstract
Transcranial magnetic stimulation (TMS) is a relatively non-invasive technique to interfere with the function of small cortical areas through currents induced by alternating magnetic fields emanating from a handheld coil placed directly above the targeted area. This technique has clear effects on a whole range of measures of brain function and has become an important research tool in neuropsychiatry. More recently, TMS has been studied in psychiatry mainly to assess its putative therapeutic effects in the treatment of refractory major depression. Most studies indicate that both low-frequency TMS and higher (20 Hz) frequency repetitive TMS may have some antidepressant properties. This is most interesting and opens a whole new avenue of low invasive techniques to stimulate the brain in major depression. However, definite therapeutic effects of clinical significance still remain to be demonstrated.
Zusammenfassung
Die transkranielle Magnetstimulation (TMS) ist eine wenig invasive Technik zur Beeinflussung der Funktion kleiner kortikaler Gebiete durch von alternierenden Magnetfeldern induzierte Ströme. Diese Magnetfelder werden mit Hilfe einer handgeführten Spule erzeugt, die unmittelbar über dem gewünschten Zielbereich positioniert wird. Diese Methode hat deutliche Auswirkungen auf ein ganzes Spektrum von Hirnfunktioen und ist stellt ein wichtiges Forschungsinstrument der Neuropsychiatrie dar. In jüngerer Zeit studiert man TMS in der Psychiatrie hauptsächlich, um ihre vermuteten Therapieeffekte in der Behandlung refraktärer majorer Depressionen zu klären. Die meisten Studien deuten darauf hin, dass sowohl niederfrequente TMS (1Hz) und höherfrequente (20 Hz) repetitive TMS (rTMS) antidepressive Eigenschaften zeigen. Dies ist höchst interessant und eröffnet eine vollkommen neue Perspektive für wenig invasive Techniken zur Stimulation des Gehirns in Fällen von majorer Depression. Überzeugende Effekte von klinischer Signifikanz gilt es jedoch noch nachzuweisen.
Resumé
La stimulation magnétique transcraniale (SMT) est une technique relativement non invasive visant à influer sur le fonctionnement de petites zones corticales au moyen de courants induits par des champs magnétiques alternatifs, provenant d’une bobine magnétique tenue à la main directement au-dessus de la zone visée. Cette technique a des effets manifestes sur toute une gamme de mesures des fonctions du cerveau et est devenue un important outil de recherche en neuropsychiatrie. Depuis quelques temps, la TMS est étudiée sur ses effets thérapeutiques supposés dans le traitement des dépressions majeures réfractaires. La plupart des études montrent que tant la TMS à basse fréquence que la TMS répétitive à fréquence plus élevée (20 Hz) (rTMS) pourraient avoir des propriétés antidépressives. Ceci est extrêmement intéressant et ouvre des perspectives entièrement nouvelles aux techniques faiblement invasives pour stimuler le cerveau dans les cas de dépressions majeures. Cependant, des effets thérapeutiques concrets avec pertinence clinique restent encore à démontrer.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
1 Transcranial magnetic stimulation—principle of action
Transcranial magnetic stimulation (TMS) refers to an in vivo technique of delivering magnetic pulses to the cortex using a handheld stimulating coil, which is applied directly to the head. The equipment necessary to deliver TMS consists of two parts: a stimulator, which generates brief pulses of strong electrical currents whose frequency and intensity can be varied and a stimulation coil connected to the stimulator. The magnetic field generated at the coil passes unimpeded through scalp and skull and induces an electrical current in the underlying tissue, which in turn depolarizes neurons. The main advantage of this method of stimulation is its non-invasiveness and the possibility to stimulate very small brain volumes. With recent technology, single-, paired or repetitive magnetic pulses can be generated and delivered. Cortical excitability may be increased or decreased depending on stimulation frequency (Hallett 2000), and TMS has been shown to modify regional cerebral blood flow (Bohning et al. 2000; Catafau et al. 2001).
Barker first demonstrated the induction of muscle potentials by magnetic stimulation of the central nervous system in 1985 (Barker et al. 1985). He induced muscle twitching with a coil of 10 cm diameter placed on the scalp over the motor cortex. A brief pulse of 110 μs with a peak current of 4,000 A was applied and pulses at a maximal rate of 0.33 Hz were delivered.
With the possibility of stimulating the motor cortex non-invasively, TMS replaced high-voltage transcutaneous electrical stimulation previously used in clinical studies to measure variables such as central motor conduction time. Altered conduction time can be associated with a variety of neurological disorders such as multiple sclerosis, amyotrophic lateral sclerosis, cervical myelopathy and degenerative ataxic disorders. TMS has great potential in the intraoperative monitoring of the integrity of motor tracts during surgery of the brain and spinal tract (Murray 1991). TMS has found widespread diagnostic use in neurology for demyelinating disorders involving the excitability and the connections of the motor cortex with other parts of the nervous system involved in motor function (Ziemann and Hallett 2000).
2 Transcranial magnetic stimulation—history
With the observation of Faraday in 1831, that a time-varying magnetic field can induce a current in a nearby conductor, the theoretical basis of inducing depolarizing currents by electromagnetic coils was established. The French scientist d’Arsonval reported on the first human application of TMS already in 1896. He was able to induce phosphenes (flickering-light sensation, not elicited by visual perception), vertigo and syncope in subjects whose head was placed in a large electromagnetic coil (Geddes 1991). In 1959, Kolin demonstrated for the first time that an alternating magnetic field is able to stimulate a sciatic frog nerve and could induce contractions of the gastrocnemic muscle (Geddes 1991). In 1965, Bickford was able to induce muscle twitching in humans by applying a pulsed magnetic field with a maximum field-strength of 20,000–30,000 G to ulnar, peroneal and sciatic nerves (Geddes 1991). The induction of muscle potentials by magnetic stimulation of the central nervous system was first demonstrated by Barker in 1985 (Barker et al. 1985). He induced muscle twitching with a coil of 10 cm diameter placed on the scalp over the motor cortex. A brief pulse of 110 μs with a peak current of 4,000 A was applied and pulses at a maximal rate of 0.33 Hz were delivered.
With the possibility of stimulating the motor cortex non-invasively (Fig. 1), TMS replaced high-voltage transcutaneous electrical stimulation used in clinical studies mainly to measure central motor conduction time. This variable may be altered by a variety of neurological disorders such as multiple sclerosis, amyotrophic lateral sclerosis, cervical myelopathy and degenerative ataxic disorders. It seems that TMS has great potential in the intraoperative monitoring of the integrity of motor tracts during surgery of the brain and spinal tract (Murray 1991). TMS has subsequently found diagnostic use in neurology for disorders such as demyelinating diseases involving the excitability and the connections of the motor cortex with other parts of the nervous system involved in motor pathways (Ziemann and Hallett 2000).
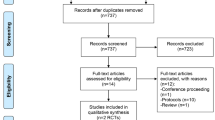
Application of repetitive transcranial magnetic stimulation. This is a usual setting for non-convulsive rTMS studies. Patients are awake, sitting relaxed in a chair while stimulation (here to the left dorsolateral prefrontal cortex) is applied. A typical stimulator, here with four booster modules affording high-frequency stimulation is used. Note the oxygen tank nearby, which would be used as most important therapy in the event of the development of a seizure
In 1987 Bickford extended the field of TMS research into neuropsychiatry: he was the first to describe transient mood elevation in several normal volunteers receiving single pulse stimulations to the motor cortex (Bickford et al. 1987). This was the starting point of the scientific investigation of effects of depolarizing magnetic fields in a variety of neuropsychiatric disorders. Soon after, open studies of the effects of TMS on patients with major depression were conducted using single pulse stimulations at frequencies less than 0.3 Hz (Höflich et al. 1993; Grisaru et al. 1994; Kolbinger et al. 1995). In these studies relatively large areas under the vertex were stimulated bilaterally and involved only very few subjects. More recent work has suggested that both slow and fast repetitive transcranial magnetic stimulation (rTMS) may have some value in depression.
3 Effects at cellular and systemic levels
Immediate early gene expression is an useful marker for activation and has been successfully used widely in psychopharmacology. Using this technique, Ji et al. reported that one single train of rTMS applied to rats in vivo induced c-fos and c-jun expression in different areas of the brain including key regions controlling circadian biological rhythms, such as the retina, the paraventricular nucleus of the thalamus, the suprachiasmatic nucleus and the pineal gland (Ji et al. 1998). The same stimulation parameters have earlier been shown to be efficacious in an animal model of depression (Fleischmann et al. 1995). These findings might point to a possible antidepressant mode of action of TMS effects via circadian rhythms. The finding that immediate-early gene expression is influenced by TMS has been replicated and further examined both in vivo and in vitro (Doi et al. 2001; Hausmann et al. 2001).
Keck measured modulatory effects of frontal rTMS in rat brain in vivo using intracerebral microdialysis (Keck et al. 2000). There was a continuous reduction in arginine vasopressin release of up to 50% within the hypothalamic paraventricular nucleus. In contrast, the release of taurine, aspartate and serine was selectively stimulated within this nucleus. Furthermore, in the dorsal hippocampus the extracellular concentration of dopamine was elevated in response to rTMS. The same group assessed effects of rTMS at 20 Hz in rats on the hippocampal, accumbal and striatal release patterns of dopamine and its metabolites using intracerebral microdialysis. They demonstrated that rTMS of frontal brain regions has a modulatory effect on both mesolimbic and mesostriatal dopaminergic systems which might contribute to the beneficial effects of rTMS in the treatment of affective disorders (Keck et al. 2002). By using positron emission tomography (PET) scanning, a reduction in 11C raclopride binding to dopamine receptors in the left dorsal caudate nucleus was observed in eight volunteers after left dorsolateral prefrontal cortex rTMS. This implies that rTMS can trigger dopamine release in these brain structures (Strafellea et al. 2001).
Several studies documented the effect of rTMS on plasma levels of a variety of hormones including cortisol, prolactin and TSH. Results from these studies are inconclusive but indicate that TMS might significantly affect neuroendocrine function (George et al. 1996; Cohrs et al. 1998; Szuba et al. 2001). TMS can transiently disrupt or induce activity in focal brain regions, depending on the region stimulated. Applied to the visual cortex, for example, strong TMS can produce phosphenes and stimuli of lower intensity induce transient scotomas (Hallett 2000). Moreover, other functions, such as linguistic processing, can be investigated with rTMS (Flitman et al. 1998). A neuromodulatory effect of subthreshold high-frequency rTMS has been observed in ten subjects. After 1,250 stimulations at 90% motor threshold, an intracortical inhibition could be measured which persisted or at least 10 min after the rTMS stimulation (Peinemann et al. 2000).
The combination of non-invasive stimulation of the brain coupled with functional neuroimaging techniques offers novel opportunities to investigate human brain function. It also allows visualization of the effects of TMS including those distant from the site of stimulation (Bohning et al. 1997, 2000; Paus et al. 1997). For example, ten medication-free subjects suffering form major depression (eight unipolar, two bipolar) received in a crossover, randomized study of rTMS at the left prefrontal cortex (LPFC), at 100% motor threshold, at either 20 or 1 Hz. After 20 Hz, an increase in rCBF in the prefrontal cortex left > right, cingulated gyrus left >> right, left amygdala, bilaterally insula, basal ganglia, hippocampus, parahippocampus, thalamus, cerebellum was observed; after 1Hz only decreases in rCBF in right prefrontal cortex, left medial cortex, left basal ganglia and left amygdala were noted. Individuals whose depressive symptoms improved with one frequency worsened with the other (Speer et al. 2000).
The multidisciplinary results mentioned above suggest that TMS has prominent and reproducible effects on the brain. This puts TMS apart from other putative approaches to treat neuropsychiatric disorders (Hallett 2000). One problem shared with antidepressants is that the link between changes at cellular levels and complex behavioral changes—such as the ones observed in depression—has been very difficult to establish. The field of neuropsychiatric research in TMS has somewhat suffered from a ‘top down’ approach in which early promising results in depression have led to an enthusiasm for clinical studies without sufficient basic data on neurobiology. Approaches integrating findings from all levels of brain systems—molecular to behavioral—are extremely important and should be undertaken in order to support ongoing clinical research.
The magnetic field induced by TMS interacts with an extremely complex biological system where essential interactions between the brain and mind take place (Kandel 1998, 1999). It is obvious that the impact of these fields on brain systems is difficult to evaluate, because monitoring functions of the living human brain is only possible by assessing summation responses which are determined by the action of ten of thousands or more cells. The current models of psychiatric disorders are integrating so-called functional systems at molecular-, cellular-, neurotransmitter-, organ- systemic- or individual- and social levels that are not very well understood. Presenting the mechanisms of action of TMS both as a research or treatment tool challenges old hypotheses of brain function and, hopefully, allows the creation of new ones. Several acute and chronic alterations at different levels, ranging from changes in gene expression of cells in the central nervous system to alterations in mood and behavior have been documented during and after the application of TMS.
4 Side effects
Compared to other methods of brain stimulation rTMS can be considered as relatively safe since it is non-invasive (Belmaker et al. 2003). Of major concern are involuntarily induced seizure, local pain during application, changes in the auditory performance due to the noise generated in the coil by the passing electrical current and headache as well as the concern of alterations of cognitive functions. Until now, in research applications, mainly short-term problems (application of TMS, follow-up of a few weeks) were addressed. Also long-term concerns have to be addressed. These might include long lasting cognitive impairment which are the most frequent unwanted long-term side effect of electroconvulsive therapy (ECT), sleep problems or potentially problems linked to effects of the influence of the strong magnetic fields on the brain.
4.1 Immediate and short-term risks
4.1.1 Seizures
The risk of causing a seizure is the primary safety concern with TMS. Even if this risk is primarily associated with rTMS, also single pulse stimulation has been reported to produce seizures in patients with large cerebral infarcts, contusions or other structural brain lesions. According to Wassermann, in patients with completely subcortical lesions, no seizures are reported (Wassermann 2000). According to the same author, there are a few articles reporting the induction of seizures in epilepsy patients without gross lesions. In at least six normal volunteers, and at least two patients with depression, inadvertent seizure occurred during rTMS stimulation (Wassermann 2000). None of the subjects who experienced rTMS-induced seizures suffered lasting sequelae. EEG recordings became normal after at least 2 days. Recorded effects were mild recall deficits, which returned to normal after 24 h in two individuals, and significant anxiety in one subject concerning the possibility of a recurrent seizure. Until today, several thousand individuals have been subjected to rTMS treatments. It seems reasonable to assume that under observation of the safety guidelines as discussed below a development of seizure activity is extremely unlikely.
4.1.2 Cognitive impairment
Mainly short-term observations concerning cognitive function after TMS administration are available. rTMS can produce transient disruption of various cerebral functions, depending on the site of stimulation. Observations reported include a significant decrease in a memory subtest within an hour after stimulation with 150 trains of rTMS at 15 Hz and 120% motor threshold delivered at four different positions (Flitman et al. 1998). Commenting this results, Lorberbaum and Wassermann (2000) concludes that these cognitive effects were due to subconvulsive epileptic activity or that the threshold for adverse effects on memory might be near that of seizure. Loo reported results from a study where 12 subjects suffering from major depression received rTMS during 4 weeks. No significant changes in neuropsychological functioning after 4 weeks were observed (Loo et al. 2001). Shajahan et al. (2002) showed in 15 patients suffering from major depression which received left dorso-lateral rTMS that cortical excitability and functional connectivity could be influenced, but no deterioration in neuropsychological function was observed. Another group was even able to demonstrate that patients receiving rTMS improved significantly in the Trail Making Test-B, a test of cognitive flexibility and conceptual tracking (Moser et al. 2002).
4.1.3 Cardiovascular effects
No significant changes in blood pressure and heart rate have been reported during and after the administration of rTMS (Foerster et al. 1997).
4.1.4 Auditory function
No significant changes in auditory threshold were observed in a study involving 12 depressed subjects undergoing rTMS during 4 weeks when assessed for 4 weeks after the end of the study (Loo et al. 2001).
4.1.5 Headache
The application of TMS may cause local pain resulting from direct stimulation of muscles underlying the coil and from stimulation of facial and scalp nerves. It is generally more painful at higher intensities and frequencies. About 5–20% of subjects experience tension headache after rTMS sessions (George et al. 1999).
4.2 Potential long-term effects
There is of course legitimate concern, whether the application of rTMS might cause brain damage in the widest sense. Mechanisms discussed are heating of neuronal tissue, exocitotoxicity and any influences of magnetic fields. As with other side effects, besides the occurrence of seizure, there are very few data and no thorough investigations available, which would address these questions. There are, however, after the administration of TMS and rTMS to many thousand subjects, no indications that their application might cause brain damage.
The kind of low-frequency, high-strength magnetic fields delivered to the human brain during rTMS are not known from other applications. Considerable evidence has accumulated about constant, strong static magnetic fields with the introduction of MRI techniques in medicine. These fields have about the same strength as the ones produced by rTMS. Since the introduction of MRI, more than 150,000,000 examinations have been performed and only seven deaths occurred due to these procedures (Schenck 2000). One involved a ferromagnetic cerebral aneurysm clip and five examinations of patients with cardiac pacemakers. High-frequency (about 1,000 MHz) electromagnetic fields as generated by cell phones rose concern in the public about adverse health effects. They are known to induce changes in sleep EEG patterns 20–50 min after electromagnetic fields were applied to awake subjects (Huber et al. 2000). In rTMS, very different energies and frequencies of electromagnetic fields are applied to the human brain. In a safety study, rTMS at therapeutic parameters has been demonstrated to have no significant effects on sleep EEG (Graf et al. 2001).
5 Effects on mood of healthy volunteers
It is of obvious importance to elucidate the exact structural and functional bases of affect to understand the neurobiology of, and putative therapeutic interventions for, human disorders like depression and mania. Converging evidence from different areas of research support the hypothesis that mood is regulated by a interconnected network of brain regions encompassing prefrontal, cingulate, parietal and temporal cortical regions an well as parts of the striatum, thalamus and hypothalamus. Among them, the limbic system integrates external stimuli with internal drives and is part of a distributed neural network that marks stimuli and events with positive or negative value (Aggleton 1993). Lesions of this network from tumor, infarction or transient disruption often result in mood changes. In addition, alterations of cerebral blood flow and metabolism in the dorsolateral, ventrolateral, orbitofrontal and medial frontal regions, as well as the subgenual prefrontal and anterior cingulate cortex have been demonstrated in patients suffering from major depression (Mayberg 1997; Soares and Mann 1997). The prefrontal cortex has been implicated with mood generation and modulation, though this view is not universal (George et al. 1995a, b; Lane et al. 1997; Paradiso et al. 1997).
Repetitive transcranial magnetic stimulation has been used in healthy subjects to help elucidate the basic neurophysiology of mood generation and modulation by stimulating the dorsolateral prefrontal cortex (DLPFC). Six studies have been published in which the effect of prefrontal rTMS on mood systems of normal volunteers was investigated. In half of the studies rTMS over the LPFC transiently induced a decrease in self-rated happiness and an increase of sadness compared to the effects of right prefrontal cortical rTMS (George et al. 1996; Pascual-Leone et al. 1996; Dearing et al. 1997). Three more recent studies (Cohrs et al. 1998; Nedjat et al. 1998; Mosimann et al. 2000) failed to demonstrate any effects on mood in healthy volunteers.
6 Effects on mood in major depression
Because of its ability to focally interfere with neuronal circuits, rTMS has been proposed and subsequently researched as a putative therapeutic approach in refractory major depression (Nemeroff 1996; Nestler 1998). As in the studies of mood modulation by rTMS, the DLPFC has been the most important target for stimulation in major depression studies. George (1995a, b) reported the first open study of the effects of rTMS in six patients with refractory depression treated with five daily rTMS sessions to the left DLPFC. He reported that two patients in this study experienced improvement as assessed by a reduction of 26% in the Hamilton rating scale for depression (HRSD) scores. Open and blinded studies of rTMS to the left DLPFC followed with varying results. A relatively large open study demonstrated that 42% of 56 patients responded to five daily rTMS sessions; the elderly exhibited a considerably lower response rate (Figiel et al. 1998). A 2-week treatment study resulted in a 41% decrease in HRSD scores in another open trial (Triggs et al. 1999). However, there are open studies that have failed to demonstrate any antidepressant activity of rTMS (Schouten et al. 1999).
In the sham-controlled, single-blinded studies of rTMS in treatment-resistant depression, effect sizes have varied considerably. In a within-subject crossover, sham-controlled study of 12 depressed patients treated for 2 weeks with stimulation to the left DLPFC only somewhat modest antidepressant efficacy of rTMS was found (George et al. 1997). In a more recent study, an antidepressant effect in 20 subjects that was statistically different from sham stimulation using similar stimulation parameters in a parallel design, but still only of modest clinical impact, was demonstrated (Berman et al. 2000). In some studies a low stimulation intensity of 80% of motor threshold was used. Generally, it seems that higher intensity may be more effective, though (Loo et al. 1999) found no differences between active and sham rTMS using a much higher stimulation intensity (110% of motor threshold)—an observation which was confirmed in a relatively older outpatient patient group (Schlaepfer et al. 2001). In a large sham-controlled trial with 71 patients that utilized low-frequency rTMS, it was demonstrated that 1 Hz stimulation to the right DLPFC was significantly more effective than sham stimulation (Klein et al. 1999). It is unclear whether stimulation of the left DLPFC at these parameters would have had the same effect. The effect of frequency was compared in a study in which 18 patients were randomized to single pulse TMS, 10 Hz rTMS and sham rTMS delivered to the left DLPFC. A mild antidepressant effect with single pulse TMS has been demonstrated (Padberg et al. 1999). A sham-controlled trial in which 20 patients were randomly assigned to receive an equivalent number of pulses at 5 or 20 Hz over 2 weeks was reported in which both active groups experienced a 45% reduction in depression severity ratings and none of the patients responded to the sham stimulation (George et al. 2000). This suggests that lower frequencies may have therapeutic efficacy as well, which is important because slow rTMS is associated with a lower seizure risk. An analysis of treatment response and cerebral metabolism suggests that patients with hypometabolism at baseline may respond better to high-frequency stimulation (20 Hz), whereas those with baseline hypermetabolism respond better to 1 Hz stimulation (Kimbrell et al. 1999). However, the effects of rTMS on mood examined in this study were not statistically significant. A very carefully designed study, assessing effects of both high- and low-frequency rTMS in depression, found that longer than previously reported treatment durations (4 versus 2 weeks) led to significantly better treatment results in both conditions (Fitzgerald et al. 2003).
There are indications that TMS stimulation at higher amplitudes might be more efficacious (Padberg et al. 2002). A negative correlation between the distance from the coil to the cortex and antidepressant response expressed as the percentage of HAMD rating decrease before and after treatment in a relatively older patient group with treatment of refractory major depression was reported (Mosimann et al. 2002). This study demonstrated that there might be a process of prefrontal atrophy that outpaces motor cortex atrophy in chronically depressed middle-aged subjects. An even more recent study demonstrated in thirty-one patients suffering from a pharmacotherapy-resistant major depressive episode, which were randomly assigned to three treatment groups receiving rTMS at different stimulation intensities, that improvement of depressive symptoms after rTMS significantly increased with stimulation intensity across the three groups. This supports the hypothesis of a relationship between stimulation intensity of rTMS and antidepressant efficacy (Padberg et al. 2002).
These observations together with the established fact that therapeutic seizures have a strong and reliable effect in depression lead to the development of another method, which uses rTMS at convulsive levels as a more targeted form of convulsive therapy. Efficacy and side effects of ECT seem to be dependent upon the path of the current passed through the brain (Sackeim et al. 1993; Sackeim 2000). Therefore targeting seizures to focal cortical areas, such as regions of the prefrontal cortex, may reduce some of the side effects of convulsive treatment. Magnetic seizure therapy (MST) has now been tested in proof of concept studies both in non-human primates and patients (Lisanby et al. 2001, 2003) and preliminary results on cognitive side effects of the treatment compared to those of ECT have been obtained (Lisanby et al. 2001, 2003). Much additional research is obviously needed to evaluate the putative clinical efficacy of this approach and to determine if it has significant advantages over ECT in terms of similar effects and a better side effect profile.
Some early data in relatively smaller patient populations in open (Grunhaus et al. 2000; Dannon et al. 2002) and randomized (Janicak et al. 2002) trials suggest that even non-convulsive rTMS at 110% of motor threshold has similar efficacy as ECT in patients with major depression. Burt et al. (2002) conducted in the framework of a large meta-analysis of rTMS studies in depression an analysis of those studies directly comparing rTMS to ECT. The general effect size for TMS in these studies was greater than in the studies comparing TMS to sham, most likely reflecting a subject selection bias. The authors suggested that TMS probably works best in patients who are candidates for ECT. Most importantly, it has been demonstrated that rTMS has no adverse memory effects compared to unilateral ECT (Schulze-Rauschenbach et al. 2005). Some authors suggest that rTMS and ECT might prove to be complimentary clinical tools, potentiating each other’s antidepressant effects (Fitzgerald 2004).
More recently, the method of meta-analysis has been applied to the body of literature in the field of rTMS in depression (Holtzheimer et al. 2001; McNamara et al. 2001; Burt et al. 2002; Martin et al. 2002, 2003). While all including different studies and applying different methods of analysis, they find that the antidepressant effect of rTMS is higher than the one of sham treatment. Overall these antidepressant effects are moderate and reviews do not agree in terms of clinical significance of the method at this point in time (Schlaepfer et al. 2003). In the future the following requirements have to be met in order to gather conclusive results (Holtzheimer et al. 2004):
-
Large, multi-site trials are warranted to clarify clinical utility of effects of rTMS.
-
Appropriate randomization, adequate blinding of subjects and therapists, better assessment of the duration of any antidepressant effects
-
More research on which patient and treatment characteristics lead to greater antidepressant effects
-
More research on potential mechanisms by which rTMS produces antidepressant effects
7 Synthesis
Today the data on clinical efficacy of rTMS in mood disorders is not unequivocal but nevertheless interesting and encouraging. Rigorously controlled, double-blinded multicenter trials are urgently needed in order to adequately address the question of rTMS’ clinical efficacy. Prior to such studies, technical problems in the application of TMS have to be solved, e.g., more satisfactory sham conditions must be developed. Today, using analogies to antidepressant drug development, valid phase II trials must be conducted. Crucial unanswered questions remain including the long-term efficacy of TMS, prevention of relapse and long-term side effects. The key findings in the acute treatment of depression have not been systematically replicated, and effect sizes have often been small and variable. Sources of variability across studies include differences in stimulation parameter settings, concomitant medications, and different characteristics of patient samples. In addition, simple and economical methods for precise and reproducible coil placement are needed, as this factor is likely important for effectiveness (Kozel et al. 2000). In much of this work, the magnitude of antidepressant effect, while often statistically significant, has been below the threshold of clinical usefulness (Berman et al. 2000) and has not lived up to expectations raised by encouraging results in animal studies. Furthermore, the persistence of antidepressant effects beyond the 1- to 2-week treatment period has rarely been examined. Initial evidence suggests that the beneficial effects may be transitory, making the development of maintenance strategies important if rTMS is to become clinically applicable.
Establishing whether non-convulsive rTMS has antidepressant properties aside from its clinical usefulness is of theoretical importance, because positive data support the notion that focally targeted manipulations of cortical function can result in mood improvement. Nonetheless, the future of rTMS is far from certain in its usefulness as a clinical addition to the antidepressant armamentarium. A recent systematic review of published and unpublished studies on the effectiveness of rTMS in the treatment of refractory major depression demonstrated both a relative lack in the overall quality of studies (compared to drug registration trials) and the lack of a main effect (Martin et al. 2003).
There is no consensus about the exact mechanisms of action of how rTMS might induce antidepressant effects. However, this is also the case for many other antidepressant treatments. Research on rTMS has mainly been empirical. There are many variables of rTMS application and a large parameter space has therefore to be carefully explored in order to find the most efficacious treatment. This process will most likely be slow, because there is only public funding available for such studies. Nevertheless, rTMS has clearly effects on the brain—which is certainly remarkable—and it might be that rTMS is a treatment modality in search of a suitable application in psychiatry, which might well be depression at other parameters of stimulation.
However, from the viewpoint of the neuroscientist, TMS is a methodology with great potential as a research tool (Hallett 2000; Lisanby et al. 2000, 2002). This technique, by itself and combined with other methods such as EEG and neuroimaging, may be useful to test functional connectivity, neuroplasticity, information processing (for example, in the visual system), indirect and direct motor control, and aspects of mood control. It affords testing of either general hypotheses of the function of the brain at different levels and hypotheses of the underlying pathology of neuropsychiatric disorders. Even if the early enthusiasm which prevailed after early studies of clinical effects in the treatment of mood disorders settled down somewhat, rTMS will be even more useful as an investigational tool of basic and clinical research.
References
Aggleton JP (1993) The contribution of the amygdala to normal and abnormal emotional states. Trends Neurosci 16(8):328–333
Barker AT, Jalinous R, Freeston IL (1985) Noninvasive magnetic stimulation of human motor cortex. Lancet 2:1106–1107
Belmaker B, Fitzgerald P, George MS, Lisanby HS, Pascual-Leone A, Schlaepfer TE, Wassermann E (2003) Managing the risks of repetitive transcranial stimulation. CNS Spectr 8(7):489
Berman RM, Narasimhan M, Sanacora G, Miano AP, Hoffman RE, Hu XS, Charney DS, Boutros NN (2000) A randomized clinical trial of repetitive transcranial magnetic stimulation in the treatment of major depression. Biol Psychiatry 47(4):332–337
Bickford RG, Guidi M, Fortesque P, Swenson M (1987) Magnetic stimulation of human peripheral nerve and brain: response enhancement by combined magnetoelectrical technique. Neurosurgery 20(1):110–116
Bohning D, Pecheny A, Epstein C, Speer A, Vincent D, Dannels W, George M (1997) Mapping transcranial magnetic stimulation (TMS) fields in vivo with MRI. Neuroreport 8(11):2535–2538
Bohning DE, Shastri A, Wasserman EM, Ziemann U, Lorberbaum JP, Nahas Z, Lomarev MP, George MS (2000) BOLD-fMRI response to single-pulse transcranial magnetic stimulation (TMS). J Magn Reson Imaging 11:569–574
Burt T, Lisanby SH, Sackeim HA (2002) Neuropsychiatric applications of transcranial magnetic stimulation: a meta analysis. Int J Neuropsychopharmacol 5(1):73–103
Catafau A, Perez V, Gironell A, Martin J, Kulisevsky J, Estorch M, Carrio I, Alvarez E (2001) SPECT mapping of cerebral activity changes induced by repetitive transcranial magnetic stimulation in depressed patients. A pilot study. Psychiatr Res 106:151–160
Cohrs S, Tergau F, Riech S, Kastner S, Paulus W, Ziemann U, Ruther E, Hajak G (1998) High-frequency repetitive transcranial magnetic stimulation delays rapid eye movement sleep. Neuroreport 9(15):3439–3443
Dannon PN, Dolberg OT, Schreiber S, Grunhaus L (2002) Three and six-month outcome following courses of either ECT or rTMS in a population of severely depressed individuals–preliminary report. Biol Psychiatry 51(8):687–690
Dearing J, George MS, Greenberg BD, Wassermann EM, Schlaepfer TE, Murphy DL, Hallet M, Post RM (1997) Mood effects of prefrontal repetitive high frequency transcranial magnetic stimulation (rTMS) in healthy volunteers. CNS Spectr 2(1):53–68
Doi W, Sato D, Fukuzako H, Takigawa M (2001) c-Fos expression in rat brain after repetitive transcranial magnetic stimulation. Neuroreport 12(6):1307–1310
Figiel GS, Epstein C, McDonald WM, Amazon-Leece J, Figiel L, Saldivia A, Glover S (1998) The use of rapid-rate transcranial magnetic stimulation (rTMS) in refractory depressed patients. J Neuropsychiatry Clin Neurosci 10(1):20–25
Fitzgerald P (2004) Repetitive transcranial magnetic stimulation and electroconvulsive therapy: complementary or competitive therapeutic options in depression? Australas Psychiatry 12(3):234–238
Fitzgerald PB, Brown TL, Marston NA, Daskalakis ZJ, De Castella A, Kulkarni J (2003) Transcranial magnetic stimulation in the treatment of depression: a double-blind, placebo-controlled trial. Arch Gen Psychiatry 60(10):1002–1008
Fleischmann A, Prolov K, Abarbanel J, Belmaker RH (1995) The effect of transcranial magnetic stimulation of rat brain on behavioral models of depression. Brain Res 699(1):130–132
Flitman S, Grafman J, Wassermann E, Cooper V, O’Grady J, Pascual-Leone A, Hallett M (1998) Linguistic processing during repetitive transcranial magnetic stimulation. Neurology 50(1):175–181
Foerster A, Schmitz JM, Nouri S, Claus D (1997) Safety of rapid-rate transcranial magnetic stimulation: heart rate and blood pressure changes. Electroencephalogr Clin Neurophysiol 104:207–212
Geddes LA (1991) History of magnetic stimulation of the nervous system. J Clin Neurophysiol 8(1):3–9
George MS, Ketter TA, Parekh PI, Horwitz B, Herscovitch P, Post RM (1995a) Brain activity during transient sadness and happiness in healthy women. Am J Psychiatry 152(3):341–51
George MS, Wasserman EM, Williams WA, Callahan A, Ketter TA, Basser P, Hallett M, Post RM (1995b) Daily repetitive transcranial magnetic stimulation (rTMS) improves mood in depression. Neuroreport 6(14):1853–1856
George MS, Wassermann EM, Williams WA, Steppel J, Pascual-Leone A, Basser P, Hallett M, Post RM (1996) Changes in mood and hormone levels after rapid-rate transcranial magnetic stimulation (rTMS) of the prefrontal cortex. J Neuropsychiatry Clin Neurosci 8(2):172–180
George MS, Wassermann EM, Kimbrell TA, Little JT, Williams WE, Danielson AL, Greenberg BD, Hallett M, Post RM (1997) Mood improvement following daily left prefrontal repetitive transcranial magnetic stimulation in patients with depression: a placebo-controlled crossover trial. Am J Psychiatry 154(12):1752–1756
George MS, Lisanby SH, Sackeim HA (1999) Transcranial magnetic stimulation: applications in neuropsychiatry. Arch Gen Psychiatry 56(4):300–311
George M, Nahas Z, Molloy M, Speer A, Oliver N, Li X, Arana G, Risch S, James C, Ballenger J (2000) A controlled trial of daily left prefrontal cortex TMS for treating depression. Biol Psychiatry 48(10):962–970
Graf T, Engeler J, Achermann P, Mosimann U, Noss R, Fisch H-U, Schlaepfer TE (2001) High frequency repetitive transcranial magnetic stimulation (rTMS) of the left dorsolateral cortex: EEG topography during waking and subsequent sleep. Psychiatry Res-Neuroimaging 107(1):1–9
Grisaru N, Yaroslavsky Y, Abarbanel JM, Lamberg T, Belmaker R (1994) Transcranial magnetic stimulation in depression and schizophrenia. Euro Neuropsychopharmacol 4:287–288
Grunhaus L, Dannon PN, Schreiber S, Dolberg OH, Amiaz R, Ziv R, Lefkifker E (2000) Repetitive transcranial magnetic stimulation is as effective as electroconvulsive therapy in the treatment of nondelusional major depressive disorder: an open study. Biol Psychiatry 47(4):314–324
Hallett M (2000) Transcranial magnetic stimulation and the brain. Nature 406:147–150
Hausmann A, Marksteiner J, Hinterhuber H, Humpel C (2001) Magnetic stimulation induces neuronal c-fos via tetrodotoxin-sensitive sodium channels in organotypic cortex brain slices in rat. Neuroscience Letters 310:105–108
Höflich G, Kasper S, Hufnagel A, Ruhrmann S, Möller HJ (1993) Application of transcranial magnetic stimulation in the treatment of drug-resistant major depression: a report of two cases. Human Psychopharmacol 8:361–365
Holtzheimer PE III, Russo J, Avery DH (2001) A meta-analysis of repetitive transcranial magnetic stimulation in the treatment of depression. Psychopharmacol Bull 35(4):149–169
Holtzheimer P, Avery D, Schlaepfer TE (2004) Significance of antidepressant effects of rTMS. Br J Psychiatry:541–542
Huber R, Graf T, Cote KA, Wittmann L, Gallmann E, Matter D, Schuderer J, Kuster N, Borbely AA, Achermann P (2000) Exposure to pulsed high-frequency electromagnetic field during waking affects human sleep EEG. Neuroreport 11(15):3321–3325
Janicak PG, Dowd SM, Martis B, Alam D, Beedle D, Krasuski J, Strong MJ, Sharma R, Rosen C, Viana M (2002) Repetitive transcranial magnetic stimulation versus electroconvulsive therapy for major depression: preliminary results of a randomized trial. Biol Psychiatry 51(8):659–667
Ji RR, Schlaepfer TE, Aizenman CD, Epstein CM, Qiu D, Huang JC, Rupp F (1998) Repetitive transcranial magnetic stimulation activates specific regions in rat brain. Proc Natl Acad Sci USA 95(26):15635–15640
Kandel ER (1998) A new intellectual framework for psychiatry. Am J Psychiatry 155:457–469
Kandel ER (1999) Biology and the future of psychoanalysis: a new intellectual framework for psychiatry revisited. Am J Psychiatry 156(4):505–524
Keck ME, Sillaber I, Ebner K, Welt T, Toschi N, Kaehler ST, Singewald N, Philippu A, Elbel GK, Wotjak CT, Holsboer F, Landgraf R, Engelmann M (2000) Acute transcranial magnetic stimulation of frontal brain regions selectively modulates the release of vasopressin, biogenic amines and amino acids in the rat brain. Eur J Neurosci 12:3713–3720
Keck M, Welt T, Muller M, Erhardt A, Ohl F, Toschi N, Holsboer F, Sillaber I (2002) Repetitive transcranial magnetic stimulation increases the release of dopamine in the mesolimbic and mesostriatal system. Neuropharmacology 43(1):101
Kimbrell TA, Little JT, Dunn RT, Frye MA, Greenberg BD, Wassermann EM, Repella JD, Danielson AL, Willis MW, Benson BE, Speer AM, Osuch E, George MS, Post RM (1999) Frequency dependence of antidepressant response to left prefrontal repetitive transcranial magnetic stimulation (rTMS) as a function of baseline cerebral glucose metabolism. Biol Psychiatry 46(12):1603–1613
Klein E, Kreinin I, Chistyakov A, Koren D, Mecz L, Marmur S, Ben-Shachar D, Feinsod M (1999) Therapeutic efficacy of right prefrontal slow repetitive transcranial magnetic stimulation in major depression: a double-blind controlled study. Arch Gen Psychiatry 56(4):315–320
Kolbinger HM, Höflich G, Hufnagel A, Möller HJ, Kasper S (1995) Transcranial magnetic stimulation (TMS) in the treatment of major depression. Human Psychopharmacol 10:305–310
Kozel FA, Nahas Z, de Brux C, Molloy M, Lorberbaum JP, Bohning D, Risch SC, George MS (2000) How coil-cortex distance relates to age, motor threshold, and antidepressant response to repetitive transcranial magnetic stimulation. J Neuropsychiatry Clin Neurosci 12(3):376–384
Lane RD, Reiman EM, Ahern GL, Schwartz GE, Davidson RJ (1997) Neuroanatomical correlates of happiness, sadness, and disgust. Am J Psychiatry 154(7):926–933
Lisanby SH, Luber BTP, Sackeim HA (2000) Transcranial magnetic stimulation: application in basic neuroscience and neuropsychopharmacology. Int J Neuropsychopharmacol 3(3):259–273
Lisanby SH, Schlaepfer TE, Fisch HU, Sackeim HA (2001) Magnetic Seizure Therapy of Major Depression. Arch Gen Psychiatry 58(3):303–305
Lisanby SH, Kinnunen LH, Crupain MJ (2002) Applications of TMS to therapy in psychiatry. J Clin Neurophysiol 19(4):344–360
Lisanby S, Luber B, Barroilhet L, Neufeld E, Schlaepfer TE, Sackeim H (2003) Safety and feasibility of magnetic seizure therapy (MST) in major depression: randomized within-subject comparison with electroconvulsive therapy. Neuropsychopharmacology 28(10):1852–1865
Loo C, Mitchell P, Sachdev P, McDarmont B, Parker G, Gandevia S (1999) Double-blind controlled investigation of transcranial magnetic stimulation for the treatment of resistant major depression. Am J Psychiatry 156(6):946–948
Loo C, Sachdev P, Elsayed H, McDarmont B, Mitchell P, Wilkinson M, Parker G, Gandevia S (2001) Effects of a 2– to 4–week course of repetitive transcranial magnetic stimulation (rTMS) on neuropsychologic functioning, electroencephalogram, and auditory threshold in depressed patients. Biol Psychiatry 49:615–623
Lorberbaum JP, Wassermann EM (2000). Safety concerns of TMS. In: George MS, Belmaker R (eds) Transcranial magnetic stimulation in neuropsychiatry. American Psychiatric Press, Washington, pp 141–161
Martin J, Barbanoj M, Schlaepfer T, Clos S, Perez V, Kulisevsky JAG (2002) Transcranial magnetic stimulation for treating depression. (Cochrane review). The Cochrane Library, Oxford
Martin JL, Barbanoj MJ, Schlaepfer TE, Thompson E, Perez V, Kulisevsky J (2003) Effectiveness of repetitive transcranial magnetic stimulation for the treatment of depression: systematic review and meta-analysis. Br J Psychiatry 182:480–491
Mayberg HS (1997) Limbic-cortical dysregulation: a proposed model of depression. J Neuropsychiatry Clin Neurosci 9(3):471–841
McNamara B, Ray JL, Arthurs OJ, Boniface S (2001) Transcranial magnetic stimulation for depression and other psychiatric disorders. Psychol Med 31(7):1141–1146
Moser DJ, Jorge RE, Manes F, Paradiso S, Benjamin ML, Robinson RG (2002) Improved executive functioning following repetitive transcranial magnetic stimulation. Neurology 58(8):1288–1290
Mosimann UP, Rihs TA, Engeler J, Fisch HU, Schlaepfer TE (2000) Mood effects of repetitive transcranial stimulation (rTMS) of left prefrontal cortex in healthy volunteers. Psychiatry Res 94(3):251–256
Mosimann U, Marré SC, Werlen S, Schmitt W, Hess CW, Fisch HU, Schlaepfer TE (2002) Antidepressant effects of repetitive transcranial magnetic stimulation in the elderly—correlation between effect size and coil-cortex distance. Arch Gen Psychiatry 59(2):560–561
Murray NMF (1991) Magnetic stimulation of cortex: clinical applications. J Clin Neurophysiol 8(1):66–76
Nedjat S, Folkerts HW, Michael ND, Arolt V (1998) Evaluation of the side effects after rapid-rate transcranial magnetic stimulation over the left prefrontal cortex in normal volunteers. Electroencephalogr Clin Neurophysiol 107:196
Nemeroff C (1996) Augmentation strategies in patients with refractory depression. Depress Anxiety 4:169–181
Nestler E (1998) Antidepressant treatments in the 21st century. Biol Psychiatriy 44:526–533
Padberg F, Zwanzger P, Thoma H, Kathmann N, Haag C, Greenberg BD, Hampel H, Moller HJ, (1999) Repetitive transcranial magnetic stimulation (rTMS) in pharmacotherapy-refractory major depression: comparative study of fast, slow and sham rTMS. Psychiatry Res 88(3):163–171
Padberg F, Zwanzger P, Keck M, Kathmann N, Mikhaiel P, Ella R, Rupprecht P, Thoma H, Hampel H, Toschi N, Moller H (2002) Repetitive Transcranial magnetic stimulation (rTMS) in major depression. relation between efficacy and stimulation intensity. Neuropsychopharmacology 27(4):638
Paradiso S, Robinson RG, Andreasen NC, Downhill JE, Davidson RJ, Kirchner PT, Watkins GL, Ponto LL, Hichwa RD (1997) Emotional activation of limbic circuitry in elderly normal subjects in a PET study. Am J Psychiatry 154(3):384–389
Pascual-Leone A, Catala MD, Pascual-Leone Pascual A (1996) Lateralized effect of rapid-rate transcranial magnetic stimulation of the prefrontal cortex on mood. Neurology 46(2):499–502
Paus T, Jech R, Thompson CJ, Comeau R, Peters T, Evans AC (1997) Transcranial magnetic stimulation during positron emission tomography: a new method for studying connectivity of the human cerebral cortex. J Neurosci 17(9):3178–3184
Peinemann A, Lehner C, Mentschel C, Münchau A, Conrad B, Siebner HR (2000) Subthreshold 5–Hz repetitive transcranial magnetic stimulation of the human primary motor cortex reduces intracortical paired-pulse inhibition. Neurosci Lett 296: 21–24
Sackeim HA (2000) Repetitive transcranial magnetic stimulation: what are the next steps? Biol Psychiatry 48:959–961
Sackeim HA, Prudic J, Devanand DP, Kiersky JE, Fitzsimons L, Moody BJ, McElhiney MC, Coleman EA, Settembrino JM (1993) Effects of stimulus intensity and electrode placement on the efficacy and cognitive effects of electroconvulsive therapy. N Engl J Med 328(12): 839–846
Schenck JF (2000) Safety of strong, static magnetic fields. J Magn Reson Imaging 12:2–19
Schlaepfer TE, Mosimann UP, Schmitt WJ, Fisch HU, Pearlson GD (2001) Repetitive transcranial magnetic stimulation (rTMS) in elderly patients with major depression. Biol Psychiatry 8S:160
Schlaepfer TE, Kosel M, Nemeroff CB (2003) Efficacy of repetitive transcranial magnetic stimulation (rTMS) in the treatment of affective disorders. Neuropsychopharmacology 28:201–205
Schouten EA, D’Alfonso AA, Nolen WA, De Haan EH, Wijkstra J, Kahn RS (1999) Mood improvement from transcranial magnetic stimulation. Am J Psychiatry 156(4):669–670
Schulze-Rauschenbach SC, Harms U, Schlaepfer TE, Maier W, Falkai P, Wagner M (2005) Distinctive neurocognitive effects of repetitive transcranial magnetic stimulation and electroconvulsive therapy in major depression. Br J Psychiatry 186:410–416
Shajahan PM, Glabus MF, Steele JD, Doris AB, Anderson K, Jenkins JA, Gooding PA, Ebmeier KP (2002) Left dorso-lateral repetitive transcranial magnetic stimulation affects cortical excitability and functional connectivity, but does not impair cognition in major depression. Prog Neuropsychopharmacol Biol Psychiatry 26(5):945–954
Soares JC, Mann JJ (1997) The anatomy of mood disorders–review of structural neuroimaging studies. Biol Psychiatry 41(1):86–106
Speer AM, Kimbrell TA, Wasserman EM, Repella JD, Willis MW, Herscovitch P, Post RM (2000) Opposite effects of high and low frequency rTMS on regional brain activity in depressed patients. Biological Psychiatry 48:1133–1141
Strafellea AP, Paus T, Barrett J, Dagher A (2001) Repetitive transcranial magnetic stimulation of the human prefrontal cortex induces dopamine release in the caudate nucleus. J Neurosci 21:RC1571–RC1574
Szuba MP, O’Reordon JP, Rai AS, Snyder-Kastenberg J, Amsterdam JD, Gettes DR, Wassermann E, Evans DL (2001) Acute mood and thyroid stimulating hormone effects of transcranial magnetic stimulation in major depression. Biol Psychiatry 50(1):22–27
Triggs WJ, McCoy KJM, Greer R, Rossi F, Bowers D, Kortenkamp S, Nadeau SE, Heilmann KM, Goodman WK (1999) Effects of left frontal transcranial magnetic simulation on depressed mood, cognition, and corticomotor threshold. Biol Psychiatry 45:1440–1445
Wassermann EM (2000) Side effects of repetitive transcranial magnetic stimulation. Depress Anxiety 12(3):124–129
Ziemann U, Hallett M (2000) Basic neurophysiological studies with TMS. In: George MS, Belmaker RH (eds) Transcranial magnetic stimulation in neuropsychiatry. American Psychiatric Press, Washington DC
Acknowledgments
Supported by grants 4038-044046 and 3231-044523 from the Swiss National Science Foundation to Dr. Schlaepfer. This is a usual setting for non-convulsive rTMS studies. Patients are awake, sitting relaxed in a chair while stimulation (here to the left dorsolateral prefrontal cortex) is applied. A typical stimulator, here with four booster modules affording high frequency stimulation is used. Note the oxygen tank nearby, which would be used as most important therapy in the event of a seizure developing.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Schlaepfer, T.E., Kosel, M. & Fisch, HU. Repetitive transcranial magnetic stimulation (rTMS) in depression. Poiesis Prax 4, 111–127 (2006). https://doi.org/10.1007/s10202-005-0019-7
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10202-005-0019-7