Abstract
Objective
This study examined health-related quality of life (HRQoL) in elderly patients with hypertension in Hong Kong (HK) by using EQ-5D-5L and estimated the minimally important difference (MID) of the EQ-5D-5L index score for this population.
Method
We analysed secondary data from a population-based cross-sectional patient experience survey in HK. The EQ-5D-5L HK version was used to assess patients’ HRQoL. The mean EQ-5D index scores for different subgroups were evaluated by ANOVA. Tobit regression models were used to investigate the relationship between hypertension and HRQoL. An instrument-defined approach was adopted to estimate the MID of the EQ-5D-5L index score.
Result
A total of 3,351 patients’ records met the selection criteria and were used in this study for our analysis. The mean age was 72.74 years, and 54.97% of respondents were female. The mean EQ-5D index score was 0.83. Most of the respondents (83.36%) reported having no problem with self-care. The Tobit regression model indicated that an increasing number of chronic conditions co-morbidity with hypertension contribute to a decrease in the EQ-5D index score. The overall MID estimate of the EQ-5D index score was 0.0917 and the adjusted MID was 0.0715. The MID estimates varied among respondents of different sexes and ages.
Conclusion
The HRQoL and MID estimate of EQ-5D for elderly individuals with hypertension was reported, which provide valuable information for assisting health-care professionals in making clinical decisions in hypertensive care.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Hypertension is a serious medical condition that causes people’s health to deteriorate across their entire lifespan. As estimated by World Health Organization (WHO), approximately 1.13 billion people are currently living with hypertension worldwide [1]. Hypertension is common among the elderly. In the UK, at least 50% of adults over 65 years have reported living with high blood pressure (a reading of 140/90 or higher) [2]. In the USA, nearly 80% of individuals aged 50 years or older live with high blood pressure or systolic hypertension [3]. In Hong Kong (HK), the prevalence of hypertension is nearly 65% among people aged 65–84 years [4]. Hypertension is usually asymptomatic; however, when it is left uncontrolled, it could increase the risk of developing many life-threatening complications and lead to poor physical and mental health-related quality of life (HRQoL) [5,6,7].
HRQoL has become increasingly important in clinical practice, and research into hypertension over the last decades [8], and provides a multidimensional perspective in that it takes into consideration a patient’s emotional and physical functioning, and social well-being [9]. Developing interventions aiming at improving HRQoL for patients is currently a primary goal of hypertension care [10]. HRQoL is evaluated mainly based on a questionnaire that is divided into two categories: generic and condition-specific measures. The generic questionnaire was further divided into preference-based (GPBM) and non-preference-based measures. The former was used to generate an index score based on public preference and then calculate the quality-adjusted life years (QALYs) for economic evaluation, whereas the latter was mainly used to detect the variance in clinical practice.
Recently, a number of studies have been published to evaluate the influence of hypertension and associated multimorbidity on HRQoL. The findings are fragmented and few of them specifically focused on elderly patients. Liu et al. reported that in China, HRQoL declined when elderly people with hypertension or associated multimorbidity reported living alone [11]. Alonso et al. found that elderly people with hypertension have low HRQoL, both mentally and physically, in a large population-based multi-centre study [12]. A systematic study pointed out that individuals, including elderly patients, with hypertension have a low HRQoL, but that the magnitude of the difference between with and without hypertension is small [13]. Another study in Vietnam indicated that respondents with advanced age and co-morbidity were negatively associated with QoL [14]. Although these studies provide some information to support hypertension-related decision making, there is an increasing need for a well-designed, reliable economic evaluation, using GPBM data, of the care of elderly patients with hypertension, to allocate the health and social resources for long-term financing and planning [15]. By 2025, hypertension is likely to affect more than 1.56 billion people around the world [16], and the majority of them will be middle-aged or elderly people, and this will have a direct impact on their life expectancy. Thus, an estimation of HRQoL among elderly hypertensive patients is critical for future policy development.
To interpret changes in health status and quality of life measures in clinical practice or primary health care [17], studies for defining and calculating the minimally important difference (MID) estimates of the index scores by using GPBM are increasing. MID has been recommended by the US. Food and Drug Administration as an important tool to quantifying minimal variations, using patients’ reported outcome measures that represent a meaningful change for the patient’s health states and can help clinicians comprehensively evaluate the efficiency of interventions [18]. This kind of MID estimation uses a patient-centred approach and explores not only the meaningful biological changes to patients, but also the value that patients attribute to the changes according to their HRQoL [19]. Although previous studies have reported the importance of MID, few MID estimates of the index score determined by using GPBM have been published worldwide [20,21,22], especially for specific diseases, such as hypertension.
EQ-5D, developed by EuroQoL group, is one of the most widely used GPBM for measuring patients’ HRQoL [23]. It is recommended as the standard measure in the application of health technology assessment in many European countries [24,25,26]. However, no study has been found using EQ-5D to specifically measure the HRQoL of elderly patients with hypertension in HK. Therefore, the current study aimed to (1) examine HRQoL using EQ-5D-5L, and (2) estimate MID of EQ-5D index scores among elderly patients with hypertension.
Methods
Data source
The data were derived from a population-wide cross-sectional patient experience on specialist outpatient services in a public health-care setting in HK [27]. The survey was conducted among the patients who attended any of the selected 26 public specialist outpatient clinics (SOPCs). Recruits had to be aged 18 years or above and able to speak and understand Cantonese. Patients who were day cases or day surveys or those from paediatric, hospice, psychiatric, dental, anaesthesiology, pathology or nurse-led or multispeciality outpatient clinics were excluded. All the patients who visited the SOPCs during the appointed surveying period were requested to answer a structured questionnaire over the phone within 1 week after their attendance at SOPCs. In addition to the evaluative questions on patient experience, the respondents were also asked to indicate their health states using EQ-5D-5L HK (descriptive system) and self-reported long-standing conditions such as their physical status and whether they had chronic conditions. A total of 13,966 patients responded to the survey. Among them, the data of 3351 patients aged 60 years or older reported having at least hypertension were elicited for analysis in this study.
Multimorbidity status
In this study, multimorbidity status was defined as the presence of chronic conditions that occur simultaneously with hypertension. If the patient only reported having hypertension, this was defined as no multimorbidity. If the patient reported having hypertension and other chronic diseases, this was defined as having multimorbidity. To define the levels of multimorbidity status, the following distinctions were made: patients who lived only with hypertension were classified as having “no multimorbidity”; at Level 1 respondents had hypertension and another chronic condition; at Level 2, hypertension and two other chronic conditions; and Level 3, hypertension together with three or more chronic conditions. The eight major chronic conditions, namely, vision problems, hearing problems, physical disabilities, learning problems, mental problems, heart disease, diabetes, and cancer were identified among the selected respondents in the study and were used to evaluate the relationship between HRQoL and the level of multimorbidity status.
Health-related quality of life measurement
EQ-5D-5L is one of the most widely used GPBMs. It has five dimensions: mobility (MO), self-care (SC), usual activities (UA), pain/discomfort (PD) and anxiety/depression (AD). Each dimension has five levels (no, slight, moderate, severe and unable/extreme problems). All the health states reported in the five dimensions can be converted into a single summary index score that can be used to estimate the QALYs for health economic evaluation [28]. The index score ranges from 0 to 1, where 1 means full health and 0 means death. The EQ-5D-5L HK version was developed and validated in an HK cultural setting in accordance with the latest international protocol [29], as such people’s HRQoL could be evaluated by taking into consideration HK perceptions of culture and value systems [29]. In this study, the EQ-5D-5L index score was calculated based on HK local algorithm [29].The normative profile of HK’s general population has been reported as well and could be used as a reference for comparison with other studies [30]. The index score was estimated using the HK population tariff in the study.
Statistical analysis
Descriptive statistics were used to describe respondents’ demographic and socioeconomic status (SES). The EQ-5D index score was reported as means and standard deviations, and stratified by age and sex. All the respondents in the sample were categorised into three age groups (60–70 years [young–old], 71–80 years [middle–old] and ≥ 81 years [old–old]) for analysis as well as based on sex (male and female) and educational levels (no/primary, secondary/post-secondary and tertiary or above). Working status (retirement, unemployment, housewife and fully employed), living status (living alone, living with families/others and living in an institute) and government allowance status (receiver or non-receiver) were used as proxy questions to understand respondents’ SES. Given that EQ-5D index scores were non-normally distributed (Shapiro–Wilk test, p value < 0.05), the differences in mean EQ-5D index scores in subpopulations were assessed using the bootstrap version (n = 600) of a robust ANOVA method [31].
The heteroscedastic Tobit regression analysis was adopted to estimate the effect of hypertension and associated multimorbidity status on HRQoL, adjusted by SES variables stratified by sex and age groups. Seven models were generated in total: overall, male young–old, male middle–old, male old–old, female young–old, female middle–old, and female old–old. The Tobit regression model is a censored model and designed to estimate the linear relationships between variables when either left- or right-censoring occurs in the dependent variable, for example, the EQ-5D index score [32]. Data were analysed using R (R Foundation, Austria). Due to multiple subgroups comparison, we applied a Bonferroni correction resulting in a significance level of 0.001 (0.05/40) [33].
An instrument-defined approach was adopted to estimate the MID of EQ-5D-5L HK index score among elderly patients with hypertension [22]. The MID estimate was based on the average scores of differences between the baseline state of health and single-level transitions with two directions to the other adjacent health states; for example, the baseline health state is ‘33,333’ and the possible adjacent health state of single-level transitions could be ‘33,332’ (less anxiety/depression, improved [better status]) and ‘33,334’ (more anxiety/depression, deteriorated [worse status]). Additionally, given that no state could be better than the best state (11,111) and no state could be worse than the worst state (55,555), these two health statuses were not included in the estimation of improved or deteriorated MID. To reduce the bias of the estimation, the maximum value of single-transition between different levels of EQ-5D dimensions should be removed [18]. According to the HK scoring algorithm, the difference in transition between Levels 3 (moderate problem) and 4 (extreme problem) of the five dimensions of EQ-5D is larger than those between any other levels. Thus, these maximum-value scoring parameters (between Levels 3 and 4) could be removed to reduce the bias of the MID estimations. In this study, four types of MID were presented: overall (oMID, all single-level transitions were included), adjusted overall MID (aMID, the maximum-value scoring parameters were removed), improved MID (iMID, based on the health state toward better direction) and deteriorated MID (dMID, based on health state towards worse direction). The effect size (ES) of MID was also reported, and the range between 0.2 and 0.5 suggests that the MID estimate reaches the minimum meaningful change in the index score. The LOESS smoothing approach was used to estimate the relationship between EQ-5D-5L observed index score and MID estimates [34].
Results
Table 1 presents the respondents’ demographics, SES status and mean EQ-5D index score. Among the respondents, 44.58% were young–old, 35.51% were middle–old, and 19.91% were old–old respondents. The mean age was 72.74 years. In addition, 54.97% were female, and nearly 80% had received secondary or above educational qualifications. Regarding multimorbidity status, 35.66%, 12.71% and 0.63% of the respondents reported the status at Level 1, Level 2 and Level 3, respectively. The mean EQ-5D index score was 0.83. Respondents who were male, highly educated, fully employed, living with family, and having hypertension alone attained a high EQ-5D index score (the index scores stratified by age and sex are presented in the supplementary document).
Figure 1 presents the distribution of the EQ-5D index score. Overall, 40% of the respondents reported having full health, and the distribution was highly negatively skewed: 60%, 50% and 30% of young–old, middle–old and old–old male respondents reported having full health, respectively, while the proportions of full health for female respondents in different age groups were 40%, 30% and 20%, respectively.
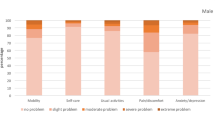
Table 2 indicates the percentage of respondents who reported having health problems in each dimension of EQ-5D and stratified by sex and age. Overall, 83.36% of the respondents reported having no problems with self-care, followed by anxiety/depression (79.17%), usual activities (70.40%), mobility (69.08%) and pain/discomfort (51.06%). For old–old females, only 34.64% reported having no problems with mobility, whereas the proportion for male respondents was 51.15%. By gender, only 63.68% and 45.45% of young–old male and female respondents reported having no problems with pain/discomfort, respectively.
The Tobit regression models indicate that female respondents reported a lower index score than male respondents (coefficient = −0.13, p < 0.001). Compared with retired respondents, fully employed (coefficient = 0.06, p < 0.05) respondents tended to have better HRQoL. The increased number of chronic comorbidities with hypertension had a statistically significant association with decreased index score (coefficient = −0.09 for level 1, coefficient = −0.11 for level 2, and coefficient = −0.35 for level 3, p < 0.001). For young–old male respondents, the index score increased with increasing age (coefficient = 0.13, p < 0.01); however, the trend was reversed in middle–old and old–old females (coefficient = −0.01, p < 0.05; coefficient = −0.02, p < 0.001) as well as middle–old males (coefficient = −0.01, p < 0.01). For the old–old respondents (both male and female), no other variables, except those for age and multimorbidity status, had a statistically significant effect on the variation of index scores (Table 3).
Four types of MID estimates are presented in Table 4. The oMID estimate was 0.0917 (SD = 0.0121, 95% confidence interval [CI] 0.0679–0.1154); the aMID, iMID and dMID estimates were 0.0715, 0.0723 and 0.0699, respectively (the MID estimates stratified by sex and age are presented in a supplementary document). Given that less than 8% of respondents reported EQ-5D index scores smaller than 0.5, in order to avoid bias we estimated the relationship between the MID estimates and the observed EQ-5D index scores greater than 0.5 (Fig. 2). There was a steady enhancement of MID estimates alongside the increasing EQ-5D index score for both male and female respondents at different age groups. The iMID and dMID estimates for different age and sex groups were varied.
Discussion
Our study presents the HRQoL of people aged 60 years or above with hypertension, and living in HK. Elderly patients with hypertension had lower EQ-5D index scores than the general population [30]. The index score decreased with increasing age, and the male respondents scored higher than female respondents. Moreover, four different types of MIDs were estimated using EQ-5D-5L for patients with hypertension and stratified by age and sex. The oMID was lower than that reported in Canada [35]. The results provide a useful reference for assessing the efficiency of clinical intervention based on patient-reported outcomes (PRO).
Age, as predicted, was negatively correlated to HRQoL. The respondents reported a decreasing HRQoL with increasing age, especially the very old respondents (old–old group), whose index score was 21.1% lower than those of the middle–old respondents. This is in line with the findings reported in previous studies. For example, Zhang et al. found that older people always reported a low EQ-5D index score in both urban and rural areas in one province in China [36]. Katsi et al. used SF-36 and reported that age is negatively associated with HRQoL among patients with hypertension [37]. In this study, the association with HRQoL varied among different age groups. Compared with middle–old and old–old respondents, the relationship between HRQoL and age was positive for young–old male respondents. It might be due to good body composition, functional fitness, and close psychosocial connection among this group of the respondents [38]. However, given no longitudinal data, it is impossible to conclude a causal relationship from our analysis, and further explorations are needed. Moreover, no SES variables were found to significantly affect the HRQoL of old–old respondents. Compared with studies indicating that people with low SES tend to have poor health conditions [39], our findings found that health condition may be not equal to HRQoL; the former is objective, but the latter is more subjective [40]. This suggests policymakers should take note that, for the elderly, especially the very old, hypertensive population, improving their HRQoL and helping them live in dignity is more important than regaining physical health. Additionally, the impact of household income, which may be an important factor affecting health of elderly hypertensive patients, on HRQoL was not directly measured in this study. Further investigations are needed to explore the relationship between growing health-care inequities and HRQoL in this large elderly population [41].
Females obtained a lower index score than males across all age groups, and the gap increased with age. This is in line with the findings of several previous studies. A Polish study found that elderly female patients with hypertension reported a lower QoL compared with male patients [42]. A UK study found that the HRQoL of older female primary care receivers is likely to be lower than that of males [43]. Previous studies explained this phenomenon mainly based on the evidence that women have longer life expectancy than men but in poor health conditions and are therefore more likely to report a low HRQoL [41,42,43]. However, we found that female respondents always scored a lower index score than males across all age groups in our sample. Further studies are expected to explore the effect of other intrinsic and instrumental factors on the hypertensive patients’ HRQoL regardless of sex on the basis of a comprehensive perspective of physical, mental and social well-being.
EQ-5D dimension analysis showed that pain/discomfort is the topmost problem that affects respondents’ HRQoL. Despite being insufficiently studied, there are some pathophysiological and clinical correlations between pain and hypertension [44]. In our study, nearly half of hypertensive patients reported suffering from pain, and females were in more pain than males. When stratified by age groups, more than 60% of old–old females showed some pain-related problems that exerted a negative influence on their mobility and usual activities. However, as pain is not a direct result of hypertension, it might be induced by other side effects [44], the conclusion that pain was attributed to hypertension in our sample should be interpreted with caution due to the nature of cross-sectional study.
As previous studies indicated [45, 46], we found there is a relationship between an increased number of chronic conditions and decreased HRQoL. The multivariable regression analysis identified that, overall, when examining the difference in index scores between levels of multimorbidity status, scores decreased dramatically for patients with hypertension co-morbidity with other chronic conditions (Level 2 vs. Level 3), where the biggest fall in coefficient was 0.26 for the young–old females (Level 2 vs. Level 3). Further analysis identified that for middle–old and old–old patients, the index score of females declined faster than in males, which was indicated by previous study [47]; however, for young–old patients, the phenomenon was reversed. As no patients in the old–old group reported having three or more chronic conditions associated with hypertension, our findings are not conclusive and more empirical evidence is needed.
It is well known that EQ-5D data have a ceiling effect. In our study, 40% of respondents indicated a state of full health, which was lower than the 46% reported by HK’s general population [30]. In addition, fewer female respondents reported full health than male respondents, and the proportion decreased with increasing age. This is in line with the findings of previous studies [33, 48]. When stratified by age, the proportion of full-health respondents dropped by 51.84% and 40.37% in the young–old to old–old group for female and male respondents, respectively, with the largest fall being 40.44% (female middle–old vs. female old–old). Although previous studies indicated that compared with males, females had significantly lower index scores even after adjusting for demographic and socioeconomic factors [49], our study added information on quantifying the variation of EQ-5D index score for elderly hypertensive patients. The variations should be further explored in other age groups for people with hypertension and other associated multimorbidity.
Although evidence is limited, we highly recommend that the MID estimate of a specific condition be developed to determine the efficiency of clinical interventions from the perspective of HRQoL. In our study, we calculated the MID estimate using the instrument-defined approach. The overall mean MID estimate was 0.0917, which is similar to the findings of Tsiplova et al. (MID estimate of 0.093, as determined by EQ-5D for adult patients with hypertension in Canada) [35]. No previous studies explored the MID estimates stratified by sex and age in the hypertension population. In the present study, we found that the oldest female respondents tended to report higher MID estimates than both their younger counterparts and male respondents. However, the results should be interpreted with caution as no ‘one-size-fits-all’ method exists for estimating the MID of HRQoL scores. For example, the MID estimate using the distribution-based method is usually larger than those using the anchor-based method [50]. As such, we should consider adopting different methods in the future to yield an MID estimate in a plausible range rather than a single value [51].
Moreover, the MID estimate for a PRO measurement is not an intrinsic characteristic that may vary across patients’ characteristics and treatments [20]. Our study found that hypertension patients in different sex and age groups have different MID estimates that may vary when patients get better or worse after receiving clinical treatment. However, Jaeschke et al. indicated that continuing experience could be accumulated among patients living with a specific disease for a long time and that it might exert an effect on the MID estimate [52]. Hypertension is a chronic disease, which means it is a lifelong condition. In our study, all the respondents were elder, suggesting that the majority of them were living with hypertension for years. Resilience and adoption might create a different MID estimate when the target population comprises young patients. Moreover, the changes in MID estimates may be affected by disease severity and the treatment context [51]. Although some factors were not considered in our MID estimate, the findings should be seen as a valuable step to help clinicians and health outcome researchers to collect information in interpreting the importance and meaningful change in assessing the effectiveness of clinical interventions for hypertension.
Hypertension is an important risk factor for cardiovascular morbidity and mortality, especially in the elderly. The sample used in our study came from a relatively large study population, which is representative of the general Chinese population. The findings could bear significant policy implications for hypertension and associated multimorbidity control, both regionally and internationally. Additionally, this is the first attempt to estimate the MID value for this population, and provides a plausible range of the smallest change in index score that may be considered meaningful to the patient. Our findings may serve as a useful supplement to inform hypertension control and management domestically and globally.
Some limitations should be addressed. First, information on chronic conditions in our survey was based on a self-report questionnaire and therefore no clinical information was collected, which may have affected the estimation of the relationship between SES and HRQoL among patients with hypertension. Second, all the respondents in the study were recruited from specialist outpatient clinics in HK and may introduce some concerns on the ability to generalise our findings to the overall population. Third, because of the limited number of patients who reported an EQ-5D index score ≤ 0.5 in our sample, the relationship between index score and MID estimate might vary when including patients with hypertension and other middle to severe health problems. Finally, anchor-based and other methods should be used in the future to make the MID estimate convincing.
Conclusion
The effects of age, educational level, working and living status and multimorbidity status on HRQoL were statistically significant among elderly patients with hypertension in HK, whereas the effects varied between different age groups. The MID estimates provide a valuable perspective to help clinicians evaluate the effectiveness of interventions for improving the health of elderly patients with hypertension in HK. Despite these challenges, future studies should be conducted to capture the variance of HRQoL for patients with hypertension co-morbidity with other chronic conditions.
Data Availability
The data may be available by contact with the corresponding author.
References
World Health Organization: A global brief on hypertension. World Health Day (2013)
Age UK: Blood pressure-do I have high blood pressure. https://www.ageuk.org.uk/information-advice/health-wellbeing/conditions-illnesses/high-blood-pressure/. Accessed 10 Oct 2019
Franklin Stanley, S., Jacobs Milagros, J., Wong Nathan, D., et al.: Predominance of isolated systolic hypertension among middle-aged and elderly us hypertensives: analysis based on National Health and Nutrition Examination Survey (NHANES) III. Hypertens. J. Am. Hear. Assoc. 37, 869–874 (2001). https://doi.org/10.1161/01.HYP.37.3.869
The Government of the Hong Kong Special Administrative Region Centre for Health Protection-Hypertension. (2016). https://www.chp.gov.hk/en/healthtopics/content/25/35390.html
Liang, Z., Zhang, T., Lin, T., et al.: Health-related quality of life among rural men and women with hypertension: assessment by the EQ-5D-5L in Jiangsu China. Qual. Life Res. (2019). https://doi.org/10.1007/s11136-019-02139-3
Alhalaiqa, F., Deane, K.H.O., Nawafleh, A.H., et al.: Adherence therapy for medication non-compliant patients with hypertension: a randomised controlled trial. J. Hum. Hypertens. 26, 117 (2011). https://doi.org/10.1038/jhh.2010.133
Buford, T.W.: Hypertension and aging. Ageing research reviews. 26, 96–111 (2016). https://doi.org/10.1016/j.arr.2016.01.007
Tchicaya, A., Lorentz, N., Demarest, S., et al.: Relationship between self-reported weight change, educational status, and health-related quality of life in patients with diabetes in Luxembourg. Health Qual. Life Outcomes 13, 149 (2015). https://doi.org/10.1186/s12955-015-0348-8
Baladón, L., Rubio-Valera, M., Serrano-Blanco, A., et al.: Gender differences in the impact of mental disorders and chronic physical conditions on health-related quality of life among non-demented primary care elderly patients. Qual. Life Res. 25, 1461–1474 (2016). https://doi.org/10.1007/s11136-015-1182-5
Benetos, A., Petrovic, M., Strandberg, T.: Hypertension management in older and frail older patients. Circ. Res. 124, 1045–1060 (2019). https://doi.org/10.1161/CIRCRESAHA.118.313236
Liu, N., Zeng, L., Li, Z., et al.: Health-related quality of life and long-term care needs among elderly individuals living alone: a cross-sectional study in rural areas of Shaanxi Province China. BMC Public Health (2013). https://doi.org/10.1186/1471-2458-13-313
Alonso, J., Ferrer, M., Gandek, B., et al.: Health-related quality of life associated with chronic conditions in eight countries: results from the International Quality of Life Assessment (IQOLA) project. Qual. Life Res. 13, 283–298 (2004). https://doi.org/10.1023/B:QURE.0000018472.46236.05
DaissonJ, T., LeilaB, M., AlessandraC, K., et al.: Health-related quality of life and hypertension: a systematic review and meta-analysis of observational studies. J. Hypertens. 29, 179–188 (2011). https://doi.org/10.1097/HJH.0b013e328340d76f
Ha, N.T., Duy, H.T., Le, N.H., et al.: Quality of life among people living with hypertension in a rural Vietnam community. BMC Public Health (2014). https://doi.org/10.1186/1471-2458-14-833
Pavlik, V.N., Greisinger, A.J., Pool, J., et al.: Does reducing physician uncertainty improve hypertension control?: rationale and methods. Circ. Cardiovasc. Qual. Outcomes 2, 257–263 (2009). https://doi.org/10.1161/CIRCOUTCOMES.109.849984
AlcocerL, CuetoL: Hypertension, a health economics perspective. Ther. Adv. Cardiovasc. Dis. 2, 147–155 (2008). https://doi.org/10.1177/1753944708090572
Brazier, J.: Measuring and valuing health benefits for economic evaluation, 2nd edn. Oxford University Press, Oxford (2007)
Mcclure, N.S., Sayah, F.A.I., Xie, F., et al.: Instrument-defined estimates of the minimally important difference for EQ-5D-5L index scores. Value Health 20, 644–650 (2017). https://doi.org/10.1016/j.jval.2016.11.015
Jayadevappa, R., Cook, R., Chhatre, S.: Minimal important difference to infer changes in health-related quality of life—a systematic review. J. Clin. Epidemiol. 89, 188–198 (2017). https://doi.org/10.1016/j.jclinepi.2017.06.009
Mcclure, N.S., Sayah, F.A.I., Ohinmaa, A., et al.: Minimally important difference of the EQ-5D-5L index score in adults with type 2 diabetes. Value Health 21, 1090–1097 (2018). https://doi.org/10.1016/j.jval.2018.02.007
Crosby, R.D., Kolotkin, R.L., Williams, G.R.: Defining clinically meaningful change in health-related quality of life. J. Clin. Epidemiol. 56, 395–407 (2003). https://doi.org/10.1016/S0895-4356(03)00044-1
NanA, L., JeffreyJ, J., StephenJ, C.: Using instrument-defined health state transitions to estimate minimally important differences for four preference-based health-related quality of life instruments. Med. Care. 48, 365–371 (2010). https://doi.org/10.1097/MLR.0b013e3181c162a2
Ramos-Goñi, J.M., Oppe, M., Slaap, B., et al.: Quality control process for EQ-5D-5L valuation studies. Value Health 20, 466–473 (2017). https://doi.org/10.1016/j.jval.2016.10.012
Sullivan, P.W., Ghushchyan, V.H.: EQ-5D Scores for diabetes-related comorbidities. Value Health 19, 1002–1008 (2016). https://doi.org/10.1016/j.jval.2016.05.018
Rencz, F., Gulácsi, L., Drummond, M., et al.: EQ-5D in Central and Eastern Europe: 2000–2015. Qual. Life. Res. 25, 2693–2710 (2016). https://doi.org/10.1007/s11136-016-1375-6
Rowen, D., Azzabi Zouraq, I., Chevrou-Severac, H., et al.: International regulations and recommendations for utility data for health technology assessment. Pharmacoeconomics 35, 11–19 (2017). https://doi.org/10.1007/s40273-017-0544-y
XU, R.H., Wong, E.L.Y.: Involvement in shared decision-making for patients in public specialist outpatient clinics in Hong Kong. Patient Prefer. Adherence 11, 505–512 (2017)
Rabin, R., Oemar, M., Oppe, M., et al.: EQ-5D-5L user guide. Basic inf how to use EQ-5D-5L instrum. 28. (2015). https://www.euroqol.org/fileadmin/user_upload/Documenten/PDF/Folders_Flyers/EQ-5D-5L_UserGuide_2015.pdf. Accessed 10 Oct 2019
Wong, E.L.Y., Ramos-Goñi, J.M., Cheung, A.W.L., et al.: Assessing the use of a feedback module to model EQ-5D-5L health states values in Hong Kong. Patient 11, 235–247 (2018). https://doi.org/10.1007/s40271-017-0278-0
Wong, E.L.-Y., Cheung, A.W.-L., Wong, A.Y.-K., et al.: Normative profile of health-related quality of life for Hong Kong general population using preference-based instrument EQ-5D-5L. Value Health 22, 916–924 (2019). https://doi.org/10.1016/j.jval.2019.02.014
Wilcox, R.R.: Introduction to Robust Estimation and Hypothesis Testing, 3rd edn. Elsevier, Amsterdam (2011). https://doi.org/10.1016/C2010-0-67044-1
Wu, M., Brazier, J.E., Kearns, B., et al.: Examining the impact of 11 long-standing health conditions on health-related quality of life using the EQ-5D in a general population sample. Eur. J. Health Econ. 16, 141–151 (2014). https://doi.org/10.1007/s10198-013-0559-z
Konnopka, A., Koenig, H.-H.: The “no problems”-problem: an empirical analysis of ceiling effects on the EQ-5D 5L. Qual. Life Res. 26, 2079–2084 (2017). https://doi.org/10.1007/s11136-017-1551-3
Cleveland, R., Cleveland, W., Terpenning, I.: STL: a seasonal-trend decomposition procedure based on loess. J. Off. Stat. 6, 3 (1990)
Tsiplova, K., Pullenayegum, E., Cooke, T., et al.: EQ-5D-derived health utilities and minimally important differences for chronic health conditions: 2011 Commonwealth fund survey of sicker adults in Canada. Qual. Life Res. 25, 3009–3016 (2016). https://doi.org/10.1007/s11136-016-1336-0
Zhang, Y., Zhou, Z., Gao, J., et al.: Health-related quality of life and its influencing factors for patients with hypertension: evidence from the urban and rural areas of Shaanxi Province China. BMC Health Serv. Res. (2016). https://doi.org/10.1186/s12913-016-1536-x
Katsi, V., Kallistratos, M.S., Kontoangelos, K., et al.: Arterial hypertension and health-related quality of life. Front. Psychiatry (2017). https://doi.org/10.3389/fpsyt.2017.00270
Gouveia, É., Gouveia, B., Ihle, A., et al.: Correlates of health-related quality of life in young–old and old–old community-dwelling older adults. Qual. Life Res. 26, 1561–1569 (2017). https://doi.org/10.1007/s11136-017-1502-z
Robert, S.A., Cherepanov, D., Palta, M., et al.: Socioeconomic status and age variations in health-related quality of life: results from the national health measurement study. J. Gerontol. Ser. B 64B, 378–389 (2009). https://doi.org/10.1093/geronb/gbp012
Chou, C.-Y., Ma, M.-C., Yang, T.-T.: Determinants of subjective health-related quality of life (HRQoL) for patients with schizophrenia. Schizophr. Res. 154, 83–88 (2014). https://doi.org/10.1016/j.schres.2014.02.011
Cassel, C.K.: Medicare matters what geriatric medicine can teach. American Health Care (2005)
Uchmanowicz, B., Chudiak, A., Mazur, G.: The influence of quality of life on the level of adherence to therapeutic recommendations among elderly hypertensive patients. Patient Prefer. Adherence 12, 2593–2603 (2018)
Eisele, M., Kaduszkiewicz, H., König, H.-H., et al.: Determinants of health-related quality of life in older primary care patients: results of the longitudinal observational AgeCoDe Study. Br. J. Gen. Pract. 65, e716 (2015). https://doi.org/10.3399/bjgp15X687337
Saccò, M., Meschi, M., Regolisti, G., et al.: The Relationship between blood pressure and pain. J. Clin. Hypertens. 15, 600–605 (2013). https://doi.org/10.1111/jch.12145
Prazeres, F., Santiago, L.: Relationship between health-related quality of life, perceived family support and unmet health needs in adult patients with multimorbidity attending primary care in Portugal: a multicentre cross-sectional study (Survey). Health Qual. Life Outcomes (2016). https://doi.org/10.1186/s12955-016-0559-7
Wang, L., Palmer, A., Cocker, F., et al.: Multimorbidity and health-related quality of life (HRQoL) in a nationally representative population sample: implications of count versus cluster method for defining multimorbidity on HRQoL. Health Qual. Life Outcomes (2017). https://doi.org/10.1186/s12955-016-0580-x
Park, B., Ock, M., Lee, H.A., et al.: Multimorbidity and health-related quality of life in Koreans aged 50 or older using KNHANES 2013–2014. Health Qual. Life Outcomes (2018). https://doi.org/10.1186/s12955-018-1016-6
Herdman, M., Gudex, C., Lloyd, A., et al.: Development and preliminary testing of the new five-level version of EQ-5D (EQ-5D-5L). An. Int. J. Qual. Life Asp. Treat Care Rehabil. 20, 1727–1736 (2011). https://doi.org/10.1007/s11136-011-9903-x
Hajian-Tilaki, K., Heidari, B., Hajian-Tilaki, A.: Are gender differences in health-related quality of life attributable to sociodemographic characteristics and chronic disease conditions in elderly people? Int. J. Prev. Med. 8, 95 (2017). https://doi.org/10.4103/ijpvm.IJPVM_197_16
Szende, A., Janssen, B., Cabases, J.: Self-reported population health: an international perspective based on EQ-5D [electronic resource]. (2014)
Revicki, D., Hays, R.D., Cella, D., et al.: Recommended methods for determining responsiveness and minimally important differences for patient-reported outcomes. J. Clin. Epidemiol. 61, 102–109 (2008). https://doi.org/10.1016/j.jclinepi.2007.03.012
Jaeschke, R., Singer, J., Guyatt, G.H.: Measurement of health status: ascertaining the minimal clinically important difference. Control Clin. Trials 10, 407–415 (1989). https://doi.org/10.1016/0197-2456(89)90005-6
Funding
No funding supported the study.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
Ethical approval was obtained from the Clinical Research Ethics Committees of the hospital authority. All of the respondents were informed of their rights, the purpose of the study and details of the research procedures before conducting the interview. The study was conducted according to the Declaration of Helsinki. All of the data were kept confidential and anonymous.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Wong, E.L.Y., Xu, R.H. & Cheung, A.W.L. Health-related quality of life in elderly people with hypertension and the estimation of minimally important difference using EQ-5D-5L in Hong Kong SAR, China. Eur J Health Econ 21, 869–879 (2020). https://doi.org/10.1007/s10198-020-01178-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10198-020-01178-9
Keywords
- Health-related quality of life
- Hypertension
- Elderly patients
- Minimally important difference
- EQ-5D
- Hong Kong
- China