Abstract
Objectives
Stroke is a leading cause for disability and morbidity associated with increased economic burden due to treatment and post-stroke care (PSC). The aim of our study is to provide information on resource consumption for PSC, to identify relevant cost drivers, and to discuss potential information gaps.
Methods
A systematic literature review on economic studies reporting PSC-associated data was performed in PubMed/MEDLINE, Scopus/Elsevier and Cochrane databases, Google Scholar and gray literature ranging from January 2000 to August 2016. Results for post-stroke interventions (treatment and care) were systematically extracted and summarized in evidence tables reporting study characteristics and economic outcomes. Economic results were converted to 2015 US Dollars, and the total cost of PSC per patient month (PM) was calculated.
Results
We included 42 studies. Overall PSC costs (inpatient/outpatient) were highest in the USA ($4850/PM) and lowest in Australia ($752/PM). Studies assessing only outpatient care reported the highest cost in the United Kingdom ($883/PM), and the lowest in Malaysia ($192/PM). Fifteen different segments of specific services utilization were described, in which rehabilitation and nursing care were identified as the major contributors.
Conclusion
The highest PSC costs were observed in the USA, with rehabilitation services being the main cost driver. Due to diversity in reporting, it was not possible to conduct a detailed cost analysis addressing different segments of services. Further approaches should benefit from the advantages of administrative and claims data, focusing on inpatient/outpatient PSC cost and its predictors, assuring appropriate resource allocation.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Stroke is one of the leading causes for disability and morbidity in the Western world [1]. According to the World Health Organization (WHO), stroke is the second leading cause of death after heart disease, accounting for almost seven million deaths in 2012 worldwide, which represents 11.1% of total deaths [2, 3]. In Europe, more than one million of new stroke cases occur each year, and currently six million of stroke survivors are estimated to be alive [4]. In 27 European Union (EU) countries, the annual costs for stroke treatment and care are estimated to be 27 billion euros, with 18.5 billion accounting for direct medical costs and 8.5 billion for indirect costs (e.g., loss of productivity). An additional 11.1 billion euros are estimated to account for informal care. In the USA, a total of $65.5 billion was spent on stroke in 2008, with 67% for direct and 33% for indirect costs [5]. The American Heart Association and The American Stroke Association projected for the years 2012 to 2030, that the total direct medical cost for stroke will triple and reach up to $184.1 billion [6].
Depending on the severity of the stroke and its consequences, patients may need constant care for the remaining lifetime. Therefore, the clinical and economic burden of the disease contributes to significant public health relevance. As reported by the National Stroke Association, 40% of all patients acquire moderate to severe impairments and need special care, while 10% require constant care in long-term care facilities [7]. For the years 2001–2005, the average cost for medication and for outpatient stroke rehabilitation services in the first year after discharge were $11,145 per patient with $7318 spent for rehabilitation services and $3376 for medication [3].
Most studies focused on cost of acute care or comparison of two or more rehabilitation programs [8,9,10,11], but only a limited number of studies evaluated costs of post-stroke care [12]. Using different types of rehabilitation services or post-stroke care programs offered in the same setting but with different care approaches, the benefits for the patient can be maximized while costs are minimized [13,14,15]. As the cost of post-stroke care imposes a considerable economic burden on the society, the identification of the major cost drivers in published studies supports an informed policy making process and promotes gaining knowledge on how to guide decisions in the organization of post-stroke care programs. Therefore, our systematic literature review aims to fill the gap by providing information on the costs of post-stroke care, identifying relevant cost drivers and discussing potential information gaps.
Methods
We conducted a systematic review of partial and full economic studies evaluating post-stroke treatment and care. The included studies comprised stroke patients who participated in post-stroke care programs, and the observed outcome was cost of post-stroke care. As our review primarily aims at describing the total cost elicited by post-stroke care, we did not cover any potential comparators to the applied interventions.
Framework
A systematic literature search was performed in Medline (PubMed), Scopus (Elsevier) and Cochrane library databases (data range from January 1, 2000 to August 1, 2016), with the algorithm presented in Online Resource 1. To ensure completeness of the search, we also searched the reference lists of included studies for additional relevant citations. We considered the need to assess gray literature, including searches via Google Scholar, which did not yield any citation beyond the traditional search. We did not apply any language filters in this search. This study is registered in PROSPERO (International prospective register of systematic reviews) under number CRD42016043521.
We included studies that were partial or full economic evaluations. Partial economic evaluation is defined as cost description (reporting only on the cost of a program, without a comparator, e.g., cost of illness, burden of illness) and cost analysis, as a central feature of all economic evaluations, where only the cost of alternatives are evaluated [16]. A full economic evaluation is defined as the comparative analysis of cost and clinical consequences of program alternatives (including cost-effectiveness, cost-minimization, cost-utility and cost-benefit analysis) [16]. All studies not reporting the costs of post-stroke care were excluded. Systematic reviews, qualitative studies, dissertations, case reports and conference abstracts were not included. Further exclusion criteria were: studies exclusively reporting on diseases other than stroke; enrolling only patients younger than 18 years; focusing only on stroke prevention, on acute stroke or transient ischemic attack (TIA) treatment, or reporting only inpatient post-stroke care costs; studies published in non-Latin languages.
The titles and abstracts screening was performed by two independent assessors (SR, HB), according to the predetermined selection criteria. Full-text articles of selected studies were reviewed and included if they met the inclusion eligibility criteria.
Data extraction and synthesis
Two authors (SR, HB) independently extracted relevant data regarding the following study criteria: first author, publication year, country, currency, study design, index year, number of patients, stroke type, follow-up period and costing perspective (“Appendix 1”, Tables 2, 3). Extracted data regarding the cost of post-stroke care program were costs of medical interventions, physiotherapy, occupational and speech therapy, nursing care, primary care visits, readmissions to hospital and emergency care during rehabilitation period, as well as medication, community services, transportation, meals on wheels, assistive devices and other health care related costs. Disagreements were resolved by consensus, and when this was not possible, by a third author (HG). Costs were extracted only for post-stroke care resource utilization. In case of reports on cost of two or more rehabilitation programs, each program was considered separately, as specific for the country where the study was performed.
At first instance, cost figures for post-stroke care were extracted. If acute care was included, this share of costs was subtracted from total costs. The remaining cost share was considered as cost of post-stroke care. To standardize results of included studies, all costs were transformed to 2015 US Dollars using purchasing power parity rates (PPP) [17] and the consumer price index (CPI) [18]. For comparison reasons, we calculated and report the cost of post-stroke care per patient month (PM), as studies reported on different follow-up periods. All calculations were performed by two authors independently (SR, HB). An example of cost calculation is provided in the Online Resource 2.
The mean costs of overall post-stroke care were calculated as the mean costs of all programs and visualized as boxplots. The mean costs of post-stroke care per country were calculated for each country independently, weighted by the number of patients for the respective country and visualized as bar charts (“naïve” analysis).
The Kolmogorov–Smirnov test was performed to check for normality of data, and the unpaired t test was used to determine if mean cost of post-stroke care differed between the short (up to 6 months) and long follow-up period (more than 6 months).
Gross domestic product (GDP) per capita for countries included in this review was derived from the World Bank data [19] in 2015 US dollars, and compared to weighted average cost of post-stroke care of each country. Acute stroke care supply and practice patterns of stroke care in each country were extracted or from the included studies or from web sites of state ministries (regarding the availability of stroke units) or from the OECD database (regarding the number of rehabilitation beds) [20]. Duration of acute care (reported in the study as length of stay in stroke unit/acute care) was derived directly from the publications included in this review. We used the Spearman`s rank correlation coefficient (rho) to calculate correlation. A meta-regression was performed based on publications that reported sufficient data to investigate heterogeneity and its reasons across the studies, using study characteristics (stroke type, costing perspective, type of health care funding, data source, presence of stroke units, follow-up period, period of data collection, detailed cost specification and duration of acute hospitalization) and post-stroke care costs. An α level of 0.05 was used to determine statistical significance explaining heterogeneity. All calculations and statistical analyses were performed in the software package STATA (Release 15, 2017. College Station, TX: StataCorp LLC) and SPSS (Version 20.0. Released 2011, Armonk, NY: IBM Corp.).
Assessment of methodological and reporting quality of included publications
The methodological quality of studies was evaluated with a checklist for assessing economic evaluations [21], as this is the most appropriate approach to ensure good quality for economic evaluations.
The Consolidated Health Economic Evaluation Reporting Standards (CHEERS) checklist [22] was used for evaluating the quality of reporting. A quality score was generated, awarding one point per each item of the checklist if this item has been reported, and zero if not, with maximum of 27 points. Three authors independently (SR, HB, JV) evaluated methodological quality of studies and quality of reporting in the studies, disagreements were resolved through consensus.
Results
Search results and description of studies
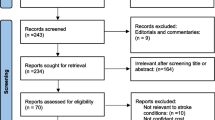
The systematic search yielded 1243 references in Medline via PubMed, 1602 in Cochrane databases and 334 in Scopus (Elsevier) database (August 1, 2016). After duplicates removal, a total of 2683 articles were selected for titles and abstracts screening. In the first step, 2607 papers were excluded: 960 due to publication type, 680 addressed diseases other than stroke, 647 addressed irrelevant intervention, 86 had outcomes other than cost of post-stroke care, 145 focused on acute stroke treatment, 20 studies were published in non-Latin languages and 69 studies evaluated a non-relevant population for the present analysis, that is, patients under 18 years old, caregivers, etc. Thereby, 76 publications were selected for full-text screening, of which 37 were excluded once they reported non-relevant outcome. A list of excluded studies, with the reason for exclusion is available in the Online Resource 3. Furthermore, three studies were selected by manual review of reference lists of all included studies. Finally, our systematic assessment of studies comprised 42 publications, see Fig. 1, flow chart of Preferred Reporting Items for Systematic reviews and Meta-Analyses (PRISMA) [23].
Published articles reflect the situation from United Kingdom (n = 7), Sweden (n = 7), Australia (n = 6), Germany (n = 4), USA (n = 4), Italy (n = 3), France (n = 2), The Netherlands (n = 2), Cuba (n = 1), Malaysia (n = 1), Canada (n = 1), Denmark (n = 1) Norway (n = 1) and Switzerland (n = 1), while one was multi-centric. All mentioned countries had public health funding, while the Malaysian health system is funded through both public and private sources [24]. Fifteen of the 42 studies reported cost about post-stroke care of ischemic and hemorrhagic stroke patients together, while five addressed only ischemic and two only hemorrhagic. Twenty studies did not provide information on type of stroke (Table 1).
The societal perspective was adopted in 17 out of 42 studies (40%). However, data on indirect costs (productivity losses related to illness or death as described by Luce et al. [25]) were not extracted since they were not part of our analysis. The follow-up period varied between 3 months and 10 years. Most of the included studies applied a follow-up period of 12 months (25 of 42 studies), while 12 adopted a follow-up of up to 6 months, and five studies reported cost on periods up to 10 years (Table 1). We observed a statistically significant difference in cost per patient month for studies that reported on shorter follow-up periods (up to 6 months) compared to longer ones (p = 0.02). Studies that provided cost for up to 6 months had higher values of cost per patient months than those reporting on 12 or more months of follow-up (mean difference of $968).
The costs in the reviewed publications were mostly obtained through hospital records, insurance administrative data, local or national registers and questionnaires. Detailed report on post-stroke care costs were presented in 40 studies, in form of inpatient and outpatient rehabilitation (including medical interventions, physiotherapy, occupational and speech therapy), nursing care (in nursing homes, specialized rehabilitation facilities or at home), primary care visits (including general physicians, specialist consultations), readmissions to hospital and emergency care during rehabilitation period, and other costs as medication, community services, transportation, meals on wheels, assistive devices and other health care related costs. General rehabilitation costs, without specification of type of care provided, were observed in two studies.
Quality assessment of studies
Methodological quality of studies was evaluated with the Drummond checklist [21], and for applicable criteria 30 studies had more than 17 score points (50% of all questions), including three criteria fulfilled by all and five criteria by more than 40 studies. Within this checklist, 83% of studies achieved yes scores regarding the study design, 85% regarding the data collection and 69% of yes scores in analysis and interpretation of results (Table 5 in Appendix 3 and Online Resource 4).
Reporting quality in studies was assessed with the CHEERS checklist [22]. All studies provided sufficient information on nine items of checklist, while on five items information was not available in more than half of included studies (Table 6 in Appendix 3 and Online Resource 4).
Cost of post-stroke care
We observed overall mean cost of post-stroke care, mean and weighted average costs regarding country of care provided (combining all studies reporting on respective country), length of follow-up period, inpatient/outpatient or outpatient-only reporting, and costing of different segments of post-stroke care.
Mean cost per patient month of post-stroke care for all programs (n = 60) reported in studies with inpatient and outpatient care setting was $1515 (SD $1396, median $1192), and $820 (SD $657, median $556) for programs (n = 17) in studies reporting only on outpatient care setting (Fig. 2).
The most expensive inpatient/outpatient post-stroke care was reported in the USA, with mean cost of $4644 per patient month, followed by Denmark ($3026), The Netherlands ($2214) and Norway ($2147). The lowest costs were reported in Italy ($845), followed by the UK ($866) and Germany ($871).
For the studies assessing only outpatient care, the highest costs were observed in the USA, with a mean of $1236 per patient month, followed by the UK ($1039). The lowest costs were reported in Malaysia ($192 per patient month), see Appendix 2, Table 4.
When the costs of post-stroke care were weighted for the number of patients of each program reported across the studies for each country, the USA ($4850) and Denmark ($3022) remained on leading positions, followed by Norway ($2147) and the Netherlands ($2016). The lowest costs per patient month were reported in Australia ($752) and Sweden ($768). For the studies that assessed only outpatient care, the highest costs were observed in the United Kingdom, with a weighted average of $883 per patient month, followed by the USA ($773). The lowest costs were reported in Malaysia ($192 per patient month), see Fig. 3 and Appendix 2, Table 4.
In addition, when the annual GDP per capita was taken into account, USA had the highest costs of post-stroke care per patient year ($58,200) compared to the GDP per capita ($55,837) and was followed by Denmark and Norway (Fig. 4). In Australia, Sweden, Switzerland and UK, costs of post-stroke care were only about one quarter of the GDP per capita. There was no information available on GDP per capita for study from Cuba, as well as for multi-centric study considering that this study covers cost data from 22 countries. For inpatient/outpatient studies, a positive correlation between GDP per capita and cost of post-stroke care is observed (ρ = 0.59, p = 0.045).
With regard to the acute stroke care supply and practice patterns of stroke care in each country (stroke units, number of rehabilitation beds available, duration of acute care), 14 studies did not report on the presence of stroke units (although stroke units were available in those countries), while in the other 16 studies presence of stroke units is reported for both outpatient and inpatient care setting (see Table 1). In outpatient-only settings, four studies reported on the presence of stroke units, while six studies did not (stroke units were available in those countries). In two publications, there were no stroke units in the hospital (one from UK [14] and one from Malaysia [24]).
Heterogeneity assessment
No statistically significant correlation was identified in the number of rehabilitation beds and cost of post-stroke care for the observed countries (ρ = 0.071, p = 0.811). Mean duration of acute care was 17.2 (SD 9.7) for inpatient and outpatient studies, and 18.6 (SD 14) days for outpatient-only studies. No statistical significant correlation could be detected regarding the duration of acute care and cost of post-stroke care (ρ = − 0.029, p = 0.957). For the assessment of heterogeneity, part of the studies included in this systematic review could be included in the meta-regression analysis. In total, six studies in the group of inpatient and outpatient studies [13, 26,27,28,29,30], and four studies in the group of outpatient-only studies [14, 15, 31, 32] have been included in the heterogeneity analysis. The remaining studies did not report the parameters needed to derive the variance needed for the meta-regression. In our (limited) meta-regression, none of the assessed characteristics contributed with statistical significance to the explanation of the heterogeneity between studies.
A detailed analysis of the costs of each service segment of post-stroke care was not possible due to heterogeneous reporting in studies. In general, rehabilitation services (including general rehabilitation, home based, inpatient, ward, day clinic, outpatient rehabilitation, nursing homes, aged care facilities and special accommodation) were identified as major contributors to the overall cost of post-stroke care in the majority of studies, in 26 studies on the first rank, and in 14 studies on the second rank. Within this category, the greatest amount of resources was allocated for rehabilitation and nursing care, which was pointed out by most of the authors. Rehabilitation service was followed by informal care and community services costs (including community and social services, home assistance and assisted living) which were recognized as the most expensive item in six studies, and on the second rank by another six studies. Rehospitalizations and medical interventions, including medications, were next segments of care on the cost-ranking list, being on the first rank in three studies, and on the second rank in eight studies.
Discussion
This systematic assessment of studies included 42 publications from which we have systematically extracted data regarding study characteristics and detailed data on cost of post-stroke care adjusted to 2015 US Dollars. We observed differences in costs of post-stroke care regarding region of care provided, and identified the USA as the country with highest cost of post-stroke care per patient month. We have recognized rehabilitation services as the main cost driver in post-stroke care, and we found significant differences in cost regarding reported diverse follow-up periods between studies. As there was no pattern for resource segments reporting, it was not possible to perform a detailed analysis of different post-stroke care segments.
Cost of post-stroke care is highly related to the stroke severity and length of stay in hospital, resulting with great impact on the level and duration of post-stroke care services utilization [33, 34]. There are several studies, including systematic reviews showing that stroke patients can benefit more from early rehabilitation services, which is also more cost-effective due to a shorter duration of stay in the hospital [8,9,10,11, 35].
To our knowledge, this is the first systematic review that addresses the cost specifically related to post-stroke care. It comprises studies conducted in different health care settings, addressing cost of post-stroke care in 14 countries from four different continents. Major strength of this research is that it provides knowledge about the overall expenses regarding post-stroke care setting, comprising also the different segments of services, and the identification of the main cost drivers in a global perspective. This review is reported according to the recommendations of PRISMA checklist, addressing all 27 items [23, 36] (Online Resource 5).
In relation to the current literature regarding the costs of the post-stroke management, most of the published studies have reported mainly on the total cost of stroke treatment or on the cost of acute care only. Demaerschalk et al. [37] reported on economic burden of stroke in the USA, including 28 articles, with main focus on short- and long-term direct costs, indirect and aggregated lifetime costs, limited only on the USA and highlighting that this search did not identify studies dealing with the cost of rehabilitation care. In this study, the most expensive segment of care was acute care, followed by next two main resource segments—nursing home and ambulatory care. In contrast, Ekman [38] and Grieve et al. [39] reported about cost of stroke in Europe. In the first study, direct costs for acute care followed by costs for hospital and home-based rehabilitation were observed as major costing items. Likewise, in the second study, outpatient costs were right after hospitalization costs as the most expensive item.
This systematic review describes the economic burden of stroke, independent of a health care region, with main focus on cost of post-stroke care, designating rehabilitation and nursing care as the major costing items. Like the other authors, we observed that more detailed research is needed in this field to fill the gap regarding accessible information in published studies. There is a need to form a methodologically and clinically supported list of segments of services that should be taken into account when reporting on cost of care. We can confirm the problem recognized by Ekman [38] and Brady et al. [8] regarding the comparability of studies based on different costs.
The highest mean cost per patient month was reported in the USA, which could be due to reports from special rehabilitation facilities described by Beeuwkes-Buntin et al. [26], where home rehabilitation was accounted for an amount of $1589, while the costs of care in inpatient rehabilitation facilities (IRF) and in skilled nursing facilities (SRF) summed up to $9379 and $6124 for a patient per month, respectively. The reason for this discrepancy could be attributed to the described type of patients who use this kind of special care and factors associated with longer stay in IRF and consequential admission to SRF (stroke severity, older age, comorbidities, absence of family caregivers, lower cognitive and functional status) [40, 41]. In Europe, higher cost of post-stroke care per patient month was observed in Denmark ($3022/PM), The Netherlands ($2016/PM) and Norway ($2147/PM) compared to other European countries. The finding could be explained by a lack of representative studies from northern European countries, or by different resource utilization in studies. This should be considered together with the fact that the weighted average cost of post-stroke care in seven studies from Sweden is estimated to be $768/PM (minimum of $548 and maximum of $2517), which is in favor of the previous argument. As reported in literature, the mean hospitalization costs of acute stroke care ranged from $8000 up to $23,000 and more [17, 37, 42], being similar to the burden in our findings, and—together with post-stroke care costs—imposing great economic importance.
The highest cost of post-stroke care were confirmed when compared to GDP per capita and USA was listed in the first place, with a weighted annual average of more than $2000 above GDP per capita. In contrast, the mean annual costs of post-stroke care in Australia were only about one-fifth of the GDP per capita (Fig. 4). Furthermore, we examined the acute stroke care supply and practice patterns of stroke care in each country. Two studies compared stroke care in stroke units and other hospital wards (Claesson et al. [43] and Kalra et al. [29]) and showed that stroke units are more cost-effective than other hospital wards. In two studies reporting on outpatient-only settings, stroke units were not available in the institution [14, 24]. The efficacy of stroke units is proven in many studies and may lead to lower costs of post-stroke care [44,45,46]. We were not able to confirm this finding in our review, which could be due to the very small number of studies reporting on institutions where stroke units were not existing. The costs of post-stroke care reported for the UK by Humphreys et al. [14] are similar to the costs reported by other authors from the same country (Patel et al. [15]) where stroke units were present.
Regarding the costs from the UK, the study from Kalra et al. [29] reports approximately two times lower post-stroke care costs than other publications [13, 47] for the same country. This difference may be explained by type of stroke patients evaluated in this study (only patients with mild stroke were included, while patients with severe stroke and those with specific neurological features were excluded).
In the available literature, we did not find information on cost differences regarding follow-up periods. We have observed that studies reporting on shorter follow-up (up to six months) exhibited significantly higher cost than those reporting on longer follow-up period (p < 0.05). This finding could be expected due to lower costs of care needed by the patients when they become more independent [48]. Furthermore, five studies [49,50,51,52,53] reported on periods longer than 1 year, and four of them described lower costs in subsequent years. In one study, due to prescription of new drugs which were more expensive than those previously used, the costs were higher in fourth year of follow-up [49].
Reporting on costs of each specific service utilization segment was diverse across studies; therefore, detailed analysis of each specific service utilization segment was not possible. Fifteen segments of specific services were observed in the reviewed studies. For example, in the studies from Hayes et al. [28] and Beeuwkes-Buntin et al. [26], only total post-stroke care cost is available, without specifying any costing details. On the other side, Bjorkdahl et al. [27] and Christensen et al. [54] reported on more than ten different costing segments of post-stroke care in their studies. This variety could be attributed to the use of a wide specter of data sources (administrative databases, insurance claims, hospital and care facility records, different kinds of registers, patient questionnaires etc.), as well as a different organization of health systems from country to country.
Our meta-regression did not identify characteristics explaining heterogeneity between studies. However, the number of studies providing the necessary evidence for inclusion into the meta-regression was limited, and therefore, it cannot be ruled out that some of the assessed characteristics do contribute to the observed heterogeneity.
There is a clear need for evaluation of post-stroke care programs, which may be offered in the same settings but with different care approaches. Considering patient education and prevention of complications, this could maximize benefits for patients while minimizing cost for society. A similar kind of evaluation was observed in four studies recognized by the present systematic review, in three studies [13,14,15] results (in terms of costs and outcomes) were in favor of the intervention, while in one study [31] there was no significant difference between the two groups compared. In those cases, use of health services was compared in the same settings, but with differences in intensity and services provided during the follow-up period. This kind of intervention does not require a structural reorganization of the health care system and could be easily integrated.
This review has several limitations. Publication and retrieval bias may occur while the results of published studies may be different from results of the studies that are not available through the databases included in our search strategy or not published at all. This bias could appear due to small sample size in studies or if the focus on cost of post-stroke care is considered to be interesting in a very limited context (e.g., national interest, health insurance). However, we performed comprehensive search strategies to minimize the retrieval bias, including manual search of the reference lists and searches via Google Scholar. In addition, to gather the most of available studies and minimize potential language bias, no filters regarding languages were applied and only studies published in non-Latin languages were excluded.
It is important to mention that even if the observed outcome (cost of post-stroke care) was the same for all publications, different post-stroke care programs were observed across the studies, including different regions, costing perspectives, monetary units, sample size, reporting on segments of services, type of stroke or level of stroke severity. It was challenging to generalize results reporting from diverse countries worldwide and to compare economical results, due to monetary difficulties (different units, floating exchange rates, purchasing power etc.). From a total number of 42 studies in this review, 40 were reporting from countries classified in the category of high income by the World Bank [42], while two studies reported on data from countries classified in the upper middle income economies (Akhavan Hejazi et al. [24] and Alonso-Freyre et al. [55]). With the use of CPI, we were able to adjust costs to unique unit system [56], and with PPP we made the costs more comparable, reducing price differences among countries [17, 57]. The lack of data from low, lower middle- and upper middle income economies (as defined by the World Bank) could lead to the overestimation of the costs in this research due to potentially lower cost of care in those categories. The way to overcome this limitation would be stimulation of further health economic research conceivably resulting in more publications from these regions.
Since the number of patients varied across the programs in studies, there was a concern that real average cost of post-stroke care for a single country could be biased. Therefore, we considered the sample size and calculated cost of post-stroke care for each country as mean and as weighted average for number of patients in each program described in studies of respective country. In our review, we could only include the data as published in the included studies, as the underlying raw data were not available. Nevertheless, it could be possible that some segments of costs are less thorough reported or differently categorized (e.g., joint in groups of the specific segments of post-stroke care) in the results of studies that reported costs less detailed. This could lead to potential bias in reporting of costs of post-stroke care segments within the studies, but not necessarily biasing overall costs.
A better picture of health services’ utilization could be captured with broader use of secondary data, as these data derive from detailed reimbursement databases and could be assumed to be nearly 100% complete, as enlightened by Swart [58] and Swart et al. [59]. Finally, the results should be viewed with some reserve as reviewed studies provide information on different health care regions, costing perspectives, heterogeneous types of stroke, different numbers of patients, and various forms of care delivered in diverse follow-up periods.
Conclusion
This review comprises cost of post-stroke care in 14 countries highlighting diversity between different health care regions worldwide. We were able to describe in which region the most costly delivery of care prevails, and identified rehabilitation services as the main contributor to the cost of post-stroke care. Due to diversity of reporting in studies, it was not possible to conduct a detailed analysis addressing different segments of services. Therefore, the need of more comprehensive research is evident to close this gap. Future research should focus on the association between the cost of post-stroke care and the supply of acute care, considering the correlation of post-stroke care costs with the availability of stroke units or the number of rehabilitation beds available. We strongly recommend reporting full information on the variance of empirical cost studies to allow for the assessment of uncertainty and the inclusion of the single study results into larger evidence syntheses such as meta-analysis, meta-regression, decision-analytic models, and value-of-information analyses [60, 61]. Future studies could benefit from the advantages of administrative and claims data, focusing on both inpatient and outpatient post-stroke care cost and its predictors, to assure appropriate resources allocation in the future.
Abbreviations
- TIA:
-
Transient ischemic attacks
- WHO:
-
World Health Organization
- PPP:
-
Purchasing power parity
- CPI:
-
Consumer Price Index
- CHEERS:
-
Consolidated Health Economic Evaluation Reporting Standards
- SRF:
-
Skilled nursing facilities
- IRF:
-
Inpatient rehabilitation facilities
- ESUS:
-
Extended stroke unit services
- OSUS:
-
Ordinary stroke unit services
- PSC:
-
Post-stroke care
- PM:
-
Patient month
- GDP:
-
Gross domestic product
- AUD:
-
Australian Dollar
- CAD:
-
Canadian Dollar
- DM:
-
Deutsche Mark
- SEK:
-
Swedish Krona
- CHF:
-
Swiss Franc
- £:
-
UK Pound
- $, USD:
-
US Dollar
References
Land Tirol. (2018). Projekt Integrierter Patientenpfad/Behandlungspfad Schlaganfall Tirol. https://www.schlaganfall-tirol.info https://www.tirol.gv.at/gesundheit-vorsorge/krankenanstalten/schlaganfall/projekt/. Accessed 4 Mar 2017
World Health Organization: Global Health Estimates: Deaths by Cause, Age, Sex and Country, 2000–2012. Geneva, WHO (2014)
Mozaffarian, D., Benjamin, E.J., Go, A.S., Arnett, D.K., Blaha, M.J., Cushman, M., de Ferranti, S., Despres, J.P., Fullerton, H.J., Howard, V.J., Huffman, M.D., Judd, S.E., Kissela, B.M., Lackland, D.T., Lichtman, J.H., Lisabeth, L.D., Liu, S., Mackey, R.H., Matchar, D.B., McGuire, D.K., Mohler, E.R. III, Moy, C.S., Muntner, P., Mussolino, M.E., Nasir, K., Neumar, R.W., Nichol, G., Palaniappan, L., Pandey, D.K., Reeves, M.J., Rodriguez, C.J., Sorlie, P.D., Stein, J., Towfighi, A., Turan, T.N., Virani, S.S., Willey, J.Z., Woo, D., Yeh, R.W., Turner, M.B.: Heart disease and stroke statistics–2015 update: a report from the American Heart Association. Circulation 131(4), e29–e322 (2015). https://doi.org/10.1161/cir.0000000000000152
Truelsen, T., Piechowski-Jozwiak, B., Bonita, R., Mathers, C., Bogousslavsky, J., Boysen, G.: Stroke incidence and prevalence in Europe: a review of available data. Eur. J. Neurol. 13(6), 581–598 (2006). https://doi.org/10.1111/j.1468-1331.2006.01138.x
Di Carlo, A.: Human and economic burden of stroke. Age Ageing. 38(1), 4–5 (2009). https://doi.org/10.1093/ageing/afn282
Ovbiagele, B., Goldstein, L.B., Higashida, R.T., Howard, V.J., Johnston, S.C., Khavjou, O.A., Lackland, D.T., Lichtman, J.H., Mohl, S., Sacco, R.L., Saver, J.L., Trogdon, J.G.: Forecasting the future of stroke in the United States: a policy statement from the American Heart Association and American Stroke Association. Stroke J. Cereb. Circ. 44(8), 2361–2375 (2013). https://doi.org/10.1161/STR.0b013e31829734f2
Stroke.org. (2018). Rehabilitation Therapy after a Stroke. http://www.stroke.org/we-can-help/stroke-survivors/just-experienced-stroke/rehab. Accessed 8 Feb 2018
Brady, B.K., McGahan, L., Skidmore, B.: Systematic review of economic evidence on stroke rehabilitation services. Int. J. Technol. Assess. Health Care 21(1), 15–21 (2005)
Anderson, C., Ni Mhurchu, C., Brown, P.M., Carter, K.: Stroke rehabilitation services to accelerate hospital discharge and provide home-based care: an overview and cost analysis. Pharmacoeconomics 20(8), 537–552 (2002)
Larsen, T., Olsen, T.S., Sorensen, J.: Early home-supported discharge of stroke patients: a health technology assessment. Int. J. Technol. Assess. Health Care 22(3), 313–320 (2006)
Tummers, J.F., Schrijvers, A.J., Visser-Meily, J.M.: Economic evidence on integrated care for stroke patients; a systematic review. Int. J. Integr. Care 12, e193 (2012)
Polder, J.J.: Cost of illness in the Netherlands: description, comparison and projection. Thesis, Erasmus University Rotterdam (2001)
Harrington, R., Taylor, G., Hollinghurst, S., Reed, M., Kay, H., Wood, V.A.: A community-based exercise and education scheme for stroke survivors: a randomized controlled trial and economic evaluation. Clin. Rehabilit. 24(1), 3–15 (2010). https://doi.org/10.1177/0269215509347437
Humphreys, I., Thomas, S., Phillips, C., Lincoln, N.: Cost analysis of the communication and low mood (CALM) randomised trial of behavioural therapy for stroke patients with aphasia. Clin. Rehabilit. 29(1), 30–41 (2015). https://doi.org/10.1177/0269215514537656
Patel, A., Knapp, M., Evans, A., Perez, I., Kalra, L.: Training care givers of stroke patients: economic evaluation. BMJ. 328(7448), 1102 (2004). https://doi.org/10.1136/bmj.328.7448.1102
Drummond, M.F., Sculpher, M.J., Torrance, G.W., O’Brien, B., Stoddart, G.L.,: Methods for the Economic Evaluation of Health Care Programmes, 3rd edn. Oxford University Press, Oxford (2005)
Wang, G., Zhang, Z., Ayala, C., Dunet, D.O., Fang, J., George, M.G.: Costs of hospitalization for stroke patients aged 18–64 years in the United States. J. Stroke Cerebrovasc. Dis. 23(5), 861–868 (2014). https://doi.org/10.1016/j.jstrokecerebrovasdis.2013.07.017
U.S. Department of Labor, Bureau of Labor Statistics, Consumer Price Index. All Urban Consumers (CPI-U). http://www.bls.gov/cpi/ (2015). Accessed 18 Dec 2015
World Bank. Data: GDP per capita. http://data.worldbank.org/indicator/NY.GDP.PCAP.CD (2016). Accessed 8 Aug 2016
OECD (2018) Hospital beds (indicator). https://doi.org/10.1787/0191328e-en
Drummond, M.F., Jefferson, T.O.: Guidelines for authors and peer reviewers of economic submissions to the BMJ. The BMJ economic evaluation working party. BMJ 313(7052), 275–283 (1996)
Husereau, D., Drummond, M., Petrou, S., Carswell, C., Moher, D., Greenberg, D., Augustovski, F., Briggs, A.H., Mauskopf, J., Loder, E.: Consolidated Health Economic Evaluation Reporting Standards (CHEERS) statement. BMC Med. 11(1), 1–6 (2013). https://doi.org/10.1186/1741-7015-11-80
Moher, D., Liberati, A., Tetzlaff, J., Altman, D.G.: Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med. 6(7), e1000097 (2009). https://doi.org/10.1371/journal.pmed.1000097
Akhavan Hejazi, S.M., Mazlan, M., Abdullah, S.J., Engkasan, J.P.: Cost of post-stroke outpatient care in Malaysia. Singap. Med. J. 56(2), 116–119 (2015)
Gold M.R., Siegel J.E., Russell L.B., Weinstein M.C.: Estimating costs in cost-effectiveness analysis. In: Cost-effectiveness in health and medicine, pp. 176–213. Oxford University Press, New York (1996)
Beeuwkes-Buntin, M.B., Colla, C.H., Deb, P., Sood, N., Escarce, J.J.: Medicare spending and outcomes after postacute care for stroke and hip fracture. Med. Care 48(9), 776–784 (2010). https://doi.org/10.1097/MLR.0b013e3181e359df
Bjorkdahl, A., Sunnerhagen, K.S.: Process skill rather than motor skill seems to be a predictor of costs for rehabilitation after a stroke in working age; a longitudinal study with a 1 year follow up post discharge. BMC Health Serv. Res. 7, 209 (2007). https://doi.org/10.1186/1472-6963-7-209
Hayes, J., Vogel, B., Reker, D.M.: Factors associated with VHA costs of care for first 12 months after first stroke. J. Rehabilit. Res. Dev. 45(9), 1375–1384 (2008)
Kalra, L., Evans, A., Perez, I., Knapp, M., Swift, C., Donaldson, N.: A randomised controlled comparison of alternative strategies in stroke care. Health Technol. Assess. (Winchester, England) 9(18), iii–iv (2005) (1–79)
Tay-Teo, K., Moodie, M., Bernhardt, J., Thrift, A.G., Collier, J., Donnan, G., Dewey, H.: Economic evaluation alongside a phase II, multi-centre, randomised controlled trial of very early rehabilitation after stroke (AVERT). Cerebrovasc. Dis. (Basel, Switzerland). 26(5), 475–481 (2008). https://doi.org/10.1159/000155984
Forster, A., Young, J., Green, J., Patterson, C., Wanklyn, P., Smith, J., Murray, J., Wild, H., Bogle, S., Lowson, K.: Structured re-assessment system at 6 months after a disabling stroke: a randomised controlled trial with resource use and cost study. Age Ageing 38(5), 576–583 (2009). https://doi.org/10.1093/ageing/afp095
Simpson, A.N., Bonilha, H.S., Kazley, A.S., Zoller, J.S., Simpson, K.N., Ellis, C.: Impact of outpatient rehabilitation medicare reimbursement caps on utilization and cost of rehabilitation care after ischemic stroke: do caps contain costs? Arch. Phys. Med. Rehabilit. (2015). https://doi.org/10.1016/j.apmr.2015.07.008
Van Exel, J., Koopmanschap, M.A., Van Wijngaarden, J.D., Scholte Op Reimer, W.J.: Costs of stroke and stroke services: determinants of patient costs and a comparison of costs of regular care and care organised in stroke services. Cost Effect. Resour. Alloc. C/E 1(1), 2 (2003)
Godwin, K.M., Wasserman, J., Ostwald, S.K.: Cost associated with stroke: outpatient rehabilitative services and medication. Top. Stroke Rehabilit. 18 Suppl 1, 676–684 (2011). https://doi.org/10.1310/tsr18s01-676
Mahler, M.P., Zuger, K., Kaspar, K., Haefeli, A., Jenni, W., Leniger, T., Beer, J.H.: A cost analysis of the first year after stroke - early triage and inpatient rehabilitation may reduce long term costs. Swiss Med. Wkly. 138(31–32), 459–465 (2008)
Liberati, A., Altman, D.G., Tetzlaff, J., Mulrow, C., Gøtzsche, P.C., Ioannidis, J.P.A., Clarke, M., Devereaux, P.J., Kleijnen, J., Moher, D.: The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: explanation and elaboration. Ann. Intern. Med. 151(4), W-65 (2009). https://doi.org/10.7326/0003-4819-151-4-200908180-00136
Demaerschalk, B.M., Hwang, H.M., Leung, G.: US cost burden of ischemic stroke: a systematic literature review. Am. J. Manag. Care 16(7), 525–533 (2010)
Ekman, M.: Economic evidence in stroke: a review. Eur. J. Health Econ. HEPAC Health Econ. Prev. Care 5(Suppl 1), 74–83 (2004). https://doi.org/10.1007/s10198-005-0292-3
Grieve, R., Hutton, J., Bhalla, A., Rastenyte, D., Ryglewicz, D., Sarti, C., Lamassa, M., Giroud, M., Dundas, R., Wolfe, C.D.: A comparison of the costs and survival of hospital-admitted stroke patients across Europe. Stroke J. Cereb. Circ. 32(7), 1684–1691 (2001)
Everink, I.H.J., van Haastregt, J.C.M., van Hoof, S.J.M., Schols, J.M.G.A., Kempen, G.I.J.M.: Factors influencing home discharge after inpatient rehabilitation of older patients: a systematic review. BMC Geriatr. 16(1), 1–14 (2016). https://doi.org/10.1186/s12877-016-0187-4
Meijer, R., Ihnenfeldt, D.S., van Limbeek, J., Vermeulen, M., de Haan, R.J.: Prognostic factors in the subacute phase after stroke for the future residence after six months to one year. A systematic review of the literature. Clin. Rehabilit. 17(5), 512–520 (2003)
Brinjikji, W., Rabinstein, A.A., Cloft, H.J.: Hospitalization costs for acute ischemic stroke patients treated with intravenous thrombolysis in the United States are substantially higher than medicare payments. Stroke J. Cereb. Circ. 43(4), 1131–1133 (2012). https://doi.org/10.1161/strokeaha.111.636142
Claesson, L., Gosman-Hedstrom, G., Johannesson, M., Fagerberg, B., Blomstrand, C.: Resource utilization and costs of stroke unit care integrated in a care continuum: a 1-year controlled, prospective, randomized study in elderly patients: the Goteborg 70 + stroke study. Stroke J. Cereb. Circ. 31(11), 2569–2577 (2000)
Jain, M., Jain, A., Jahromi, B.S.: Strategies to improve cost-efficiency of stroke care: Stroke units and telestroke. In: Robinson, J.S., Walid, M.S., Barth, A.C.M. (eds.) Toward Healthcare Resource Stewardship. Hauppauge, New York: Nova Publishers (2012)
Saka, O., Serra, V., Samyshkin, Y., McGuire, A., Wolfe, C.C.: Cost-effectiveness of stroke unit care followed by early supported discharge. Stroke J. Cereb. Circ. 40(1), 24–29 (2009). https://doi.org/10.1161/strokeaha.108.518043
Te Ao, B.J., Brown, P.M., Feigin, V.L., Anderson, C.S.: Are stroke units cost effective? Evidence from a New Zealand stroke incidence and population-based study. Int. J. Stroke 7(8), 623–630 (2012). https://doi.org/10.1111/j.1747-4949.2011.00632.x
Miller, P., Gladman, J.R., Cunliffe, A.L., Husbands, S.L., Dewey, M.E., Harwood, R.H.: Economic analysis of an early discharge rehabilitation service for older people. Age and ageing (2005). https://doi.org/10.1093/ageing/afi058
Saka, R.O., McGuire, A., Wolfe, C.D.A.: Economic Burden of Stroke in England. University of London. https://www.nao.org.uk/wp-content/uploads/2005/11/0506452_economic_analysis.pdf (2003). Accessed 8 Aug 2016
Ghatnekar, O., Persson, U., Glader, E.L., Terent, A.: Cost of stroke in Sweden: an incidence estimate. Int. J. Technol. Assess. Health Care 20(3), 375–380 (2004)
Ghatnekar, O., Persson, U., Asplund, K., Glader, E.L.: Costs for stroke in Sweden 2009 and developments since 1997. Int. J. Technol. Assess. Health Care 30(2), 203–209 (2014). https://doi.org/10.1017/s0266462314000075
Kolominsky-Rabas, P.L., Heuschmann, P.U., Marschall, D., Emmert, M., Baltzer, N., Neundorfer, B., Schoffski, O., Krobot, K.J.: Lifetime cost of ischemic stroke in Germany: results and national projections from a population-based stroke registry: the Erlangen Stroke Project. Stroke J. Cereb. Circ. 37(5), 1179–1183 (2006). https://doi.org/10.1161/01.str.0000217450.21310.90
Gloede, T.D., Halbach, S.M., Thrift, A.G., Dewey, H.M., Pfaff, H., Cadilhac, D.A.: Long-term costs of stroke using 10-year longitudinal data from the North East Melbourne Stroke Incidence Study. Stroke J. Cereb. Circ. 45(11), 3389–3394 (2014). https://doi.org/10.1161/strokeaha.114.006200
Spieler, J.F., De Pouvourville, G., Amarenco, P.: Cost of a recurrent vs. cost of first-ever stroke over an 18-month period. Eur. J. Neurol. 10(6), 621–624 (2003)
Christensen, M.C., Morris, S.: Association between disability measures and short-term health care costs following intracerebral hemorrhage. Neurocrit. Care 9(3), 313–318 (2008). https://doi.org/10.1007/s12028-008-9124-5
Alonso-Freyre, J.L., Basanta, L., Vasquez-Roque, A., Vera-Miyar, C.R., Santos-Monzon, Y., Lopez-Hernandez, L.: Degree of independence and cost of ischaemic stroke. Revista de neurologia 32(9), 897–899 (2001)
Fearon, W.F., Shilane, D., Pijls, N.H., Boothroyd, D.B., Tonino, P.A., Barbato, E., Juni, P., De Bruyne, B., Hlatky, M.A.: Cost-effectiveness of percutaneous coronary intervention in patients with stable coronary artery disease and abnormal fractional flow reserve. Circulation. 128(12), 1335–1340 (2013). https://doi.org/10.1161/circulationaha.113.003059
Schreyer, P., Koechlin, F.: Purchasing Power Parities—Measurement and Uses. OECD Statistics Brief, No. 3, March. OECD, Paris (2002)
Swart, E.: Health care utilization research using secondary data. In: Janssen, C., Swart, E., von Lengerke, T. (eds.) Health Care Utilization in Germany: Theory, Methodology, and Results, pp. 63–86. Springer, New York (2014)
Swart, E., Ihle, P., Gothe, H., Matusiewicz, D.: Routinedaten im Gesundheitswesen. Handbuch Sekundärdatenanalyse: Grundlagen, Methoden und Perspektiven. 2. vollständig überarb. Aufl. Hans Huber, Bern (2014)
Siebert, U.: When should decision-analytic modeling be used in the economic evaluation of health care? Eur. J. Health Econ. 4(3), 143–150 (2003). https://doi.org/10.1007/s10198-003-0205-2
Siebert, U., Rochau, U., Claxton, K.: When is enough evidence enough? Using systematic decision analysis and value-of-information analysis to determine the need for further evidence. Zeitschrift fur Evidenz, Fortbildung und Qualitat im Gesundheitswesen. 107(9–10), 575–584 (2013). https://doi.org/10.1016/j.zefq.2013.10.020
Anderson, C., Rubenach, S., Mhurchu, C.N., Clark, M., Spencer, C., Winsor, A.: Home or hospital for stroke rehabilitation? Results of a randomized controlled trial: I: health outcomes at 6 months. Stroke J. Cereb. Circ. 31(5), 1024–1031 (2000)
Cadilhac, D.A., Carter, R., Thrift, A.G., Dewey, H.M.: Estimating the long-term costs of ischemic and hemorrhagic stroke for Australia: new evidence derived from the North East Melbourne Stroke Incidence Study (NEMESIS). Stroke J. Cereb. Circ. 40(3), 915–921 (2009). https://doi.org/10.1161/strokeaha.108.526905
Dewey, H.M., Thrift, A.G., Mihalopoulos, C., Carter, R., Macdonell, R.A., McNeil, J.J., Donnan, G.A.: Cost of stroke in Australia from a societal perspective: results from the North East Melbourne Stroke Incidence Study (NEMESIS). Stroke J. Cereb. Circ. 32(10), 2409–2416 (2001)
Dewey, H.M., Thrift, A.G., Mihalopoulos, C., Carter, R., Macdonell, R.A., McNeil, J.J., Donnan, G.A.: Lifetime cost of stroke subtypes in Australia: findings from the North East Melbourne Stroke Incidence Study (NEMESIS). Stroke J. Cereb. Circ. 34(10), 2502–2507 (2003). https://doi.org/10.1161/01.str.0000091395.85357.09
Spieler, J.F., Lanoe, J.L., Amarenco, P.: Costs of stroke care according to handicap levels and stroke subtypes. Cerebrovasc. Dis. (Basel, Switzerland). 17(2–3), 134–142 (2004). https://doi.org/10.1159/000075782
Abbas, S., Ihle, P., Hein, R., Schubert, I.: Rehabilitation in geriatric patients after ischemic stroke—a comparison of 2 organisational systems in Germany using claims data of a statutory health insurance fund. Die Rehabil. 52(6), 375–382 (2013). https://doi.org/10.1055/s-0033-1334914
Weimar, C., Lüngen, M., Wagner, M., Kraywinkel, K., Evers, T., Busse, O., Haberl, R.L., Laaser, U., Lauterbach, K.W., Diener, H.C.: Cost of stroke care in Germany—an analysis of the stroke data bank of the German foundation stroke-aid. Aktuelle Neurol. 29(4), 181–190 (2002). https://doi.org/10.1055/s-2002-30690
Weimar, C., Weber, C., Wagner, M., Busse, O., Haberl, R.L., Lauterbach, K.W., Diener, H.C.: Management patterns and health care use after intracerebral hemorrhage. A cost-of-illness study from a societal perspective in Germany. Cerebrovasc. Dis. (Basel, Switzerland). 15(1–2), 29–36 (2003)
Fattore, G., Torbica, A., Susi, A., Giovanni, A., Benelli, G., Gozzo, M., Toso, V.: The social and economic burden of stroke survivors in Italy: a prospective, incidence-based, multi-centre cost of illness study. BMC Neurol. 12, 137 (2012). https://doi.org/10.1186/1471-2377-12-137
Gerzeli, S., Tarricone, R., Zolo, P., Colangelo, I., Busca, M.R., Gandolfo, C.: The economic burden of stroke in Italy. The EcLIPSE Study: Economic Longitudinal Incidence-based Project for Stroke Evaluation. Neurol. Sci. 26(2), 72–80 (2005). https://doi.org/10.1007/s10072-005-0439-0
Torbica, A., Calciolari, S., Fattore, G.: Does informal care impact utilization of healthcare services? Evidence from a longitudinal study of stroke patients. Soc. Sci. Med. 1982(124), 29–38 (2015). https://doi.org/10.1016/j.socscimed.2014.11.005
van Eeden, M., van Heugten, C., van Mastrigt, G.A., van Mierlo, M., Visser-Meily, J.M., Evers, S.M.: The burden of stroke in the Netherlands: estimating quality of life and costs for 1 year poststroke. BMJ Open. 5(11), e008220 (2015). https://doi.org/10.1136/bmjopen-2015-008220
Andersson, A., Levin, L.A., Oberg, B., Mansson, L.: Health care and social welfare costs in home-based and hospital-based rehabilitation after stroke. Scand. J. Caring Sci. 16(4), 386–392 (2002)
Claesson, L., Linden, T., Skoog, I., Blomstrand, C.: Cognitive impairment after stroke—impact on activities of daily living and costs of care for elderly people. The Goteborg 70+ Stroke Study. Cerebrovasc. Dis. (Basel, Switzerland). 19(2), 102–109 (2005). https://doi.org/10.1159/000082787
von Koch, L., de Pedro-Cuesta, J., Kostulas, V., Almazan, J., Widen Holmqvist, L.: Randomized controlled trial of rehabilitation at home after stroke: one-year follow-up of patient outcome, resource use and cost. Cerebrovasc. Dis. (Basel, Switzerland). 12(2), 131–138 (2001)
Roderick, P., Low, J., Day, R., Peasgood, T., Mullee, M.A., Turnbull, J.C., Villar, T., Raftery, J.: Stroke rehabilitation after hospital discharge: a randomized trial comparing domiciliary and day-hospital care. Age Ageing. 30(4), 303–310 (2001)
Fjaertoft, H., Indredavik, B., Magnussen, J., Johnsen, R.: Early supported discharge for stroke patients improves clinical outcome. Does it also reduce use of health services and costs? One-year follow-up of a randomized controlled trial. Cerebrovasc. Dis. (Basel, Switzerland). 19(6), 376–383 (2005). https://doi.org/10.1159/000085543
Rasmussen, R.S., Ostergaard, A., Kjaer, P., Skerris, A., Skou, C., Christoffersen, J., Seest, L.S., Poulsen, M.B., Ronholt, F., Overgaard, K.: Stroke rehabilitation at home before and after discharge reduced disability and improved quality of life: A randomised controlled trial. Clin. Rehabil. (2015). https://doi.org/10.1177/0269215515575165
Teng, J., Mayo, N.E., Latimer, E., Hanley, J.: Wood-Dauphinee S, Cote R, Scott S. Costs and caregiver consequences of early supported discharge for stroke patients. Stroke J. Cereb. Circ. 34(2), 528–536 (2003)
Funding
This work was supported by the Erasmus-Western Balkans mobility programme (ERAWEB), a project funded by the European Commission. The funding source had no influence on study design, analysis and interpretation of data, in the writing of the manuscript and the decision to submit the manuscript for publication.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethical Committee
This work was approved by the Research Committee for Scientific and Ethical Questions (RCSEQ), University for Health Sciences, Medical Informatics and Technology (UMIT), Hall in Tirol, Austria (Date: April 26, 2016; reference number: 1697).
Conflict of interest
The authors declare that they have no conflict of interest.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Appendices
Appendix 1: Evidence tables
Appendix 2
See Table 4.
Appendix 3
Rights and permissions
About this article
Cite this article
Rajsic, S., Gothe, H., Borba, H.H. et al. Economic burden of stroke: a systematic review on post-stroke care. Eur J Health Econ 20, 107–134 (2019). https://doi.org/10.1007/s10198-018-0984-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10198-018-0984-0