Abstract
Objectives
The economic crisis in Europe might have limited access to some innovative technologies implying an increase of waiting time. The purpose of the study is to evaluate the impact of waiting time on the costs and benefits of transcatheter aortic valve replacement (TAVR) for the treatment of severe aortic stenosis.
Methods
This is a cost-utility analysis from the perspective of the Spanish National Health Service. Results of two prospective hospital registries (158 and 273 consecutive patients) were incorporated into a probabilistic Markov model to compare quality adjusted life years (QALYs) and costs for TAVR after waiting for 3–12 months, relative to immediate TAVR. We simulated a cohort of 1000 patients, male, and 80 years old; other patient profiles were assessed in sensitivity analyses.
Results
As waiting time increased, costs decreased at the expense of lower survival and loss of QALYs, leading to incremental cost-effectiveness ratios for eliminating waiting lists of about 12,500 € per QALY. In subgroup analyses prioritization of patients for whom higher benefit was expected led to a smaller loss of QALYs. Concerning budget impact, long waiting lists reduced spending considerably and permanently.
Conclusions
A shorter waiting time is likely to be cost-effective (considering commonly accepted willingness-to-pay thresholds in Europe) relative to 3 months or longer waiting periods. If waiting lists are nevertheless seen as unavoidable due to severe but temporary budgetary restrictions, prioritizing patients for whom higher benefit is expected appears to be a way of postponing spending without utterly sacrificing patients’ survival and quality of life.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Growing demand alongside rising costs is a major concern for public funding of medical innovations, especially in times of crisis. Resource constraints may limit access to certain expensive but effective treatments, which might lead to an important loss in quality of life and even to higher mortality. Since the beginning of the economic crisis in Spain, waiting times for some elective interventions have started rising again after years of stable trends [1,2,3]. In this context, assessing the cost-effectiveness of longer against shorter waiting times for different indications can shed light on the clinical and economic consequences of restricting access to expensive interventions and might provide useful information to decision makers.
The case of transcatheter aortic valve replacement (TAVR) for the treatment of aortic stenosis (AS) is specially challenging. AS is an increasingly prevalent cause of morbidity and mortality in the elderly [4,5,6,7]. Surgical replacement of the aortic valve is the standard treatment [8] for aortic stenosis but TAVR is a cost-effective option for inoperable or high risk patients [9, 10].
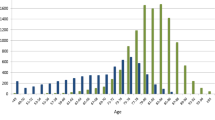
TAVR was introduced in Europe in 2008 and, although adoption trends in Spain seemed to flatten between 2008 and 2012 in comparison with other European countries [11], its use has doubled since 2012 [12,13,14]. According to the last available update of the Spanish Registry [12], TAVR procedures increased from 845 in 2012 to 1586 in 2015. Osnabrugge and colleagues [15] gave an estimate of 17,712 (95% CI: 7590–32,691) new TAVR candidates each year in a group of 19 European countries; it should be observed that their estimate was performed before the publication of new TAVR guidelines [16] which expand the indications to the intermediate risk population [17, 18]. Thus, an even steeper increase in demand is to be expected in the coming years.
The high rate of adverse events in patients on the waiting list for TAVR observed in a previous study [9] and our own clinical experience, led us to perform this analysis. Our main objective was to evaluate the efficiency of restricting access to TAVR if that implies a waiting list. Specifically, we aimed to evaluate: (1) the clinical consequences of having to wait for TAVR and; (2) whether the potential economic savings compensate the losses in effectiveness.
Methods
Model overview
We used a Markov model to trace patients with severe AS from the moment of indication for TAVR until death in 3-month cycles. We compared costs, survival, and health-related quality of life associated with immediate TAVR (waiting for less than 3 months) vs waiting for 3, 6, 9, or 12 months.
We simulated a cohort of 1000 patients, male, and 80 years old. The primary outcome was established as the costs avoided per quality-adjusted life year (QALY) lost due to waiting for TAVR or, alternatively, the incremental cost-effectiveness ratio (ICER) of eliminating waiting lists.
Figure 1 provides an overview of the model. Patients with indication for TAVR may enter the state of waiting for intervention or receive immediate TAVR. Patients entering the waiting state remain there for one to four cycles. In the waiting state patients are at higher risk of suffering AS related complications (including death) that result in hospitalization or emergency visits, and may undergo valvuloplasty. Patients who survive after TAVR enter the post-TAVR state where they remain until death and may require hospitalization or emergency visits.
Data sources
We estimated utilities, costs and transition probabilities from two prospective observational studies with data collection before and after receiving TAVR.
We estimated utilities and costs incurred in the different health states from the TEVAS study. The cohort has been described elsewhere [9]. Briefly, it consisted of 147 consecutive patients receiving TAVR through transfemoral access in six Spanish hospitals (between October 2011 and July 2013), with mean age of 81 and mean EuroScore of 14.5 (SD: 9.7). Of these, 145 were centrally interviewed by phone to assess EQ-5D-3L and resource consumption at 1, 3, 6, and 12 months; and 58 were interviewed while they were on the waiting list. Resource consumption during index hospitalization was collected at each centre by the local investigators; after discharge, resource use was collected through a patient logbook. In case of admission before or after the intervention, clinical records were centrally checked to collect resource consumption.
Transition and event probabilities were estimated from 237 consecutive patients attending the coordinating centre (the “VH cohort”) between 2008 and 2014. One hundred and fifty-two out of 237 patients with indication for TAVR eventually received it, 42 were still waiting by the end of 2014, and 43 died while waiting (31 due to cardiovascular causes). See the Online Supplementary material for a description of the VH cohort: Online Supplementary Table 1 shows baseline characteristics by waiting time for patients who received TAVR. The proportion of patients waiting for up to 3, 3–6, 6–9, 9–12, or > 12 months, was 17, 24, 18, 11, and 30%, respectively. Online Supplementary Figure 1 shows survival curves during waiting time and after TAVR.
Hospitalizations and emergency room visits were prospectively collected by a member of the “heart team” attending patients with AS. The date at which the “heart team” considered that the patient met the criteria for TAVR indication following standard international guidelines [19], was taken as the initial point for computing waiting time.
Model parameters
Table 1 shows the estimates for utility penalties and costs. We derived utilities from the EQ-5D-3L generic quality of life instrument [20]. Observations in the TEVAS study were stratified by the health states and events distinguished in the model (descriptive statistics of EQ-5D-3L scores and monthly costs used to estimate the model parameters can be found in Online Supplementary Table 2). To estimate the utility penalties due to waiting and due to complications before or after TAVR, we calculated differences in mean EQ-5D-3L utility values before and after TAVR for patients with and without complications. In each 3-month cycle patients remained in the waiting state and/or experienced complications, these utility penalties were subtracted from the reference EQ index values for the Spanish general population of the same age and sex [21]. Following expert opinion (which was in accordance with our data), patients were assumed to return after TAVR to utility levels equal to those of the Spanish general population of the same sex and age. Expert opinion was gathered from a clinical cardiologist attending patients with AS (IF), a clinical cardiologist attending AS patients who were candidates for intervention (VS), an interventional cardiologist (BGB) and a methodologist with experience in quality of life assessment (AR), in several meetings prior the start of data collection.
Costs were determined from the perspective of the Spanish health services. Unit costs (expressed in euros for 2012) were primarily obtained from cost accounting records of the coordinating centre; costs of medical attention outside the hospital were based on reimbursement tariffs. Table 2 lists all resource items and unit costs used.
Mortality before and after TAVR was based on Spanish life tables, corrected for the excess risk observed in the VH cohort relative to the general population of the same age and sex. For the base case analysis the excess risk was assumed to be additive.
Table 1 summarizes the transition and event probabilities. Event rates estimated in the VH cohort (which are shown in Online Supplementary Table 3) were converted into probabilities [22]. Changes in parameters to fit the specific subgroups defined further are also listed in Table 1.
A discount rate of 3% per year was applied to adjust future costs and benefits.
Sensitivity analysis
Probabilistic (PSA), one-way sensitivity, and scenario analyses were conducted to assess sampling and parameter uncertainty. PSA was performed using Monte Carlo simulation (1000 iterations), assuming the distributions shown in Table 1. The simulation results were plotted on a cost-effectiveness plane and a cost-effectiveness acceptability curve was calculated showing the probability of waiting for TAVR being more cost-effective than immediate intervention as a function of the willingness to pay for a QALY.
In one-way sensitivity analyses, parameters were varied ± 25% of their base-case values. The scenario analyses assessed alternative assumptions regarding sex and age, excess mortality post TAVR (multiplicative instead of additive mortality risk vs the general population), and discount rate (0 and 5%).
In order to estimate outcomes for certain subgroups of patients who might benefit particularly from shorter waiting times, we defined three patient profiles by changing some of the base-case parameters (as shown in Table 1):
- Subgroup 1.:
-
Patients experiencing acute decompensation of heart failure or syncope were assumed a much higher probability of hospitalization prior to TAVR.
- Subgroup 2.:
-
Patients with marked progression of symptoms were assumed a higher probability of hospitalization prior to TAVR, a more severely impaired quality of life and a smaller further decline in quality of life due to complications while waiting.
- Subgroup 3.:
-
Patients with absolute contraindication for surgery for anatomic reasons or calcified aorta without other comorbidities, were assumed to have a mortality risk closer to that of the general population of the same age and sex after TAVR.
Results
Base-case model results
The main study results are shown in Table 3. The longer patients have to wait, the more of them die before TAVR, and consequently the fewer devices are implanted. On the other hand, the increasing number of patients suffering from complications while waiting leads to additional resource consumption due to hospitalizations, emergency visits, and valvuloplasties. Altogether, net cost savings are achieved, but at considerable loss of life expectancy and QALYs. Incremental cost-effectiveness is estimated at approximately 12,500 € per QALY lost. Regarding budget impact, however, postponing TAVR can have a very big temporary effect in the year when the decision is adopted; this impact is largely, but not completely, reversed in following periods, thus leading to a permanent reduction in spending (Fig. 2).
Sensitivity analysis
We present sensitivity analysis results for a waiting time of 12 months, but similar results were obtained for the other waiting times.
Figure 3 shows the distribution of incremental costs and QALYs in the cost-effectiveness plane after bootstrap resampling. Since cost savings are closely related to interventions avoided due to mortality before TAVR, there is a strong correlation between cost savings and QALYs lost. The ICER variability falls mostly between the 10,000 and 20,000 €/QALY boundaries, and the probability that waiting vs immediate TAVR is cost-effective at a willingness to pay threshold of 20,000 €/QALY is less than 10% (see Fig. 4 for the complete cost-effectiveness acceptability curve).
In one-way sensitivity analyses (Fig. 5), model estimates were most sensitive to changes in the cost of the TAVR device and the post-TAVR excess mortality relative to the general population.
ICER results obtained depending on patients’ sex and age are shown in Fig. 6. Panel A shows results under the assumption that excess risk is additive, i.e., that the mortality rate after TAVR is 1.5% points higher than that of the age- and sex-adjusted general population, and panel B shows ICER results assuming that excess risk is multiplicative, i.e., that mortality is 2.0 times higher than that of the age- and sex-adjusted general population.
Table 4 compares findings for a waiting time of 12 months under different scenarios. Online supplementary Table 4 shows results for the other waiting times. Age (or equivalently, life expectancy after TAVR) has an important impact on model outcomes. Marked differences are also found between particular subgroups of patients. When patients require hospitalization before TAVR because of aortic stenosis related complications (subgroup 1), costs incurred during waiting time exceed the costs avoided due to mortality. For patients with marked progression of symptoms (subgroup 2), higher benefits are achieved in terms of quality of life after TAVR, while savings from waiting are close to zero. For patients with contraindications for surgery only for anatomical reasons or calcified aorta (subgroup 3) the resulting ICER is closer to that seen for the base case. Savings are somewhat higher but, because patients have a greater life expectancy after TAVR, health gains with immediate treatment are higher too.
Discussion
It has been argued in the health economics literature that letting patients wait for medical interventions can be economically efficient because it avoids idle capacity and might deter patients from treatment, thus reducing costs [23]. On the other hand, waiting can have negative consequences on effectiveness, which in turn may also have an impact on costs. In empirical research, these arguments in favour of waiting lists have shown to hold true only for very short waiting times or interventions with relatively little benefit [23]. In practice, the formation of waiting lists is usually not explained by hospital managers or head clinician as a desire to match supply and demand or to optimise operational efficiency, but is more typically justified with reference to externally imposed limitations, particularly financial restrictions and budget cutbacks. The reduction of a particular hospital activity will only have an immediate effect on spending, however, if it is possible to stop paying for the required resources relatively quickly. As opposed to activities that mostly use fixed resources (i.e., in-house MRI equipment or permanent staff), interventions that require expensive devices that have to be purchased for each patient (as is the case for TAVR) are therefore logical first candidates for restrictions.
We analysed whether, apart from being a logical first candidate, TAVR is also a good candidate for restricted use, if that implies a waiting list. Our findings indicate that, under the modelled assumptions, waiting lists for TAVR have an immediate alleviating impact on hospital budgets, which in the short term can be considerable. However, the achieved cost savings are essentially due to a steep increase in patient mortality leading, together with strongly diminished quality of life during waiting time, to a situation in which so many QALYs are lost that it appears difficult to sustain the argument that restricting access to the technology is economically efficient or ethically unproblematic. Stating this conclusion inversely, the elimination of waiting lists for TAVR appears to be a relatively cheap way to extend life expectancy and achieve additional QALYs in patients with severe AS. This is especially true for patients for whom a greater benefit of treatment is expected because of clinical condition or age.
Whether TAVR is a bad candidate for usage restrictions also depends on the (in)efficiency of alternative courses of action available to hospital management, that is, whether measures restricting other hospital activities with a similar budget impact would lead to more or to fewer QALYs lost per euro saved than the ICER found for waiting for TAVR. Our research does not say anything about the expected outcomes of alternative courses of action, and some caution is therefore warranted. In any case, in the context of an economic crisis in which restrictions and disinvestment seem to play an increasingly prominent role, the (empirical) determination of costs avoided per QALY lost (as the mirror image of costs incurred per QALY gained) should become more common than it currently is.
A related question is whether the willingness to give up QALYs for a given amount of money saved is symmetric to the willingness to pay the same amount for a QALY gained. The answer might appear obvious from a rational perspective, but due to behavioural habits or psychological prejudice, decision makers might be more reluctant to increase investment than to reduce savings [24]. However, even considering that the threshold required for savings might be empirically lower than the threshold for incremental spending, our results are well below the opportunity cost of 20,000–25,000 € per QALY recently estimated from budget allocations observed in the Spanish setting [25].
Our results are clearly of concern for decision makers but the notion of efficiency should also be of concern for clinicians in their clinical practice. In the presence of unavoidable waiting lists clinicians tend to adopt prioritization criteria favouring more severe patients or those who are expected to benefit more from treatment. Our subgroup analyses indicate that prioritization criteria based on implicit clinical judgement can also be meaningful in terms of economic efficiency; prioritizing the right patients increases the overall number of QALYs gained for a given budget. Refining indication criteria to decide the optimal therapy for a given patient (TAVR vs open surgery vs medical treatment) and establishing explicit prioritization criteria when waiting lists are unavoidable is of paramount importance. Our findings support the use of economic evaluation as a tool for establishing formal prioritization strategies that maximize health benefits given limited health care resources [26].
The results of the sensitivity analyses deserve further attention. The impact of waiting for TAVR was found to be affected most by: (1) the price of the TAVR device, which is a constant in our model, but can vary between different hospitals and countries due to pricing strategies; and (2) the excess mortality after TAVR compared to the general population of the same age and sex—the higher the excess mortality after TAVR, the lower the QALY gain from eliminating the waiting list is. The latter is in accordance with cost-effectiveness results of TAVR vs medical treatment which have been shown to be highly dependent on life expectancy after TAVR [27]. Moreover, according to current clinical guidelines [19], patients with poor life expectancy have no indication for TAVR, thus they should not be admitted to the waiting list.
The parameter values used in our model were based on two “real data” cohorts. Although this is clearly a strength of the study, it might also be seen as a limitation in certain aspects. First, sample size for the estimation of some parameters was limited for some subgroups of patients; especially for the estimation of costs and utilities for patients on the waiting list and for patients with complications. However, according to the one-way sensitivity analyses, a variation of ± 25% in these parameters would have very little impact on the model estimates. Second, the observed waiting list was managed with prioritization based on clinical judgement and not with a first-in first-out criterion (which would have led to an equally distributed waiting time among patients with different degrees of severity). Moreover, bias could be avoided by randomising patients to shorter or longer waiting times, but this is hardly feasible, and ethically unacceptable, when dealing with a highly lethal and limiting disease such as severe AS. To estimate parameter values from an exhaustive literature review was not an option either, because published data on TAVR registries do not include events occurring between the indication and the intervention. Another potential weakness of our study is that the Markov model might be considered too simple to explain such a complex phenomenon as the formation of waiting lists. We could have included several additional health states and transitions or used more sophisticated techniques, like discrete event simulation [28, 29], but since the main effects are driven by simple facts, we believe that a more complex model would have led to a roughly equivalent result. In any case, further research to develop similar or perhaps more specific methods for this purpose would be desirable, given the progressively rising costs of new technologies and thus predictably increasing restrictions on access to them in the future.
Koopmanschap and colleagues illustrated that the impact of waiting on the cost-effectiveness of one technology versus another is very scenario dependent and may be substantial, especially if health loss while waiting is partly or completely non-reversible (as is the case of the TAVR waiting list, as death accounts for the main health losses) [30]. However, our study investigated the impact of different waiting times for patients for whom open surgery is not an option. Therefore, we did not compare one technological alternative to another. This also leaves for future research the question of whether TAVR is still cost-effective when having to wait for it, in patients for whom open surgery is clinically feasible but not cost-effective in the absence of waiting lists.
The impact of waiting time on the cost-effectiveness of technological innovations has been scarcely evaluated [23, 30,31,32,33]. Taking the case of TAVR as an example, we have shown how classical cost-effectiveness methodology can be articulated to estimate the effects of a waiting list on health losses, cost savings, and budget impact. We have thus explained a phenomenon that might be generalized to other medical technologies which share common features with TAVR (subject to constraints due to growing demand and high cost, and marked alleviation of symptoms and improved expected survival when appropriately indicated). Indeed, it appears that for any cost-effective technology that saves lives but adds costs, delaying its use will temporally alleviate budgets but cannot possibly be cost-effective.
Conclusion
In conclusion, when making the decision to incorporate (or to continue offering) a costly but effective technology (like TAVR) in a context of limited resources, decision makers should consider and decide upon the savings that would compensate a QALY that will probably be lost due to waiting for treatment. In the case of TAVR, the savings per QALY lost due to waiting are substantially below the willingness to pay thresholds commonly accepted to gain a QALY, suggesting that avoiding or eliminating waiting lists would be a cost-effective choice.
References
Morgan, D., Astoli, R.: Health spending growth at zero: whichcountries, which sectors are most affected?, OECD Health Working Papers, No. 60, OECD Publishing, Paris (2013). http://dx.doi.org/10.1787/5k4dd1st95xv-en
Siciliani, L., Moran, V., Michael, Borowitz: Measuring and comparing health care waiting times in OECD countries. Health Policy (New York) 118, 292–303 (2014)
Departament de Salut: CatSalut. Servei Català de la Salut. http://catsalut.gencat.cat/ca/ciutadania/serveis-atencio-salut/com-accedeix/llistes-espera/operacions-quirurgiques/consulta/. Accessed 21 Nov 2017
Eveborn, G.W., Schirmer, H., Heggelund, G., Lunde, P., Rasmussen, K.: The evolving epidemiology of valvular aortic stenosis. The Tromsø Study. Heart 99, 396–400 (2013)
Lindroos, M., Kupari, M., Heikkilä, J., Tilvis, R.: Prevalence of aortic valve abnormalities in the elderly: an echocardiographic study of a random population sample. J. Am. Coll. Cardiol. 21, 1220–1225 (1993)
Nkomo, V.T., Gardin, J.M., Skelton, T.N., Gottdiener, J.S., Scott, C.G., Enriquez-Sarano, M.: Burden of valvular heart diseases: a population-based study. Lancet 368, 1005–1011 (2006)
Ferreira-González, I., Pinar-Sopena, J., Ribera, A., Marsal, J.R., Cascant, P., González-Alujas, T., Evangelista, A., Brotons, C., Moral, I., Permanyer-Miralda, G., García-Dorado, D., Tornos, P.: Prevalence of calcific aortic valve disease in the elderly and associated risk factors: a population-based study in a Mediterranean area. Eur. J. Prev. Cardiol. 20, 1022–1030 (2013)
Rosenhek, R., Zilberszac, R., Schemper, M., Czerny, M., Mundigler, G., Graf, S., Bergler-Klein, J., Grimm, M., Gabriel, H., Maurer, G.: Natural history of very severe aortic stenosis. Circulation 121, 151–156 (2010)
Ribera, A., Slof, J., Andrea, R., Falces, C., Gutiérrez, E., Del Valle-Fernández, R., Morís-De La Tassa, C., Mota, P., Oteo, J.F., Cascant, P., Altisent, O.A.J., Sureda, C., Serra, V., García-Del Blanco, B., Tornos, P., Garcia-Dorado, D., Ferreira-González, I.: Transfemoral transcatheter aortic valve replacement compared with surgical replacement in patients with severe aortic stenosis and comparable risk: cost-utility and its determinants. Int. J. Cardiol. 182, 321–328 (2015)
Indraratna, P., Ang, S.C., Gada, H., Yan, T.D., Manganas, C., Bannon, P., Cao, C.: Systematic review of the cost-effectiveness of transcatheter aortic valve implantation. J. Thorac. Cardiovasc. Surg. 148, 509–514 (2014)
Mylotte, D., Osnabrugge, R.L.J., Windecker, S., Lefèvre, T., de Jaegere, P., Jeger, R., Wenaweser, P., Maisano, F., Moat, N., Søndergaard, L., Bosmans, J., Teles, R.C., Martucci, G., Manoharan, G., Garcia, E., Van Mieghem, N.M., Kappetein, A.P., Serruys, P.W., Lange, R., Piazza, N.: Transcatheter aortic valve replacement in Europe: adoption trends and factors influencing device utilization. J. Am. Coll. Cardiol. 62, 210–219 (2013)
Jiménez-Quevedo, P., Serrador, A., Pérez de Prado, A., Pan, M.: Registro Español de Hemodinámica y Cardiología Intervencionista. XXV Informe Oficial de la Sección de Hemodinámica y Cardiología Intervencionista de la Sociedad Española de Cardiología (1990–2015). Rev. Española Cardiol. 69, 1180–1189 (2016)
Salinas, P., Moreno, R., Calvo, L., Sánchez-Recalde, Á., Jiménez-Valero, S., Galeote, G., López-Fernández, T., Ramírez, U., Riera, L., Plaza, I., Moreno, I., Mesa, J.M., López-Sendón, J.L.: Long-term follow-up after transcatheter aortic valve implantation for severe aortic stenosis. Rev. Española Cardiol. 69, 37–44 (2016)
Avanzas, P., Pascual, I., Muñoz-García, A.J., Segura, J., Alonso-Briales, J.H., Suárez de Lezo, J., Pan, M., Jiménez-Navarro, M.F., López-Aguilera, J., Hernández-García, J.M., Morís, C.: Long-term follow-up of patients with severe aortic stenosis treated with a self-expanding prosthesis. Rev. Española Cardiol. 70, 247–253 (2016)
Osnabrugge, R.L.J., Mylotte, D., Head, S.J., Van Mieghem, N.M., Nkomo, V.T., Lereun, C.M., Bogers, A.J.J.C., Piazza, N., Kappetein, P.: Aortic stenosis in the elderly: disease prevalence and number of candidates for transcatheter aortic valve replacement: a meta-analysis and modeling study. J. Am. Coll. Cardiol. 62, 1002–1012 (2013)
Baumgartner, H., Falk, V., Bax, J.J., De Bonis, M., Hamm, C., Holm, P.J., Iung, B., Lancellotti, P., Lansac, E., Muñoz, D.R., Rosenhek, R., Sjögren, J., Tornos Mas, P., Vahanian, A., Walther, T., Wendler, O., Windecker, S., Zamorano, J.L.: 2017 ESC/EACTS guidelines for the management of valvular heart disease. Eur. Heart J. 38, 2739–2791 (2017)
Leon, M.B., Smith, C.R., Mack, M.J., Makkar, R.R., Svensson, L.G., Kodali, S.K., Thourani, V.H., Tuzcu, E.M., Miller, D.C., Herrmann, H.C., Doshi, D., Cohen, D.J., Pichard, A.D., Kapadia, S., Dewey, T., Babaliaros, V., Szeto, W.Y., Williams, M.R., Kereiakes, D., Zajarias, A., Greason, K.L., Whisenant, B.K., Hodson, R.W., Moses, J.W., Trento, A., Brown, D.L., Fearon, W.F., Pibarot, P., Hahn, R.T., Jaber, W.A., Anderson, W.N., Alu, M.C., Webb, J.G.: PARTNER 2 investigators: transcatheter or surgical aortic-valve replacement in intermediate-risk patients. N. Engl. J. Med. 374, 1609–1620 (2016)
Reardon, M.J., Van Mieghem, N.M., Popma, J.J., Kleiman, N.S., Søndergaard, L., Mumtaz, M., Adams, D.H., Deeb, G.M., Maini, B., Gada, H., Chetcuti, S., Gleason, T., Heiser, J., Lange, R., Merhi, W., Oh, J.K., Olsen, P.S., Piazza, N., Williams, M., Windecker, S., Yakubov, S.J., Grube, E., Makkar, R., Lee, J.S., Conte, J., Vang, E., Nguyen, H., Chang, Y., Mugglin, A.S., Serruys, P.W.J.C., Kappetein, A.P.: SURTAVI investigators: surgical or transcatheter aortic-valve replacement in intermediate-risk patients. N. Engl. J. Med. 376, 1321–1331 (2017)
Vahanian, A., Alfieri, O., Andreotti, F., Antunes, M.J., Barón-Esquivias, G., Baumgartner, H., Borger, M.A., Carrel, T.P., De Bonis, M., Evangelista, A., Falk, V., Lung, B., Lancellotti, P., Pierard, L., Price, S., Schäfers, H.-J., Schuler, G., Stepinska, J., Swedberg, K., Takkenberg, J., Von Oppell, U.O., Windecker, S., Zamorano, J.L., Zembala, M.: Guidelines on the management of valvular heart disease (version 2012): the Joint Task Force on the Management of Valvular Heart Disease of the European Society of Cardiology (ESC) and the European Association for Cardio-Thoracic Surgery (EACTS). Eur. J. Cardiothorac. Surg. 42, S1–S44 (2012)
Ramos-Goni, J.M., Rivero-Arias, O.: eq5d: a command to calculate index values for the EQ-5D quality-of-life instrument. Stata J. 11, 120–125 (2011)
Ministerio de Sanidad, Servicios Sociales e Igualdad. Instituto Nacional de Estadística. Encuesta Nacional de Salud. España 2011/12. Ministerio de Sanidad, Servicios Sociales e Igualdad, Madrid, 2013. http://www.msssi.gob.es/estadEstudios/estadisticas/sisInfSanSNS/nivelSalud.htm. Accessed 21 Nov 2017
Briggs, A., Sculpher, M.: An introduction to Markov modelling for economic evaluation. Pharmacoeconomics 13, 397–409 (1998)
Siciliani, L., Stanciole, A., Jacobs, R.: Do waiting times reduce hospital costs? J. Health Econ. 28, 771–780 (2009)
Kahneman, D., Tversky, A.: Prospect theory: an analysis of decision under risk. Econometrica 47, 263–291 (1979)
Vallejo-Torres, L., García-Lorenzo, B., Castilla, I., Valcárcel Nazco, C., García-Pérez, L., Linertová, R., Serrano-Aguilar, P.: Valor Monetario de un AVAC: Estimación empírica del coste de oportunidad en el Sistema Nacional de Salud, Ministerio de Sanidad, Servicios Sociales e Igualdad. Servicio de Evaluación del Servicio Canario de la Salud; 2015. Informes de Evaluación de Tecnologías Sanitarias. http://www3.gobiernodecanarias.org/sanidad/scs/contenidoGenerico.jsp?idDocument=e690e0c1-cbed-11e5-a9c5-a398589805dc&idCarpeta=993a9b1d-7aed-11e4-a62a-758e414b4260. Accessed 21 Nov 2017
Henriksson, M., Palmer, S., Chen, R., Damant, J., Fitzpatrick, N.K., Abrams, K., Hingorani, A.D., Stenestrand, U., Janzon, M., Feder, G., Keogh, B., Shipley, M.J., Kaski, J.-C., Timmis, A., Sculpher, M., Hemingway, H.: Assessing the cost effectiveness of using prognostic biomarkers with decision models: case study in prioritising patients waiting for coronary artery surgery. BMJ 340, b5606 (2010)
Watt, M., Mealing, S., Eaton, J., Piazza, N., Moat, N., Brasseur, P., Palmer, S., Busca, R., Sculpher, M.: Cost-effectiveness of transcatheter aortic valve replacement in patients ineligible for conventional aortic valve replacement. Heart 98, 370–376 (2012)
Jahn, B., Pfeiffer, K.P., Theurl, E., Tarride, J.E., Goeree, R.: Capacity constraints and cost-effectiveness: a discrete event simulation for drug-eluting stents. Med. Decis. Making 30, 16–28 (2010)
Comas, M., Castells, X., Hoffmeister, L., Román, R., Cots, F., Mar, J., Gutiérrez-Moreno, S., Espallargues, M.: Discrete-event simulation applied to analysis of waiting lists. Evaluation of a prioritization system for cataract surgery. Value Health 11, 1203–1213 (2008)
Koopmanschap, M., Brouwer, W.B.F., Hakkaart-Van Roijen, L., Van Exel, N.J.: Influence of waiting time on cost-effectiveness. Soc. Sci. Med. 60, 2501–2504 (2005)
Tuominen, U., Sintonen, H., Hirvonen, J., Seitsalo, S., Paavolainen, P., Lehto, M., Hietaniemi, K., Blom, M.: Is longer waiting time for total knee replacement associated with health outcomes and medication costs? Randomized clinical trial. Value Health 13, 998–1004 (2010)
Tuominen, U., Sintonen, H., Aronen, P., Hirvonen, J., Seitsalo, S., Lehto, M., Hietaniemi, K., Blom, M.: Cost-utility of waiting time in total joint replacements: a randomized clinical trial. Int. J. Technol. Assess. Health Care 29, 27–34 (2013)
Chauvin, P., Josselin, J.-M., Heresbach, D.: The influence of waiting times on cost-effectiveness: a case study of colorectal cancer mass screening. Eur. J. Health Econ. 15, 801–812 (2014)
Acknowledgements
Mar Vila and Joan Sagarra provided costs from the cost accounting records at University Hospital Vall d’Hebron and Hospital Clínic. Josep Ramon Marsal provided statistical advice. Teresa Fernández provided administrative support. Gaietà Permanyer-Miralda and Joan MV Pons contributed to the article drafting and revision. Manuel Castellà, Joaquim Cevallos, Manel Sabaté, Gerald Lébano, Lucía Fernández, Isabel González, and Carolina Álvaro contributed to data collection.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Funding
Financial support for this study was provided in part by a grant from Instituto de Investigación Carlos III (FIS). The Spanish Ministry of Economy and Competitiveness (Reference number: PI10/00369) and CIBERESP. The funding agreement ensured the authors’ independence in designing the study, interpreting the data, writing, and publishing this report.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Ribera, A., Slof, J., Ferreira-González, I. et al. The impact of waiting for intervention on costs and effectiveness: the case of transcatheter aortic valve replacement. Eur J Health Econ 19, 945–956 (2018). https://doi.org/10.1007/s10198-017-0941-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10198-017-0941-3