Abstract
Introduction
Diabetes mellitus is a chronic degenerative disease associated with a high risk of chronic complications and comorbidities. However, very few data are available on the associated cost. The objective of this study is to identify the available information on the epidemiology of the disease and estimate the average annual cost incurred by the National Health Service and Society for the Treatment of Diabetes in Italy.
Methods
A probabilistic prevalence cost of illness model was developed to calculate an aggregate measure of the economic burden associated with the disease, in terms of direct medical costs (drugs, hospitalizations, monitoring and adverse events) and indirect costs (absenteeism and early retirement). A systematic review of the literature was conducted to determine both the epidemiological and economic data. Furthermore, a one-way and probabilistic sensitivity analysis with 5,000 Monte Carlo simulations was performed to test the robustness of the results and define a 95 % CI.
Results
The model estimated a prevalence of 2.6 million patients under drug therapies in Italy. The total economic burden of diabetic patients in Italy amounted to €20.3 billion/year (95 % CI €18.61 to €22.29 billion), 54 % of which are associated with indirect costs (95 % CI €10.10 to €11.62 billion) and 46 % with direct costs only (95 % CI €8.11 to €11.06 billion).
Conclusions
This is the first study conducted in Italy aimed at estimating the direct and indirect cost of diabetes with a probabilistic prevalence approach. As might be expected, the lack of information means that the real burden of diabetes is partly underestimated, especially with regard to indirect costs. However, this is a useful approach for policy makers to understand the economic implications of diabetes treatment in Italy.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Diabetes mellitus (DM) is a chronic degenerative disease associated with a high risk of chronic complications and comorbidities, with a significant impact on both life expectancy and quality of life [1]. It is well established that DM-related complications involve debilitating consequences, affecting the functioning of vital organs, which may cause cardiovascular disease, hypertension, dyslipidemia, diabetic nephropathy, diabetic neuropathy, diabetic retinopathy, diabetic foot and erectile dysfunction [2, 3]. The consequences of DM cannot be overlooked because of their potential multiple economic impacts: on the one hand, the direct medical costs including the costs for hospitalization, physician office visits, specialist services, drugs, self-monitoring of blood glucose (SMBG) and treatment of hypoglycemic events; on the other, a patient with diabetes is subject to the inability to work at full capacity or at all, resulting in absenteeism or early retirement [4]. Despite the importance of this disease, comprehensive studies on diabetes costs are limited, particularly those including indirect costs [4].
An epidemiological survey conducted in Italy describes DM as a widespread disease in the population. The authors estimated a type 1 and type 2 DM prevalence equal to 5.8 % in 2010 with an increasing trend (+13 % compared to 2007 analysis) [1]. Of these, 4 % were estimated to have type 1 DM [1]. Information concerning direct costs at the national level is limited. The ARNO Observatory estimates that the average annual direct cost per patient spent by the NHS amounted to €2,756 in 2010, 57 % of which was due to hospitalization, 29 % to drugs and 14 % to specialist services. However, the analysis did not take into account SMBG, a very important component of direct costs in diabetes therapy [5]. Furthermore, there is no standard diabetes therapy for all patients, but it is diversified into various types of treatment: oral therapy (OT), basal supported oral therapy (BOT) and basal-bolus insulin therapy (BBT).
A European study published in 2010 comparing the national cost of diabetes in five EU countries reports a total direct medical cost (drugs, hospitalizations, health specialist services) of approximately €7.92 billion in Italy. The authors extrapolated to the national population by using the OECD population estimates and the ISTAT 4.8 % national prevalence estimate [4]. As far as the 2010 indirect costs of diabetes are concerned, they amount to a total of €12.64 billion in Italy, and they include €5.36 billion for absenteeism, €7.19 billion for early retirement and €0.97 billion for social benefits [4].
The main objective of this study was to address the foregoing gap: (1) by estimating the total direct medical costs associated with DM treatment in Italy and (2) by providing an aggregate measure of the total indirect costs for abseenteism and early retirement due to DM.
Methods
Study design
A probabilistic prevalence cost of illness (COI) model was developed in order to calculate an aggregate measure of the economic burden associated with DM in Italy. The model aims at estimating both the direct medical costs and indirect costs of the disease in Italy. In our approach, direct costs measure the value of the resources used for treating a particular illness (drugs, hospitalizations, monitoring and AE), whereas indirect costs measure the value of lost resources due to the illness condition (absenteeism and early retirement) [6].
In order to estimate the direct medical costs, a bottom-up approach was used. It estimates the cost by calculating the average cost of treatment multiplied by the illness prevalence in Italy. The average cost of treatment is calculated by adding up the various treatments [7]. For the estimation of the indirect costs, the human capital method was used. It measures the lost productivity in terms of lost earnings of a patient or caregiver [8].
The data used in the model were estimated through a systematic literature review at the national and international level [9]. A 1-year time horizon and social perspective were considered.
Systematic literature review
As mentioned above, the secondary data used to inform estimates were identified via a literature review. The flow of information through the different phases of the systematic review is shown in Fig. 1.
Search strategy and selection criteria: In order to collect related secondary data, we carried out a systematic search in the following electronic databases: MEDLINE (PubMed), ISTAT (Italian National Institute of Statistics) and EpiCentro (Italian Epidemiology Portal). The systematic literature review included four steps: identification, screening, eligibility and inclusion [9]. The research was limited in time (articles published over the last 5 years) and space (articles about Italy). The keywords used for the search were: cost of illness, cost, burden of disease, burden of illness, diabetes and DM.
All the studies used in the epidemiologic and economic synthesis were required to meet at least one of the following inclusion criteria:
-
1.
Epidemiological data on diabetes (with particular attention to the illness prevalence and its treatments) resulting from population databases, such as national surveys or registries;
-
2.
Data on the direct medical costs of the illness evaluated from the perspective of the payer and expressed in monetary values;
-
3.
An observational study of epidemiological data on diabetes and their connected direct costs, simultaneously observed in the same cohort of patients;
-
4.
Studies containing indirect cost data of the illness or data on lost productivity associated with diabetes.
A total of 541 studies were identified, and 42 of them were eligible for inclusion, 32 of which were excluded because they did not meet the economic or epidemiologic inclusion criteria. Ten studies were used for the implementation of the model: three for the epidemiological analysis, six for the economic parameter and one for both. The main items identified by the systematic review of the literature are reported in Appendix A.
Model parameters
The data extrapolated from the records identified through the systematic review were aggregated to obtain estimates including inside intervals (minimum and maximum available data from the literature). This approach was based on the assumption that differences found in various sources could indicate a probability distribution reflecting the available information in real-world data. The average value of the distribution was estimated from a particularly reliable source in the literature or from the average minimum and maximum values, assuming an equal distribution at the two extremes. The probability distribution of the parameters was attributed by the common practice of health economics modeling. For cost parameters a gamma distribution was assigned, while the epidemiological parameters (prevalence or proportions) were modeled as a beta distribution [10]. The parameters used for the implementation of the model are reported in Table 1.
Epidemiologic synthesis
In 2012 the Italian population was approximately 60 million people [11]. The diabetes prevalence provided by ISTAT [12] was equal to 5.5 % in 2012. However, other sources estimated diabetes prevalence within a range between 4.9 % [3] in 2011 and 5.8 % [1] in 2010. On average, 79 % of diabetic patients (between 70 % [1] and 88 % [13]) were on treatment, while the remaining 21 % were able to control the disease thanks to a healthy lifestyle, diet and physical activity [1, 13]. Treated patients were divided into three groups: oral therapy (OT, about 76 %), BOT (about 11 %) and basal-bolus therapy (BBT, approximately 13 %) [1]. The proportion was assumed steady over time, as indicated in the ARNO estimates where the variation between 2007 [14] and 2011 [1] related to the three groups was about 1 % (+1 % OT patients treated, +1 % BOT patients treated, >0.5 % BBT patients treated). This variability estimated the variation range.
Economic synthesis: direct medical costs
The selection of direct cost parameters was based on the “2009–2010 Italian standard treatment of DM” published by the Diabetologists Medical Association (AMD) [2]. The selected parameters to estimate the total direct cost of diabetes treatment were: costs of drugs, costs of hospitalizations, costs of specialist services, costs of self monitoring of blood glucose (SMBG) and costs of treatment and care of hypoglycemic events. If the costs were referred to different years before 2012, they were amended with the “ISTAT compound consumer price index rate (CCPI rate)” and expressed in euros (2012 values) [15]. Specifically, the costs have been estimated as follows.
Costs of drugs
This cost per patient was calculated as the ratio of gross pharmaceutical expenditure associated with the diabetic population compared to the total diabetic population. The maximum and minimum values were drawn from the ARNO report [1] and an Emilia-Romagna publication, respectively [16].
Costs of hospitalizations
This cost per patient was calculated as the ratio of gross hospitalization expenditure associated with the diabetic population compared to the total diabetic population. Hospital expenditure refers to monetary values for hospital disease-related groups (DRGs) and outpatient tariffs. The DRG system aggregates all activities, including surgical interventions, administered drugs, materials and health personnel, for each individual diagnosis. Furthermore, it establishes the reimbursement rate, corresponding to the sum of all provided interventions to be paid to the hospital [17]. Like the cost of drugs, the maximum and minimum values were drawn from the ARNO report and an Emilia-Romagna study, respectively [1, 16].
Costs of health specialist services
This cost per patient was calculated as the ratio of specialist service gross expenditure associated with the diabetic population compared with the total diabetic population. Specialist service gross expenditure is the amount of total expenditure of each specialist service. The specialist services include: non-hospital services (outpatient), specialist visits, cycles of rehabilitation services, laboratory tests and diagnostic imaging. Also in this case, the maximum and minimum values were drawn from the ARNO report [1] and the Emilia-Romagna study, respectively [16].
Costs of SMBG
This cost depends on the use of daily tests for glycemic control. The cost of SMBG per patient was calculated as the average single test cost [5, 18] multiplied by the average of daily tests used for glycemic control [2]. The number of tests is not the same in the different treatments: patients under BBT use on average from four to seven tests per day [2, 17], those under BOT use from three to four tests per day [2, 5] and patients under OT use from 0.6 to 2.3 tests per day [2, 5].
Costs of hypoglycemic events
The model considered two types of hypoglycemic events: mild/moderate and severe. For moderate hypoglycemic events, it was assumed that there was no additional use of any other drugs, but a simple injection of glucose followed by a glycemic control after a few minutes [2]. Therefore, these costs were already included in the SMBG costs. If a patient had one severe event, the model assumed that he or she took glucagon plus six additional daily tests with respect to patients making normal blood glucose controls [2]. The cost of an event (six tests + glucagon [2, 19]) was then multiplied by the annual probability of such an event [2]. Table 1 shows the costs associated with severe hypoglycemic events.
Economic synthesis: indirect cost
Due to the lack of information on indirect costs, it was possible to estimate the absenteeism and early retirement costs only. In order to estimate them, a study from Danish population registries was used [20], thus assuming that the Italian diabetic population has the same behavior as the Danish one. In order to calculate costs caused by absenteeism, the following elements were taken into account: the average daily earnings in 2011 in Italy [21, 22] multiplied by the diabetic population in active employment [3]; the average lost working days in a year because of the disease [20]. For the costs resulting from early retirement, an average gross income at retirement [23] was used, multiplied by the probability of early retirement of the diabetic population [20]. All the parameters used for the estimation of indirect costs are summarized in Table 2.
Sensitivity analysis
Sensitivity analysis is recommended any time there is uncertainty [25]. In order to verify the uncertainty of the model results, a deterministic one-way and probabilistic sensitivity analysis (DSA and PSA, respectively) was performed [26]. In DSA, each sensible parameter of the model was subject to a variation of ±25 % [26], and the model results were compared to the value of the base case. The DSA results were represented by a tornado diagram.
Probabilistic sensitivity analysis provides a useful technique to quantify the level of confidence of a decision-maker in drawing conclusions from an economic evaluation [26]. At each model parameter, a probability distribution (Table 1) used to make 5,000 Monte Carlo simulations was assigned in order to test the robustness of the results and define a 95 % CI.
Results
In 2012 3.3 million diabetic people were estimated in Italy. With reference to patients under pharmacological treatment, the model estimated about 2.6 million patients totally in Italy in 2012 (Table 3). The majority of these patients were treated with OT (2.0 million people), while only a small part of them was treated with BOT and basal bolus (273,681 and 338,843, respectively). In Italy, about 1.2 million people had to prematurely retire or lost working days (567,749 and 620,662, respectively) because of the disease in 2012. The average annual indirect cost per treated patient is €3,640. Obviously, it depends on the considered therapy group: OT has an average cost per patient equal to €3,487, BOT €3,909 and BBT €4,330.
Regarding the indirect costs, the estimated average annual expenditure per patient is equal to €4,098. The average annual expenditure of absenteeism per patient is €2,612, while early retirement amounts to €15,957 per patient yearly.
The model estimated that the total expenditure for the treatment and care of DM amounted to €20.2 billion in Italy, ranging from €18.3 to €22.0 billion. Approximately 53 % of this total expenditure is due to indirect costs and 47 % to direct medical costs.
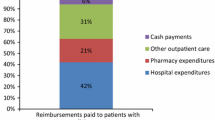
The direct medical costs to the Italian NHS amount to €9.6 billion (95 % CI €8.09–€11.07). Table 4 shows the total expenditure related to drugs, SMBG, specialist services and hypoglycemic events. The most important direct cost is hospitalization: €3.83 billion associated with patients under OT (95 % CI €3.09–€4.64), €530 million with BOT patients (95 % CI €0.42; €0.64) and €650 million with patients under BBT (95 % CI €0.52–€0.72), for a total expenditure of €5.05 (95 % CI €4.1–€6.0). Table 5 shows the model estimated a total indirect cost caused by diabetes in Italy of €10.7 billion (95 % CI €9.94–€11.42), €9.0 billion of which is due to early retirement and €1.62 billion to absence from work, with a corresponding 95 % CI of €8.39–€9.74 billion and €1.50–€1.74 billion, respectively.
Figure 2a shows how the deterministic variation of each parameter affects the estimate of total expenditure on direct medical costs associated with diabetes. As a result, the prevalence of diabetes is the parameter that requires the highest level of variation in expenditures. The second sensitive parameter of the model is the cost of hospitalizations. The prevalence of diabetes is, again, the most important parameter to estimate the total indirect costs (Fig. 2b). However, the probability of early retirement involves an equally relevant variation.
Discussion
Chronic non-communicable diseases are one of the most difficult challenges for health systems because of their steady and relentless growth. Undoubtedly, the most paradigmatic example is DM [27]. However, many governments and health programs are unaware of the consequences of an increase in the incidence of diabetes and its serious complications.
To our knowledge, the present study is the first attempt to evaluate the annual economic burden of diseases associated with diabetes from both NHS and social perspectives, with a probabilistic model considering the heterogeneity and scarcity of the information available in Italy.
The study showed that DM is a widespread disease in the population (prevalence of 5.5 % in 2012), with an average annual expenditure of €20.45 billion (95 % CI €18.61 to €22.29 billion). This result includes both the expenditure of the Italian NHS (direct costs) and that incurred by social welfare (indirect costs). For the latter, a total expenditure of €10.7 billion was estimated, €9.0 billion of which is associated with early retirement caused by the disease and €1.62 billion with absenteeism caused by the severity of the disease. These results are different from those of the study of Kanavos et al. [4] estimating a total expenditure of €5.36 billion in 2010 associated with absenteeism and €7.19 billion with early retirement. With reference to early retirement, the difference can be attributed to a higher estimate of early retirees (+12.3 %), which can be caused by a higher prevalence of the disease in 2012. This study too used the average annual income at retirement instead of the average annual pension considered in the study of Kanavos et al., which is slightly higher (+9.5 %). As far as absenteeism is concerned, the difference between the two approaches is due to a lower number of diabetics in active employment (our estimation is 53.5 % less). This difference is due to the different data sources. In fact, while in this study the estimate was made using the data reported by ISTAT [3, 23], Kanavos et al. reported a survey developed by the author. In our opinion ISTAT data [3, 23] seem to be the most reliable source available in Italy.
However, the study confirms that the expenditure on indirect costs should never be overlooked. In fact, more than half of the total disease expenditure is linked to this cost item. It should be noted that the expenditure on indirect costs can be estimated only for absenteeism and early retirement; therefore, our approach may underestimate these types of costs.
The expenditure on the estimated direct medical cost to the Italian NHS was approximately €9.59 billion (95 % CI €8.11 to €11.06). In this case, the estimated expenditure was in line with the value identified by Kanavos et al. [4] (€8.5 billion) that was included within the confidence interval estimated by our study. With reference to 2012, the total health care expenditure of the Italian NHS was €114.5 billion [28]. Our study estimated that the COI related to diabetes care in Italy absorbs 8.3 % of the total public health expenditure.
The estimated average annual cost associated with direct medical costs was €3,640 for each diabetic patient. This estimation not only includes the costs of hospitalizations, medications and specialist services, but also the costs of SMBG and hypoglycemic events, not taken into account in other studies [1, 2]. In addition to this, the study pointed out the various costs associated with the therapies used to keep diabetes under control: OT, BOT and BT. Although the information was not totally exhaustive, the study demonstrated that the OT is the least expensive and most widespread; BB and BOT therapies have much higher costs with respect to OT (BB +24 % and BOT +12).
In general, one of the objectives of the Italian NHS is the percentage of diabetic patients hospitalized. In fact, the costs related to the hospitalization of diabetic patients are a negative symptom in terms of both complications and the incapacity of the territorial services to take care of the patients. In our model, the cost of hospitalization was the main item of health care costs for the treatment of diabetes in Italy. Hospitalizations can be caused by a high prevalence of the disease, but also by deficiencies in the management of patient care [3]. The opportunity to reduce this cost could be the main objective of economic and health policies in the future years. One-way sensitivity analysis confirms that, reducing the number of hospitalizations to about 25 %, the total DM direct costs decrease to €1.2 million (−13.2 % vs. the base case). Considering this, pursuing a policy of appropriate drug treatment and diabetes monitoring could allow a better allocation of resources and potential savings to the NHS.
Finally, several studies [29] showed that in a large number of the people suffering from diabetes, the disease is diagnosed a few years after its onset. Even if the disease does not show any clear symptoms, the risk of vascular complications is already present. Therefore, it may be assumed that prevention and screening policies are the right actions to reduce the costs of diabetes.
However, this study has some limitations. First, it was not possible to identify a single national source collecting all data related to costs of the epidemiological disease. This issue has been approached carrying out a systematic literature review following specific guidelines accepted by the scientific community [9]. In this way, it was possible to organize the available data in a clear and scientific way in order to extract as much evidence as possible. Second, the epidemiological data are poor and heterogeneous, particularly regarding the patient distribution by type of treatment and associated costs. It is often necessary to depend on sample data or data based on a single Italian region. Furthermore, the data detected by the ARNO Diabetes Observatory are based on an enrolled patient population of 9,465,492 subjects of 29 ASLs [1], so it is a survey of objective data reporting clinically diagnosed diseases. Instead, the data collected by ISTAT are based on the questionnaire proposed by the Multiscopo Survey [12]. This means that each patient subjectively reported the diagnosis. However, the probabilistic sensitivity analysis made it possible to take into account the heterogeneity of the different data available. Finally, the cost parameter considered in the model did not come from a single source, and it was not possible to clearly distinguish the different costs of diabetes. In particular, hypoglycemia and glucose monitoring costs are exposed to a risk of double counting, and information on indirect costs was provided by Danish population registers [20]. Finally, it should be noted that the COIs are only evaluated for treated patients, and nothing was assumed regarding patients without drug therapy.
Conclusion
In conclusion, this work has provided, for the first time, a probabilistic estimation of direct and indirect costs associated with DM in Italy considering the available literature. This model should be a good tool for policy makers to properly understand the economic implications of diabetes treatment and care in the national context of reference.
References
ARNO observatory diabetes. The profile of the care population with diabetes. Report 2011 Volume XVII—Series “Reports ARNO” Cineca. (2011)
Association of Diabetologists—Italian Society of Diabetology. Standard Italian for the treatment of diabetes mellitus 2009–2010. Turin, (2010)
National Institute of Statistics. Diabetes in Italy 2012 ISTAT, Rome (2012)
Kanavos. P., van den Aardweg., P, Shurer., W.: Diabetes expenditure, burden of disease and management in 5 EU countries. LSE Health, London School of Economics
Ravasio, R.: Analysis of cost-effectiveness of exenatide versus insulin glargine in the treatment of type 2 pazientidiabetici secondary failure to oral hypoglycemic double. Ital. J. Health Technol. Assess. 1(1), 21–30 (2008)
Kirsten., R.: Disease-specific estimates of direct and indirect costs of illness and NIH support: fiscal year 2000 Update. http://odpp.odnih.gov/ecostudies/COIreporterweb.htm. Accessed Dec 2013
Joel, E., Segel, B.A.: Cost-of-illness studies-a primer. RTI International RTI-UNC Center of Excellence in Health Promotion Economics. (2006)
Hodgson, T.A., Meiners, M.R.: Cost of illness methodology: a guide to current practice and procedures. Milbank Meml Fund Q 60(3), 429–462 (1982)
Moher, D., Liberati, A., Tetzlaff, J., et al.: Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med 6, e 10000097 (2009)
Briggs, A., Claxton, K., Sculpher, M.: Decision modelling for health economic evaluation. Oxford University Press, New York (2007)
National Institute of Statistics. Resident population in Italy (2012). http://demo.istat.it/pop2012/index.html (Accessed Nov 2013)
National Institute of Statistics–Statistical Yearbook 2012 Italian Rome, Oct (2012)
S.I.M.G. (Italian Society of General Medicine)–VII Report Search Health Research Institute of the Italian Society of General Medicine Year 2011–2012. Florence, (2012)
ARNO Observatory diabetes. Analysis of 10 years of prescriptions. Report 2007 vol. XI-Ed. Centauro srl, Bologna, (2007)
National Institute of Statistics. Revaluation and documentation on prices, costs and contractual wages. Consumer price index for families of workers and employees. http://rivaluta.istat.it/ (2013). Accessed Nov 2013
Emilia–Romagna Regional Health Service. Dossier No. 179/2009-Care profiles and costs of diabetes in Emilia–Romagna, empirical analysis through administrative data 2005–2007. Emilia-Romagna, Bologna, (2009)
Baio, G., Capone, A., Marcellusi, A., Mennini, F.S., Favato, G.: Economic burden of human papillomavirus—related diseases in Italy. PLoS One 7(11), e49699 (2012). doi:10.1371/journal.pone.0049699
Tunis, S.L., Willis, W.D., Foos, V.: Self-monitoring of blood glucose (SMBG) in patients with type 2 diabetes on oral anti-diabetes drugs: cost-effectiveness in France, Germany, Italy, and Spain. Curr. Med. Res. Opin. 26(1), 163–175 (2010)
Federfarma. http://www.federfarma.it/Farmaci-e-farmacie/Cerca-un-farmaco.aspx. Accessed Dec 2013
Sorensen, J.: Attributable costs of complications among people with diabetes. In Centre for Applied Health. Services Research and Technology Assessment. Syddansk universitet (2009)
Organization for Economic Co-operation and Development (OECD). Gross domestic product: GDP per head, US$, current prices, current PPPs. http://www.oecd-ilibrary.org/economics/country-statisticalprole-italy_20752288-table-ita. Accessed Dec 2013
Calculator working days in Italy. www.giorni-lavorativi.com. Accessed Dec 2013
National Institute of Statistics—Unemployment rate 15–64 years in 2012. http://www.istat.it/it/lavoro. Accessed Dec 2013
National Institute of Statistics. Pension and beneficiaries: a gender analysis year 2011 Rome, (2013)
Briggs, A.: Handling uncertain in economic evaluation. BMJ 319(7202), 120 (1999)
Taylor, M.: What is sensitivity analysis? Hayward Medical Communications. (2009)
Lauro, R., Nicolucci, A.: Facts and figures about the diabetes in Italy. In: Public Health and Health Policy “an informed health policy on chronic diseases” pp. 27–41 (2011)
National Institute of Statistics. Public health expenditure.http://noiitalia.istat.it/index.php?id=7&user_100ind_pi1[id_pagina]=432&cHash=e92dffa8e3b7988b531609bbc6fdcd73. Accessed Dec 2013
International Diabetes Federation: IDF diabetes atlas, 6th edn. International Diabetes Federation, Brussels (2013)
Acknowledgments
The study was partially supported with unrestricted funding from Abbott, Italy.
Author information
Authors and Affiliations
Corresponding author
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Marcellusi, A., Viti, R., Mecozzi, A. et al. The direct and indirect cost of diabetes in Italy: a prevalence probabilistic approach. Eur J Health Econ 17, 139–147 (2016). https://doi.org/10.1007/s10198-014-0660-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10198-014-0660-y