Abstract
In 2009, the National Institute for Health and Clinical Excellence (NICE) issued supplementary advice to its Appraisal Committees to be taken into account when appraising life-extending, ‘end-of-life’ treatments. This indicated that if certain criteria are met, it may be appropriate to recommend the use of such treatments even if they would not normally be considered cost-effective. However, NICE’s public consultation revealed concerns that there is little scientific evidence to support such a policy. This study examines whether there is public support for giving higher priority to life-extending, end-of-life treatments than to other types of treatment. In face-to-face interviews, respondents answered six questions asking them to choose which of two hypothetical patients they would prefer to treat, assuming that the health service has enough funds to treat one but not both of them. The various scenarios were designed so as to control for age- and time-related preferences. Fifty members of the general public in England were interviewed in July 2011. We find some evidence of support for giving priority to the patient with shorter remaining life expectancy, but note that a nontrivial minority of respondents expressed the opposite preference. Substantial preference for quality-of-life improvement over life extension was observed. Very few respondents expressed indifference or unwillingness to choose between the patients. Whilst there cannot be described to be a single ‘consensus’ set of preferences, we conclude that there are ways in which the results suggest that the current NICE policy may be insufficient.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Background
The National Institute for Health and Clinical Excellence (NICE) is responsible for producing advice on the use of new and existing health technologies to the National Health Service (NHS) in England and Wales. NICE’s Technology Appraisals are guided by clinical and cost-effectiveness analyses, usually using the quality-adjusted life year (QALY) [1] to measure health outcomes. Current guidelines used by NICE [2] define a ‘reference case’ position whereby all equal-sized health gains are of equal social value, regardless of to whom they accrue and the context in which they are enjoyed. As well as evaluating the scientific evidence, those responsible for formulating NICE advice also need to make social value judgements [3]. These are concerned with what is appropriate and acceptable for society in delivering health care across the NHS.
In January 2009, NICE issued supplementary advice to its Appraisal Committees (independent committees responsible for formulating NICE guidance based on the available evidence) to be taken into account when appraising life-extending, ‘end-of-life’ treatments [4]. This advice constitutes an explicit departure from the reference case position described above. It indicates that if certain criteria are met, it may be appropriate to recommend the use of treatments for terminal illness that offer an extension to life even if their base case cost-effectiveness estimates exceed the range normally considered acceptable [5]. Some aspects of the supplementary advice were revised following a 5-week public consultation exercise [6]. The current criteria [7] are reproduced below; if met, the Appraisal Committee is asked to consider the impact of giving greater weight to the health gains achieved in the later stages of disease.
-
C1.
The treatment is indicated for patients with a short life expectancy, normally less than 24 months;
-
C2.
there is sufficient evidence to indicate that the treatment offers an extension to life, normally of at least an additional 3 months, compared to current NHS treatment; and
-
C3.
the treatment is licensed, or otherwise indicated, for small patient populations.
The advice also states that the Appraisal Committees should be satisfied by the robustness of the estimates and assumptions used in the economic modelling and that all calculations should consider the cumulative population for each licensed indication.
One way of understanding whether such a policy is appropriate and acceptable for society is to establish whether it is consistent with the preferences of members of the general public. In line with the NHS’s policy objective of ensuring public involvement in health-care priority setting activities [8, 9], NICE’s position on social value judgements is that “advice from NICE to the NHS should embody values that are generally held by the population of the NHS” [5]. Empirical studies of public preferences can provide meaningful information about these values as long as the methods used are scientifically defensible [10]. Richardson and McKie [11], amongst others, have argued that such studies should form part of an ‘empirical ethics’ approach to allocating health care resources.
However, the consultation revealed concerns that there is little evidence to support the premise that society is prepared to fund life-extending end-of-life treatments that would not meet the cost-effectiveness criteria used for other treatments [6]. Whilst there is a growing body of evidence indicating a societal preference for giving greater weight to the health gains accruing to the severely ill [12], severity is typically described in terms of quality of life rather than length of life or proximity to death. Most of the empirical studies in the health economics literature do not make it clear how duration is to be considered. Furthermore, a review undertaken by the UK Department of Health in 2010 [13] noted that “there is currently no robust evidence in the literature to support a particular magnitude of weighting” of health gains accruing to patients who are severely ill or at the end of life.
Since then, some researchers have sought to investigate people’s preferences regarding end-of-life treatments more directly. In a pan-European study seeking to develop methods for determining the monetary value of a QALY, Donaldson et al. [14] tested the hypothesis that health gains arising at the end of life would be valued less than gains of the same magnitude arising more imminently. They found that across countries the median values for health gains at the end of life were considerably smaller than for the corresponding health gains now. In a small-scale exploratory study, Baker et al. [15] found that the majority of general public respondents in Scotland expressed preference for a treatment that extends the lives of a relatively small number (five) of terminally ill cancer patients by a short duration over a treatment that improves quality of life for a relatively large number (100) of patients with a non-life-threatening condition.
In a study of the preferences of members of the general public in Spain, Pinto Prades et al. [16] found that QALYs gained at the end of life were valued more highly than those gained from alleviating temporary health conditions and that quality-of-life-improving end-of-life treatments were valued more highly than life-extending end-of-life treatments. Finally, Linley and Hughes conducted a large-scale study of preferences of members of the general public in Great Britain regarding a variety of prioritisation criteria, including the so-called ‘end-of-life premium’ [17]. Respondents were asked how they would prefer NHS money to be spent when faced with a choice between treating one patient group with a remaining life expectancy of 18 months and another patient group with a remaining life expectancy of 60 months. The results suggest, all else being equal, that the end-of-life premium is not supported, with about two-thirds of respondents opting not to allocate more resources to the group with shorter remaining life expectancy.
Notwithstanding these recent additions to the empirical literature, the evidence remains limited, and NICE has acknowledged a need for further exploration of the issues [6].
Objectives
The aim of this study is to examine whether the policy of giving higher priority to life-extending end-of-life treatments (as specified by NICE) than to other types of treatment is consistent with the preferences of members of the general public. The study focuses on criteria C1 and C2 of the supplementary advice above.
The survey was designed so as to enable testing of the following hypotheses: (1) the majority of people wish to give higher priority to the treatment of end-of-life patients than to non-end-of-life patients; (2) concern about age is not a motivating factor for any observed preference for giving higher priority to the treatment of end-of-life patients; (3) time preference is not a motivating factor for any observed preference for giving higher priority to the treatment of end-of-life patients; (4) the majority of people wish to give equal priority to life-extending and quality-of-life-improving treatments for end-of-life patients; and (5) concern about age is not a motivating factor for any observed preference for giving higher priority to either life-extending or quality-of-life-improving treatments for end-of-life patients.
Methodology
Survey instrument
The survey used six scenarios (S1–S6) to address the research questions posed. In each scenario, information was presented about two hypothetical individuals (patient A and patient B) who have been diagnosed with illness. Both patients could benefit from treatment but the respondents were asked to assume that the health service had enough funds to treat one but not both of them. Each scenario comprised two tasks. The first task required respondents to indicate which of three statements best described their view: (1) “I would prefer the health service to treat patient A”; (2) “I have no preference”; (3) “I would prefer the health service to treat patient B”. The second task required respondents to consider a list of 18 statements, each describing a possible reason for their choice in the first task (these are reproduced in the “Appendix”). They were asked to indicate, by ticking the relevant boxes, which of those statements were consistent with their own reasons. This task is hereafter referred to as the ‘tick-box task’.
Table 1 summarises the information provided to respondents for all six scenarios. In S1, S2 and S3, treatment would extend the life of either patient A or patient B by 6 months (with certainty); the patients differed in terms of age and the amount of time between diagnosis and expected death. These scenarios did not examine quality of life—respondents were advised that the patients’ illnesses were asymptomatic and that treatment would not affect their quality of life.
In S4, S5 and S6, the illnesses were described as having a negative effect on quality of life, with both patients experiencing their final year of life at 50 % of full health. The concept of ‘50 % health’ was explained to respondents as follows: “Patients have told us that being in this health state for 2 years is equally desirable as being in full health for 1 year”. In these scenarios, treatment would restore patient A to full health (with no effect on life expectancy) or extend the life of patient B by 1 year (with no effect on quality of life).
Under the conditions that that 2 years in 50 % health is equivalent to 1 year in full health, and that a health gain today is equivalent to an equal-sized health gain in the future, both patients will gain exactly the same amount of health from treatment in all six scenarios—half of a QALY.
Scenario S1 provides a simple test of whether respondents wish to give higher priority to the treatment of end-of-life patients, as the only difference between the two patients at the start of the scenario is that patient B has a shorter amount of time left to live than patient A (1 year would be classed as ‘short life expectancy’ under criterion C1, whereas 10 years would not).
However, the scenario design is such that there may be reasons for choosing to treat patient B in S1 other than favouring the treatment of end-of-life patients. First, without treatment patient A will be 9 years older when they die than patient B will be when they die. Hence, a preference to treat patient B may be driven by a social preference for giving priority to the young. A review by Dolan et al. [18] suggests that there is some evidence of public support for age weighting based on equity concerns. To address this issue, scenario S2 replicates S1 except that patient B is 9 years older than patient A at the start of the scenario, which means that both patients will die at the same age without treatment.
Second, the benefit from treating patient A would not take place until 10 years into the future (compared to 1 year into the future for patient B). Hence, a preference to treat patient B may be driven by a preference for enjoying benefits sooner rather than later. In general, it is assumed by decision makers in the UK that society has a positive time preference [19], which means that the further into the future benefits are accrued, the lower the value of those benefits. To address this issue, scenario S3 replicates S2 except that patient A is described as having been diagnosed with their illness 9 years prior to the start of the scenario. This means that the benefits from treating patient A would now take place 1 year into the future—the same as for patient B. Thus both patients are at the ‘end of life’ in S2, but patient B’s progression to this state has been more sudden than that of patient A.
Considerations of quality of life are introduced in scenarios S4, S5 and S6. S4 and S5 involve choosing between treatments that extend life and those that improve quality of life. NICE’s end-of-life criteria accommodate life extensions but not quality-of-life improvements. The two scenarios are identical except for the ages of the patients. In S4, both patients are younger adults (30 years old); in S5, they are older adults (70 years old). Comparing the results of S4 and S5 will therefore provide an indication of whether the preference for a particular type of treatment (life-extending or quality-of-life-improving) for end-of-life patients is dependent on the life stage of the patients. Scenario S6 combines elements of S2 and S4/S5 in that it involves choosing between treating a non-end-of-life patient (patient A) and an end-of-life patient (patient B) and between a quality-of-life-improving treatment (to patient A) and a life-extending treatment (to patient B).
We conjecture that a supporter of NICE’s end-of-life policy would choose to treat patient B in all scenarios, except perhaps S2 where it is less clear whether the supplementary advice applies (the criteria do not distinguish between sudden and non-sudden disease progression).
Administration of survey
The survey was administered using face-to-face interviews, undertaken by a team of six interviewers employed by a market research agency. The interviewers completed training on the specifics of the methodology and procedures for this study. All interviews were carried out in a one-to-one setting in the homes of respondents.
Background information (age, social grade and gender of the respondent) was collected at the beginning of the interview. Respondents then considered the scenarios one at a time, progressing to the next scenario once they had been given time to consider their views and had provided answers to the questions. The interviewers permitted respondents to amend their answers to earlier questions if they changed their mind during the course of the interview.
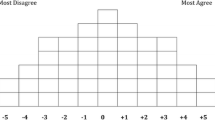
Information about the scenarios was presented in three ways: (1) the full scenario description was read aloud to the respondent by the interviewer, following a script; (2) key pieces of information were presented schematically using a diagram; and (3) key pieces of information were presented in a summary table beneath the diagram. A selection of the interview materials are reproduced in the “Appendix”. The diagram and summary tables were included in a paper booklet handed to each respondent. The booklets were also used to record respondents’ answers to the questions.
After concluding the interview, the interviewer was asked to answer three ‘diagnostic’ multiple choice questions. These were concerned with assessing: (1) how well the respondent had “understood and carried out the tasks”; (2) how much “effort and concentration” the respondent had put into the tasks; and (3) the extent to which there were “disruptions and interruptions” in the interview environment.
All data were collated and entered into an Excel database by the market research agency.
Sample
The survey was administered on a sample of adult members of the general public, split evenly between two areas of southeast England (London and Kent). The target sample size of 50 respondents was determined on the basis of available resources. A ‘minimum quota’ approach was used to recruit a sample that was broadly representative of the UK general population in terms of age, social grade and gender. The sample was recruited using a ‘door knock’ approach, with the interviewer approaching a household member of every fourth home in a randomly allocated postal area and scheduling interview appointments for those individuals that agreed to participate. A small cash payment was offered as an incentive for participation.
The survey was given ethics approval by the Ethics Committee of the University of Sheffield’s School of Health and Related Research.
Piloting
The study design was informed by a pilot, which used a convenience sample of 21 members of non-academic staff and postgraduate research students at the University of Sheffield. The pilot survey was administered using face-to-face interviews by one of the authors, Koonal K. Shah (KKS), and used a similar design to that of the study described in this article. The pilot was completed successfully, which indicated that a similar approach could be used for a larger scale study using a general public sample.
One of the aims of the pilot was to develop a better understanding of the reasons and principles underpinning people’s priority setting preferences, so respondents were encouraged to ‘think aloud’ and to discuss the reasons for their choices with the interviewer. The interview included a set of probing questions that were used to elicit detailed qualitative information about respondents’ preferences.
The findings from the pilot informed the design of the current study in a number of ways, in particular: the inclusion of a warm-up scenario; the inclusion of two scenarios (S4 and S5) exploring the extent to which preferences regarding end-of-life treatments are driven by considerations of the ‘life stage’ of patients; equal visual prominence for all three response options in respondents’ answer booklets; increased clarity in the description of what is meant by ‘50 % health’; and changes to the ways in which information about the scenarios was presented to respondents. The list of statements included in the tick-box task for each scenario was developed in accordance with the qualitative data obtained in the pilot.
A detailed report of the pilot study is provided elsewhere [20].
Results
Interviews were completed in July 2011. The sociodemographic characteristics of the sample are presented in Table 2. The sample includes a larger proportion of older individuals and a smaller proportion of middle-aged individuals than in the general population [21]. The sample also includes a relatively large proportion of individuals in the lowest social grades.
All 50 respondents completed the survey in full. According to the interviewers, the majority of interviews were carried out in distraction-free environments, with respondents who concentrated on and showed a good understanding of the survey tasks.
Response data
Table 3 reports aggregate response data for each of the six scenarios.
In S1, S2 and S3, preferring to treat patient B (the patient whose remaining life expectancy is shorter or who has known about their illness for less time) was the most popular choice, although it is only in S1 that the majority of respondents (60 %) made this choice, and even this result is not statistically significantly greater than 50 % at the 5 % level (binomial test using normal approximation; p = 0.08). In all three scenarios, there were more respondents who preferred to treat patient A than there were respondents who said that they had no preference between the two patients. In S4 and S5, the majority of respondents (58 and 56 %, respectively) preferred to treat patient A, for whom treatment would deliver a ½ QALY quality-of-life improvement. The remainder of respondents were roughly evenly split between preferring to treat patient B, for whom treatment would deliver a ½ QALY life extension, and having no preference. In S6, the majority of respondents (62 %) preferred to treat patient A, which involved giving a ½ QALY quality-of-life improvement to the non-end-of-life patient.
Tables 4, 5, 6 7 provide cross-tabulations of the response data from selected combinations of scenarios that help us to test the hypotheses set out in “ Objectives”. In these tables, the value in each cell refers to the number of respondents expressing that set of preferences.
The most common pair of choices in S1 and S2 was to prefer to treat patient B in both scenarios (made by 19 respondents—38 %) (Table 4). The most common reasons given in the tick-box task for preferring to treat patient B were that this choice benefits the patient ‘who is closest to death’ and who has ‘less time to prepare for death’. Four respondents (8 %) switched from preferring to treat patient B in S1 to having no preference in S2. Three of these respondents indicated in the tick-box task for S1 that their choice ‘benefits the patient who will die at a younger age’. A further seven respondents (14 %) preferred to treat patient B in S1 and to treat patient A in S2. There does not appear to be a consensus set of reasons given for this pair of choices. Three of these respondents did not give any reasons linked to the ages of patients; of the four that did give reasons linked to age, two gave reasons that were factually incorrect (e.g. stating that treating patient A in S2 involved benefiting the patient ‘who will die at an older age’).
The second most common pair of choices was to prefer to treat patient A in both scenarios (9 respondents—16 %). Almost all of the respondents who chose to treat patient A indicated in the tick-box tasks that they did so because they wished to benefit the patient ‘who has longer left to live’. Overall, there no statistically significant evidence of an association between patient age and the propensity to favour the treatment of patient B (χ 2 test of association; p = 0.16).
The most common pair of choices in S2 and S3 was to prefer to patient B in both scenarios (made by 10 respondents—20 %) (Table 5). The majority of the respondents who made this pair of choices ticked the boxes that read ‘My choice benefits the patient with less time to prepare for death’ for both scenarios. Eight of the 10 respondents ticked for box that read ‘My choice benefits the patient who is closest to death’ for S2, whilst three gave the equivalent reason for S3, when the statement was factually incorrect.
Five respondents (10 %) preferred to treat patient B in S2 and had no preference in S3. Of these respondents, only one ticked the box for S2 that read ‘My choice delivers the benefit today rather than far away in the future’. More popular reasons given for preferring to treat patient B in S2 were that patient B: ‘is older today’, ‘has less time to prepare for death’, and/or ‘can make the most of their remaining time’.
Seven respondents (14 %) preferred to treat patient B in S2 and to treat patient A in S3. There does not appear to be a consensus set of reasons given for this pair of choices. The most commonly given reason was that preferring to treat patient B in S2 ‘delivers the benefit today rather than far away in the future’ (three of the seven respondents ticked this box). A further seven respondents (14 %) preferred to treat patient A in S2 and to treat patient B in S3. The only reason that was given consistently for this pair of choices was that patient A has ‘longer left to live’ in S2 (six of the seven respondents ticked this box).
Overall, there is no statistically significant evidence of an association between the timing of the scenario and the propensity to favour the treatment of patient B (χ 2 test of association; p = 1.00).
The majority of respondents made the same choice in both S4 and S5—22 respondents (44 %) preferred to treat patient A in both scenarios; 8 respondents (16 %) expressed no preference in both scenarios; and 6 respondents (12 %) preferred to treat patient B in both scenarios (Table 6). Five respondents (10 %) preferred to treat patient B in S4 and to treat patient A in S5. Four respondents (8 %) made the reverse pair of choices, preferring to treat patient A in S4 and to treat patient B in S5. Some, but less than half, of the respondents who made each pair of choices gave reasons that were consistent with those choices—i.e. by ticking the relevant box that read ‘I think it is better to [improve health/extend life] than to [extend life/improve health] in this situation’. Another commonly given reason (particularly for respondents who preferred to treat patient A in S4 and to treat patient B in S5) was that their choice ‘benefits the patient who can make the most out of their remaining time’.
Considering all of the 14 respondents who did not make the same choice in both S4 and S5, there was no consensus as to whether it is preferable to give a quality-of-life improvement to a younger adult and a life extension to an older adult, or vice versa. In fact, the data suggest a fairly even split between these two views.
Overall, there is statistically significant evidence that the majority of respondents do not wish to give equal priority to life-extending and quality-of-life-improving treatments for end-of-life patients (binomial test using normal approximation; p = 0.00). However, there is no statistically significant evidence of an association between the life stage of the patient and the propensity to choosing either of these types of treatment (χ 2 test of association; p = 0.97).
The most common pair of choices in S2 and S6 was to prefer to treat patient B in S2 and to treat patient A in S6 (made by 15 respondents—30 %) (Table 7). The most commonly given reasons for this pair of choices were that treating patient B in S2 ‘benefits the patient with less time to prepare for death’ and that ‘it is better to improve health than extend life’ in the situation depicted in S6 (both boxes were ticked by seven of the 15 respondents). A small number of respondents ticked boxes relating to age and/or the timing of the benefits to explain their choices.
Overall, there is statistically significant evidence of an association between the availability of quality-of-life-improving treatment and the propensity to give priority to life-extending end of life at the 10 % level of confidence, but not at the 5 % level (χ 2 test of association; p = 0.06).
Across the six scenarios, there were 70 instances of respondents giving reasons in the tick-box task that were inconsistent with their choice or with other reasons they gave for that scenario. More than half of these came from six respondents who failed the ‘consistency checks’ on four or more occasions. The majority of respondents did not fail any of these checks. The ‘None of the above’ box was ticked on six occasions across all scenarios, five of which were for the tick-box task for S3. In all cases, respondents who ticked the ‘None of the above’ box did not tick boxes for any other reasons.
Considering the various combinations of choices made across all six scenarios, 39 different sets of choices were made by the 50 respondents. The most popular set of choices (‘BBBAAA’) was made by four respondents (8 %); most sets were made by only one respondent. Three respondents had no preference throughout the six scenarios (‘======’). No respondents made the set(s) of choices implied by the NICE end-of-life policy of giving greater priority to life-extending end-of-life treatments than to non-end-of-life treatments and to quality-of-life-improving end-of-life treatments (‘BBBBBB’ or ‘BB=BBB’).
Discussion
This study has elicited the preferences of a sample of the general public in England over health-care priority setting scenarios. Whilst the results should be interpreted with a degree of caution given the limited size and geographic coverage of the sample, we have been able to provide a number of insights on whether there is public support for a policy that gives higher priority to life-extending end-of-life treatments (as specified by NICE) than to other types of treatment.
The results suggest that: (1) there is weak evidence that people wish to give higher priority to the treatment of end-of-life patients than to non-end-of-life patients; (2) there is no evidence that concern about age is a motivating factor for giving higher priority to the treatment of end-of-life patients; (3) there is no evidence that time preference is a motivating factor for giving higher priority to the treatment of end-of-life patients; (4) there is strong evidence that people do not wish to give equal priority to life-extending and quality-of-life-improving treatments for end-of-life patients (favouring quality-of-life-improving treatments overall); and (5) there is no evidence that concern about the life stage of end-of-life patients is a motivating factor for preferring either life-extending or quality-of-life-improving treatments for those patients.
The fact that the most popular choice was to treat patient B in S1 and S2 indicates support for the prioritisation of the treatment of patients with shorter remaining life expectancy, but in both cases there is no statistically significant evidence at the 5 % level that the majority of respondents held this view. Moreover, a non-trivial minority of respondents indicated the opposite—that is, they preferred to give higher priority to the treatment of patients with longer remaining life expectancy. Data from the tick-box tasks suggest that such preferences may be driven by a belief that patients with longer remaining life expectancy are better placed to make the most out of a short life extension.
The most popular choice in S3 was also to prefer to treat patient B. This preference may be driven by concern about how much time the patient has had to ‘prepare for death’. Since patient B’s disease progression has been more sudden, they have had less time to prepare for death. The reasons given for choosing to treat patient B in the tick-box task for S3 support this explanation.
The response data for S4 and S5 provide evidence of an overall preference for giving priority to quality-of-life-improving rather than life-extending treatments for patients with short remaining life expectancy. Furthermore, the data for S6 suggest that some respondents prefer to give priority to quality-of-life-improving over life-extending treatments even when the quality-of-life improvement accrues to a non-end-of-life patient and the life extension (of equal size, in QALY terms) accrues to an end-of-life patient. One interpretation of these results is that the preference for giving priority to quality-of-life-improving treatments is so strong that it outweighs any preference for giving priority to end-of-life treatments. Another interpretation is that the respondents have misunderstood (or rejected) the concept of the QALY, believing that a ½ QALY quality-of-life improvement is in fact more desirable than a ½ QALY life extension for the patients themselves. This issue is likely to exist in any study where quality of life needs to be quantified in this manner.
Comparing the response data for S1 and S2 allowed us to examine whether respondents’ preferences for treating the end-of-life or the non-end-of-life patient depended on the ages at which the patients would die without treatment. Similarly, comparing the response data for S4 and S5 allowed us to examine whether respondents’ preferences for either life-extending or quality-of-life-improving treatments for end-of-life patients depended on the life stage of the patients (i.e. whether they were younger adults or older adults). In both cases, the particular combinations of ages that we used in the scenarios do not appear to have influenced the choices of most of the respondents. However, concerns about age might have been more evident had the difference in ages been greater in S1 and S2 or if different life stages had been presented in S4 and S5 (for example, if the patients were described as teenagers aged 15 years in S4 and as oldest old individuals aged 90 years in S5).
In all six scenarios, the least popular choice was for respondents to express no preference between treating patient A and patient B. This is consistent with findings from the pilot and adds to the evidence that people do not support a strict health-maximisation objective when making priority setting choices [18], choosing instead to prioritise based on the characteristics of the patient, disease or treatment. It may be the case, however, that for some respondents health maximisation is the primary objective, but when there is nothing to choose between the two patients in terms of (undiscounted) health gain, they refer to other factors (such as remaining life expectancy) as a ‘tie breaker’. Following concerns about framing effects in the pilot, we took steps to make the ‘no preference’ option explicit and prominent in this study so as to make it clear to respondents that this was an acceptable response and that they were not obliged to choose to treat patient A or patient B. The tick-box task for each scenario also included several statements referring to reasons for having no preference. However, most respondents still preferred to treat one patient or the other and in general provided reasons in the tick-box tasks that were consistent with their choices.
There cannot be described to be a ‘consensus’ combination of preferences—the most popular set of choices (‘BBBAAA’) was made by only four respondents (8 %). This choice set indicates a preference for giving priority to those at the end of life (preferring to treat patient B in S1 and S2) and whose disease progression has been sudden (preferring to treat patient B in S3); a preference for quality-of-life-improving rather than life-extending treatments (preferring to treat patient A in S4 and S5); and a preference for quality-of-life-improving treatments that outweighs the preference for giving priority to those at the end of life (preferring to treat patient A in S6).
Policy implications and directions for future research
It is difficult to describe a single approach to priority setting that reflects the heterogeneous preferences elicited in this study. It is of note, however, that no respondents made the set of choices implied by the NICE end-of-life policy of giving greater priority to life-extending end-of-life treatments than to non-end-of-life treatments and to quality-of-life-improving end-of-life treatments (‘BBBBB’ or ‘BB=BBB’).
The study results suggest that the current policy may be insufficient in two ways. First, whilst it is concerned with patients’ remaining life expectancy, the supplementary advice does not distinguish between sudden and non-sudden disease progression. Findings from the pilot, coupled with an examination of the reasons given by respondents in the tick-box tasks, suggest that for many people the preference for prioritising the treatment of end-of-life patients is driven by concern about how much time the patients will have had to prepare for death. This may explain why over 40 % of respondents preferred to treat patient B in S3, despite the fact that patient B is no closer to their end of life than patient A in this scenario. However, it should be noted that no respondents made the choice set ‘BBBBBB’ (which implies support for an adjusted NICE policy that gives priority to patients whose disease progression has been most sudden). It should also be noted that of the six occasions when respondents ticked the box that read ‘None of the above’ when providing reasons for their choices, five referred to their choice in S3. This suggests that there are rationales for choosing either patient A or patient B in S3 beyond those that we had conjectured and that more work is needed to better understand people’s preferences regarding prioritisation according to the speed of disease progression.
Second, the NICE policy involves giving greater weight to life-extending but not to quality-of-life-improving treatments for those at the end of life. This is inconsistent with the finding that many respondents favoured the prioritisation of the quality-of-life-improving treatment over the life-extending treatment in S4, S5 and S6.
Whilst the results of this study provide an indication of whether there is public support for the policy of giving higher priority to life-extending end-of-life treatments than to other types of treatment, they do not give us any indication of the strength of the preferences for any individual respondent, nor do they allow us to determine whether the cut offs in the current NICE criteria (e.g. defining short remaining life expectancy as “normally <24 months”) are commensurate with public preferences. For these purposes, a further study would need to be undertaken. A great deal of uncertainty remains about how best to design equity-weighting studies [22] and how to overcome the challenges involved in incorporating equity weights into cost-effectiveness analysis [23].
Nevertheless, there are a number of ways in which the findings of this study can help inform the design of a future study seeking to derive a set of robust equity weights to reflect people’s preferences regarding end-of-life treatments. A key challenge for these types of study is defining attributes and levels that are policy relevant and salient to respondents [24]. We found evidence to suggest that the amount of time the patient has had to prepare for death and the nature of the health gain offered by the treatment (quality-of-life-improving or life-extending) are key drivers of preferences. We would therefore recommend that any weighting study should seek to better understand the strength of preferences regarding these attributes. On the other hand, we found little evidence to suggest that respondents’ preferences regarding end-of-life treatments are influenced by the age of the patients, so we would not recommend making age a core attribute of a weighting study (although it should be borne in mind that we elicited only preferences regarding younger adults and older adults; scenarios examining children, for example, may well have generated different results). Including a variety of levels for attributes such as remaining life expectancy can help us to understand whether those attributes exhibit non-linear or threshold effects on respondents’ preferences. For instance, it may be the case that people prefer to give priority to patients with shorter life expectancy up to a point, but when the life expectancy becomes extremely short (e.g. <3 months) then this preference no longer holds.
In this study, all of the scenarios were designed such that both patients received the same amount of undiscounted health gain—½ QALY in all cases. In reality, the NICE end-of-life policy has led to a situation whereby some end-of-life treatments offering very small improvements in health have been recommended for use in the NHS [25], whilst non-end-of-life treatments offering much larger benefits have not been recommended. It would be useful to understand the extent to which people are willing to sacrifice overall health benefit in order to give priority to the treatment of end-of-life patients. This could be examined by varying the levels of the ‘health gain from treatment’ attribute.
Public preference studies can help us to understand what people consider to be appropriate and acceptable for society. In order to obtain a comprehensive picture, however, it is important to capture not only respondents’ choices but also the reasons for their choices. The tick-box tasks were valuable in this respect, but were limited in that many respondents simply ticked boxes that referred to ‘factually correct’ statements but that did not necessarily offer any insight into the nature of their preferences. Moreover, a large number of respondents gave reasons that were inconsistent with each other or with their choices. Future studies should consider alternative ways of eliciting information to aid the interpretation of observed preferences.
Conclusion
In this article we have described a study that examined whether the policy of giving higher priority to life-extending end-of-life treatments (as specified by NICE) than to other types of treatment is consistent with the preferences of members of the general public. We report some weak evidence of public support for giving priority to the patient with shorter remaining life expectancy, but note that a sizeable minority of respondents expressed the opposite preference. The current NICE policy does not cover quality-of-life-improving end-of-life treatments and is not concerned with whether the treatments under appraisal are indicated for patients whose disease progression has been sudden. Yet our results suggest that people’s preferences regarding the end-of-life scenario may be influenced by these factors. We recommend conducting a larger scale study to derive a set of robust equity weights to reflect people’s preferences regarding end-of-life treatments.
References
Weinstein, M.C., Stason, W.B.: Foundations of cost-effectiveness analysis for health and medical practices. N. Engl. J. Med. 296, 716–721 (1997)
NICE: Guide to the Methods of Technology Appraisal. NICE, London (2008)
NICE: Social Value Judgements: Principles for the Development of NICE Guidance, 2nd edn. NICE, London (2008)
NICE: Appraising life-extending, end of life treatments. NICE, London (2009)
Rawlins, M.D., Culyer, A.J.: National Institute for Clinical Excellence and its value judgments. BMJ 329, 224–227 (2004)
NICE: End of Life Treatments: Summary Response to Consultation. NICE, London (2009)
NICE: Appraising Life-Extending, End of Life Treatments. NICE, London (2009). Revised in July 2009
Department of Health: The New NHS: Modern, Dependable. Department of Health, London (1997)
Department of Health: Involving Patients and the Public in Healthcare: A Discussion Document. Department of Health, London (2001)
Ryan, M., Scott, D.A., Reeves, C., Bate, A., van Teijlingen, E.R., Russell, E.M., et al.: Eliciting public preferences for healthcare: a systematic review of techniques. Health Technol. Assess. 5(5), 1–185 (2001)
Richardson, J., McKie, J.: Empiricism, ethics and orthodox economic theory: what is the appropriate basis for decision-making in the health sector? Soc. Sci. Med. 60, 265–275 (2005)
Shah, K.K.: Severity of illness and priority setting in healthcare: a review of the literature. Health Policy 93, 77–84 (2009)
Department of Health: Impact Assessment of Proposal for a Cancer Drug Fund. Department of Health, London (2010)
Donaldson, C. (project co-ordinator) et al.: European value of a quality adjusted life year: final publishable report. (2011) Available at: http://research.ncl.ac.uk/eurovaq/ Accessed 27 Dec 2012
Baker, R., McHugh, N., Mason, H., Currie, G., Donaldson, C.: Valuing end of life technologies, investigating the existence of a ‘cancer premium’ and methodological questions for health economics virtuous. Paper presented at the Health Economists’ Study Group meeting, Bangor (2011)
Pinto-Prades, J.L., Sanchez-Martinez, F.I., Corbacho, B.: Valuing QALYs at the end of life. Working paper 11.15. Universidad Pablo de Olavide, Seville (2011)
Linley, W.G., Hughes, D.G.: Societal views on NICE, Cancer Drugs Fund and value-based pricing criteria for prioritising medicines: a cross-sectional survey of 4118 adults in Great Britain. Health Economics (early view), doi:10.1002/hec.2872
Dolan, P., Shaw, R., Tsuchiya, A., Williams, A.: QALY maximisation and people’s preferences: a methodological review of the literature. Health Econ. 14, 197–208 (2005)
Treasury, H.M.: The Green Book: Appraisal and Evaluation in Central Government. TSO, London (2003)
Shah, K.K., Tsuchiya, A., Wailoo, A.J.: Valuing health at the end of life: an exploratory preference elicitation study. OHE Research Paper 11/06. Office of Health Economics, London (2011)
ONS: 2001 Census: standard area statistics (England and Wales). http://www.neighbourhood.statistics.gov.uk/dissemination/ (2001). Accessed 1 June 2012
Baker, R., Bateman, I., Donaldson, C., Jones-Lee, M., Lancsar, E., Loomes, G., et al.: Weighting and valuing quality-adjusted life-years using stated preference methods: preliminary results from the Social Value of a QALY Project. Health Technol. Assess. 14, 1–162 (2010)
Wailoo, A., Tsuchiya, A., McCabe, C.: Weighting must wait: incorporating equity concerns into cost-effectiveness analysis may take longer than expected. Pharmacoeconomics 27, 983–989 (2009)
Lancsar, E., Louvriere, J.: Conducting discrete choice experiments to inform healthcare decision making: a user’s guide. Pharmacoeconomics 26, 661–677 (2008)
Longson, C., Littlejohns, P.: Update Report on the Application of the ‘End-of-Life’ Supplementary Advice in Health Technology Appraisals. NICE, London (2009)
Acknowledgments
This article is based on work funded by the National Institute for Health and Clinical Excellence through its Decision Support Unit. The views, and any errors or omissions, expressed in this article are of the authors only. We are grateful for the contributions of Meindert Boysen, John Brazier, Bérengère Davin, Simon Dixon, Jenny Dunn, Karen Gerard, Arne Risa Hole, Jonathan Michaels, Bhash Naidoo, Janet Robertson, Andrew Stevens, Aurélia Tison and Rebecca Trowman. We would also like to thank all of the respondents who took part in the study.
Author information
Authors and Affiliations
Corresponding author
Appendix
Appendix
Excerpt from interviewer script (description for scenario S1)
Consider two patients, patient A and patient B. Both patients are adults, and are the same age as each other. Suppose that both patient A and patient B have just been diagnosed with illnesses. The illnesses are asymptomatic – that is, they have no effect on the patient’s health-related quality of life.
Patient A will live for 10 years, from today, before dying. Patient B will live for 1 year, from today, before dying.
There is a treatment, which, if taken today, would extend the life of either patient A or patient B by 6 months. Treatment would not affect either patient’s health-related quality of life. However, the health service has only enough funds to treat one of the two patients, and there are no alternative treatments available. Furthermore, the nature of the illnesses is such that further treatment will not be possible if either patient is not treated today–this is the only opportunity for treatment.
Please complete the questions for Scenario 1.
Excerpt from participant booklet (diagram and table for scenario S1)
See Fig. 1.
-
1.
If the health service has only enough funds to treat one of the two patients, which of the following statements best describes your view? (tick one box only)
-
□ I would prefer the health service to treat patient A
-
□ I have no preference
-
□ I would prefer the health service to treat patient B
-
-
2.
Which of the following statements reflect the reason(s) for your answer to question 1? (tick all boxes that apply)
-
□ My choice delivers the largest benefit
-
□ My choice is the most fair
-
□ My choice delivers the benefit today rather than far away in the future
-
□ My choice benefits the patient who is closest to death
-
□ My choice benefits the patient who has longer left to live
-
□ My choice benefits the patient with less time to prepare for death
-
□ My choice benefits the patient who can make the most out of their remaining time
-
□ My choice benefits the patient who is worse off
-
□ My choice benefits the patient who is younger today
-
□ My choice benefits the patient who is older today
-
□ My choice benefits the patient who will die at a younger age
-
□ My choice benefits the patient who will die at an older age
-
□ I think that it is better to improve health than to extend life in this situation
-
□ I think that it is better to extend life than to improve health in this situation
-
□ I think that both patients are equally deserving of treatment
-
□ I think that it is unfair to choose between the patients
-
□ I am unwilling to choose between the patients
-
□ None of the above.
-
Rights and permissions
About this article
Cite this article
Shah, K.K., Tsuchiya, A. & Wailoo, A.J. Valuing health at the end of life: an empirical study of public preferences. Eur J Health Econ 15, 389–399 (2014). https://doi.org/10.1007/s10198-013-0482-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10198-013-0482-3