Abstract
Background
Attention deficit hyperactivity disorder (ADHD) is one of the most common behavioural disorders among children and adolescents. The number of patients as well as prescriptions to treat this disease has continuously increased over the past few years. The aim of the present study was to analyse the costs for treating ADHD patients from the perspective of a major German health insurance fund.
Methodology
Anonymised administrative claims data were available for the study. All services reimbursed by the health fund for the selected ADHD patients were recorded. Apart from the resource use attributed directly to ADHD, co-morbidities as well as incremental costs were described based on a control group design.
Results
A total of 30,264 ADHD patients were diagnosed in 2008. The total costs for these patients were €3,888, and the incremental costs were €2,902. The largest proportions of incremental costs were due to therapeutic devices and remedies like occupational therapy amounting to €1,270. Proportionate costs of €263 have been settled for pharmacotherapy with Methylphenidate and Atomoxetine. However, 41 % of the patients were not treated with ADHD-related pharmaceuticals.
Conclusions
ADHD costs are relevant from health insurance perspective. The expenses for occupational therapy constitute the cost driver. Compared to the findings of studies from the United States and contrarily to the backdrop of public discussions about considerably increased prescriptions of ADHD-specific drugs, the significantly higher additional expenses for occupational therapy services are impressing. This kind of therapy is internationally rather unknown and is therefore not acknowledged as a therapeutic standard.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Background
Attention deficit hyperactivity disorder (ADHD) is one of the most common behavioural disorders among children and adolescents. It is a chronic disorder with considerable restrictions for the affected patients. ADHD can be diagnosed in case of inattentive and impulsive behaviour in combination with or without obvious hyperactivity which does not depend on the patient’s age or stage of development and which leads to clear negative effects in social relationships as well as at school and in occupation [1].
Depending on data collection method and diagnostic criteria, the estimates of prevalence of ADHD in childhood and adolescence vary from 2 to 10 % [2]. In 2008, approximately 407,000 insurees of the German Statutory Health Insurance (SHI) suffered from ADHD and were treated with drugs related to ADHD [3]. The number of patients with ADHD as well as the number of prescriptions has continuously increased over the past few years [4].
The costs of ADHD are increasing, and simultaneously resources are limited within the German healthcare system [5, 6]. Nevertheless, systematic cost analyses based on health economic methods have rarely been performed in Germany. However, considering the growing economic impact and the limitation of resources in the health sector, detailed cost analyses are gaining increased practical relevance. Detailed information on particular cost components is just an important evidence on individual and structural causes of variances in the utilisation of healthcare services. Based on cost-of-illness studies, quantitative relations can be demonstrated and are considered as a basis information for evidence-based decisions for allocations in health care [7].
The aim of the present study was to calculate the costs of treating ADHD patients from the perspective of a major health insurance fund based on claims data.
Methodology
Data and study population
Anonymised claims data of a major German health insurance fund (Techniker Krankenkasse) with approximately 6.3 million insurees in 2008 were available. The study population includes all insurees with at least one inpatient ADHD diagnosis (ICD-10 F90.0, F90.1, F90.8 and F90.9) or at least one secured outpatient ADHD diagnosis (diagnosis in the data set with the additional attribute “secured”) in two different quarters of 2008.
Complete claims data of all identified patients for the year 2008 were extracted. Besides individual information regarding age, gender, and comorbidity, detailed information was available on a patient-related basis for the following resource and cost domains:
-
Outpatient care: All services supplied to non-hospitalised patients by medical doctors or accredited psychotherapists in private practice.
-
Inpatient care: All services supplied to hospitalised patients.
-
Pharmaceuticals: Prescribed by medical doctors (only prescriptions filled by patients).
-
Therapeutic devices and remedies: Prescribed by medical doctors but provided by other therapists for instance occupational therapists (in Germany, occupational therapy incorporates types of behavioural therapy).
-
Rehabilitation: In Germany, rehabilitation is often prescribed subsequent to a hospital stay to allow full recovery.
-
Sick leave payments: Payment for patients unable to work longer than 3 weeks.
All available information from the different healthcare settings could be linked via an anonymised identification number for each patient.
Calculation of costs and control group design
Since the perspective of a health fund was used in this analysis, all resource use and costs in connection with ADHD, including all co-morbidities, were taken into account. Co-payments or out of pocket payments by patients are not relevant from this perspective as they do not have an impact on the budget [8]. Average direct costs were analysed separately by cost domain in order to be able to calculate and identify potential cost drivers. In addition, overall healthcare costs were calculated as a sum of all domains.
It is necessary that the analysis focuses only on those resource consumption which stay in relationship to ADHD. Hence, the costs of patients with ADHD were compared to a 1:5 matched control group adjusted for age and gender using an incremental approach for the disease-specific costs. An adequate consideration of all co-morbidities and concomitant diseases is possible with this approach. Since reliable information on the importance of ADHD-related co-morbidities is not available in Germany, this comparison additionally serves as quantification of the increased occurrence in patients with ADHD.
The basic analysis includes patients of all age groups due to the fact that a broad consensus in ADHD-specific research exists that this disorder should not be restricted to certain age groups [4]. Nevertheless, additional subgroup analyses were performed for the age groups newborn to 5 years, 6–18 years and ≥18 years to examine the particularities of the total costs and the payments for individual types of costs. The classification of age groups is largely justified by the existing approval of relevant pharmaceutical products and the frequency of diagnoses in school age [9].
In Germany, there are special valuation practices for the outpatient sector based on weighted points instead of direct monetary payment. Therefore, an accurate monetary assessment of outpatient services is very complex [10]. In 2008, points usually invoiced were indicated instead of monetary resource use. For monetary evaluation, currently valid points were attributed according to the Uniform Valuation Scheme (EBM). Thus, a uniform average value per point is usually used for comparison [11]. Following the Kassenärztliche Bundesvereinigung [National Association of Statutory Health Insurance Physicians], a uniform orientation value of €0.035 per point was assumed for the present study [12].
Results
A total of 30,264 patients with ADHD were identified with the described inclusion criteria. The mean age of these patients was 15 years, and the proportion of male patients was 76 %.
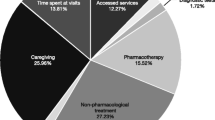
In 2008, the mean overall direct costs amounted to €3,888 (see Table 1). Therapeutic devices and remedies accounted for the largest proportion of the total costs with an amount of €1,704 (44 %). However, the costs for outpatient treatment (22 %), hospital treatment (20 %) and medication (12 %) were relevant. The costs for sick leave and rehabilitation were low on average but can also be remarkable in certain cases.
On average, the age- and gender-adjusted control group of 151,320 insurees without an ADHD diagnosis had lower reimbursement payments in all cost categories. The difference in mean costs accounted for additional treatment expenses for ADHD patients due to their medical condition. In 2008, these incremental costs added up to €2,902 on average per patient in all cost categories (Table 2). The costs for therapeutic devices and remedies accounted for the largest proportion of €1,270. Of these costs, €971 were for occupational therapy.
The average additional expenses for pharmaceuticals amounted to €359 with €263 being attributed to medication for ADHD with the agents Methylphenidate and Atomoxetine. The remaining additional drug costs of €97 mainly arised from the treatment for concomitant diseases. A total of 12,497 patients (41 %) did not receive any specific ADHD drug therapy.
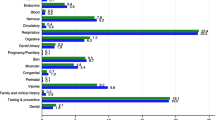
ADHD is associated with several of co-morbidities which may have an effect on treatment costs. Based on a control group approach, it is possible to analyse medical conditions which patients with ADHD suffer from more frequently than the age- and gender-adjusted control group. “Specific Developmental Disorders of Scholastic Skills” (diagnosis F81*) were diagnosed in 4,609 ADHD patients (15.23 %) (Table 3). However, only in 1,816 patients (1.20 %) of the control group this diagnosis appeared. Based on these percentages, the odds ratio to get diagnosed with disorders of scholastic skills is almost 15.
Subgroup analyses
Table 4 summarises the distribution of 30,264 ADHD patients over three age groups and the respective mean costs within the different sectors.
As expected, the group of newborn to 5-year-old patients formed the smallest group with 552 patients (2 %) of all ADHD patients identified in this study. These patients were 5 years old on average, and the proportion of male patients was 78 %. In the age group of 6–17 years, 24,268 ADHD patients (80 %) were identified. The average age of these patients was about 12 years, and the proportion of male patients was 79 %. The group of patients with an age of 18 years and older consisted of 5,444 insurees (18 %). On average, these patients were 34 years, old and the proportion of male patients was 62 %.
Only the newborn to 5-year-old patients differed significantly from the basic analysis in relation to mean total costs. The costs in the ADHD group and the control group (€6,284 vs. €1,656) as well as the ADHD-specific costs (€4,628), respectively, were markedly higher than in the other groups.
See Fig. 1 for the differences in ADHD-specific costs among the three age groups for the most important types of costs on the basis of the control group comparison. Therapeutic devices and remedies constituted the largest cost factor both in absolute terms and as ADHD-specific costs. However, expenses in this service sector were considerably lower within the older age groups.
Next to inpatient and outpatient treatments, medication expenses ranked fourth in all subgroups. As expected, they were significantly higher for the group of 6- to 17-year-old patients. In this subgroup, the average additional expenses for medication amounted to €354 with €295 to be attributed to medications for ADHD with the agents Methylphenidate and Atomoxetine. The remaining additional pharmaceutical spending of €59 arised from treatment for concomitant diseases. A total of 8,484 ADHD patients (35 %) in the group of 6- to 17-year olds have not received any disease-specific pharmaceutical treatment.
For the newborn to 5-year-old patients, the mean additional expenses for medication amounted to €76 of which €9 were be assigned to medical treatment for ADHD. With the ≥18-year olds in the ADHD group, the mean additional expenses for medication amounted to €413 and a proportion of €142 were related to ADHD-specific medication. The proportion of those patients without pharmaceutical treatment was equal to 93 % in the group of newborn to 5-year olds and equal to 64 % in the group of ≥18-year olds.
The evaluation of co-morbidities confirmed the differences for the subgroups as shown in Table 5. For instance, there was a growing tendency towards the following co-morbidities within older age groups: “Specific Developmental Disorders of Scholastic Skills (F81.*)”, “Phobic Anxiety Disorders” and “Other Anxiety Disorders” (F40.*, F41.*), as well as “Injury, Poisoning and Certain Other Consequences of External Causes (S00–T98)”.
Discussion
From an international perspective, there are several studies which analysed the costs of ADHD [13–22]. To date, a cost-of-illness analysis on ADHD has not yet been published for Germany in a scientific journal. A paper published in a conference contribution shows considerably lower costs for 2003 than those calculated in the present study [23]. The total costs of ADHD patients were €622 as compared to €244 in an age- and gender-adjusted control group. However, these findings did not include key cost categories such as therapeutic devices and remedies which were not available in the data set.
ADHD costs are relevant from the perspective of a German health fund. The expenses for therapeutic devices and remedies constitute the cost driver. The advantages of this study are the reflection of a large national sample of a major health fund as well as the description of real healthcare services based on claims data. The calculated consumption of resources represents the de facto costs for health insurance funds. This is a key advantage of SHI claims data compared to other primary and secondary sources for health economic cost analyses from the health insurance perspective.
Compared to former evaluations of claims data, the non treatment-specific inclusion criterion for ADHD patients is a major advantage [24]. It has become apparent that 41 % of the patients did not receive any pharmaceutical therapy. 35 % of the group of 6- to 17-year-old ADHD patients were not treated with drug therapy. Consequently, patient identification via medication would be too limited for an overall analysis of the costs of illness.
Against the backdrop of public discussion on considerably increased prescriptions of ADHD-specific medication, significantly higher costs for therapeutic devices and remedies in the present analysis are particularly interesting. A large part of these costs has to be attributed to occupational therapy. This form of therapy is internationally rather unknown or acknowledged as therapeutic standard for children or adolescents with ADHD.
While other studies are based on the expert adjustment of the total costs by eliminating all non-disease-related costs, [25, 26] the present study calculates the incremental costs of ADHD by means of a comparison to a control group adjusted for age and gender. The key advantage of this study design is the inclusion of all disease-related costs from the perspective of a health fund. The analysis of the concomitant diseases and co-morbidities underlines the importance of this segment for the disease of ADHD. The control group comparison can thus prevent an underestimation of the economic disease burden.
As expected, the developmental disorders of scholastic skills with an odds ratio of nearly 15 were most impressing among the co-morbidities of patients with ADHD. However, a higher frequency of injury associated with ADHD is also mapped. Although the subgroup analysis of the 6- to 17-year-old patients (80 % of all ADHD patients) reveals that these patients clearly suffer less from psychological concomitant diseases, the corresponding odds ratios of the control group comparison largely match. Nonetheless, it must be ascertained that ADHD co-morbidities could more often be encoded since these patients are under regular medical treatment and the corresponding co-morbidities can thus more frequently be diagnosed than in the control group.
Apart from the advantages mentioned, this study has some limitations. The demographical data do not include any further socio-economic information such as income and social status of the insurees. Assuming that the control groups differ with respect to these parameters which additionally may influence reimbursement costs, an adjustment only for age and gender would be insufficient. Clinical data, such as disease severity, are not yet available in the data of German health insurance funds. Furthermore, drugs prescribed in hospital are directly included in hospital remuneration and is not listed separately in the claims data of health insurance funds.
Due to very different accounting practices in the particular administrative districts of the National Associations of SHI physicians, the monetary assessment of the invoiced Uniform Value Scale points presents challenges. The monetarisation of the points was enabled on a calculated mean value. However, the point values for outpatient medical treatment may differ from the mean value in some regions. The effects of the current budgeting of outpatient services are not considered either.
In summary, this is the first study to represent an ADHD cost calculation including consumption of resources based on a broad database of approximately 6.3 million insurees with the inclusion criterion ADHD. A comprehensive design of the control group (1:5 matching) of more than 150,000 insurees without ADHD allows a reliable calculation of incremental costs. Further research will show if this approach can be considered superior compared to classic cost analysis calculating indication-specific costs.
References
Arbeitsgemeinschaft ADHS der Kinder- und Jugendärzte e.V. (Hrsg.) [ADHD Association of Paediatricians and Adolescent Medical Doctors, registered association (publisher)]. ADHS bei Kindern und Jugendlichen (Aufmerksamkeits-Defizit-Hyperaktivitäts-Störung) - Leitlinie der Arbeitsgemeinschaft ADHS der Kinder- und Jugendärzte e.V [ADHD in Children and Adolescents (Attention Deficit Hyperactivity Disorder)––Guideline of the ADHD Association of Paediatricians and Adolescent Medical Doctors, registered association]. Updated Version January (2007)
Alm B. ADHS bei Erwachsenen: Wenn Zappelphilipp erwachsen wird. [ADHD in Adults: If Fidgeting Will Develop.] Dtsch Med Wochenschr (2009); 134, Nr. 24
ABDA (Hrsg. [publisher]) – Bundesvereinigung Deutscher Apothekerverbände: Pressemitteilung 30. März (2009). [Federal Union of German Associations of Pharmacists: Press Release 30th March (2009)]. www.abda.de [Download 22/07/2011]
Sachverständigenrat zur Begutachtung der Entwicklung im Gesundheitswesen [Advisory Council on the Assessment of Developments in the Health Care System]. Gutachten 2009 des Sachverständigenrates zur Begutachtung der Entwicklung im Gesundheitswesen - Koordination und Integration Gesundheitsversorgung in einer Gesellschaft des längeren Lebens [Report 2009 of the Advisory Council on the Assessment of Developments in the Health Care System––Coordination and Integration––Health Care in an Ageing Society]. Köln: Bundesanzeiger Verlag (2009)
Schöffski, O., Sohn, S., Happich, M.: Die gesamtgesellschaftliche belastung durch die hyperkinetische störung (HKS) bzw. Aufmerksamkeitsdefizit-/hyperaktivitätsstörung (ADHS). Gesundheitswesen 70, 398–403 (2008)
Wehmeier, P.M., Schacht, A., Rothenberger, A.: Change in the direct cost of treatment for children and adolescents with hyperkinetic disorder in Germany over a period of four years. Child. Adolesc. Psychiatr. Mental. Health. 3, 3 (2009). doi:10.1186/1753-2000-3-3
Schöffski, O.: Grundformen gesundheitsökonomischer evaluationen [Basic forms of health economic evaluations]. In: Schöffski, O., von der Schulenburg, J.M. (eds.) Gesundheitsökonomische Evaluationen, 3rd edn, pp. 65–94. Springer, Berlin (2007)
Greiner, W., Schöffski, O.: Grundprinzipien einer wirtschaftlichkeitsuntersuchung [Basic principles of economic studies]. In: Schöffski, O., von der Schulenburg, J.M. (eds.) Gesundheitsökonomische Evaluationen, 3rd edn, pp. 167–191. Springer, Berlin (2007)
Ärzteblatt (Hrsg. [publisher]). G-BA: ADHS-Medikamente auch für Erwachsene [Joint Federal Committee: ADHD Medication for Adults as Well]. Available at URL: http://www.aerzteblatt.de/nachrichten/46378/G-BA_ADHS-Medikamente_auch_fuer_Erwachsene.htm [Download 19/07/2011]
Holle, R., Behrend, C., Reitmeir, P., John, J.: Methodenfragen der Nutzung von GKV-Routinedaten für kostenanalysen [Methodological questions on the use of SHI routine data for cost analyses]. In: Swart, E., Ihle, P. (eds.) Routinedaten im Gesundheitswesen: Grundlagen, Methoden und Perspektiven, pp. 301–318. Huber, Bern (2005)
Prenzler A, Zeidler J, Braun S, von der Schulenburg JM. Bewertung von Ressourcen im Gesundheitswesen aus der Perspektive der deutschen Sozialversicherung [Assessment of health care resources from the viewpoint of the German social insurance]. PharmacoEconomics––German Research Articles 2010; 8(1): 47–66
Kassenärztliche Bundesvereinigung (Hrsg.)]National Association of Statutory Health Insurance Physicians (publisher)]. Beschluss des erweiterten Bewertungsausschusses gemäß §87 Abs. 4 SGB V in seiner Sitzung am 23. Oktober 2008 zur Anpassung des Einheitlichen Bewertungsmaßstabs (EBM) sowie zur Neuordnung der vertragsärztlichen Vergütung im Jahr 2009 [Decision of the Extended Valuation Committee Pursuant To Section 87 Paragraph 4 SGB V [Social Security Code V] in its meeting on 23rd October 2008 on the Adjustment of the Uniform Value Scale as well as the Reorganisation of Remunerating SHI Physicians in 2009] Available at URL: http://www.kbv.de/8157.html [Download 19/07/2011]
Guevara, J., Lozano, P., Wickizer, T., Mell, L., Gephart, H.: Utilization and cost of health care services for children with attention-deficit/hyperactivity disorder. Pediatrics 108, 71–78 (2001)
Leibson, C.L., Katusic, S.K., Barbaresi, W.J., Ransom, J., O’Brien, P.C.: Use and costs of medical care for children and adolescents with and without attention-deficit/hyperactivity disorder. JAMA 285(1), 60–66 (2001)
Chan, E., Zhan, C., Homer, C.J.: Health care use and costs for children with attention-deficit/hyperactivity disorder: national estimates from the medical expenditure panel survey. Arch. Pediatr. Adolesc. Med. 156, 504–511 (2002)
Burd, L., Klug, M.G., Coumbe, M.J., Kerbeshian, J.: Children and adolescents with attention deficit-hyperactivity disorder: 1. prevalence and cost of care. J. Child Neurol. 18, 555–561 (2003)
Leibson, C.L., Long, K.H.: Economic implications of attention-deficit hyperactivity disorder for healthcare systems. Pharmacoeconomics 21, 1239–1262 (2003)
Swensen, A.R., Birnbaum, H.G., Secnik, K., Marynchenko, M., Greenberg, P., Claxton, A.: Attention-deficit/hyperactivity disorder: increased costs for patients and their families. J. Am. Acad. Child Adolesc. Psychiatr. 42(12), 1415–1423 (2003)
Birnbaum, H.G., Kessler, R.C., Lowe, S.W., Secnik, K., Greenberg, P.E., Leong, S.A., Swensen, A.R.: Costs of attention deficit-hyperactivity disorder (ADHD) in the US: excess costs of persons with ADHD and their family members in 2000. Curr. Med. Res. Opin. 21(2), 195–205 (2005)
Matza, L.S., Paramore, C., Prasad, M.: A review of the economic burden of ADHD. Cost. Eff. Resour. Alloc. 3, 5 (2005). doi:10.1186/1478-7547-3-5
Ray, T.G., Levine, P., Croen, L.A., Bokhari, F.A.S., Hu, T.W., Habel, L.A.: Attention-deficit/hyperactivity disorder in children- excess costs before and after initial diagnosis and treatment cost differences by ethnicity. Arch. Pediatr. Adolesc 160, 1063–1069 (2006)
Pelham, W.E., Foster, M.E., Robb, J.A.: The economic impact of attention deficit/hyperactivity disorder in children and adolescents. J. Pediatr. Psychol. 32(6), 711–727 (2007)
Schlander, M., Trott, G.E., Schwarz, O.: Gesundheitsökonomie der aufmerksamkeitsdefizit-/hyperaktivitätsstörung in Deutschland -Teil 1: Versorgungsepidemiologie und krankheitskosten [The health economics of attention deficit hyperactivity disorder in germany. part 1: health care utilization and cost of illness]. Nervenarzt 81(3), 289–300 (2010)
Gebhardt B, Finne E, von Rahden O, Kolip P, Glaeske G, Würdemann E. ADHS bei Kindern und Jugendlichen––Befragungsergebnisse und Auswertungen von Daten der Gmünder ErsatzKasse [ADHD in Children and Adolescents––Survey Results and Evaluation of Data of the Gmünder ErsatzKasse]. Schriftenreihe zur Gesundheitsanalyse, Band 65. St. Augustin: Asgard-Verlag (2008)
Ruof, J., Hülsemann, J.L., Mittendorf, T., Handelmann, S., von der Schulenburg, J.M., Zeidler, H., Merkesdal, S.: Costs of rheumatoid arthritis in Germany: a micro-costing approach based on healthcare payer’s data sources. Ann. Rheum. Dis. 62(6), 544–549 (2003)
Wu, E., Chen, L., Birnbaum, H., Yang, E., Cifaldi, M.: Cost of care for patients with rheumatoid arthritis receiving TNF-antagonist therapy using claims data. Curr. Med. Res. Opin. 23(8), 1749–1759 (2007)
Conflict of interest
The mission of the Scientific Institute of the TK for Benefit and Efficiency in Health Care (Wissenschaftliches Institut der TK für Nutzen und Effizienz im Gesundheitswesen, WINEG) is to investigate the value of innovations and new programmatic approaches within the statutory health insurance framework. The authors Prof. Dr. Roland Linder, Dr. Susanne Engel and Dr. Frank Verheyen declare that because they belong to the Techniker Krankenkasse, a potential conflict of interest exists according to the guidelines of the International Committee of Medical Journal Editors.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Braun, S., Zeidler, J., Linder, R. et al. Treatment costs of attention deficit hyperactivity disorder in Germany. Eur J Health Econ 14, 939–945 (2013). https://doi.org/10.1007/s10198-012-0440-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10198-012-0440-5