Abstract
Background
Increased population flowing from abroad has generated an intense debate regarding the economic consequences of migration in public services such as health, where new and specific demands are being created. This new demand for health care gives rise to the need to identify those factors which influence the user’s decision to contact the health services and those which determine the quantity of services consumed. The aim of this study is to identify which variables affect these two stages of the use of such services in the Girona Health Region (RSG), where immigrant population represents 21.96% of the total population.
Methods
Specification of a Hurdle model with a count response variable related to primary health care service visits in the RSG for 2006. The study data is based on a sample of users (immigrants and natives) taken from the population assigned to primary health care services in eight Basic Health Areas (ABS) of the RSG.
Results
Contacting primary health care services is associated with variables that ought to affect use of health care such as chronic illness and taking prescribed medication as well as being aged between 46 and 55. Using primary health care services once makes users more likely to make further visits. The number of visits is related not only with variables that ought affect use of health care but also with variables that ought not to affect use of health care such as working without a contract, living in rented accommodation, or being unemployed. Additionally, if we consider the birthplace of the user, we observe the same pattern, with different directions and intensities, depending on the origin of the patient. For example, a higher likelihood of first contact is shown in Eastern Europeans, South Americans, and North Africans that suffer from cholesterol. A higher attendance is observed in natives and Eastern Europeans that take prescribed medication as well as natives, Eastern Europeans, and North Africans living in rented accommodation. On the other hand, working without a contract supposes a higher attendance in natives but a lower attendance in Eastern Europeans and sub-Saharan Africans.
Conclusions
We do not detect any socioeconomic barriers associated with making a first contact with primary health services for the users analyzed. However, we do note evidence of horizontal inequity in terms of attending health services, related to variables that ought to affect use of health care as well as socioeconomic factors (variables that ought not to affect use of health care). The user’s origin is an important key in detecting different intensities of access and regular visits to primary health care services.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Economic migrations are linked to the differences existing between countries in terms of income and quality of life. These international migrations comprise population flows from lower income countries to higher income countries and they place the immigrant within a completely new social, cultural, working, and living environment which, sometimes, leads to a situation of social segregation. Recent studies in the field of immigration and health consider that inequalities in social and economic factors between individuals in the host country determine the differences in morbidity attended and the use of health services between immigrants and the native population. Once integrated into their new reality immigrants tend to identify and adopt the behavior of the native population; however, certain restrictions related to education, employment, culture, communication, or legislation generate different behaviors in the morbidity attended and utilization of health services [1, 2]. Because factors related to personal situation of each individual are elements that determine morbidity attended and health care services use [3], comparative studies on morbidity attended and on the use of health services by immigrants and natives need to take into account a whole range of social, economic, demographic, and epidemiological variables, as well as the individual’s country of origin [4, 5].
The Catalan health care system is a public financing system with universal coverage guaranteed by the National Health Service (CatSalut). It is a mixed model that integrates into a single network of public use, all health and social resources (whether or not publicly owned). The purchase of these services is made by providers of primary care (Primary Attention Centers—CAP-) and by organizations that provide specialized care and other services (hospital care, healthcare, mental health, drugs, or pharmaceuticals). The deployment of the regional structure of the Catalan Health system is in seven Health Regions (RS). Each RS is subdivided into areas of health that usually cover between 200,000 and 250,000 inhabitants. The health region contains several Basic Health Areas (ABS), each one with its own Primary Care Team (EAP). This is the first point of contact between the population and the health system.
Increased population flowing from abroad [6], the progressive aging of the native population, and the high birthrate among the immigrant population have generated a new social and demographic reality in Spain [7], where new and specific demands in public services (education and health) are being created [8, 9]. In 2010, the regular foreign population in Spain was 14%. Catalonia, receives 19.94% of new arrivals, a figure which represents 17.45% of its total population. The province of Girona receives 12.61% of the immigrants that reside in Catalonia, which represents 21.96% of the total population [10]. In Girona Health Region (RSG), this has meant an increased population who uses health system. In January 2008, about 725.000 inhabitants were users of health care system.[11].
Health systems should ensure that individuals with the same level of health need receive the same amount of service, without other external factors constraining the use of these services. Therefore, in defining equity, it is usual to distinguish between need variables (that ought to affect use of health care) and non-need variables (that ought not to affect use of health care) [12]. Factors related to own health (being ill, requiring preventive consultation, taking prescribed medicines, etc.) and modifiers of these factors (i.e., age and gender) should affect the use of health services. In contrast, characteristics unrelated to own health should not affect the use of these services (cultural, social, or economic factors) [13].
Because need for care must be distinguished from the demand for care and from the use of health services [14], one of the most common ways of explaining the decision-making process in the consumption of health care are principal-agent models [15]: the doctor (agent) determines use on behalf of the patient (principal), after the latter has made initial contact with the health services [16–18]. So, from a quantitative viewpoint, what is important is to identify which factors influence the user’s decision to contact the health services, and which elements determine the quantity of service consumed.
For this reason, our main hypothesis is that, having monitored for age and gender, while making the first contact to health services is determined only by need variables, demanded quantity (number of visits) depends on both need and non-need variables. Thus, we believe that horizontal equity exists in first contact to health services but it does not exist in frequency of visits.
This study has a dual objective. First, to characterize demographic, social and economic profiles, morbidity attended and use of primary health services for the diverse collectives of the immigrant and native populations residing in the RSG. Second, to produce a theoretical model for determining factors that influence first contact to and frequency of use of health services, monitoring the age, gender, and origin of the patient.
Subjects and methods
Data and variables
The study data are taken from a non-proportional random stratified sample of 575 users (340 immigrants and 235 natives) of the primary health services in eight ABS of the RSG (See Table 1). Information regarding explanatory variables (demographic, social and economic factors as well as health status) is obtained from a questionnaire administered in person to these users [19]. Data regarding the response variable (number of visits made during 2006 for each user interviewed) is obtained from the e-Cap, the medical history computer program used in primary health care in Catalonia [20]. Although the questionnaire is anonymous, the Health Care Identification Number (NIA) is obtained for each interviewed user. The definitive database used for the analysis, links the information gathered from the questionnaire (explanatory variables) with data regarding frequency of visits for each user (explained variable) on the basis of the personal identifier [21].
Estimation models and methods
All of the information analyzed corresponds to users of the primary health care services, who may have had one or more contacts with these health services. Therefore (and in line with the principal—agent theory), we suppose that initial contact with these services depends solely on need variables or, if not, due to moderators of these (age and gender). On the other hand, the use of these services more than once is also influenced by non-need variables [16, 18, 22, 23] (See Table 2).
This reasoning led us to use a two-part model. The first part studies factors that have a greater or lesser influence on likelihood of making the first contact with primary health care services. The second part analyzes factors that have a greater or lesser effect on frequency of visits for those users who have made use of the service more than once. Note that the response variable is a count variable, which is why, in this case, the model is called a Hurdle model [24]. Thus, the model to be estimated is specified as follows:
where Y is the response variable, i.e., the number of contacts with the AP services; \( \Pr \left( {Y = 1} \right) \) refers to the likelihood of making only one contact and is modeled by a logistic regression in the first part of the Hurdle model, i.e., the Use pattern Eq. 1; X refers to the group of j need variables and moderators of these; Z refers to the group of k non-need variables; \( \mu_{ij} \)is the expected conditional mean of the response variable, modeled as a Poisson in the second part of the Hurdle model, i.e., the Frequency of use pattern Eq. 2; the β refers to the coefficients of the model, with the subindex j for the need variables and moderators and with the subindex k for the non-need variables; \( \beta_{0} \) refers to the basal effect; and finally, the subindex i denotes the individual.
The special feature offered by this model is that it introduces the heterogeneity associated with the origin of the user through a normal random effect \( \beta^{\prime}_{0l} = \beta_{0l} + \eta_{l} \), where \( \eta_{l} \to \left( {0,\tau_{\eta } } \right) \). This modification allows us to collect the group effects that are not explained by the explanatory variables of the model (those that depend uniquely on the patient’s origin). In this way, we define two models. First, a Fix Effects Model Eq. 1 and 2, which refers to the likelihood of making the first contact and to the factors that have a greater or lesser effect on frequency of visits regardless of the origin of the user. Second, a Random Effects Model Eq. 3 and 4 , which shares the same approach as the Fix Effects Model, but takes into account the origin of the user. Note that the baseline effect has only been supposed as random effect in the second part of the model Eq. 4 due to problems with identification [18].
Due to the multiple advantages it provides within the context of this study, the aforementioned models are estimated using the Bayesian approach [25]. In this case, we use the complete Bayesian approach, with a priori conjugated distributions and a numerical integration based on Markovian Chain Monte Carlo methods (MCMC). One of the simplest algorithms for designing these chains is the “Gibbs Sampling” algorithm introduced by Geman and Geman [26, 27], and one of those used by the WinBUGS program [28]. Due to its iterative form, the convergence of simulations (the speed at which the distribution of the parameter of interest resembles the a posteriori distribution [25]) allows us to validate the results obtained with the complete Bayesian method [29]. Graphically, convergence is detected when the graphical representation of simulations is distributed randomly around a constant mean. Analytically, it is observed when the Brooks–Gelman–Rubin statistic (known as R-hat) is close to the unit [30]. Once iterations converge, effectiveness is checked by carrying out additional iterations and observing that the standard Monte Carlo error (or MC error) is less than 5% of the standard deviation of a posteriori estimation of a parameter of interest [25].
Results
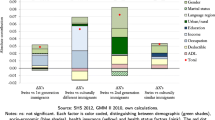
Table 3 shows the factors that influence making the first contact with primary health care services (Use pattern), and the factors that influence the quantity of service consumed (Frequency use pattern) without considering the origin of the user (Fix Effects Model). This demonstrates that only need variables influence the decision to make the first contact. Specifically, having cholesterol problems and having consumed tranquilizers the 2 days prior to the interview represents a greater likelihood of using health services (13,838.3 and 823.1%, respectively) in comparison with individuals who do not have this type of chronic illness and/or behavior with regard to pharmaceuticals. By contrast, we observe that both, need and non-need variables (and moderators of both), influence the quantity of service consumed. With regard to need variables, the factors influencing a greater likelihood of more frequent visits are related to suffering chronic diseases (such as cholesterol–39.2%- or allergies–23.5%-), taking drugs (taking prescribed medication–26.3%- or tranquilizers–35.9%-), and perceiving one’s own health as being poor (30.0% or more). With regard to non-need variables, a greater likelihood of more frequent visits are linked with working without a contract (17.0%), living in rented accommodation (23.8%) or with friends (52.5%), being unemployed (10.0%) or being disabled (66.8%). Moreover, less likelihood of more frequent visits is associated with doing household chores (9.9%) or being a student (22.3%). Finally, for the moderator variables, it is observed that the mere fact of using the health services represents a greater likelihood of more frequent visits (307.7%), as do being aged 46–55 (22.0%) and having arrived in Spain after 1986, the longer the period of residence, greater is the likelihood of more frequent visits (13.8% for more recent immigrants—1996/2000—and up to 55.2% for earlier ones—1986/1990).
Tables 4 and 5 show the same information as Table 3, but introduces contextual information related to the patient’s specific area of birth (Random Effects Model). In the use pattern, we continue to observe the fact that only need variables and moderators of these influence the decision to make the first contact with the primary health services, although only for some specific groups. Thus, those individuals who demonstrate a greater likelihood of making this first contact are those from North Africa who perceive their health to be poor (1929.1%), Eastern Europeans, South Americans, and North Africans suffering from cholesterol (711.9, 612.9 and 824.4%, respectively) and natives who had taken prescribed medication in the 2 days prior to the interview (110.5%). With regard to the moderator variables, a greater likelihood of use is observed in native women (82.7%) and in immigrants from North Africa who arrived between 1986 and 1990 (1,176.7%). By contrast, in the frequency pattern, it is observed that frequency of visits to primary health services is influenced by both need and non-need variables and their moderators, although only for specific groups. There is a greater likelihood of more frequent visits among natives and North Africans who perceive their health to be poor (135.7 and 276.4%, respectively); in natives, Eastern Europeans and South Americans who have problems with cholesterol (14.5, 93.9, and 246.2%, respectively); in natives and Eastern Europeans who had taken medication in the 2 days prior to the interview (72.4 and 42.7%, respectively); and in natives, South Americans, and Central Americans who took tranquilizers (34.1, 49.7 and 157.9%, respectively). There is less likelihood of more frequent visits among Eastern European and Central American immigrants who consider their own health to be poor (75.8 and 96.8%, respectively). With regard to non-need variables, a greater likelihood of more frequent visits is observed among unemployed natives (79.8%); Eastern European and sub-Saharan immigrants who do household chores (34.0 and 60.5%, respectively); South Americans working without a contract (81.9%) and natives, Eastern Europeans and South Americans living in rented accommodation (31.9, 19.5 and 19.6%, respectively). There is a lesser likelihood of more frequent visits among natives and North Africans who do household chores (20.2, 23.3, respectively); sub-Saharan and North Africans without an employment contract (45.2 and 30.3%, respectively) and Central Americans living in rented accommodation (40.7%). With regard to moderator variables, greater likelihood of more frequent visits is detected among native, South American, and sub-Saharan women (26.9, 21.0 and 93.6%, respectively); in native, South American, and North African users aged 46–55 (12.6, 73.8 and 53.7%, respectively); and in South and Central American and sub-Saharan African immigrants who arrived between 1986 and 1990 (50.8, 155.5 and 132.1%, respectively). By contrast, Central American and sub-Saharan African users aged between 46 and 55 demonstrate less likelihood of frequent visits (34.8 and 25.9%). Finally, it is again observed that once the contact with health services has been made, the likelihood of more frequent visits is evident in all users, no matter what their origin is. However, this likelihood is higher in patients from North Africa (504.4%) and lower among Eastern Europeans (207.5%).
Discussion
From the results presented here, we can conclude that the factors influencing first contact with health services depend solely on need variables and their moderators, whether we consider the population as a whole or groups with specific origins. In other words, we have not found any access barriers in the decision of the principal (the patient), because contacting the health services depends exclusively on morbidity and perception of one’s own health.
However, if we analyze quantity of services consumed, all variables come into play—need variables, non-need variables, and their respective moderator variables—whether we consider the population as a whole or specific users groups. For the population as a whole, a greater use is clearly associated with worse morbidity and a worse perception of health on the one hand, and a worse working situation and home ownership conditions on the other. This pattern repeats itself when we also take into account the specific origin of the patient, with the occasional exception. African workers in a more precarious labor situation, Central Americans in a worse situation with regard to home ownership, and natives and North Africans who do household chores display less likelihood of more frequent visits. Finally, for the moderator variables, we observe that the older the immigrants are and the longer they have been resident in the host country, the greater likelihood of use, which also applies to native, South American and sub-Saharan women.
In summary, although first contact with health services does not display problems of horizontal inequity, the quantity of health resources consumed does suffer from this problem, for both the population as a whole and for some particular user groups, but with varying intensities. Due to the fact that we have found the greatest likelihood of more frequent visits in those individuals with the lowest socioeconomic capacities (for both groups of immigrants and for native users), it is reasonable to think that when more frequent visits (and specialized treatment) are required, users with greater spending power use alternative private services [18, 21]. Equally plausible is the theory that a poor socioeconomic situation means worse morbidity and therefore a greater need for use.
On the basis of the surveys administered (regarding use of the health service, morbidity, demographic and socioeconomic variables) to people who have used the primary health service at least once, and through application of the principal-agent theory using a two-part model, we have been able to separately identify those factors which exercise greater influence on first contact with the health service and those which influence the quantity of service consumed while taking into account the origin of the patient studied.
References
Ministerio de Trabajo e inmigración: Permanent observatory of immigrantion [In Spanish]. Anuario estadístico de la inmigración (2007). Available on: http://extranjeros.mtas.es
Scheppers, E., van Dongen, E., Dekker, J., Geertzen, J., Dekker, J.: Potential barriers to the use of health services among ethnic minorities: a review. Family Pract. 23, 325–48 (2006)
Duran, A., Lara, J.L., van Waveren, M.: Spain: health system review. In: Health systems in transition, vol.8, issue 4 (2006)
Jansà, J.M., García de Olalla, P.: Health and immigration: new situations and challenges [In Catalan]. In: Borrell C, Benach J. (eds) Inequalities in health in Catalonia [In Catalan]. Barcelona (2003)
Costa, J., Garcia, J.: Demand for private health insurance: how important is the quality gap? Health Econom. 12, 587–599 (2003)
Ministerio de Sanidad y Consumo. National Health System. Health Statistics [In Spanish]. Available on: http://www.msc.es/estadEStudios/estadisticas/sisInfSanSNS/home.htm
Balanzó, X., Faixedas, M.T., Guayta, R.: Immigrants and their health [In Catalan]. Quaderns de bona praxis. 16(3), 5–13 (2003)
Saura, R.M., Suñol, R., Vallejo, P., Lahoz, S., Atxotequi, J., Monouari, M.: The health care and social environment of the North African immigrant population in Catalunya [In Spanish]. Gac. Sanit. 22(6), 547–554 (2008)
Cots, F., Castells, X., García, O., Riu, M., Felipe, A., Vall, A.: Impact of immigration on the cost of emergency visits in Barcelona (Spain). BMC Health Serv. Res. 19, 7–9 (2007)
Instituto Nacional de Estadística (INE). Continuous Population Census. Genuary 2010 [In Spanish]. Available on: http://www.ine.es
Servei Català de la Salut. Annual report of CatSalut activities, 2008 [In Catalan]. Available on: http://www10.gencat.cat/catsalut
Elgar, E., Gravelle, H.C., Morris, S., Sutton, M.: Econimic studies of equity in the consumption of health care. In: Jones, A.M. (ed). Elgar companion to health economics, pp. 193–204. Edward Elgar, London (2006)
Clavero Barranquero, A., González Álvarez, M.L.: A review of econometric models applied to the analysis of demand and utilization of health services [In Spanish]. Hacienda Pública Esp. 173, 129–62 (2005)
Matthew, G.K.: Measuring need and evaluating services. In: G McLachlan (ed), Portfolio for health, 6th Series. Oxford University Press, London
Zweifel, P.: Supplier—induced demand in a model of physician behaviour. In: van der Gaag, J., Perlman M. (eds) Health, economics, and health economics. North Holland, Amsterdam (1981)
Deb, P., Trivedi, P.K.: The structure of demand for health care: latent class versus two-part models. J. Health Econom. 21, 601–625 (2002)
Pohlmeier, W., Ulrich, V.: An econometric model of the two part decision-making process in the demand for health care. J. Human Resour. 30, 339–361 (1995)
Saez, M., Saurina, C., Coenders, G., González-Raya, S.: Use of primary health care services according to the different degrees of obesity in the Girona health region, Spain. Health Econom. 15, 173–193 (2006)
Saurina, C., Saez, M., Coromina, L.l., Pons, J.C., Vall-llosera, L.: “Survey of health status and utilization of health services in the Girona Health Region” [In Catalan]. Intellectual Property Registry. Application number: GI-197-07. Filing and effect date: 15/06/2007
Gené, J., Marzo, M.: Clinical leadership in the primary organization [In Catalan]. Fulls Economics Sist. Sanit. 37,29–32 (2003)
Vall-llosera, L., Saurina, C., Saez, M.: Immigration and health: needs and utilization of primary health care services by immigrants in the Girona Health Region [In Spanish]. Rev. Esp. Salud Pública. 83,291–307 (2009)
Gerdtham, G.: Equity in health care utilization: further tests based on hurdle models and swedish micro data. Health econom. 6, 303–319 (1997)
Álvarez, B.: The attended demand of medical consultations and emergy services in Spain [In Spanish]. Investigaciones Económ. XXV (1), 93–138 (2001)
Mullahy, J.: Specification and testing of some modified count data models. J. Econom. 33, 341–65 (1986)
Best, N.: Bayesian approaches to cancer survival analysis. Short course on cancer survival: principles, methods and applications. London, 3–7 April (2006)
Geman, S., Geman, D.: Stochastic relaxation, Gibbs distributions and the Bayesian restoration of images. IEEE Trans. Pattern Anal. Mach. Intell. 12, 609–628 (1984)
Gelfand, A.E., Smith, A.F.M. Sampling-based approaches to calculating densities. J. Am. Stat. Assoc. 85, 398–409 (1990)
Brooks, S., Gelman, A.: Some issues in monitoring convergent of iterative simulations. In: Proceedings of the Section on Statistical Computing, ASA. (1998). Available on: http://citesser.ist.psu.edu/brooks98some.html
Barceló, M.A, Saez, M., Cano-Serral, G., Martínez-Benito, M.A., Martínez, J.M., Borrell, C., Ocaña-Riola, R., Montoya, I., Calvo, M., López-Abente, G., Rodríguez-Sanz, M., Toro, S., Alcalá, J.T., Saurina, C., Sánchez-Villegas, P., Figueiras, A.: Methods for smoothing mortality indicators: application to the analysis of inequalities in mortality in cities of Spain (MEDEA project) [In Spanish]. Gac. Sanit. 22(6), 596–608 (2008)
Brooks, S.P., Gelman, A., Alternatives methods for monitoring convergence of iterative simulations. J. Comput. Graph. Stat. 7(434), 55 (1998)
Acknowledgments
We express our thanks to the health care and other professionals in the Basic Health Areas of Banyoles, Blanes, Girona 3, Olot, Roses, Salt, Santa Coloma de Farners, and Sarrià de Ter for their involvement and effort in the process of identifying the population and data gathering. Also, we thank the cooperation of Catalan Health Institute in implementing the data gathering software. Finally, we would like to thank two anonymous reviewers that improved a previous version of this work. This study is partially funded by means of the Spanish Health Research Fund (FIS 04/0495 and FIS 07/0156) and the Autonomous Government of Catalonia (AMIC 10025).
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Saurina, C., Vall-llosera, L. & Saez, M. Factors determining access to and use of primary health care services in the Girona Health Region (Spain). Eur J Health Econ 13, 419–427 (2012). https://doi.org/10.1007/s10198-011-0313-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10198-011-0313-3