Abstract
This contribution seeks to measure preferences for health insurance of individuals with and without chronic conditions in two countries, Germany and the Netherlands. The objective is to test the presumption that preferences between these two subpopulations differ and to see whether having a chronic condition has a different influence on preferences depending on the country. The evidence comes from two Discrete Choice Experiments performed in 2005 (Germany) and 2006 (the Netherlands, right after a major health reform). Results point to an even more marked resistance against restrictions of physician choice among individuals with chronic conditions in both countries. Thus, the alleged beneficiaries of Disease Management Programs would have to be highly compensated for accepting the restrictions that go with them.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
This paper considers the preferences with regard to health insurance of individuals with and without chronic conditions in two countries, Germany and the Netherlands. While culturally similar, the two countries differ in their health policy in that the Netherlands had carried out a major pro-competitive reform in 2006 while Germany had introduced new laws and ordnances almost annually in an attempt to keep down the cost of health care. At the same time, there is the belief that preferences for attributes of health insurance strongly depend on health status (one instance of the low-risk/high-risk distinction in the pioneering model by Rothschild and Stiglitz [14]; see also Glazer and McGuire [6]). Empirical evidence bearing on this belief is scarce, however. In this situation, experimental evidence may be of some interest. It comes from two Discrete Choice Experiments (DCE) that were performed in Germany (2005) and in the Netherlands (2006, right after a major pro-competitive reform). In both samples, participants reported whether or not they suffered from chronic conditions.
This information provides an opportunity to simultaneously throw light on two issues. First, is it true that individuals with a chronic condition value attributes of health insurance differently from others? Second, does it matter whether these individuals live in Germany or the Netherlands? This paper is structured as follows. First, it provides some institutional background for the two countries. Next, it introduces readers to the methodology of DCE, providing also information about the design of the two DCE. After the econometric specification, results in the guise of willingness-to-pay values are presented and compared between individuals with and without chronic conditions in the two countries. The last section concludes.
Institutional background
The Netherlands
In 2006, the Netherlands underwent a major healthcare reform. Prior to 2006, public insurance covered 60% of the population, while the remaining 40% had private health insurance [13]. As of January 1, 2006, this division was lifted, with (formerly) public and private health insurers mandated to offer a uniform basic package [12]. At the same time, every Dutch resident had to explicitly choose a health insurance policy by the end of March 31, 2006; silently extending the pre-existing contract was disallowed. However, consumers were free to purchase additional coverage for, e.g., dental treatment or physiotherapy.
Dutch health care is financed from two sources. First, individuals pay annual income-based contributions to the risk adjustment scheme. Employers are required to compensate their employees for these contributions. Second, adults pay premiums directly to their insurer of choice, which sets its own community-rated premium. About two-thirds of Dutch households receive an income-related subsidy from the government—a maximum of €1,464 per household per year [16].
Consumers have the right to form groups (usually through their work place) to obtain a premium reduction of up to 10%. Individuals with chronic conditions have also started groups, but their success importantly depends on whether the disease in question is a factor in the risk adjustment formula [1]. If in addition the group is sizable, insurers are more likely to develop specific products for particular groups of patients, e.g., of diabetes.
In order to neutralize the incentive for risk selection induced by premium regulation, adjustment schemes compensate insurers for taking on high-risk enrollees [19]. Conversely, insurers can compete through product innovations such as Managed Care and Disease Management Programs and by creating and staffing their own facilities. In addition, they may sell other products such as supplementary health insurance or car insurance. Increasingly, these rights will give them greater leverage in negotiating prices, volumes of service, and quality of care.
Since participants in a DCE are made to hypothetically choose between the status quo and an alternative, actual switching behavior is of considerable interest. The opportunity for switching exists with the new system since consumers are free to change their insurer and insurance plan annually. If not satisfied with the premium or quality of care, they are expected to switch to another insurer, exposing insurers to competition for high quality of care at low premiums [4, 9]. De Jong et al. [9] found that while the main reason for the general population to switch was a lower premium, chronically ill patients took both coverage and premium into consideration. Approximately 18% of the Dutch population switched their insurer in 2006 [5]. One reason for the lack of relevance of quality may be that Dutch patients had little choice in the domain of ambulatory care since they were subject to gatekeeping by general practitioners, who decide about prescribing drugs as well as referrals patients to hospital and specialist care [13].
Germany
Germany has the third highest GDP share of health care expenditure among Organization for Economic Co-operation and Development (OECD) countries [15]. The average person made 10.0 physician visits per year in 2006 [15], compared to 7.8 for all European countries and 6.8 for the EU [18].
The last major healthcare reform in Germany occurred in 2000, when members of the statutory health insurance scheme (SHI) obtained the right to choose between sick funds. Since then, there have been minor changes accompanied by heated debate, with politicians striving to keep the rate of contributions paid out of labor income for SHI stable on average. However, the main distinguishing feature was never touched. While high-income earners (with a gross monthly salary exceeding EUR 3,862 as of 2004) can opt out of SHI, those below this threshold are obliged to join one of the 300 statutory sick funds [7]. Approximately 88% of the population are “locked in” with SHI, while 6% are fully covered privately [15, 17]. Another 6% (including civil servants and pensioners) are insured by governmental schemes [15, 17]. One other minor reform worth mentioning, introduced in 2004, is the copayment of EUR 10 per quarter, payable for each initial physician visit (which includes referrals to a specialist unless authorized by a general practitioner).
Methodology of DCE
The premise of the DCE [2] is that rational individuals will always choose the alternative with the higher level of expected utility. The decision is therefore based on a comparison of utility levels attained. Denoting V ij as individual i’s indirect utility given choice j, one typically posits.
Here, a j is a vector of attributes (pertaining to a health insurance contract in the present context), p j is the price (the contribution paid), y i , the individual’s income, and s i , his or her sociodemographic characteristics. The term ε ij is a stochastic variable predicated by the Random Utility Model [11]. This does not mean that decisions are made in a random way; rather, ε ij reflects the fact that experimenters can never observe all determinants of utility. For them, registered choices therefore contain a random element. Also note that in a first step, the function v i (·) is identical across individuals, an assumption that will be relaxed later on. As usual, this function is split up into a systematic component w(·) and an additive error term ε ij . Thus, respondent i will choose contract j rather than contract l if
In stochastic terms, the probability P ij of choosing alternative j rather than l equals the probability of inequality (2) occurring, i.e.,
This can be rearranged to become an inequality involving a stochastic and a deterministic part,
Thus, the choice in favor of j rather than l requires the noise on the left-hand side to be dominated by the systematic utility difference on the right-hand side. Additionally, the utility function is assumed to be linear in the K attributes [8],
The parameters β 1,…,β K can be interpreted as the marginal utilities of the attributes. The marginal rate of substitution between two attributes k and m is given by
with the marginal utilities taken from the estimated utility function. The marginal WTP for a specific attribute amounts to a special type of MRS. Since a variation in the price attribute is the negative of the same variation in disposable income, the marginal WTP of attribute k can be calculated applying Eq. (6), with the denominator given by the derivative w.r.t. price (the contribution in the present context).
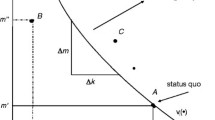
Figure 1 illustrates the case of two attributes, freedom of physician choice (m) and income net of the contribution to health insurance (k). The slope –Δm/Δk of the indifference curve equals MRS k,m . It indicates how much income the respondent is willing to forego in order to obtain more freedom of physician choice, which is nothing but the marginal WTP for that attribute. It can be inferred from choices as follows. Let the experimenter offer combination A. If the respondent opts for A rather than status quo S, then his or her indifference curve runs below A. Next, let the experimenter propose B. If the respondent prefers the status quo S, it must be true that his or her indifference curve is above B. Evidently, repeated choices allow the experimenter to interpolate the indifference curve and to estimate MRS k,m and hence marginal WTP. Accordingly, econometric inference calls for a probit estimation since the dependent variable is either 0 (choosing the status quo) or 1 (choosing the alternative). With respondents making several choices, the data has a panel structure, suggesting a random-effects specification [2, 10].
Experimental design
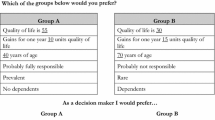
Two different DCEs were designed featuring hypothetical insurance contracts, one for Germany and one for the Netherlands. Each DCE had five attributes plus their levels that include the status quo. This makes for a large number of potential choice sets (see Table 1 for Germany and Table 2 for the Netherlands). Pretests performed in Germany resulted in the attributes listed in Table 1. The survey, involving some 1,000 members of the TNP Panel, was performed in September 2005. Since the number of possible combinations of attribute levels is excessive, the statistical design optimization procedure Gosset was used to reduce their number to 24, which were randomly split into three groups of eight choices each.
In the case of the Netherlands, differences in the status quo suggested two changes from the German DCE (which were verified in a pretest). First, the gatekeeper model had to become the benchmark (see “Institutional background”), with free choice an element of the alternative. Second, in view of the public debate about long waits for obtaining hospital treatment, the attribute “Hospital wait” replaced “Second opinion”, with the wait limited to 4 weeks as a possible element of the alternative. Third, the Dutch already were exposed to variable rebates for no claims in health insurance, which however, could not exceed EUR 255 per year. This value (rather than zero in Germany) was therefore part of the status quo, while EUR 500 per year (as in Germany) was part of the possible alternatives. The main survey was fielded in March 2006, after every resident had explicitly selected a health insurance contract. It involved 763 respondents, again members of the TNP Panel. They had to make eight choices in 3 groups as well.
In both surveys, the questionnaire also contained a number of socioeconomic characteristics in addition to age, sex, and region of residence. In particular, it included four indicators of health status, viz. (1) subjective health (excellent to poor), (2) presence of a chronic condition (subjective), (3) health-related physician visit(s) during the past 12 months, and (4) hospital visit(s) during the previous 12 months.
For the present study, variant (2) was retained for the following reasons. On the one hand, the more objective indicators (3) and (4) are influenced by ease of access to physicians and hospitals, which differ markedly between the two countries. Second, among the subjective indicators, (1) proved less informative than (2) in preliminary investigations, likely because current subjective health status contains a strong transitory component which is absent from the chronic/non-chronic distinction. No less than 32.5% of German respondents stated to suffer from a chronic condition, compared to 27% of their Dutch counterparts.
Econometric specification
First, country-specific core models involving attributes only were estimated. The equation for the Netherlands (NL), e.g., reads
Here, NLPr(Alt) ij denotes the probability of choosing the alternative rather than the status quo in the Dutch sample. Note that all explanatory variables are defined in terms of a difference between the alternative and the status quo. Accordingly, \( \varphi_{ij} = \left( {\varepsilon_{il} - \varepsilon_{ij} } \right) \), as in Eq. (4).
The results from the two country-specific estimations suggested three things. First, both (NLContrib)2 and (GEContrib)2 proved to be insignificant. Therefore, the evidence suggests that in the Dutch (NL) as well as in the German (GE) sample, the marginal utility of income is constant. Second, the interaction variables of the type Attribute*C (with C = 1 if the respondent stated to suffer from a chronic condition) turned out to be significant for the majority of attributes, pointing to systematic differences in the marginal utilities of attributes between the chronic and non-chronic subpopulations. Third, the standard error of the estimate, while somewhat smaller in the Dutch estimate (0.042294 vs. 0.042315) was of a comparable magnitude as the German estimate. These findings support the merging of the two datasets, resulting in the following specification (NL = 1 if the observation relates to the Netherlands),
The following remarks pertain to this specification. First, Physfree is an example of an attribute that is relevant only to the Dutch sample. It therefore only appears interacted with the NL dummy variable. As before, the possible differences between the Dutch chronic and non-chronic subpopulations call for an additional interaction variable, Physfree*NL*C. Physlist is an example of an attribute present in both samples. It is interacted with NL to account for differences in the status quo in Germany (which is Physfree in Germany rather than Gatekeeper as in the Netherlands) with C for differences between the chronic and non-chronic subpopulations, and with NL*C for these differences in the case of the Netherlands. Therefore, the reference group is German non-chronic respondents. Second, it is likely that the attributes retained do not reflect all determinants of utility. These neglected determinants may shift the utility and hence probit function up or down. Apart from age, sex, and the other socioeconomic characteristics, nationality and permanent health presumably play an important role, which is reflected by NL, C, and NL*C.
Estimated parameters from Eq. (8) can be used to derive marginal WTP values. In case of the physician list for the Dutch (NL = 1), chronic (C = 1) respondents, e.g., one obtains, applying Eq. (6),
Analysis of choice behavior
Preliminary analysis suggested that the Dutch were more likely to break away from the status quo in three out of four cases, defined as Dutch vs. German (NL = 0, 1) and with versus without chronic condition (C = 1, 0). The one exception was Dutch and German respondents without a chronic condition, who switched to the alternative with the same frequency. Therefore, Table 4 reports the choice behavior of the two national samples combined. It shows that 20% of respondents never chose the alternative insurance contract. However, among the ones with chronic conditions, this figure reaches 29%. Conversely, about 80% of respondents were flexible in that they switched to the alternative at least once (out of the eight occasions). Even among respondents with chronic conditions, this share amounts to more than 70% and does not go to zero but remains at 2% for the maximum of eight choices of the alternative. In summary, even the chronic subsample “crossed the indifference curve” (see Fig. 1 again) sufficiently often to permit inferences about its slope and location (Table 3).
Overview of WTP values
This section is devoted to a general discussion of the WTP estimates referring to the column entitled, “Combined sample” of Table 4. Focusing on the overlapping attributes first (panel A), one notices that typical MC attributes such as a physician list put together by the health insurer (Physlist) and adherence to a physician network (Network) are rejected by both the Dutch and German respondents. The implied compensation asked for by the Dutch is even higher than by the Germans. This is amazing because the Dutch are familiar with gatekeeping by physicians, and policymakers tend to argue that familiarity fosters acceptance.
Next, additional services provided by the insurer are not really valued by the Dutch respondents (NLServices) but clearly by their German counterparts, at the tune of EUR 123 per year. Both populations agree in their rejection of an annual EUR 500 deductible. However, the Dutch value of EUR -407/year is even more marked than the German (EUR -247/year). Note that a compensation at this tune (through reduced contributions) could easily be financed because the health insurer is relieved not only of EUR 500 but also saves on administrative expense and from mitigation of moral hazard effects (Zweifel et al. [20], Chap. 6.3) Without that compensation, however, it becomes understandable why the Dutch government had to revoke a (non-compensated) mandatory deductible a decade earlier.
The two populations differ again with regard to promoting health-conscious behavior (Bonus). While the Dutch sample does not exhibit a positive WTP value, the German sample values this attribute at some EUR 202 per year.
Finally, the two populations agree in their preference for the status quo. However, status quo bias in the Dutch sample (EUR 260) amounts to only one-half of the German value (EUR 500). A possible reason is that the Dutch respondents had been made to bear the cost of decision-making in the course of the 2006 reform which required them to explicitly choose a health insurance policy. By way of contrast, the Germans had been exposed to a great deal of public debate but were never made to consider alternatives to the status quo. This interpretation is supported by the observation that standard errors of WTP estimates are considerably smaller in the Dutch population in spite of a smaller sample size. This points to greater homogeneity of opinions in the Dutch sample, which may well be the consequence of having borne the cost of information.
Turning to the non-overlapping attributes (panel B of Table 4), their signs and magnitudes are in line with theoretical expectations. First, given that Dutch participants are subject to gatekeeping under the status quo, they see free choice of physician as a utility gain, valued at EUR 75 per year. Conversely, German participants would have to be compensated to give up free physician choice (their status quo) for gatekeeping. Incidentally the required compensation of EUR 115 is in the same order of magnitude as the WTP value for the Dutch to accept the opposite change. Second, the Dutch sample does not exhibit any WTP to deviate from their current rebate for no claims. This can be interpreted to mean that on average, they are satisfied with the EUR 255 value. In the German sample, there is positive WTP for such a high rebate. Since the current value of the rebate is zero, it is not surprising that their WTP value is a high EUR 358. What is not known is whether WTP would be even greater for a smaller value of the rebate than the proposed EUR 500/year.
Dutch individuals with and without a chronic condition compared
It is important to note that the two Dutch subpopulations qualitatively agree on the valuation of all attributes, with the sole exception of the bonus for health-conscious behavior which tends to have a positive WTP value among the group without but a negative value among the group with chronic condition. However, the two estimates are not statistically significant. The two Dutch subpopulations also agree on the magnitude except for one or possibly two attributes. First, status quo bias among individuals with chronic conditions amounts to EUR 355 rather than 229, a statistically significant difference (p < 0.0001). This is importantly due to the fact that the marginal utility of income is low among those with chronic conditions (p < 0.0001). To be worthwhile, an investment requires extended payback time. However, individuals suffering from a chronic condition have lower remaining life expectancy and hence payoff time. Therefore, to them, a change away from the status quo is unlikely to constitute a profitable investment.
The second difference lacks statistical significance but is worth mentioning. There is some indication that participants with chronic conditions would have to be compensated almost twice as much (EUR 116 rather than 65/year) to accept adherence to a physician network. This points to a contradiction with established policy views that advance Disease Management Programs (DMPs) as an innovation benefitting especially the chronically ill. It appears that the potential beneficiaries fear above all the lock-in effect of DMPs which entail physician networks.
German individuals with and without chronic conditions compared
Among German participants, the two subpopulations are again in agreement concerning the qualitative valuation of attributes—this time even without exception. Moreover, there is also agreement concerning WTP values for attributes. The only exception is a significant difference in status quo bias (p < 0.0001). The chronic population requires a compensation amounting to EUR 634 rather than 444 to change away from the status quo, which is about 50% more, very much like their Dutch counterpart (EUR 355 vs. 229). Again, this difference is importantly due to participants’ with chronic conditions exhibiting a significantly lower marginal utility of income (p < 0.0000). Finally, it may be worthwhile to point out that these participants would have to be compensated by a contribution reduction of EUR 444 rather than 322/year for a physician list. It appears that they fear the lock-in effect of such as list even more than the general population, causing them to resist DMPs.
Individuals with a chronic condition: Germany versus The Netherlands
This section addresses the issue of whether persons with chronic conditions have different preferences depending on nationality. When comparing the WTP values for the overlapping attributes shown in panel A of Table 4, one notices that the German subsample generally exhibits higher absolute amounts, with one exception. The Dutch would have to be compensated by as much as EUR 410/year to accept an annual deductible of EUR 500, the Germans, by 278/year. Other differences may be caused by a difference in the status quo. Specifically, starting from gatekeeping, the Dutch sample would require an EUR 98 compensation to go along with a physician list. However, if free choice of physician had been the point of departure, EUR 58 of WTP would have to be added to this figure (assuming that the transition from gatekeeping to free choice is valued the same as the transition from free choice to gatekeeping once status quo bias is controlled for; see panel B). Therefore, changing from free physician choice to an insurer-imposed physician list requires an estimated EUR 156 (= 98 + 58) which still falls short of the EUR 444 in the German sample.
Likewise, the Dutch figure of EUR 116 to compensate for adherence to a physician network would have to be scaled up by EUR 98 to become EUR 214 if free choice had been the status quo. This is quite close to the German figure of EUR 217. Thus, persons with chronic conditions in both countries reject two important Managed Care features, with the Germans even more opposed to a physician list. A marked difference concerns the bonus for health-conscious behavior. Dutch people with chronic conditions do not place positive value on this, whereas their German counterparts would be willing to pay EUR 114. Finally, while status quo bias amounts to EUR 355 among the Dutch participants, it reaches the maximum of EUR 643 among the German participants, again due to a lower marginal utility of income.
Individuals without a chronic condition: Germany versus The Netherlands
Among individuals without chronic conditions, once more the German WPT values are larger, with the exception of the compensation required for accepting an EUR 500 deductible. Such a deductible is rejected as strongly by the Dutch non-chronic as the German non-chronic subpopulation. With regard to the two Managed Care attributes, WTP values of the two countries again have to be adjusted for differences in status quo. Noting that WTP for free choice amounts to EUR 86 in the Dutch sample (see panel B of Table 4), one can estimate the compensation required for accepting a physician list as EUR 236 (=150 + 86), which is not much less than the EUR 322 for the German sample (measured from free choice of physician). In the case of a physician network, the value becomes EUR 151 (=65 + 86), only slightly lower than the EUR 207 estimated for the German sample. As in the case of individuals with chronic conditions, Dutch respondents put a lower value on extra insurer services than the German subsample, and they have no positive WTP for a bonus honoring health-conscious behavior (valued at EUR 196/year by German non-chronic respondents). Finally, status quo bias amounts to EUR 229, less than the EUR 444 in the German sample (p < 0.0012). This is remarkable because the Dutch have a lower marginal utility of income than the German respondents (p < 0.0000), which per se causes WTP values to be high.
Discussion and conclusion
This paper seeks to measure preferences for health insurance attributes as a function of health status in two countries, Germany and the Netherlands. Since observed choices are distorted by regulated contributions that do not reflect the marginal cost of these attributes, market experiments of the Discrete Choice (DCE) type were performed in 2005 (Germany) and 2006 (the Netherlands, right after a health reform), respectively. The two major research questions were (1) Do individuals with a chronic condition (as an indicator of permanent health status) value attributes of health insurance differently from the other? and (2) Do these valuation depend on the country?
With regard to the first question, the answer is clear. In both countries, Managed Care features such as a physician list established by the insurer or a physician network tend to be more strongly resisted by respondents with chronic conditions. This suggests that Disease Management Programs (which typically impose restrictions of this type on participants) may not match the preferences of designated beneficiaries. Moreover, the chronic subpopulations exhibit even stronger status quo bias than their non-chronic counterparts, which would have to be overcome by a compensation as high as EUR 643 in the case of Germany.
As to the second question, yes it does make a difference whether a Dutch or a German person has a chronic condition. Even when measuring the Dutch WTP values from free physician choice (the German status quo), estimates point to less resistance to a physician list in the Netherlands than in Germany. Also, Dutch persons with a chronic condition do not value additional services provided by the health insurer whereas the Germans do. On the other hand, they resist an EUR 500 annual deductible even more strongly than their German counterparts, the required compensation reaching EUR 410/year. This is in accordance with the fact that the Dutch government had to repeal the introduction of a (non-compensated) deductible a decade earlier. Also, Dutch status quo bias amounts to an estimated EUR 355, clearly lower than the EUR 643 cited above for the Germans. Since a similar difference holds true for the non-chronic subpopulations as well, it may well be due to the Dutch 2005/6 reform, which made citizens explicitly choose their health insurance contract.
There are a few limitations to this study that need to be pointed out. First, the non-chronic German subpopulation exhibits systematically lower WTP values than the Dutch counterpart. This is due to their significantly higher marginal utility of income [see Eq. (6) again]. A possible explanation is that this reflects the fact that the non-chronic German subpopulation is financially better off than the Dutch (while chronic populations have similar income levels).
Second, there is the difficulty that for between-country comparisons, WTP values need to be measured from a common status quo. However, it is unclear whether the Dutch value a change from gatekeeping to free physician choice (which was part of the DCE) the same way as from free physician choice to gatekeeping, although status quo bias was controlled for. The reason is that changing one single attribute likely evokes a status quo bias different from changing all of them [an issue addressed by so-called effects coding, see Beck and Gyrd-Hansen [3]].
In spite of these limitations, however, two results stand out. First, Managed Care restrictions typically imposed as part of Disease Management Programs tend to be resisted especially by those with chronic conditions, the designated beneficiaries. Second, deductibles would have to be compensated in both countries and in both subpopulations. These findings do not forebode well for policy makers who consider introducing Disease Management Programs or copayments without making a binding commitment in the guise of reduced health insurance contributions or taxes.
References
Bartholomee, Y., Maarse, H.: Empowering the chronically ill? Patient collectives in the new Dutch health insurance system. Health Policy 84(2–3), 162–169 (2007). doi:10.1016/j.healthpol.2007.03.008
Ben-Akiva, M., Lerman, S.R.: Discrete choice analysis. MIT Press, Cambridge, Mass (1985)
Beck, M., Gyrd-Hansen, D.: Effects coding in discrete choice experiments. Health Econ. 14, 1079–1083 (2005). doi:10.1002/hec.984
Cunningham, P.J., Denk, C.: Do consumers know how their health plan works? Health Aff. 20(2), 159–166 (2001). doi:10.1377/hlthaff.20.2.159
Douven, R., Lieverdink, H., Ligthart, M., Vermeulen, I.: Measuring short-term price elasticities in Dutch health insurance: a new method (June 14, 2007). iHEA 2007 6th World Congress: Explorations in Health Economics Paper. Available at SSRN: http://ssrn.com/abstract=993741
Glazer, J., McGuire, T.: Optimal risk adjustment in markets with adverse selection: an application to managed care. Am. Econ. Rev. 90, 1055–1071 (2000)
Green, D., Benedict, I.: Health care in France and Germany: lessons for the UK. Civitas, Institute for the Study of Civil Society, London (2005)
Hensher, D., Louviere, J., Swait, J.: Combining sources of preference data. J. Econom. 89, 197–231 (1999). doi:10.1016/S0304-4076(98)00061-X
de Jong, J.D., Van den Brink-Muinen, A., et al.: The Dutch health insurance reform: switching between insurers. A comparison between the general population and the chronically ill and disabled. BMC Health Serv. Res 8, 5 (2008). doi:10.1186/1472-6963-8-58
Louviere, J.L., Hensher, D.A., et al.: Stated choice methods. Analysis and applications. Cambridge University Press, Cambridge, Mass (2000)
McFadden, D.: Conditional logit analysis of qualitative choice behavior. In: Zarembka, P. (ed.) Frontiers in econometrics, pp. 105–142. Academic Press, New York (1974)
Ministry of Health, Welfare and Sports (2008, February 25, 2008), Health insurance system, Retrieved 29 April 2008
Okma, K.G.H.: Health care, health policies and health care reforms in the Netherlands. Ministry of Health, The Hague (2001)
Rothschild, M., Stiglitz, J.: Equilibrium in competitive insurance markets. An essay on the economics of imperfect information. Q. J. Econ. 90(4), 629–649 (1976). doi:10.2307/1885326
Schreyögg, J., Markus, G.: Copayments for ambulatory care in Germany: a natural experiment using a difference-in-difference approach, SOEP paper (96). German Institute for Economics, Berlin, Germany (2008)
Schut, F.I.: Universal mandatory health insurance in the Netherlands: a model for the United States? Health Aff. 27(3), 771–781 (2008). doi:10.1377/hlthaff.27.3.771
Tamm, M., Tauchmann, H., Wasem, J., Greß, S.: Elasticities of market shares and social health insurance choice in Germany: a dynamic panel data approach. Health Econ. 16(3), 243–256 (2007). doi:10.1002/hec.1167
WHO: Health for all Database, World Health Organization (2008)
Zweifel, P., Breuer, M.: The case for risk-based premiums in public health insurance, health economics. Policy Law 1(2), 171–188 (2006)
Zweifel, P., Breyer, F., Kifmann, M.: Health economics, 2nd edn. Springer, Boston (2009)
Acknowledgments
Helpful suggestions and criticisms were provided by participants of the Ottobeuren 2008 workshop (in particular Stefan Felder) as well as Harry Telser and Karen Becker (Polynomics Inc.), and Stephanie Berner (University of Zurich). Financial support by the Bertelsmann Foundation and Büchner Foundation is gratefully acknowledged.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Vroomen, J.M., Zweifel, P. Preferences for health insurance and health status: does it matter whether you are Dutch or German?. Eur J Health Econ 12, 87–95 (2011). https://doi.org/10.1007/s10198-010-0248-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10198-010-0248-0