Abstract
This paper estimates the financial cost of skin cancer in England. National Health Service (NHS) costs were calculated by combining published data on health service use by patients with skin cancer with published data on the unit cost of services. Indirect costs arising from individuals’ inability to function in their usual role as a result of skin cancer were estimated from incapacity benefit claims and numbers of registered deaths due to skin cancer. The total costs of skin cancer were around £240 million. Costs to the NHS represented 42% of the total.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Skin cancer is one of the most common forms of cancer in the United Kingdom (UK), with recent figures suggesting an annual incidence of at least 70,000 cases [1–4], and accounting for at least 20% of all cases of cancer [1]. This is almost certainly an underestimate because registration of non-melanoma skin cancer is incomplete and it is estimated that the actual number of skin cancer cases in the UK each year is at least 100,000. There are in excess of 2,000 deaths from skin cancer each year in the UK, of which around three-quarters are due to malignant melanoma [2, 4, 5]. Evidence shows that cases of malignant melanoma have increased by a larger amount than many other major cancers in recent years, and that the incidence has more than doubled since the early 1970s [6]. Given the sizable number of cases of skin cancer and the increased number of cases in recent times there is a growing interest in skin cancer prevention in the UK. For instance, the SunSmart campaign is a UK-wide skin cancer campaign commissioned by UK health departments in 2003 and run by Cancer Research UK [7]. Its activities include the provision of evidence-based information about skin cancer and sun protection for the general public and health professionals. This includes campaigning to raise awareness about the magnitude of the burden of skin cancer and strategies to reduce this burden.
In additional to raising awareness about the health impacts of skin cancer, it is also informative to consider its financial cost, to the health service, to patients, and to the wider economy. That is the aim of this study: to estimate the financial cost of skin cancer in England. A search of the National Health Service (NHS) Economic Evaluations Database [8] reveals this to be the first study to estimate this figure. Cost analyses of skin cancer have been undertaken in other countries, but these have tended to focus on one aspect of skin cancer, such as non-melanoma skin cancer only [9, 10].
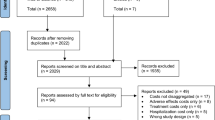
Methods
The cost of skin cancer comprises costs to the NHS, costs incurred by patients in the receipt of care, and indirect costs arising from people’s inability to work due to their illness. The latter are based on lost working days due to skin cancer morbidity (called here indirect morbidity costs), and lost working life years due to deaths from skin cancer (indirect mortality costs). We do not explicitly consider indirect costs caused by reduced health related quality of life due to skin cancer, though this will be captured in part in the indirect morbidity costs.
NHS costs are calculated using data on the number of general practitioner (GP) consultations, inpatient stays, day cases, and outpatient visits due to skin cancer. Unit costs are taken from published national sources and applied to each category to give an overall estimate of the cost to the NHS of skin cancer. We use routinely available data sources that are commonly used in UK economic evaluations.
The perspective for the analysis is societal, in that both NHS and wider costs are included. All costs are reported in 2002 UK pounds sterling (£). Where appropriate, future costs are discounted into present value terms at a rate of 3.5%, which is the rate recommended by the National Institute for Health and Clinical Excellence (NICE) [11].
Costs are estimated separately for two classifications of skin cancer defined using the ninth and tenth revisions of the International Classification of Diseases (ICD-9 and ICD-10, respectively): malignant melanoma (ICD-9 code 172, ICD-10 code C43); and other malignant neoplasms of the skin (173 and C44, respectively).
GP consultations
Annual rates of total GP consultations for skin cancer per new case were obtained from Morbidity Statistics from General Practice by ICD-9 code for 1991–1992 [12]. These rates were then applied to 2001 data on the incidence of skin cancer based on comparable ICD-10 codes from Cancer Statistics: Registrations [1]. It is known that skin cancer registration data by cancer registries in England are incomplete, which means that the true incidence will be underestimated using these figures [13]. A study by Stefoski Mikeljevic et al. [14] conducted in one region of England showed that 87.5% of individuals with malignant melanoma and 83.1% of individuals with non-melanoma skin cancer were registered—i.e., 12.5 and 16.9% of cases, respectively, were not included in the registrations data. Stefoski Mikeljevic et al. show that these proportions are similar to those in earlier studies undertaken in other parts of the UK and we therefore apply their estimates to registrations data for the whole of England: we multiplied the incidence data for malignant melanoma and for other malignant neoplasms of the skin by adjustment factors 1.14 (=100/87.5) and 1.20 (=100/83.1), respectively to adjust for incomplete registrations. The rates of total GP consultations for skin cancer per new case were multiplied by the adjusted incidence data to give the number of GP consultations associated with skin cancer. The cost of GP consultations was obtained by multiplying the number of consultations by the unit cost per consultation, taken from the Unit Costs of Health and Social Care [15].
Inpatient stays and day cases
The number of hospitalisations for skin cancer by ICD-10 code were taken from Hospital Episodes Statistics [16] in three categories: inpatient emergency admissions; inpatient elective admissions; and day cases. The total cost of each type of hospitalisation was then calculated using data from NHS Reference Costs 2002 [17]. This is a national database of costs based on returns from NHS hospital trusts and is based on healthcare resource groups (HRGs), which are a systematic classification of interventions into categories that are clinically distinct and that also have similar resource implications. We multiplied the number of admissions of each type by the mean cost per admission of each type using HRG code J43 (major skin tumours), which is the only code that relates explicitly to malignant skin tumours.
Outpatient attendances
Outpatient attendance data for all attendances in England were recently made available in Hospital Episodes Statistics. The recording of ICD-10 codes is incomplete. We therefore calculated the proportion of all attendances where an ICD-10 code was recorded that were attributable to skin cancer. We then multiplied the total number of outpatient attendances by this proportion to estimate the total number of outpatient attendances that were attributable to skin cancer. Note this assumes that the non-reporting of ICD-10 codes is equally as unlikely for skin cancer cases as for other diseases. The cost of skin-cancer-specific outpatient attendances was then calculated by multiplying the number of outpatient attendances due to skin cancer by the unit cost calculated from NHS Reference Costs 2002 [17]. A number of unit costs are listed for outpatient attendances related to skin cancer in the Dermatology HRG label (codes J01op to J10op). The unit cost used was the weighted mean of these where the weights were the proportion of the total attendances charged under each HRG code reported in the reference cost database.
Costs incurred by patients receiving treatment
Costs incurred by patients in the receipt of treatment for skin cancer include travel costs and costs associated with lost earnings from time off work. These items were computed for each component of NHS costs.
National unit costs incurred by patients when attending a GP consultation were taken from the Unit Costs of Health and Social Care [15]. These include the weighted mean loss of waged and non-waged time (based on the proportion of patients who are economically active) plus travel costs. Note that these costs do not overlap with the indirect morbidity costs (considered below), since the latter pertain to absences from work of more than 3 days. This cost was multiplied by the number of GP consultations for skin cancer to give the total costs incurred by patients for GP skin cancer consultations.
Unit costs incurred by patients for hospitalisations were based on Kernick et al. [18], who report average transport costs and economic inactivity costs incurred by patients from GP consultations and outpatient attendances. For inpatient admissions we include only the travel cost component based on the estimates for outpatient attendances because the economic activity costs of inpatient admissions are considered in the indirect morbidity costs (see below). Travel costs for inpatient admissions were calculated by multiplying the unit travel costs given in Kernick et al. [18] by the number of hospital inpatient emergency and elective admissions. Patient costs incurred for day case treatment were based on average patient transport costs and economic inactivity costs for outpatient attendances reported in Kernick et al. [18]. The unit patient costs were multiplied by the relevant number of each type of hospital attendance to estimate the total patient costs associated with hospitalisations.
Patient costs for outpatient attendances were calculated by multiplying the unit costs reported in Kernick et al. [18] by the number of skin cancer outpatient attendances.
Indirect costs
Indirect costs of skin cancer arise when individuals with skin cancer are unable to function in their usual role as a result of their illness. This is manifested by their inability to work, arising from skin cancer morbidity and mortality and skin cancer treatment.
Morbidity costs
Morbidity costs were based on the total number of days of registered incapacity benefit for the period 1 April 1 2001 to 31 March 31 2002 for the diagnosis of skin cancer, based on ICD-10 codes. The data were obtained on application from the Department of Work and Pensions by age and sex groups. They do not include absences from work of 3 days or less because Statutory Sick Pay of this duration is paid by employers. This means that total absences from work due to skin cancer may be underestimated. It also means that the economic inactivity costs associated with GP, outpatient visits and day cases described above will not be double-counted in these data since they pertain to a period of less than 4 days. Time off work due to inpatient admissions may be greater than 3 days and so to avoid double counting we only include patient travel costs in these unit costs (see above). This will underestimate the costs from time off work due to inpatient admissions where the length of stay is less than 4 days. The figures in each group were multiplied by age- and sex-specific mean daily wages from the New Earnings Survey for 2002 reported in the Annual Abstract of Statistics [19].
Mortality costs
The number of deaths in England and Wales due to skin cancer were obtained by age and sex groups from Mortality Statistics: Cause [5]. The figures were adjusted to values for England by multiplying the number of deaths in each age and sex category by the proportion of the population of England and Wales living in England, reported in the Annual Abstract of Statistics [19]. The state retirement age in England is currently 65 years for males and 60 years for females. Using this threshold, residual years of working life assuming full employment were computed by subtracting age at death from the gender-specific state retirement age. The data were then adjusted for the proportion of males and females in employment taken from the Labour Force Survey reported in the Annual Abstract of Statistics [19] and the residual years of working life estimates were then discounted into present value terms. The discounted employment adjusted years of residual working life lost due to skin cancer mortality were then multiplied by annual earnings data from the New Earnings Survey reported in the Annual Abstract of Statistics [19] to give the indirect mortality costs associated with skin cancer. Note that this cost component focuses on years of working life lost and does not include all residual life years lost.
Results
Registrations
According to cancer registry data there were 56,456 new registrations of skin cancer, of which 11% were for malignant melanoma (Table 1). Of these, 52% of cases occurred in males, and 71% of cases were in individuals who were older than the state retirement age (65 years for males, 60 years for females). There were 275,044 new registrations of all cancers combined across all ages and both sexes; registered skin cancers therefore accounted for 20% of the total.
NHS costs
After adjusting for incomplete registry data, there were an estimated 67,571 new cases of skin cancer, of which 6,928 were malignant melanomas and 60,643 were for other malignant neoplasms of the skin. The annual GP consultation rate per new case was 3.43 for malignant melanoma and 1.78 for other malignant neoplasms of the skin on average across all age groups. Hence, the predicted number of GP consultations was 131,880, of which 23,755 were for malignant neoplasms and 108,126 were for other malignant neoplasms of the skin. The unit cost per GP consultation was £20, and therefore the total NHS cost of GP consultations was £2.6 million.
There were 14,000 inpatient admissions and 49,000 day cases due to skin cancer, incurring a total NHS cost of £24.9 and £13.5 million, respectively.
The number of outpatient attendances due to skin cancer was estimated to be 907,000. The weighted mean cost per attendance was £67 and hence the estimated cost was £60.5 million.
The resulting costs of skin cancer borne by the NHS were estimated to be £101.6 million (Table 2). The cost of each component and the proportion of total NHS costs attributable to each component are also shown. Of the total cost to the NHS, 20% is due to malignant melanoma, which is greater than the percentage of new cases (11%) suggesting that malignant melanoma is relatively more costly to the NHS than other skin cancers.
Costs incurred by patients receiving treatment
The mean cost incurred by a patient when attending a GP consultation was £6.90, and the private costs of GP consultations were £0.9 million. The mean cost per patient was £4.18 for inpatient admissions and £19.16 for day cases (the former includes travel costs only, the latter also includes economic inactivity costs) and hence the private costs were estimated to be £0.06 and £0.9 million, respectively. The mean cost per patient for an outpatient attendance was £19.16 and hence the private costs were £17.4 million. The total patient costs were £19.3 million, which is 19% of the magnitude of the NHS costs.
Indirect morbidity costs
Claimant data for incapacity benefit indicate that 218,000 working days were lost as a result of skin cancer. This results in total lost earnings of £20.9 million.
Deaths from skin cancer and indirect mortality costs
The estimated number of deaths from skin cancer is 1,819 (Table 1). This represents just over 1% of all 132,378 cancer deaths. Of these, 77% of skin cancer deaths were due to malignant melanoma. 54% of all deaths from skin cancer occurred in males, and 67% of deaths occurred in individuals past the normal retirement age. Deaths from skin cancer were estimated to result in the loss of an estimated £98.2 million (Table 2).
Total cost
The total cost of skin cancer in England in 2002 is estimated to be approximately £240 million. NHS costs account for 42% of the total, with the remainder being attributable to patient costs (8%), indirect morbidity costs (9%) and indirect mortality costs (41%). Fifty-eight percent of the total cost of skin cancer is due to malignant melanoma.
By dividing the total cost by the number of adjusted registrations it is possible to estimate the mean cost per case. The mean cost to the NHS per case of malignant melanoma is £2,945, and the mean total cost is £19,981. Mean costs for other malignant skin neoplasms are £1,339 and £1,673, respectively.
Conclusions
In this study, data from routine published English sources have been used to calculate the cost of skin cancer in England in 2002. NHS costs, including costs incurred for GP consultations, inpatient stays, day cases and outpatient attendances, are estimated to be £101.5 million per annum. Since most skin cancers are caused by damage from ultraviolet rays in sunlight, the majority of cases are thought to be preventable [7]. If these cases were avoided then, to put this into perspective, with the amount of money calculated in this study that is spent on skin cancer each year it would be possible to employ around an additional 650 hospital consultants for 1 year [15], or to employ an additional 2,900 E-grade nurses for 1 year [15]. To further highlight the relative cost of skin cancer, Liu et al. [20] compare the NHS cost of selected diseases in the UK. Converting their results to 2002 prices using the NHS Pay and Prices Index [15] and to figures for England on the basis of the resident population [19], we find that the annual NHS costs associated with skin cancer are greater than those for multiple sclerosis (£75 million) and migraine (£40 million).
The cost of skin cancer to the NHS in England is considerable, though it represents a relatively small proportion of total NHS expenditure on all cancers. Bosanquet and Sikora [21] report that total annual expenditure on all cancers in the UK NHS is £2,105 million. Converting this estimate to figures for England on the basis of the resident population [19] means that around £1,800 million is spent annually on cancer in the English NHS. Skin cancer accounts for around 4% of this total, yet it accounts for at least 20% of all cases of cancer [1]. A similar finding has been reported in the United States for non-melanoma skin cancer [10]. This might be explained by the fact that skin cancer is managed efficiently and effectively, and that many skin cancers can be treated on an outpatient basis, not requiring the need for expensive inpatient care. An alternative explanation is that, on average, skin cancers tend to be less lethal than other cancers and typically require less aggressive, primarily outpatient-based management. Both views are supported by the observations from Table 1 that while skin cancer accounts for at least 20% of all cases of cancer it accounts for only around 1% of all cancer deaths.
It is likely that the cost estimates presented in this paper have been underestimated for a number of reasons. First, GP consultations for skin cancer were costed using the rate of consultations per case taken from general morbidity statistics from 1991 to 1992 [12]. Given the general trend for the increased use of health services over time, this number is likely to be an underestimate. Second, the estimated costs of skin cancer exclude certain aspects of patient management. This is due to the lack of availability of reliable estimates of the health resource use for certain cost components, such as home visits by GPs and the cost of contacts with other members of the primary care team. Third, it is recognised that the incidence of non-melanoma skin cancers in England is underestimated [13]. However, it should be borne in mind that the NHS costs are based on health service contacts by disease code, and so it is unlikely that the under-reporting of new cases will have an impact on these figures.
The analysis also considers patient costs associated with the receipt of care for skin cancer, and the indirect costs. Indirect costs represent the value of lost production to society, and the human capital approach is used. This approach computes the lost income from the time that patients are absent from work because of sickness, and the lost future income due to premature mortality. A criticism of the human capital approach is that it discriminates against those who are not in employment. This is especially relevant in the case of skin cancer, since the majority of cases occur in individuals of retirement age or older—in this analysis no indirect cost is calculated for such individuals. Furthermore, the indirect morbidity estimates were derived from the number of lost days using incapacity benefit claims data made by employers classified by diagnostic codes for skin cancer. Claims for incapacity benefit underestimate the actual number of working days lost, since they do not include short periods of sickness of 3 days or less of Statutory Sick Pay, which are payable by employers. Note also that the number of days off work from skin cancer due to diagnoses other than malignant melanoma were reported by the Department of Work and Pensions as being nil or negligible (numbers are reported to the nearest 1,000 days). The upshot is that, taken in combination, it is likely that the NHS and total cost estimates presented in this study will probably underestimate the true cost of skin cancer in England.
Caveats notwithstanding, there appears to be little doubt that skin cancer is a major public health issue, and it is hoped that the figures presented in this paper motivate research interest and resources to address the problem of skin cancer, in particular from an economics perspective. It is also worth pointing out that while cost of illness studies of the kind presented here are useful as a means of providing summary figures for the magnitude of the impact of a particular disease, they are unlikely to be useful for setting priorities in terms of funding for treatment and prevention. Of more use for this purpose are cost-effectiveness analyses, which take into account the costs and benefits associated with specific interventions aimed at treating and preventing a particular problem. A good example in the case of skin cancer is the evaluation of a national skin cancer primary prevention campaign by Carter et al. [22], which demonstrates that a comprehensive, well-funded national skin cancer health promotion campaign would prove excellent value for money from the perspective of the Federal government in Australia. Studies are being undertaken to assess similar programmes in other countries, e.g. the United States [23]. Unfortunately, cost-effectiveness analyses in the treatment and prevention of skin cancer are few and far between, with none focussing on the UK [8]. This is lamentable given the importance of skin cancer as a growing public health problem in the UK.
References
Office for National Statistics: Cancer statistics: registrations, series MB1 No. 32. Office for National Statistics, London
ISD Online: Information and Statistics Division, NHS Scotland. http://www.isdscotland.org/isd/1048.html. Accessed 26 June 2008
Welsh Cancer Intelligence and Surveillance Unit: Cancer incidence 2002 report. Welsh Cancer Intelligence and Surveillance Unit (2004)
Northern Ireland Cancer Registry: Cancer incidence and mortality. http://www.qub.ac.uk/research-centres/nicr/Data/OnlineStatistics/Non-MelanomaSkinCancer/. Accessed 26 June 2008
Office for National Statistics: Mortality statistics: cause, series DH2 no. 29. Office for National Statistics, London
Quinn, M., Babb, P., Brock, A., et al.: Cancer trends in England and Wales, 1950–1999. The Stationery Office, London (2001)
http://info.cancerresearchuk.org/healthyliving/sunsmart/. Accessed 26 June 2008
http://www.york.ac.uk/inst/crd/crddatabases.htm. Accessed 26 June 2008
Housman, T.S., Feldman, S.R., Williford, P.M., et al.: Skin cancer is among the most costly of all cancers to treat for the Medicare population. J. Am. Acad. Dermatol. 48(3), 425–429 (2003)
Chen, J.G., Fleischer, A.B., Smith, E.D., et al.: Cost of nonmelanoma skin cancer treatment in the United States. Dermatol. Surg. 27, 1035–1038 (2001)
National Institute for Clinical Excellence: Guide to the methods of technology appraisal (reference N0515). National Institute for Clinical Excellence, London (2004)
Office for Population Censuses and Surveys: Morbidity statistics from general practice: fourth national study 1991–1992, series MB5 no. 3. HMSO, London (1995)
Cancer Research UKL: Cancer stats incidence—UK. Cancer Research, UK (2004)
Stefoski Mikeljevic, J., Johnston, C., Adamson, P.J., Wright, A., Bishop, J., Newton, A., Batman, P., Neal, R.D., Forman, D.: How complete has skin cancer registration been in the UK? A study from Yorkshire. Eur. J. Cancer Prev. 12(2), 125–133 (2004)
Netten, A., Curtis, L.: Unit costs of health and social care 2003. Personal social services research unit. University of Kent, Canterbury (2003)
Department of Health: Hospital episodes statistics, England: financial year 2002–2003. Department of Health, London (2003)
Department of Health: NHS reference costs 2002. Department of Health, London (2003)
Kernick, D.P., Reinhold, D.M., Netten, A.: What does it cost the patient to see the doctor? Br. J. Gen. Pract. 50, 401–403 (2000)
Office for National Statistics: Annual abstract of statistics No. 140. The Stationery Office, London (2004)
Liu, J.L., Maniadakis, N., Gray, A., Rayner, M.: The economic burden of coronary heart disease in the UK. Heart 88, 597–603 (2002)
Bosanquet, N., Sikora, K.: The economics of cancer care in the UK. Lancet. Oncol. 5, 568–574 (2004)
Carter, R., Marks, R., Hill, D.: Could a national skin cancer primary prevention campaign in Australia be worthwhile? An economic perspective. Health. Promot. Int. 14, 73–82 (1999)
Kyle, J.W., Hammitt, J.K., Lim, H.W., et al.: Economic evaluation of the US Environmental Protection Agency’s SunWise program: sun protection education for young children. Pediatrics 121(5), e1074–e1084 (2008)
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Morris, S., Cox, B. & Bosanquet, N. Cost of skin cancer in England. Eur J Health Econ 10, 267–273 (2009). https://doi.org/10.1007/s10198-008-0127-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10198-008-0127-0