Abstract
The effect of colchicine was evaluated in a large cohort of Behçet’s disease (BD) patients and compared to placebo. In a randomized, double-blind, controlled crossover trial, 169 patients without major organ involvement were selected consecutively. They fulfilled the International Criteria for Behçet’s Disease. Patients were randomly assigned to colchicine or placebo. At 4 months, they were swapped over (colchicine to placebo, placebo to colchicine) for another 4 months. The primary outcome was the overall disease activity index, the IBDDAM. The secondary outcome was the responses of the individual symptoms. A Student’s paired t test was used to evaluate results within each group, and an ANOVA to check for differences between colchicine and placebo. Analysis was performed using the “intention to treat” method. For placebo, IBDDAM worsened from 3.17 to 3.63 (t = 1.750, P = 0.08). For colchicine, IBDDAM improved from 3.35 to 2.75 (t = 4.143, P < 0.0001). Oral aphthosis, genital aphthosis, pseudofolliculitis, and erythema nodosum improved significantly with colchicine but not with placebo. According to the ANOVA, the difference in IBDDAM between colchicine and placebo was highly significant (F = 14.674, P = 0.00016). The difference between the results for males and females was not significant (F = 0.181, P = 0.67). In conclusion, colchicine, but not placebo, significantly improved the overall disease activity index. The difference between the results for colchicine and placebo was also statistically significant.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Colchicine was first used to treat Behçet’s disease (BD) in 1977, concomitantly by Mizushima et al. [1] and Haim and Friedman-Birnbaum [2]. Case reports soon confirmed the efficacy of colchicine treatment [3–8]. It was used to treat lesions caused by the disease, and resulted in some improvement. However, all of the case reports focused on a few patients, with the largest studying five cases [5]. On the other hand, a double-blind controlled study [9] of 35 patients indicated that colchicine treatment was ineffective, except for erythema nodosum and arthralgia. A later trial from the same team [10] showed the same inefficacy of colchicine, except for genital aphthosis and erythema nodosum in women, and for arthritis in both genders. However, an open trial of 54 patients with oral aphthosis indicated that colchicine treatment was effective overall [11]. Other authors, based on their experiences, have also confirmed the value of colchicine treatment in BD [12–14].
For Yurdakul and colleagues [10], the unresponsiveness of their patients could be explained by genetic differences between Silk Road BD and sporadic BD from other parts of the world. To test their hypothesis (the inefficacy of colchicine treatment for Silk Road BD), we designed a randomized, double-blind, controlled crossover study in Iran, which is in the middle of the Silk Road, and has the second highest prevalence of BD in the world [15]. The study was designed in the Rheumatology Research Center (RRC), Tehran University for Medical Sciences (TUMS). The protocol was approved by the Research Committee of RRC and TUMS and the Ethical Committee of TUMS. The protocol is registered on ClinicalTrials.gov under the ID: NCT00700297.
Materials and methods
Patients
Patients were selected on a consecutive basis. The entry criteria were: age between 14 and 60 years, confirmed diagnosis of Behçet’s disease, absence of major organ involvement (eye, brain, major intestinal, lung, and cardiovascular involvement), at least one active symptom, and no treatment for at least 1 month. The patients had the study design explained to them, and they then gave signed written consent. During the two phases of the study, patients that showed major organ involvement were moved out of the study. All patients fulfilled the new International Criteria for Behçet’s Disease.
Method
Patients were randomized at the start of the study to take either colchicine or placebo. The dose of colchicine was 1 mg (one milligram tablet), taken at night. The dose remained stable throughout the study, with no dose escalation. Patients were not permitted to take any other medication for the disease during the two phases of the study. At 4 months, the colchicine and placebo groups were swapped (those who were taking colchicine went on the placebo, and those on the placebo went on colchicine). Thus, each patient tried both colchicine and placebo during the study. The primary outcome was the effect of colchicine on the disease activity index, the IBDDAM [16, 17]. To calculate the overall baseline IBDDAM, the IBDDAM for the last 12 months (prior to the study) for each manifestation was calculated, and these were then added together. The overall disease activity index was then divided by the number of months (12) to give the mean activity index per month. The IBDDAM was then measured every 2 months (in the middle and at the end of each arm of the study). The total IBBDAM for the 4 months was then divided by four to get the mean activity index per month. The secondary outcome was to evaluate how the individual symptoms responded to colchicine (IBDDAM for each manifestation).
IBDDAM calculation
IBDDAM is calculated as follows. In each attack, 1 point is given for each 5 oral aphthous lesion, one genital aphthous lesion, 10 pseudofolliculitis, 5 erythema nodosum, arthralgia (any number of joints), cephalalgia, superficial phlebitis, and positive pathergy test. Two points are given for monoarthritis, deep vein thrombosis, and epididymitis. Three points are given for polyarthritis, mild CNS involvement (central or peripheral), and mild intestinal lesions. Six points are given for large vessel thrombosis (each vessel), severe CNS, and GI manifestations. Eyes are calculated separately by assigning 1–4 points for each inflammatory lesion of each segment (anterior uveitis, posterior uveitis, retinal vasculitis). The results for each section are multiplied by an aggravation coefficient: 1 for anterior uveitis, 2 for posterior uveitis, and 3 for retinal vasculitis. All eye results are then added together. If any of the abovementioned lesions last for more than 1 month, the points are awarded again.
Statistical analysis
Analysis was performed by the “intention to treat” method.
As the difference in IBDDAM before and after treatment exhibited a normal distribution, a Student’s t test for paired samples was used to evaluate the outcomes of the colchicine and placebo groups. As Levene’s test indicated homogeneity of variance, ANOVA and linear regression were used to test the effect of treatment (colchicine and placebo) and gender on patient outcome. The dependent variable was the change in IBDDAM (before and after the treatment). The independent variables were treatment and gender. SPSS 15 was used for all statistical calculations.
Results
Gender
Among the patients, 32.3% were male (confidence interval (CI) at 95% was 45.5–60.3%), and 47.3% were female (95% CI was 39.7–54.5%). The male-to-female ratio was 1.11:1.
Age
Mean age was 32.1 years, with a standard error of the mean (SEM) of 0.64 and a standard deviation (SD) of 8.29. Minimum age was 14 and maximum age was 63 years. Median was 32 years. Among the male patients, the mean age was 32.3 years (SEM 0.88, SD 8.22, minimum age 17, maximum age 63, median 30). Among the female patients, the mean age was 32.5 years (SEM 0.0.94, SD 8.42, minimum age 14, maximum age 56, median 32.5). There was no statistically significant difference between them.
ESR
Normal ESR was seen in 40.5% of the patients (95% CI was from 33.5 to 48.1%). ESR was 21–50 in 46% of patients (95% CI was 38.6–53.4%). ESR was 51–100 in 13.5% of patients (95% CI was 9.2–19.6%). The mean patient ESR was 30.1 mm in the first hour (SE 1.5, SD 18.6, minimum 10, maximum 100, median 25). There was not much difference between male and female ESRs: normal ESR was 45.3% in males vs. 35.1% in females (95% CI 35–55.3 vs. 25.5–46%). An ESR of 21–50 was seen in 47.7% vs. 44.1% (95% CI 37.2–57.5 vs. 33.4–54.7%). This difference in ESR between males and females was not statistically significant. An ESR of 51 to 100 was detected in 7 vs. 20.8% (95% CI 2.9–14.3% vs. 13.7–31.6%). This difference was statistically significant (p 0.01); a high ESR was seen more often in females than in males. The mean ESR in males was 27 mm in the first hour (SEM 1.8, SD 16.4), and in females it was 37 mm (SEM 2.3, SD 20.4). This difference was statistically significant (P < 0.001).
Pathergy test
Pathergy test was positive in 51.5% of the patients (95% CI 43.9–59%). In males, it was positive in 61.4% (95% CI 50.9–70.8%) and in females in 40.3% (95% CI 30–51.4%) of the cases. This difference was statistically significant (P < 0.01).
HLA-B51
This was searched for in 158 patients (84 males and 74 females). It was present in 41.7% of the patients (95% CI 34.2–49.5%). In male patients it was detected in 45.8% (95% CI 35.5–56.5%), and in female patients it was seen in 37% (95% CI 26.8–48.5%). This difference was not statistically significant.
Duration of disease
The mean duration at entry to the study was 6.4 years (SEM 0.43, SD 5.52). The median was 5 years, the minimum was 6 months and the maximum was 23 years. In male patients, the mean duration was 5.8 years (SEM 0.5, SD 5.1), and in female patients it was 7.2 years (SEM 0.7, SD 5.9). This difference was not statistically significant.
Patients and drop-outs
One hundred sixty-nine (169) patients were enrolled into the study. In the placebo arm, 112 finished the first 2 months of the study and 97 finished the full 4 months. In the colchicine arm, 113 patients finished the first 2 months of the study and 105 patients the full 4 months. The drop-out rate was the same for the first 2 months of the study in both arms. It was slightly higher for the placebo group in the second period of 2 months in the study (64 for colchicine versus 72 in the placebo arm; difference was not statistically significant). After adjusting them by the intention to treat method, the data for 136 patients on colchicine and 146 patients for placebo were made available for statistical analysis.
Major organ involvement
Eight patients were removed from the study: six for ocular lesion and two for intractable lesion attacks (one arthritis and one erythema nodosum). Two were on colchicine when the attack occurred and six were on placebo. Six of the cases were in their first 4 months of the trial (five were taking placebo, one was taking colchicine), while two patients were in their crossover period (one on colchicine and one on placebo).
Side effects
Eighteen patients (10.6%) experienced side effects: nine on colchicine and nine on placebo. Only one of them had to stop their medication (colchicine), due to nausea and vomiting. The patient was taking only 1 mg per day. Four patients on colchicine experienced diarrhea, which did not necessitate discontinuation of medication. In one case, antibiotics stopped the diarrhea. In the three other cases the diarrhea stopped spontaneously. Two cases on colchicine experienced mild elevation of liver enzymes (SGOT-SGPT). One case was at the end of the study period and had normally to stop the medication according to the protocol. In the other, the liver enzymes dropped back down to normal without discontinuing the colchicine. One patient on colchicine complained of a urinary tract infection, which disappeared with antibiotics. Three patients on the placebo had diarrhea, which disappeared spontaneously. One case of abdominal pain, one case of purpura, one case of dysesthesia in the legs, one case of parotiditis, one case of hematuria, and one case of zona was seen while the patients were taking placebo.
Overall results (primary outcome) obtained by intention to treat analysis
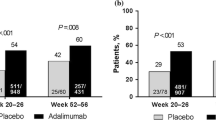
The difference at baseline in the mean overall IBDDAM between colchicine and placebo was not statistically significant (P = 0.28). The mean IBBDAM at baseline was 3.55 in the colchicine group. It improved to 2.75 after treatment. The Student’s paired t test was 4.143 with a P value of <0.001 (Table 1). For the placebo group, the mean IBDDAM increased (worsened) from 3.17 to 3.63. The t (paired samples) was 1.750 with a p value of 0.08 (Table 1).
One-way ANOVA demonstrated a highly significant difference between colchicine and placebo (F 14.674, P < 0.001) (Table 2). The difference between genders was not significant (F 0.181, P = 0.67) (Table 3).
In the colchicine group, 49% of the patients improved, 22% did not change, and 29% worsened. In the placebo group, 29% improved, 24% did not change, while 47% worsened.
Overall results (primary outcome) for patients who completed the treatment
In the colchicine group, the mean IBBDAM improved from 3.28 to 2.25. The t test (paired samples) was 4.348 with a p value of <0.001 (Table 4). For the placebo group, the mean IBDDAM increased (worsened) from 3.13 to 3.38, with t = −0.742 and P = 0.46 (Table 4).
ANOVA demonstrated a very significant difference between colchicine and placebo (F 9.994, P = 0.002) (Table 5). The difference between genders was not significant (F 0.010, P = 0.92) (Table 6).
Subgroup results
Oral aphthosis (OA)
Intention to treat analysis (Tables 1–3)
For OA, the difference in IBDDAM at baseline between colchicine and placebo was not statistically significant (t = 0.748, P = 0.46). For the colchicine group, the mean IBBDAM at baseline was 2.29. It improved to 1.83 after treatment. The difference was statistically significant, with a t (paired samples) of 2.926 corresponding to a p value of 0.004. For the placebo group, the mean IBDDAM aggravated (increased) from 2.11 to 2.38. The difference was not statistically significant, with t = 1.470 corresponding to a P value of 0.14.
ANOVA demonstrated a significant difference between colchicine and placebo (F 8.887, P = 0.003). However, the difference between men and women was not significant (F 0.048, P = 0.83).
Patients who completed treatment (Tables 4–6)
In the colchicine group, the mean IBBDAM improved from 2.20 to 1.64. The t for paired samples was 2.880 with a p value of 0.005. For the placebo group, the mean IBDDAM increased (aggravated) from 2.13 to 2.24 with t = −0.484 and P = 0.63.
ANOVA demonstrated a very significant difference between colchicine and placebo (F 4.891, P = 0.028). The difference between genders was not significant (F 0.025, P = 0.88).
Genital aphthosis (GA)
Intention to treat analysis (Tables 1–3)
The difference at baseline for GA IBDDAM between colchicine and the placebo group was not statistically significant (t = 0.692, P = 0.49). The mean IBBDAM at baseline was 0.46 for the colchicine group. It improved to 0.3 after treatment. The t test (paired samples) was 2.091 (P = 0.038). For the placebo group, the mean IBDDAM increased (worsened) from 0.38 to 0.46. The t test (paired samples) was −0.908 (P = 0.37).
ANOVA demonstrated a significant difference between colchicine and placebo (F 4.299, P = 0.039). The difference between genders was not significant (F 1.939, P = 0.16).
Patients who completed treatment (Tables 4–6)
In the colchicine group, the mean IBBDAM improved from 0.40 to 0.19. The t test (paired samples) was 2.240 (P = 0.027). For the placebo group, the mean IBDDAM increased (aggravated) from 0.40 to 0.47 with t = −0.608, and P = 0.54.
ANOVA did not demonstrate any significant difference between colchicine and placebo (F 3.648, P = 0.058), nor between males and females (F 0.948, P = 0.33).
Skin lesions
Intention to treat analysis (Tables 1–3)
For skin lesions at baseline, the difference in IBDDAM between colchicine and placebo was not statistically significant (t = −0.19, P = 0.98). With colchicine, the mean IBBDAM improved from 0.46 to 0.35 (t = 2.495, P = 0.014). For the placebo group, it worsened (increased) from 0.46 to 0.48 (t = −0.266, P = 0.79).
The ANOVA did not demonstrate any significant difference between colchicine and placebo (F = 1.907, P = 0.17). The difference between genders was not also significant (F = 0.181, P = 0.67).
Patients who completed treatment (Tables 4–6)
The mean IBBDAM improved from 0.41 to 0.25 (t = 2.779, P = 0.006) in the colchicine group. For the placebo group, the mean IBDDAM improved from 0.41 to 0.39 (t = 0.139, P = 0.89).
ANOVA failed to demonstrate any significant difference between colchicine and placebo (F 1.280, P = 0.26). The same was true for gender (F = 1.686, P = 0.20).
Joint manifestations
Intention to treat analysis (Tables 1–3)
The IBDDAM difference at baseline for joint manifestations between the colchicine and the placebo groups was not statistically significant (t = 1.09, P = 0.28). In the colchicine group, the mean IBBDAM improved from 0.26 to 0.19 (t = 1.673, P = 0.1). For the placebo group, the mean IBDDAM increased (aggravated) from 0.19 to 0.25 (t = −1.528, P = 0.13).
ANOVA demonstrated a significant difference between colchicine and placebo (F = 5.080, P = 0.025). The difference between genders was not significant (F = 0.298, P = 0.59).
Patients who completed treatment (Tables 4–6)
The mean IBBDAM improved from 0.20 to 0.12 (t = 1.471, P = 0.14) in the colchicine group. For the placebo group, the mean IBDDAM increased (worsened) from 0.16 to 0.21 (t = −1.244, P = 0.22).
ANOVA did not show any significant difference between colchicine and placebo (F 3.670, P = 0.057), or between genders (F = 0.020, P = 0.89).
Discussion
For the patients who dropped out, there reasons for doing so are not known, except in the cases of the eight patients that we removed from the study because of major organ involvement (six cases) or intractable lesions (one case of erythema nodosum and one case of arthritis). The remaining patients did not come back for their periodic follow-ups. One of the reasons for this could be inefficacy of the treatment. As the patients knew that they could be on placebo instead of colchicine, they could have bought colchicine over the counter instead. Another reason could be efficacy of the treatment, or a periodic remission in their symptoms. They did not come for their follow-ups and resorted to over-the-counter colchicine. The compliance of BD patients with the RRC is usually very good for severe cases, because they are all basically referral patients, and so they are sent back if they consult another physician. However, compliance deteriorates in mild cases, mainly because they know that their lesions are not important and proceed with attacks and remissions.
IBDDAM was selected as the disease activity index for this study [16, 17]. The Behçet’s disease current activity form (BDCAF) is another disease activity index for Behçet’s disease [18]. BDCAF is, however, unsuitable for comparisons between countries [19]. BDCAF performed less well with Iranian patients than IBDDAM [20]. This was the reason for our selection of IBDDAM as the disease activity index for this study.
According to intention to treat analysis, the results for IBDDAM (the overall disease activity index) demonstrate that BD responds favorably to colchicine. During the placebo period, the patients slightly aggravated their IBDDAM (not to a statistically significant degree though). When the patients were on colchicine, their IBDDAMs significantly improved. The comparison of colchicine with placebo, using ANOVA, showed a highly significant difference. This study failed to demonstrate any significant difference between men and women. Upon analyzing the patients who completed their treatment courses, the results remained the same.
Although our study was not designed to test individual symptoms and their outcomes under colchicine treatment, the results nevertheless show that the mean disease activity index of oral aphthosis improved significantly from the baseline, while that of the patients on placebo worsened. Comparison by ANOVA of the mean changes for the colchicine and placebo groups also showed a statistically significant difference. The same was true of other symptoms, except for skin manifestations. However, the mean improvement in skin manifestations was statistically significant for colchicine, but not for placebo.
The daily experiences and the general feelings of experts are that colchicine is of some use in BD, mainly for mucocutaneous lesions [1–8, 12–14]. While it is rare to observe complete remission with colchicine, lesions usually become less awkward, exhibiting shorter healing times and longer remission periods. In a recent (2002) open study of a cohort of 54 patients by Fontes et al. [11], after 3 months of treatment, remission from oral aphthosis was observed in 22%, a significant improvement (at least 50% improvement) was seen in 41%, and failure was noted for 37%. In the present study, the rate of failure for oral aphthosis was the same as for the group of patients who completed treatment, and slightly less than that observed in the intention to treat analysis.
Yurdakul and colleagues in 2001 [10], studied 116 patients in a double-blind, randomized, controlled study of colchicine versus placebo, and demonstrated the inefficacy of colchicine. Colchicine was only efficient for genital aphthosis, erythema nodosum, and arthritis in women, as well as for arthritis in men. There are many differences in the ways in which the Yurdakul study and our study were conducted. First, in their study, they only considered lesions present at the time of control (once monthly), not attacks that were resolved between the two visits. In our study, in contrast, all attacks (whether present or absent at the time of visit) were taken in account. Second, in their study, only young patients (18–35) were selected. In our study, all patients above 14 years old were accepted in the study. The inclusion criteria of Yurdakul et al. would have considered only two-thirds of our patients. Third, in their study, they included patients with up to 2 years of disease duration, discarding all others. In our study, we looked at all kinds of patients, from those with new disease onset to those experiencing a very long and chronic disease (from 6 months to 23 years, with a mean of 6.4 years; median 5 years). If we had applied the two limitations that Yurdakul and colleagues used in their study, we would have eliminated 92.6% of our patients, making our’s a study of a minority of BD patients (7.4%) who would not be representative of the BD population. Fourth, in their study, patients were permitted to use local treatment for their oral and genital ulcerations, while they were not permitted to do so in our study. The use of local steroids can influence the speed at which mucosal lesions heal, making them disappear before patients attend their monthly visit. Fifth, the disease activity indices (DAIs) used in the two studies are different. Of the two DAIs used, IBDDAM is the only validated DAI [17, 20]. Sixth, they studied two different groups of patients (placebo and controls), although the demographic data of both groups were very similar. Our study was done as crossover study, making each patient their own control. Finally, the number of patients in each of their study arms (four arms: male colchicine, male placebo, female colchicine, female placebo) was low, leading to a type 2 error in their calculations, as recognized by the authors themselves.
Conclusion
Colchicine is an effective treatment for mucocutaneous and joint manifestations in cases with Behçet’s disease. It is yet to be demonstrated whether colchicine can improve or prevent major organ involvement, and so this warrants further studies.
References
Mizushima Y, Matsumura N, Shimizu T, Fukushima B, Mimura Y, Saito K, et al. Colchicine in Behçet’s disease. Lancet. 1977;2:1037.
Haim S, Friedman-Birnbaum R. Colchicine in Behçet’s disease. Harefuah. 1977;93:399–400.
Hazen PG, Michel B. Management of necrotizing vasculitis with colchicine. Improvement in patients with cutaneous lesions and Behçet’s syndrome. Arch Dermatol. 1979;115:1303–6.
Raynor A, Askari AD. Behçet’s disease and treatment with colchicine. J Am Acad Dermatol. 1980;2:396–400.
Miyachi Y, Tanigushi S, Ozaki M, Horio T. Colchicine in the treatment of the cutaneous manifestations of Behçet’s disease. Br J Dermatol. 1981;104:67–9.
Moreno Moraga J, Estrada Saiz RV, Chantres Antoraz MT, Rivas Flores J, Gilsanz Garcia V. Therapeutic values of colchicine in Behçet’s disease. Med Clin (Barc). 1981;77:18–20.
Harper RM, Allen BS. Use of colchicine in the treatment of Behçet’s disease. Int J Dermatol. 1982;21:551–4.
Sander HM, Randle HW. Use of colchicine in Behçet’s syndrome. Cutis. 1986;37:344–8.
Aktulga E, Altac M, Muftuoglu Y, Pazarli H, Tuzun Y, Yalcin B, et al. A double blind study of colchicine in Behçet’s disease. Haematologica. 1980;65:399–402.
Yurdakul S, Mat C, Tuzun Y, Ozyazgan Y, Hamuryudan V, Omer Uysal, et al. A double-blind trial of colchicine in Behçet’s syndrome. Arthritis Rheum. 2001;44:2686–92.
Fontes V, Machet L, Huttenberger B, Lorette G, Vaillant L. Recurrent aphthous stomatitis: treatment with colchicine. An open trial of 54 cases. Ann Dermatol Venereol. 2002;129:1365–9.
Vidaller Palacin A, Robert Olalla J, Sanuy Jimenez B, Rufi Rigau G, Folch Civit J, Charte Gonzales A. Behçet’s disease therapy review. Ann Med Int. 2002;19:594–8.
Wechsler B. Colchicine and Behçet’s disease: an efficacious treatment finally recognized. Rev Med Int. 2002;23:355–6.
Lange U, Schumann C, Schmidt KL. Current aspects of colchicine therapy—classical indications and new therapeutic uses. Eur J Med Res. 2001;20:150–60.
Davatchi F, Jamshidi AR, Tehrani-Banihashemi A, Gholami J, Forouzanfar MH, Moradi M, et al. Prevalence of Behçet’s disease in Iran: a WHO-ILAR COPCORD Stage 1 study. APLAR J Rheumatol. 2007;10:239–43.
Davatchi F, Akbarian M, Shahram F, Tebbi ME, Chams C, Shams H. Iran Behçet’s disease dynamic activity measure. Abstracts of the XIIth European Congress of Rheumatology. Hungarian Rheumatol 1991;32(Suppl):FP10–100.
Jamshidi A, Shahram F, Akbarian M, Gharibdoost F, Nadji A, Chams C, et al. The accuracy of IBDDAM (Iran Behçet’s disease dynamic activity measure) in the treatment evaluation of Behçet’s disease. APLAR J Rheumatol. 2001;4:161–3.
Bhakta BB, Brennan P, James TE, Chamberlain MA, Noble BA, Silman AJ. Behçet’s disease evaluation of a new instrument to measure clinical activity. Rheumatology. 1999;38:728–33.
Lawton G, Bhakta BB, Chamberlain MA, Tennant A. The Behçet’s disease activity index. Rheumatology 2004;43:73–8.
Shahram F, Khabbazi A, Nadji A, Ziaie N, Tehrani Banihashemi A, Davatchi F. Comparison of the existing disease activity indices in the follow up of patients with Behçet’s disease. Mod Rheumatol 2009;19 (in press).
Acknowledgment
The study was approved by the Research Committee of the Rheumatology Research Center and the Research Committee of Tehran University for Medical Sciences under the number RRC23. The project was approved by the Tehran University for Medical Sciences Ethical Committee. It was entirely sponsored by the Rheumatology Research Center. The project was registered at ClinicalTrials.gov under the ID: NCT00700297.
Author information
Authors and Affiliations
Corresponding author
About this article
Cite this article
Davatchi, F., Sadeghi Abdollahi, B., Tehrani Banihashemi, A. et al. Colchicine versus placebo in Behçet’s disease: randomized, double-blind, controlled crossover trial. Mod Rheumatol 19, 542–549 (2009). https://doi.org/10.1007/s10165-009-0200-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10165-009-0200-2