Abstract
Vascular disease has been proposed as a contributing factor for presbyacusis (age-related hearing loss). While this hypothesis is supported by pathological evidence of vascular decline in post-mortem human and animal studies, evidence in human subjects has been mixed with associations typically reported between a measure of vascular health and low frequency hearing in older women. Given the difficulty of characterizing the in vivo health of the cochlear artery in humans, an estimate of cerebral small vessel disease was used to test the prediction that age-related change in low frequency hearing and not high frequency hearing is related to a global decline in vascular health. We examined the extent to which these associations were specific to women and influenced by a history of high blood pressure in 72 older adults (mean age 67.12 years, SD = 8.79). Probability estimates of periventricular white matter hyperintensities (WMH) from T1- and fluid attenuated T2-weighted magnetic resonance images were significantly associated with a low frequency hearing metric across the sample, which were independent of age, but driven by women and people with a history of high blood pressure. These results support the premise that vascular declines are one mechanism underlying age-related changes in low frequency hearing.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Vascular disease has been proposed as a contributor to age-related hearing loss or presbyacusis for many years (Alexander 1902; Rosen and Olin 1965). This hypothesis is supported, in part, by observations of stria vascularis atrophy in human tissue (Schuknecht 1974; Nelson and Hinojosa 2003; Suzuki et al. 2006). In addition, older gerbils raised without exposure to noise or ototoxic drugs exhibit stria vascularis atrophy with pronounced capillary loss and a reduction in the endocochlear potential, which provides the voltage to the outer hair cells (cochlear amplifier) (Johnsson and Hawkins 1972; Pauler et al. 1988; Schulte and Schmiedt 1992; Gratton et al. 1996, 1997; Thomopoulos et al. 1997). Consistent with evidence for vessel disease affecting the stria vascularis, as well as the spiral ganglion (Makishima 1978), there is cross-sectional evidence that cardiovascular risk factors and vascular events are correlated with age-related hearing loss (Susmano and Rosenbush 1988; Perez Villa et al. 1995; Brant et al. 1996; Friedland et al. 2009).
There have been non-significant cardiovascular and hearing results (Drettner et al. 1975; Pratt et al. 2009), however, as well as evidence for inflammatory disease rather than vascular disease underlying presbyacusis (Bainbridge et al. 2010; Verschuur et al. 2012). Inconsistent vascular findings may be due to evidence that associations between metrics of vascular health and hearing appear to be most consistent for low frequency hearing thresholds (Gates et al. 1993; Pirodda et al. 1999; Rosenhall and Sundh 2006; Helzner et al. 2011). These low frequency findings are supported by evidence for pronounced capillary atrophy at the apex of the cochlea compared to the base (Mom et al. 2005). In addition, vascular health associations with low frequency hearing appear to be most consistent when analyses are performed separately for males and females (Gates et al. 1993; Rosenhall and Sundh 2006). For example, Gates et al. (1993) examined the impact of cardiovascular risk factors on the likelihood of low frequency hearing loss in 996 women and 676 men. A history of coronary heart disease nearly doubled the odds of low frequency hearing loss in women. Moreover, gender-specific effects are consistent with evidence that hearing loss is more likely in women when there is a history of myocardial infarction (Torre et al. 2005) and evidence of retinopathy (Liew et al. 2007). These findings suggest that women, who on average are more likely to experience low frequency hearing loss than men (Lee et al. 2005), are at risk for low frequency hearing loss when vascular disease affects the small vessels that support the stria vascularis.
The cochlear artery receives its blood supply from the vertebral artery and has small distal vessels that support the stria vascularis. As part of the cerebral vessel system, the cochlear artery may experience vessel disease seen throughout the central nervous system. In support of this premise, sclerosis of the internal auditory artery and circle of Willis was observed in a post-mortem examination of tissue from people who had age-related hearing loss and high blood pressure (Makishima 1978). In addition, a retrospective study of audiograms in patients with histories of vascular events demonstrated that people with flat and low sloping audiograms were significantly more likely to have had a cerebrovascular event than people with other audiometric profiles (Friedland et al. 2009).
White matter hyperintensities (WMH) in fluid attenuated T2-weighted images and reduced white matter contrast in T1-weighted images in periventricular regions are markers of cerebral small vessel disease (Eckert et al. 2010). A large body of literature shows that these hyperintensities, which typically occur in periventricular white matter, increase with age and occur with cardiovascular risk factors such as high and variable blood pressure (Brickman et al. 2010; Soderlund et al. 2003), pulse pressure (Waldstein et al. 2012), ultrasound measures of common carotid artery diameter and middle cerebral artery pulsatility (Heliopoulos et al. 2012), and anti-hypertensive medication history (Kuo et al. 2010). Although there are multiple reasons for WMH (Gouw et al. 2011), periventricular WMH in post-mortem tissue from otherwise neurologically normal older adults have been associated with reduced small vessel density, reduced myelin, and increased vacuolation (Murray et al. 2012). Therefore, neuroimaging measures of periventricular white matter damage can reflect changes in vascular health. The overarching goal of this study was to test the prediction that older adults, and women in particular, with age-related changes in low frequency hearing are more likely to have WMH with the appearance and distribution that is typical of small vessel disease.
Methods
Participants
A total of 72 adults with a mean age of 67.12 years (range = 51.04–88.35 years; 39 female) participated in this study and were part of a longitudinal project on presbyacusis and/or a speech training project at the Medical University of South Carolina. 29 cases, or 40 % of the sample, reported a history of high blood pressure. Evidence of high blood pressure medication dosage, treatment compliance, and quality of high blood pressure control was not available, but some subjects reported taking medications for hypertension (n = 32), high cholesterol/hyperlipidemia (n = 28), stroke prevention (i.e., aspirin, n = 15), and diabetes (n = 6). Only the use of hypertension medication was related to a self-report history of high blood pressure (χ (1,72) 2 = 56.35, p = 6.07 E − 14; 100 % with reported high blood pressure and 9 % of people not reporting high blood pressure reported taking medication for hypertension. One case reported high blood pressure but could not recall their medications. There was no difference between males and females in the frequency of reported high blood pressure (χ (1,72) 2 = 0.39, ns) or use of anti-hypertension medications (χ (1,71) 2 = 0.41, ns). The impact of hormone replacement therapy on hearing thresholds could not be examined given that only two women reported receiving hormone replacement therapy. Exclusionary criteria for participants recruited for this neuroimaging study included a history of head trauma, seizures, self-reported central nervous system disorders, conductive hearing loss or otologic disease, and contraindications for safe MRI scanning. Participants provided written informed consent before participating in this Medical University of South Carolina Institutional Review Board approved study.
Audiometric evaluation
Pure-tone thresholds at conventional frequencies (250, 500 1,000, 2,000, 3,000, 4,000, 6,000, and 8,000 Hz) were obtained with a Madsen OB922 clinical audiometer calibrated to appropriate ANSI standards (ANSI 2004) and equipped with TDH-39 headphones. Bone conduction testing (500, 1,000, 2,000, 3,000, 4,000 Hz) was performed for all subjects to exclude the possibility that elevated thresholds were due to conductive hearing loss. Cerumen management was performed prior to audiometric evaluation for participants whose otoscopic evaluation demonstrated excessive cerumen. Low frequency and high frequency hearing metrics were obtained by standardizing the hearing thresholds relative to the factor analysis weights from a large sample of older adult audiograms that are reported by Eckert et al. (2012). Specifically, factor analysis weights derived from the thresholds of 1,704 ears (mean age = 69.92 years [SD = 7.24] that was 56 % female), which are presented in Table 1 of Eckert et al. (2012), were applied to the thresholds in the current study by: (1) standardizing each pure tone threshold to the respective mean and SD of 1,704 ears; (2) multiplying the standardized pure tone score by the respective pure tone frequency component coefficient; and (3) summing the values from step 2 for each component across pure tone variables. These statistically independent low and high frequency hearing metrics (r (70) = −0.10, ns) provided hearing estimates that are normalized relative to hearing thresholds in the population and were used in analyses with the brain imaging metrics described below.
MRI data acquisition and image pre-processing
A Siemens 3 T Tim Trio and 32 channel head coil were used to collect structural images that are sensitive to periventricular white matter damage. T1-weighted images that demonstrate white matter damage as hypointense contrast were collected with the following parameters: 160 slices; 256 × 256 matrix, TR = 2250 ms, TE = 4.15 ms, flip angle = 9 °, TI = 900 ms; slice thickness = 1 mm, no slice gap, and an in plane resolution = 1.0 × 1.0 mm. Fluid attenuated T2-weighted images (i.e., FLAIR images), which demonstrate white matter damage as hyperintense contrast were acquired with the following parameters: 40 slices; 384 × 384 matrix, TR = 9,000 ms, TI = 2,500 ms, TE = 94 ms, flip angle = 180 °, slice thickness = 3 mm, slice gap=3 mm, and an in plane resolution = 0.5 × 0.5 mm.
White matter hyperintensity estimation
Each participant’s FLAIR image was co-registered to their T1-weighted image using a rigid body mutual information algorithm using SPM8. Figure 1A shows an example of co-registered FLAIR and T1-weighted images and shows that WMH in the FLAIR image occurs in regions where there is reduced white matter contrast in the T1-weighted image. These hypointense regions exhibit elevated gray matter probabilities when the T1-weighted images are segmented, using SPM8 unified segmentation in this study, into gray matter, white matter, and CSF images (Fig. 1A). This spatially complementary information was used to estimate the probability of white matter damage with the Lesion Segmentation Toolbox (LST; Schmidt et al. 2012) and the VBM8 toolbox (http://dbm.neuro.uni-jena.de/vbm). The LST initially defines the location of WMH based on outlier values across the FLAIR and segmented T1-weighted images (Fig. 1A). The LST then uses a lesion growing algorithm with Markov Random Fields modeling to define the extent of the lesion. The default LST settings were used with the exception of kappa, a value that reflects the likelihood that a voxel value reflects typical gray matter or white matter relative to the likelihood of white matter damage in the FLAIR image where smaller values are more sensitive to white matter damage. Visual inspection of the probability maps across subjects using different kappa (K) lesion growing values, indicated that a K = 0.18 was the optimal value for our Siemens images collected with a 32 channel head coil to maximize sensitivity while limiting false positive results (Fig. 1A). The analyses described below were repeated with a K = 0.25 based on the Schmidt et al. (2012) findings for K, but this K value did not substantively change the results (not shown). This automated method for quantifying white matter damage has been shown to have a high degree of agreement with manual delineation of WMH in FLAIR images with different image dimensions (Schmidt et al. 2012).
Defining white matter hyperintensity (WMH) regions indicative of cerebral small vessel disease in periventricular white matter space. A Co-registered FLAIR and T1-weighted images from an 82-year-old female with a history of high blood pressure (HBP) are presented. The hyperintensity in the FLAIR image, which appears as a white matter hypointensity in the T1-weighted image, is segmented as gray matter (GM) and CSF in comparison to white matter (WM) in the T1-weighted segmented images (orange arrows). The LST conservatively identified WMH across the white matter of this participant (pink transparent WMH overlay). B Non-parametric one sample t-tests using the WMH probability images demonstrated significant p < 0.05 (red) to p < 0.0001 (yellow) corrected results across the sample. Note that regions in the anterior thalamic radiation, adjacent to the anterior horn of the lateral ventricle, appeared to be more affected across participants compared to regions adjacent to the occipital horn of the lateral ventricle.
The lesion segmentation toolbox generated lesion probability images that were normalized into a study specific space by applying normalization parameters that were estimated for the co-registered T1-weighted images. The T1-weighted segmented gray and white matter images were normalized, preserving concentration of signal intensity, into a study-specific coordinate space using diffeomorphic image registration (DARTEL) in SPM8 (Ashburner and Friston 2005) to preserve cortical topology using a membrane bending energy or Laplacian model (Ashburner 2007). Diffeomorphic normalization, which we have used previously to effectively normalize images from a wide age range of adults (Eckert et al. 2010), was applied to the co-registered FLAIR images from this older adult sample.
Statistics
Evidence of cerebral small vessel disease
Voxel-based statistical analyses were performed within regions where there was evidence of consistent cerebral small vessel disease across participants. This allowed for verification that effects occurred in regions with vessel disease and to limit the number of comparisons to regions where there was sufficient variance in the probability of WMH in comparison to regions where only one subject (outliers) might contribute to an effect. To define this space, one-sample permutation testing was performed with the FSL randomise algorithm using 10,000 permutations to identify brain regions exhibiting consistent patterns of WMH (p < 0.05, corrected) using the unsmoothed WMH images. This non-parametric test was used because the WMH probability data exhibited a bimodal distribution across cases. Threshold free cluster enhancement also was used in this analysis to ensure sensitivity to both diffuse and focal effects (Salimi-Khorshidi et al. 2011; Smith and Nichols 2009).
Associations with hearing thresholds
Voxel-based regression analyses were performed to test the predictions that variation in low frequency hearing, but not high frequency hearing, was related to cerebral small vessel disease. These analyses were performed using the WMH probability images and again were limited to the space of significant small vessel disease across the sample with a corrected significance value of p < 0.05. The FSL randomise regression analyses with 10,000 permutations included the low and high frequency hearing metrics, as well as estimates of whole brain gray matter volume, which were obtained from the segmented T1-weighted images to control for brain size effects that vary with gender and age. Total gray matter volume was used as a covariate because of its strong association with age (r = −0.54, p = 5.72 E − 9), gender (r = −0.40, p = 0.00003), and an estimate of WMH load (Rostrup et al. 2012) or total WMH (r = −0.30, p = 0.01). Thus, using total gray matter volume as a covariate provided the opportunity to characterize associations with hearing that were independent of potentially confounding or indirect factors.
We examined the extent to which hearing acuity was associated with vessel disease in groups with and without a reported history of high blood pressure because of evidence for cerebrovascular events relating to an audiometric configuration in cardiac patients (Friedland et al. 2009). We reasoned that individual variation in the severity of vessel disease could produce individual differences in WMH and hearing. We also examined the extent to which brain structure and hearing loss associations could be explained by gender because of evidence that vascular findings and low frequency hearing loss are more often observed in women (Gates et al. 1993; Torre et al. 2005; Rosenhall and Sundh 2006; Liew et al. 2007).
Results
Global white matter effects
Significantly elevated WMH probabilities were observed throughout periventricular white matter regions that are commonly observed to exhibit WMH in normal older adults (p < 0.05, corrected; Fig. 1B; e.g., Soderlund et al. 2003). The average WMH probability from voxels exhibiting significant WMH across the group (Rostrup et al. 2012) was associated with low frequency and high frequency hearing threshold estimates (low frequency: r (70) = 0.24, p = 0.04; high frequency: r (70) = 0.21, p = 08). However, these associations appear to be dependent on global changes in white matter health that occur across the age range of this sample because the hearing associations were not significant after controlling for age (low frequency: partial r (69) = 0.19, ns; high frequency: partial r (69) = −0.20, ns). Thus, there were general effects of age on WMH load and the hearing metrics.
Locally specific white matter and hearing effects
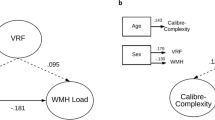
The non-parametric voxel-based regression analyses demonstrated that low frequency hearing was significantly associated with increased WMH probability in voxels corresponding to the anterior thalamic radiation that are adjacent to the anterior horn of the right lateral ventricle (Fig. 2A), even after accounting for variance due to high frequency hearing loss and global changes in gray matter volume (p < 0.05, corrected). These effects were present for the low frequency thresholds (250, 500 Hz) and were consistent across ears (Fig. 2B,C). The average WMH probability from voxels in the significant anterior thalamic radiation region (Fig. 2A) was used to demonstrate that the low frequency hearing association with WMH was not dependent on age (partial r (69) = 0.46, p = 0.0005). This association also could not be explained by an interaction between low and high frequency hearing metrics (r (70) = 0.05, ns). No significant associations with WMH were observed across the sample for high frequency hearing.
People with low frequency hearing loss, but not high frequency hearing loss, were more likely to have periventricular WMH. A WMH probabilities for voxels in the anterior thalamic radiation (ATR) at the anterior horn of the right lateral ventricle were positively associated with a standardized estimate of low frequency hearing for which elevated values reflects worse hearing (p < 0.05, corrected). B The bar graph shows the strength of the ATR white matter hyperintensity probability value (average probability from red voxels in A) with each left (blue) and right ear (red) pure tone threshold, after controlling for age, to demonstrate the specificity of the effect to low frequency thresholds. C Scatterplots of the 250 Hz result in B. demonstrate the distribution of thresholds for each ear and their linear relation with ATR WMH probability. D The low frequency hearing result was largely driven by females (circles) and people with a history of high blood pressure (orange). The x-axis is the average probability of WMH from across the significant effects shown in A. People with elevated WMH probabilities were more likely to have relatively elevated low frequency thresholds than people with low probability of WMH who were more likely to have better than average low frequency hearing thresholds. Note that the female-specific effect is due in part to a restricted range of low frequency hearing in males (squares). E WMH and hearing associations were specific to low frequency hearing as demonstrated by the non-significant association between high frequency hearing and the average WMH probability across the result in A. HBP high blood pressure.
Gender and high blood pressure effects
The average WMH probability estimate from the right anterior thalamic radiation above (Fig. 2A) also was used to further interrogate the low frequency hearing findings and test the predictions that vascular effects on low frequency hearing are most prominent in women and people with a history of high blood pressure. The association between WMH probability and low frequency hearing was specific to women (Fig. 2D; female: r (37) = 0.53, p = 0. 0005; male: r (31) = 0.17, ns) and people reporting a history of high blood pressure (Fig. 2D; high blood pressure: r (27) = 0.62, p = 0. 0004; no history of high blood pressure: r (41) = 0.13, ns). Because a history of high blood pressure was related to taking hypertension medications, we also examined the relation between low frequency hearing and the right anterior WMH probability estimate within people who reported taking hypertension medication (r (30) = 0.59, p = 0. 0003) and reported not taking hypertension medication (r (37) = 0.12, p < ns). In summary, women with a history of high blood pressure were more likely to demonstrate low frequency hearing loss compared to other participants (Fig. 2D).
Discussion
The results demonstrate a significant association between low frequency hearing and a putative measure of small vessel disease that highlight important factors affecting the likelihood of observing associations between hearing and vascular disease. First, the effects were specific to low frequency hearing. Second, evidence for more prominent effects in female participants could be due to the greater likelihood of low frequency hearing loss in females compared to males (Pearson et al. 1995; Lee et al. 2005) and exaggerated by unique vascular effects (Gates et al. 1993). Third, the effects were present only within people reporting a history of high blood pressure and who were taking medication for hypertension. Thus, women with high blood pressure may be at particular risk for low frequency hearing loss.
The low and high frequency hearing estimates used in this study were derived from a factor analysis of pure tone hearing thresholds in a very large sample of audiograms from older adults that identified two hearing components (Eckert et al. 2012), which also were observed in a previous factor analysis of audiograms from older adults (Jerger and Chmiel 1997). While the low frequency estimate is not by itself a marker of metabolic presbyacusis, people with metabolic presbyacusis are more likely to have elevated low frequency thresholds than people whose hearing loss is due to sensory cell loss secondary to noise or ototoxic drug exposure (Schmiedt 2010). The degree to which our results reflect an underlying vascular contribution to metabolic presbyacusis is unclear, however. A decline in the cochlear amplifier would produce the range of low frequency hearing loss observed in our participants, with just one case exhibiting low frequency thresholds that exceeded 40 dB (Fig. 2C; Schmiedt 2010). However, low frequency and cardiovascular findings have been reported for people with >40 dB of low frequency hearing loss (Gates et al. 1993; Friedland et al. 2009) that would not be indicative of metabolic presbyacusis (Schmiedt 2010). Vascular disease likely affects not just the stria vascularis, but also injures the spiral ganglion (Makishima 1978) and perhaps hair cells, which collectively could produce hearing loss >40 dB HL. Thus, vascular effects on hearing could appear as metabolic, sensory, and/or neural presbyacusis.
On average, women exhibit greater low frequency hearing loss than men, who are more likely to exhibit high frequency hearing loss (Pearson et al. 1995; Lee et al. 2005). This well-known gender difference in hearing profile probably stems from differences in occupation and lifestyle and appears to have a significant impact on the likelihood of observing associations between hearing loss and metrics of vascular disease (Gates et al. 1993; Rosenhall and Sundh 2006; Liew et al. 2007). In addition to an important methodological consideration as an explanation for inconsistent findings between hearing loss and vascular disease, gender differences in vascular aging could contribute to low frequency hearing loss in women. For example, women can exhibit smaller and less compliant carotid and vertebral arteries (Hansen et al. 1995; Gatzka et al. 2001). In addition, the modiolar branches of the cochlear artery that support the stria vascularis are controlled by nitric oxide in male but not female gerbils (Reimann et al. 2011), suggesting that the stria vascularis is at greater risk for ischemia and hemorrhage in females when atherosclerosis increases blood pressure in vessels that have limited autoregulation. A gradual decline in the stria vascularis, due to chronic hypertension that produces leaky vessels and that also would produce WMH, could therefore account for the results of the current study and a finding of low frequency hearing loss and retinopathy in women (Torre et al. 2005).
In support of the vascular explanation for presbyacusis, the cochlear artery is susceptible to embolic and hemorrhagic events based on evidence for sudden sensorineural hearing loss due to vertebral artery distribution stroke (Walsted et al. 2000; Lee et al. 2002; Ciccone et al. 2012). These effects are seen in males and females with hypertension, however. In addition, one argument against a female-specific small vessel disease effect on hearing is that men are more likely to experience large and small vessel disease than women (Forster et al. 2009). It is important to note that the male participants contributed to the associations observed in this current study but had relatively reduced probability of WMH and low frequency hearing loss. Future studies could focus on a direct comparison of males and females with hypertension and matched low frequency hearing thresholds to determine the extent to which associations are present only in females when the range and median of low frequency thresholds is equivalent across gender groups.
We have used the term putative small vessel disease to characterize the WMH findings because WMH are consistently related to measures of vascular health (Brickman et al. 2010; Kuo et al. 2010; Soderlund et al. 2003; Cook et al. 2004; Waldstein et al. 2012). There is a possibility that other factors, such as inflammation that produces a leaky blood–brain barrier, could contribute to the current results (Taheri et al. 2011). Indeed, one might expect that people with a history of high blood pressure would have significantly worse low frequency hearing than those without if there was a direct link between vascular disease and hearing. Our results do not show this effect, but rather show an association between WMH and low frequency hearing within people reporting high blood pressure. There are at least three explanations for these high blood pressure specific effects that could not be examined in the current study. First, participants may have varied in how well their high blood pressure was controlled. Second, there could be individual differences in secondary inflammatory and/or autoimmune problems, although diabetes does not appear to be a factor in our sample. Third, the variation in WMH and hearing could reflect the severity of vascular disease and delay in treatment. For example, a study of people with well controlled high blood pressure demonstrated that variation in WMH was related to kidney function (Takami et al. 2012). Longstanding untreated hypertension could affect kidney function and produce widespread vascular damage. Thus, prospective studies on vascular disease and hearing loss will be necessary to characterize if the severity of vascular disease, the quality of high blood pressure control, or other vascular and/or inflammatory risk factors contribute to low frequency hearing loss.
The FLAIR estimate of WMH has been consistently related to vascular health and the distribution of WMH effects in the current study, including the preponderance of large effects in anterior white matter, are consistent with previous findings (Rostrup et al. 2012). Importantly, the WMH association with low frequency hearing occurred in the thalamic radiation that is in a watershed distribution of middle cerebral and anterior cerebral artery support (van der Zwan et al. 1992). The anterior thalamic radiation location of this effect does not likely represent a specific effect of anterior or middle cerebral artery decline on low frequency hearing, but more likely represents regions where our WMH metric was sensitive to small vessel disease and where there was a sufficient range of variation for our correlational analyses to detect effects. Indeed, we would have expected a more posterior circulation effect if there was a specific vessel disease effect in the vertebral artery that supplies that cochlear artery. Future in vivo and ex vivo studies involving quantitative and more sensitive measures of vascular disease than used in the current study are predicted to replicate our results and may be more sensitive to vascular changes throughout the CNS. Importantly, our results appear to be consistent with evidence of retinal vasculature damage in people with low frequency hearing loss (Nash et al. 2011) and may reflect a general decline in vascular health in people with high blood pressure.
The results of the current study add to the extant literature to indicate that vascular disease is one factor that contributes to a pattern of low frequency hearing loss. It is important to note that the findings in the current study were observed in high functioning older adults with a typical range of low frequency hearing thresholds who did not exhibit signs of mild cognitive impairment. While our findings are preliminary due to limited information about the duration and severity of high blood pressure in our participants, they were observed in a relatively large imaging study that is likely representative of the healthy older adult population for whom widespread vessel disease may also affect vascular support to the cochlea and produce a decline in the stria vascularis that causes a drop in the endocochlear potential. As suggested by epidemiological findings (Nash et al. 2011), low frequency hearing loss may be driven in part by factors that can be mediated to limit presbyacusis.
References
Alexander G (1902) Zur pathologischen histologie des ohrenlabyrinthes mit besonderer berücksichtigung des cortischen organes. Arch Ohrenheilkd 56:1–23
Ashburner J (2007) A fast diffeomorphic image registration algorithm. Neuroimage 38:95–113
Ashburner J, Friston KJ (2005) Unified segmentation. Neuroimage 26:839–851
Bainbridge KE, Cheng YJ, Cowie CC (2010) Potential mediators of diabetes-related hearing impairment in the U.S. population: National Health and Nutrition Examination Survey 1999–2004. Diabetes Care 33:811–816
Brant LJ, Gordon-Salant S, Pearson JD, Klein LL, Morrell CH, Metter EJ, Fozard JL (1996) Risk factors related to age-associated hearing loss in the speech frequencies. J Am Acad Audiol 7:152–160
Brickman AM, Reitz C, Luchsinger JA, Manly JJ, Schupf N, Muraskin J, DeCarli C, Brown TR, Mayeux R (2010) Long-term blood pressure fluctuation and cerebrovascular disease in an elderly cohort. Arch Neurol 67:564–569
Ciccone MM, Cortese F, Pinto M, Di Teo C, Fornarelli F, Gesualdo M, Mezzina A, Sabatelli E, Scicchitano P, Quaranta N (2012) Endothelial function and cardiovascular risk in patients with Idiopathic Sudden Sensorineural Hearing Loss. Atherosclerosis 225:511–516
Cook IA, Leuchter AF, Morgan ML, Dunkin JJ, Witte E, David S, Mickes L, O'Hara R, Simon S, Lufkin R, Abrams M, Rosenberg S (2004) Longitudinal progression of subclinical structural brain disease in normal aging. Am J Geriatr Psychiatry 12:190–200
Drettner B, Hedstrand H, Klockhoff I, Svedberg A (1975) Cardiovascular risk factors and hearing loss. A study of 1,000 fifty-year-old men. Acta Otolaryngol 79:366–371
Eckert MA, Keren NI, Roberts DR, Calhoun VD, Harris KC (2010) Age-related changes in processing speed: unique contributions of cerebellar and prefrontal cortex. Front Hum Neurosci 4:10–21
Eckert MA, Cute SL, Vaden KI Jr, Kuchinsky SE, Dubno JR (2012) Auditory cortex signs of age-related hearing loss. J Assoc Res Otolaryngol 13:703–713
Forster A, Gass A, Kern R, Wolf ME, Ottomeyer C, Zohsel K, Hennerici M, Szabo K (2009) Gender differences in acute ischemic stroke: etiology, stroke patterns and response to thrombolysis. Stroke 40:2428–2432
Friedland DR, Cederberg C, Tarima S (2009) Audiometric pattern as a predictor of cardiovascular status: development of a model for assessment of risk. Laryngoscope 119:473–486
Gates GA, Cobb JL, D'Agostino RB, Wolf PA (1993) The relation of hearing in the elderly to the presence of cardiovascular disease and cardiovascular risk factors. Arch Otolaryngol Head Neck Surg 119:156–161
Gatzka CD, Kingwell BA, Cameron JD, Berry KL, Liang YL, Dewar EM, Reid CM, Jennings GL, Dart AM, ANBO2 investigators (2001) Australian Comparative Outcome Trial of Angiotensin-Converting Enzyme Inhibitor- and Diuretic-Based Treatment of Hypertension in the Elderly. Gender differences in the timing of arterial wave reflection beyond differences in body height. J Hypertens 19:2197–2203
Gouw AA, Seewann A, van der Flier WM, Barkhof F, Rozemuller AM, Scheltens P, Geurts JJ (2011) Heterogeneity of small vessel disease: a systematic review of MRI and histopathology correlations. J Neurol Neurosurg Psychiatry 82:126–135
Gratton MA, Schmiedt RA, Schulte BA (1996) Age-related decreases in endocochlear potential are associated with vascular abnormalities in the stria vascularis. Hear Res 102:181–190
Gratton MA, Schulte BA, Smythe NM (1997) Quantification of the stria vascularis and strial capillary areas in quiet-reared young and aged gerbils. Hear Res 114:1–9
Hansen F, Mangell P, Sonesson B, Lanne T (1995) Diameter and compliance in the human common carotid artery—variations with age and sex. Ultrasound Med Biol 21:1–9
Heliopoulos I, Artemis D, Vadikolias K, Tripsianis G, Piperidou C, Tsivgoulis G (2012) Association of ultrasonographic parameters with subclinical white-matter hyperintensities in hypertensive patients. Cardiovasc Psychiatry Neurol 2012:616572
Helzner EP, Patel AS, Pratt S, Sutton-Tyrrell K, Cauley JA, Talbott E, Kenyon E, Harris TB, Satterfield S, Ding J, Newman AB (2011) Hearing sensitivity in older adults: associations with cardiovascular risk factors in the health, aging and body composition study. J Am Geriatr Soc 59:972–979
Jerger J, Chmiel R (1997) Factor analytic structure of auditory impairment in elderly persons. J Am Acad Audiol 8:269–276
Johnsson LG, Hawkins JE Jr (1972) Strial atrophy in clinical and experimental deafness. Laryngoscope 82:1105–1125
Kuo HK, Chen CY, Liu HM, Yen CJ, Chang KJ, Chang CC, Yu YH, Lin LY, Hwang JJ (2010) Metabolic risks, white matter hyperintensities, and arterial stiffness in high-functioning healthy adults. Int J Cardiol 143:184–191
Lee FS, Matthews LJ, Dubno JR, Mills JH (2005) Longitudinal study of pure-tone thresholds in older persons. Ear Hear 26:1–11
Lee H, Sohn SI, Jung DK, Cho YW, Lim JG, Yi SD, Lee SR, Sohn CH, Baloh RW (2002) Sudden deafness and anterior inferior cerebellar artery infarction. Stroke 33:2807–2812
Liew G, Wong TY, Mitchell P, Newall P, Smith W, Wang JJ (2007) Retinal microvascular abnormalities and age-related hearing loss: the Blue Mountains hearing study. Ear Hear 28:394–401
Makishima K (1978) Arteriolar sclerosis as a cause of presbycusis. Otolaryngol 86:322–326
Mom T, Chazal J, Gabrillargues J, Laurent G, Avan P (2005) Cochlear blood supply: an update on anatomy and function. Otorhinolaryngol Française 88:81–88
Murray ME, Vemuri P, Preboske GM, Murphy MC, Schweitzer KJ, Parisi JE, Jack CR Jr, Dickson DW (2012) A quantitative postmortem MRI design sensitive to white matter hyperintensity differences and their relationship with underlying pathology. J Neuropathol Exp Neurol 71:1113–1122
Nash SD, Cruickshanks KJ, Klein R, Klein BE, Nieto FJ, Huang GH, Pankow JS, Tweed TS (2011) The prevalence of hearing impairment and associated risk factors: the Beaver Dam Offspring Study. Arch Otolaryngol Head Neck Surg 137:432–439
Nelson EG, Hinojosa R (2003) Presbycusis: a human temporal bone study of individuals with flat audiometric patterns of hearing loss using a new method to quantify stria vascularis volume. Laryngoscope 113:1672–1686
Pauler M, Schuknecht HF, White JA (1988) Atrophy of the stria vascularis as a cause of sensorineural hearing loss. Laryngoscope 98:754–759
Pearson JD, Morrell CH, Gordon-Salant S, Brant LJ, Metter EJ, Klein LL, Fozard JL (1995) Gender differences in a longitudinal study of age-associated hearing loss. J Acoust Soc Am 97:1196–1205
Perez Villa J, Perez Villa FC, Morello A, Betriu A, Traserra J (1995) Neurosensory hearing loss associated with ischemic heart disease. Features and prognostic values. Acta Otorrinolaringol Espanola 46:165–170
Pirodda A, Ferri GG, Modugno GC, Gaddi A (1999) Hypotension and sensorineural hearing loss: a possible correlation. Acta Otolaryngol 119:758–762
Pratt SR, Kuller L, Talbott EO, McHugh-Pemu K, Buhari AM, Xu X (2009) Prevalence of hearing loss in black and white elders: results of the Cardiovascular Health Study. J Speech Lang Hear Res 52:973–989
Reimann K, Krishnamoorthy G, Wier WG, Wangemann P (2011) Gender differences in myogenic regulation along the vascular tree of the gerbil cochlea. PLoS One 6:e25659
Rosen S, Olin P (1965) Hearing loss and coronary heart disease. Arch Otolaryngol 82:236–243
Rosenhall U, Sundh V (2006) Age-related hearing loss and blood pressure. Noise Health 8:88–94
Rostrup E, Gouw AA, Vrenken H, van Straaten EC, Ropele S, Pantoni L, Inzitari D, Barkhof F, Waldemar G, group Ls (2012) The spatial distribution of age-related white matter changes as a function of vascular risk factors—results from the LADIS study. Neuroimage 60:1597–1607
Salimi-Khorshidi G, Smith SM, Nichols TE (2011) Adjusting the effect of nonstationarity in cluster-based and TFCE inference. Neuroimage 54:2006–2019
Schmidt P, Gaser C, Arsic M, Buck D, Forschler A, Berthele A, Hoshi M, Ilg R, Schmid VJ, Zimmer C, Hemmer B, Muhlau M (2012) An automated tool for detection of FLAIR-hyperintense white-matter lesions in Multiple Sclerosis. Neuroimage 59:3774–3783
Schmiedt RA (2010) Chapter 2: The physiology of cochlear presbycusis. In: Gordon-Salant S, Frisina RD, Popper AN, Fay RR (eds) Springer handbook of auditory research. The aging auditory system, vol 34. Springer, New York, pp 9–38
Schuknecht HF (1974) Presbyacusis. Harvard University Press, Cambridge, MA
Schulte BA, Schmiedt RA (1992) Lateral wall Na, K-ATPase and endocochlear potentials decline with age in quiet-reared gerbils. Hear Res 61:35–46
Smith SM, Nichols TE (2009) Threshold-free cluster enhancement: addressing problems of smoothing, threshold dependence and localisation in cluster inference. Neuroimage 44:83–98
Soderlund H, Nyberg L, Adolfsson R, Nilsson LG, Launer LJ (2003) High prevalence of white matter hyperintensities in normal aging: relation to blood pressure and cognition. Cortex 39:1093–1105
Susmano A, Rosenbush SW (1988) Hearing loss and ischemic heart disease. Am J Otol 9:403–408
Suzuki T, Nomoto Y, Nakagawa T, Kuwahata N, Ogawa H, Suzuki Y, Ito J, Omori K (2006) Age-dependent degeneration of the stria vascularis in human cochleae. Laryngoscope 116:1846–1850
Taheri S, Gasparovic C, Huisa BN, Adair JC, Edmonds E, Prestopnik J, Grossetete M, Shah NJ, Wills J, Qualls C, Rosenberg GA (2011) Blood–brain barrier permeability abnormalities in vascular cognitive impairment. Stroke 42:2158–2163
Takami T, Yamano S, Okada S, Sakuma M, Morimoto T, Hashimoto H, Somekawa S, Saito Y (2012) Major risk factors for the appearance of white-matter lesions on MRI in hypertensive patients with controlled blood pressure. Vasc Health Risk Manag 8:169–176
Thomopoulos GN, Spicer SS, Gratton MA, Schulte BA (1997) Age-related thickening of basement membrane in stria vascularis capillaries. Hear Res 111:31–41
Torre P, Cruickshanks KJ, Klein BE, Klein R, Nondahl DM (2005) The association between cardiovascular disease and cochlear function in older adults. J Speech Lang Hear Res 48:473–481
van der Zwan A, Hillen B, Tulleken CA, Dujovny M, Dragovic L (1992) Variability of the territories of the major cerebral arteries. J Neurosurg 77:927–940
Verschuur CA, Dowell A, Syddall HE, Ntani G, Simmonds SJ, Baylis D, Gale CR, Walsh B, Cooper C, Lord JM, Sayer AA (2012) Markers of inflammatory status are associated with hearing threshold in older people: findings from the Hertfordshire Ageing Study. Age Ageing 41:92–97
Waldstein SR, Wendell CR, Lefkowitz DM, Siegel EL, Rosenberger WF, Spencer RJ, Manukyan Z, Katzel LI (2012) Interactive relations of blood pressure and age to subclinical cerebrovascular disease. J Hypertens 30:2352–2356
Walsted A, Andreassen UK, Berthelsen PG, Olesen A (2000) Hearing loss after cardiopulmonary bypass surgery. Eur Arch Otorhinolaryngol 257:124–127
Acknowledgments
This work was supported by the National Institutes of Health/National Institute on Deafness and Other Communication Disorders (P50 DC 00422), South Carolina Clinical and Translational Research (SCTR) Institute, with an academic home at the Medical University of South Carolina, National Institutes of Health/National Center for Research Resources (UL1 RR029882), and the MUSC Center for Biomedical Imaging. This investigation was conducted in a facility constructed with support from Research Facilities Improvement Program (C06 RR14516) from the National Center for Research Resources, National Institutes of Health. We thank the study participants and members of the MUSC Hearing Research Program, including Lois Matthews, and Anita Ramsetty, MD, who provided guidance about medication classification.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Eckert, M.A., Kuchinsky, S.E., Vaden, K.I. et al. White Matter Hyperintensities Predict Low Frequency Hearing in Older Adults. JARO 14, 425–433 (2013). https://doi.org/10.1007/s10162-013-0381-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10162-013-0381-4