Abstract
Background
Thrombotic microangiopathy (TMA) includes hemolytic uremic syndrome (HUS) and thrombotic thrombocytopenic purpura (TTP). This study examined the epidemiological characteristics of pediatric patients with TMA classified according to etiology.
Methods
The survey evaluated 258 Japanese pediatric patients diagnosed with TMA between 2012 and 2015.
Results
The primary diseases responsible for TMA were categorized as TTP (15 cases), Shiga toxin-producing Escherichia coli-associated HUS (STEC-HUS) (166 cases), atypical HUS (aHUS) (40 cases), and secondary TMA (27 cases). The remaining 10 cases were unable to be classified to one of the four categories of the primary disease. Renal replacement therapy was required in the acute phase in 103 patients with TMA, including 65 with STEC-HUS, 22 with aHUS, two with TTP, 10 with secondary TMA, and four unclassified cases. The last observational findings were normal renal function in 95 patients and chronic kidney disease (CKD) stage 1 in 62. For 31 patients, chronic renal insufficiency (CKD stage 2-5) persisted, including four patients with end-stage kidney disease (CKD stage 5). Seventeen patients suffered recurrence of TMA, and eight patients died.
Conclusion
This study clarified differences in the relative proportions of primary diseases between patients from Japan and North America and Europe. The difference may be attributable to the lower estimated incidence of STEC-HUS in Japan.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Thrombotic microangiopathy (TMA) is a systemic pathological phenomenon comprising systemic consumptive thrombocytopenia, microangiopathic hemolytic anemia, and microvascular thrombosis, with potential end-organ damage resulting from deposition of micro thrombi. Common forms of TMA include hemolytic uremic syndrome (HUS) and thrombotic thrombocytopenic purpura (TTP) caused by severely reduced activity (≤ 10% of normal) of a disintegrin-like metalloproteinase with thrombospondin type I repeat motifs (ADAMTS13). The term HUS encompasses a heterologous group of disorders, including STEC-HUS (typical HUS) due to infection by Shiga toxin-producing Escherichia coli (STEC), and atypical HUS (aHUS), in which there is genetic or acquired dysregulation of the alternative pathway of the complement system. Additionally, HUS can occur as a complication of various diseases and conditions, including autoimmune disease, pregnancy, medications, cancers, and hematopoietic stem-cell or solid organ transplantation. These conditions have been referred to as secondary HUS or secondary TMA.
In the past two decades, experimental, genetic, and clinical studies have helped clarify the pathogenesis and pathophysiological mechanisms of TMA including HUS and TTP as well as classification of the disease based on etiology. The current study sought to clarify in detail the epidemiological and demographic characteristics of pediatric patients with TMA classified according to etiology. This study describes the basic epidemiological and demographic characteristics of Japanese children with TMA treated between 2012 and 2015.
Methods
Data collection
We conducted a cross-sectional nationwide survey in 2015 to evaluate Japanese pediatric patients who were diagnosed with TMA and followed between 2012 and 2015. Individual patient data included age at onset, gender, primary underlying disease, and significant events such as death.
Data were collected from questionnaires sent in two phases. The first questionnaire was aimed at patients diagnosed with TMA and followed between 2012 and 2015 and was sent to 1701 hospitals throughout Japan that had more than 20 beds and specialized in pediatrics. The second questionnaire, which asked for data about individual patients, was sent to the hospitals that reported having patients with TMA.
Statistical analysis
Data are expressed as median, range or number, as appropriate. Statistical analyses were performed using JMP software (ver. 12.0; SAS Institute, Cary, NC, USA). The Mann–Whitney U test was used for non-categorical variables in univariate analyses.
Results
Patients collected for the survey
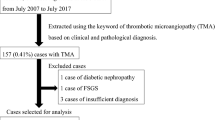
The first questionnaire was sent to 1701 hospitals, and 1077 (63.8%) responded. Among them, 96 hospitals reported having patients with TMA between 2012 and 2015 and agreed to cooperate with the second phase of the survey. Responses to the first questionnaire yielded 302 patients. The second questionnaire was sent to the 96 hospitals, and 75 (78.9%) responded. They reported 258 pediatric patients with TMA, including 111 male patients, 140 female patients, and seven patients for whom gender was not specified.
Primary diseases responsible for TMA
Among the 258 pediatric patients with TMA evaluated in this study, the primary diseases responsible for TMA were categorized as (1) TTP, (2) STEC-HUS, (3) aHUS (complement-associated HUS), and (4) secondary TMA, according to the TMA classification of TMA adopted in the clinical guide for atypical HUS in Japan [1]. The most frequent primary disease was STEC-HUS, which was present in 64.3% (166 cases) of these patients, followed by atypical HUS (40 cases, 15.5%), secondary TMA (27 cases, 10.1%), TTP (15 cases, 5.8%), and unknown primary disease (10 cases, 3.9%). The gene mutations previously reported to be causative for aHUS were detected in only 22 patients (55%) diagnosed as having aHUS. Among patients with secondary TMA, infection-related HUS was the most frequently reported etiology (14/27 cases, 51.8%), followed by rheumatic disease-associated HUS (6/27 cases, 22.2%), and transplantation-associated HUS (5/27 cases, 18.5%). Of the other two patients with secondary HUS, one had drug-associated HUS (cyclophosphamide was considered the causative drug), and the other patient’s mother had been affected by gestational hypertension. Patients diagnosed with infection-associated HUS were categorized into bacterial and viral groups according to the causative organism. The bacterial group included two cases of Streptococcus pneumonia, and one case each of Bordetella pertussis, Staphylococcus aureus, and Mycoplasma pneumonia. The viral group included two cases of Epstein–Barr virus, and one case each of herpes simplex virus, herpes zoster virus, human herpesvirus-6, and clinically diagnosed hand-foot-mouth disease-associated (the causative virus was not determined for virology). The causative pathogen was not identified in the other three cases. Only two patients were reportedly diagnosed with Streptococcus pneumonia-associated HUS among those classified with infection-associated HUS. Patients diagnosed with rheumatic disease-associated HUS included two patients with systemic lupus erythematosus, two with anti-phospholipid syndrome, one with systemic lupus erythematosus and Sjögren’s syndrome, and one with NFκB essential modulator dysfunction. The serotypes of STEC that contributed to the development of HUS are shown in Table 1. Although STEC O157 was detected most frequently (134/166 cases, 80.7%), other STEC serotypes (O111, O121, O6, O126, O76, O26, O25, O165, O145, O1, and O18) were present.
Clinical characteristics, complications in the acute phase, treatment, and final outcomes
The characteristics, complications in the acute phase, treatment, and final outcomes of the patients in the four categories are shown in Tables 2 and 3. Median ages at onset for STEC-HUS, aHUS, TTP, and secondary TMA were 4.1, 4.2, 8.9, and 5.2 years, respectively. There were no significant differences in age at onset among patients in the four categories.
Various complications manifested in the acute phase. The most frequent complication in the acute phase was hypertension (82/258 cases, 31.8%), followed by neurological involvement (69/258 cases, 26.7%) including convulsion, consciousness disturbance, intracranial hemorrhage, cerebral infarction, acute encephalopathy, polyneuritis, and posterior leukoencephalopathy syndrome. The cardiovascular complications (10/258 cases, 3.9%) were in the acute phase included myocarditis, congestive heart failure, pulmonary hypertension, pericardial effusion, and cardiac tamponade. Gastrointestinal complications in the acute phase occurred in 55 (33.1%) of the 166 patients with STEC-HUS. Excluding characteristic gastrointestinal symptoms of STEC infection such as hemorrhagic colitis, hematochezia, and intestinal swelling, 21 patients (12.7%) had other severe gastrointestinal symptoms, including colon stricture, gastrointestinal perforation, intussusception, cholelithiasis, cholecystitis, and pancreatitis. Gastrointestinal symptoms also occurred in patients with aHUS (7/40 cases, 17.5%), TTP (1/15 cases, 6.7%), and secondary TMA (12/27 cases, 44.4%). In total, gastrointestinal involvement was evident in 77 cases (29.8%) of TMA in the acute phase.
Renal replacement therapy was required in the acute phase in 103 patients with TMA, including 65 with STEC-HUS, 22 with aHUS, two with TTP, 10 with secondary TMA, and four unclassified cases. The last findings in terms of renal functions are shown in Table 3. Among 188 patients for whom urinary findings were reported, 95 (36.8%) had normal renal function with normal urinalysis parameters, and 62 (24.0%) were classified as chronic kidney disease (CKD) stage 1. However, in 31 patients (12.0%), chronic renal insufficiency (CKD stage 2–5) persisted, including four patients with end stage kidney disease (CKD stage 5). The patients with stage 5 CKD included two with aHUS (one had a CFH mutation and the other had no mutation), one patient with systemic lupus erythematosus and Sjögren’s syndrome-associated HUS, and one unclassified case. Among the four disease categories, none of the patients with STEC-HUS or TTP were at CKD stage 5, and all patients with TTP had final renal outcomes that were CKD stage 1, including eight with normal urinalysis parameters.
Eight patients died but there were no fatal outcomes among those with STEC-HUS. The eight patients who died included two with aHUS (one had a C3 R425C mutation and the other had no mutation), one with TTP, four with secondary HUS (three with hematopoietic stem cell transplantation-associated HUS and the other with drug-induced HUS), and one unclassified case. Seventeen patients suffered recurrence of TMA (five with TTP, nine with aHUS, two with secondary HUS, and one not specified). Among extrarenal complications, the most frequent final outcomes in all four categories were hypertension (15 patients) and neuro-psychological complications (13 patients) including epilepsy, seizure, hemiparesis, autism, hyperkinesis, and attention deficit/hyperactivity disorder (ADHD).
Discussion
This study clarified the epidemiological and demographic background of Japanese pediatric patients with TMA between 2012 and 2015, including incidence, primary disease responsible for TMA, and outcomes. It is reported that among children with HUS, 85–90% have STEC-HUS, 5–10% have aHUS and ~ 5% have Streptococcus pneumoniae-associated HUS, with TTP and secondary HUS apparently being very rare in children [2]. In North Italian cohorts, the ratio of STEC-HUS to aHUS, including pneumonia-associated HUS, methyl-malonic aciduria, and complement-associated HUS, was reported to be about 9:1 [3]. In the current study, we found that the incidences of aHUS, TTP, and secondary TMA were relatively higher than in previous reports, although STEC-HUS was predominant in this current Japanese pediatric series.
In Japan, any case of enterohemorrhagic Escherichia coli infection must be reported to the public health center, and the annual number of new patients is recorded. According to a report from the National Institute for Infectious Diseases in Japan [4,5,6,7], the numbers of pediatric patients under 15 years of age newly diagnosed with STEC-HUS each year between 2012 and 2015 were 64, 71, 76, and 59, respectively. In this 4-year period, the total number of pediatric patients with STEC-HUS under 15 years of age was 270. In the current series, 302 pediatric patients with TMA were reported among the responses to the first questionnaire. As the rate of response to the first questionnaire was 63.8%, and the ratio of TMA patients with STEC-HUS was 64.3%, the estimated number of patients who would have developed STEC-HUS during these 4 years would have been 306 if the disease ratio had been constant. This estimated value is similar to that reported by the National Institute for Infection Diseases, suggesting that the number of such patients in this study reliable.
The annual incidence of STEC-HUS in Japan estimated from the number of patients reported by the National Institute for Infectious Diseases between 2012 and 2015 was 0.37–0.47 cases per 100,000 children aged < 15 years. This is approximately half the corresponding incidence reported in North America and Europe [3, 8]. Therefore, the ratio of aHUS, TTP, and secondary TMA might have become comparatively high. Because the estimated annual incidence of STEC-HUS was estimated calculated among ≤ 18-year-old children in North America and Europe and ≤ 15-year-old children in Japan, the annual incidence in Japan might be underestimated compared with North America and Europe [9]. On the other hand, because beef cattle are considered to carry STEC in their intestine, the difference in the annual consumption of beef cattle might be related to the incidence of STEC-HUS. However, although the annual consumption of beef per person in North America and Europe is much higher than that in Japan, the annual incidence of STEC infection in the United States is approximately equivalent to that in Japan [10, 11]. From this view point, although the high rate of cattle beef consumption per person might influence the severity of STEC-HUS in North America and Europe, the difference in the annual incidence of STEC-HUS in North America and Europe versus Japan cannot be clearly explained.
The causative pathogens of infection-associated HUS were various viruses and bacteria in this study. A further study is necessary to clarify whether the reported infectious pathogens cause HUS or trigger the occurrence of HUS.
Various extrarenal complications occur in the acute phase of STEC-HUS, including hypertension, severe gastrointestinal involvement, pancreatitis, diabetes mellitus, central nervous system involvement, and myocardial involvement [12]. Hypertension and neurological involvement have been reported in up to 25 and 20–30% of patients with STEC-HUS, respectively [13,14,15]. In the current study, hypertension and neurological symptoms occurred in 25.9 and 19.3% of STEC-HUS patients, respectively. These incidence rates are similar to those in previous reports [13,14,16].
Gastrointestinal symptoms were reported in 55 patients (33.1%) with STEC-HUS. The number of STEC-HUS patients presenting with gastrointestinal symptoms appears low. A reason for this might be that gastrointestinal symptoms including hemorrhagic colitis, hematochezia, and intestinal swelling were not included in the questionnaire as gastrointestinal complications of STEC-HUS in the acute phase as they are the main complications associated with acute enterocolitis due to STEC infection.
Twenty-one patients (12.7%) with STEC-HUS had severe gastrointestinal complications including colon stricture, gastrointestinal perforation, intussusception, cholelithiasis, cholecystitis, and pancreatitis. The frequency of gastrointestinal complications was compatible with a previous report [2]. Gastrointestinal complications in the other three categories included hematochezia, hemorrhagic colitis, and intestinal swelling. Over 10% of TMA patients except those with STEC-HUS showed gastrointestinal involvement. This result was compatible with previous reports in which as many as 30% of aHUS patients had at least some gastrointestinal symptoms [2, 17]. Therefore, aHUS should not be excluded based only on the presence of gastrointestinal symptoms, including diarrhea. Especially in Japan, where the incidence of aHUS is relatively higher than that in other countries, the differential diagnoses of aHUS and STEC-HUS should be considered with extreme caution.
Our survey revealed that central nervous system involvement was a common and important feature. In the acute phase, hypertension and neurological complications were most frequent and appeared in 31.8 and 26.7% of patients, respectively. Although these frequencies decreased to 5.8 and 4.2%, respectively, at the final observation point, careful observation and therapy for both complications are necessary from the acute phase to the chronic phase.
Forty patients with aHUS were reported in this series, among whom only 22 (55%) had complement gene mutations, with the remaining 18 (45%) having no detectable mutations. In Japan, most patients diagnosed with aHUS are registered in an aHUS registry, and gene mutation analysis for aHUS, which includes seven genes (CFH, CFI, C3, CFB, MCP, THBD, and DGKE) is performed. The ratio of gene mutation detection was compatible with that reported previously [17,18,19]. Therefore, an absence of causative genetic mutations does not always exclude a diagnosis of aHUS, even though confirmatory diagnosis of aHUS requires genetic testing for known causative genes and analysis of anti-complement factor H antibodies.
With regard to renal function of patients with TMA at the time of the last observation, the percentage of those with urinary abnormalities including hematuria or proteinuria was around 40% in all categories. There was no difference in percentages among the four categories of TMA. The percentage of TMA patients with moderate to severe deterioration of renal function (CKD stage 3–5) was 4.0% and was higher in patients with secondary TMA (11.1%) and aHUS (5.0%) than those with STEC-HUS (1.8%). The mortality rate of patients with TMA was 2.7%, although none of the patients reported to have had STEC-HUS died. The percentage of patients with aHUS who showed progression to end-stage kidney disease or who died was 10.0%. This percentage is compatible with a previously reported value of 9.0% in a 1-year follow-up study after introduction of eculizumab therapy [2].
Various extrarenal sequelae were observed in the current study. Among them, hypertension and neuro-psychological sequelae, including epilepsy, encephalopathy, and autism affected about 5–6% of patients. As the central pathological features of TMA are endothelial cell injury and microthrombus formation, and as TMA is a systemic disease, detailed follow-up for extra-renal complications is necessary.
In conclusion, this survey of epidemiological and demographic information for Japanese pediatric patients with TMA between 2012 and 2015 confirmed the differences in the proportions of underlying primary diseases that have been reported previously. The lower annual incidence of STEC-HUS in Japan might have contributed to the differences in the proportions of primary diseases in comparison with those documented previously.
References
Kato H, Nangaku M, Hataya H, Sawai T, Ashida A, Fujimaru R, Hidaka Y, Kaname S, Maruyama S, Yasuda T, Yoshida Y, Ito S, Hattori M, Miyakawa Y, Fujimura Y, Okada H, Kagami S, The Joint Committee for the Revision of Clinical Guides of Atypical Hemolytic Uremic Syndrome in Japan. Clinical guides for atypical hemolytic uremic syndrome in Japan. Clin Exp Nephrol. 2016;20:536–43. https://doi.org/10.1007/s10157-016-1276-6.
Fakhouri F, Zuber J, Frémeaux-Bacchi V, Loirat C. Haemolytic uraemic syndrome. Lancet. 2017. https://doi.org/10.1016/S0140-6736(17)30062-4 (Epub ahead of Print).
Ardissino G, Salardi S, Colombo E, Testa S, Borsa-Ghiringhelli N, Paglialonga F, Paracchini V, Tel F, Possenti I, Belingheri M, Civitillo CF, Sardini S, Ceruti R, Baldioli C, Tommasi P, Parola F, Tedeschi S. Epidemiology of haemolytic uremic syndrome in children. Data from the North Italian HUS network. Eur J Pediatr. 2016;175:465–73. https://doi.org/10.1007/s00431-015-2642-1.
National Institute of Infection Diseases and Tuberculosis and Infectious Diseases Control Division, Ministry of Health, Labour and Welfare. Infectious agents surveillance report. 2016;37:85–102. http://www.nih.go.jp/niid/ja/iasr.html. Accessed 7 June 2017
National Institute of Infection Diseases and Tuberculosis and Infectious Diseases Control Division, Ministry of Health, Labour and Welfare. Infectious agents surveillance report. 2015;36:73–92. http://www.nih.go.jp/niid/ja/iasr.html. Accessed 7 June 2017
National Institute of Infection Diseases and Tuberculosis and Infectious Diseases Control Division, Ministry of Health, Labour and Welfare. Infectious agents surveillance report. 2014;35:117–36. http://www.nih.go.jp/niid/ja/iasr.html. Accessed 7 June 2017
National Institute of Infection Diseases and Tuberculosis and Infectious Diseases Control Division, Ministry of Health, Labour and Welfare. Infectious agents surveillance report. 2013;34:123–54. http://www.nih.go.jp/niid/ja/iasr.html. Accessed 7 June 2017
Ong KL, Apostal M, Comstock N, Hurd S, Webb TH, Mickelson S, Scheftel J, Smith G, Shiferaw B, Boothe E, Gould LH. Strategies for surveillance of pediatric hemolytic uremic syndrome: Foodborne disease active surveillance network (FoodNet), 2000–2007. Clin Infect Dis. 2012;54:S424–31. https://doi.org/10.1093/cid/cis208.
OECD-FAO Agricultural outlook (2017) Meat consumption. https://data.oecd.org/agroutput/meat-consumption.htm. Accessed 7 June 2017
Centers for Disease Control and Prevention. Morbidity and Mortality Weekly Report (MMWR). Incidence and trends of infection with pathogens transmitted commonly through food—foodborne disease active surveillance network, 10 US sites, 2006–2013. https://www.cdc.gov/mmwr/preview/mmwrhtml/mm6315a3.htm. Accessed 7 June 2017
Morita-Ishihara T, Iyoda S, Iguchi A, Ohnishi M. Emerg Infect Dis. 2016;22:2181–4. https://doi.org/10.3201/eid2212.160783.
Scheiring J, Andreoli SP, Zimmerhackl LB. Treatment and outcome of Shiga-toxin-associated hemolytic uremic syndrome (HUS). Pediatr Nephrol. 2008;23:1749–60. https://doi.org/10.1007/s00467-008-0935-6.
Gerber A, Karch H, Allerberger F, Verweyen HM, Zimmerhackl LB. Clinical course and the role of Shiga toxin-producing Escherichia coli infection in the hemolytic-uremic syndrome in pediatric patients, 1997–2000, in Germany and Austria: a prospective Study. J Infect Dis. 2002;186:493–500. https://doi.org/10.1086/341940.
Spinale JM, Ruebner RL, Copelovitch L, Kaplan BS. Long-term outcomes of Shiga toxin hemolytic uremic syndrome. Pediatr Nephrol. 2013;28:2097–105. https://doi.org/10.1007/s00467-012-2383-6.
Rosales A, Hofer J, Zimmerhackl LB, Jungraithmayr TC, Riedl M, Giner T, Strasak A, Orth-Höller D, Wüzner R, Karch H, For the German–Austrian HUS Study Group. Need for long-term follow-up in enterohemorrhagic Escherichia coli-associated hemolytic uremic syndrome due to late-emerging sequelae. Clin Infect Dis. 2012;54:1413–21. https://doi.org/10.1093/cid/cis196.
Durkan AM, Kim S, Craig J, Elliot E. The long-term outcomes of atypical haemolytic uraemic syndrome: a national surveillance study. Arch Dis Child. 2016;101:387–91. https://doi.org/10.1136/archdischild-2015-309471.
Noris M, Caprioli J, Bresin E, Mossali C, Pianetti G, Gamba S, Daina E, Fenili C, Castelletti F, Sorosina A, Piras R, Donadelli R, Maranta R, van der Meer I, Conway EM, Zipfel PF, Goodship TH, Remuzzi G. Relative role of genetic complement abnormalities in sporadic and familial aHUS and their impact on clinical phenotype. Clin J Am Soc Nephrol. 2010;5:1844–59. https://doi.org/10.2215/CJN.02210310.
Fremeaux-Bacchi V, Fakhouri F, Gamier A, Bienaímé F, Dragon-Durey MA, Ngo S, Moulin B, Servais A, Provot F, Rostaing L, Burtey S, Niaudet P, Deschênes G, Lebranchu Y, Zuber J, Loirat C. Genetics and outcome of atypical hemolytic uremic syndrome: a nationwide French series comparing children and adults. Clin J Am Soc Nephrol. 2013;8:554–62. https://doi.org/10.2215/CJN.04760512.
Maga TK, Nishimura CJ, Weaver AE, Frees KL, Smith RJH. Mutations in alternative pathway complement proteins in American patients with atypical hemolytic uremic syndrome. Hum Mutat Brief. 2010;31:E1445–60. https://doi.org/10.1002/humu.21256.
Acknowledgements
This study was supported by a grant from the Ministry of Health, Labour and Welfare of Japan for Research on Rare Intractable Diseases of the Kidney and Urinary Tract (H26-nanchitou (nan)-ippan-036 to Kazumoto Iijima). The authors thank the patients and their families, physicians, and the institutions who contributed to this study. They also thank Edanz Group (http://www.edanzediting.com) for editing a draft of this manuscript.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Kazumoto Iijima had endowed department by Astellas Pharma, and has received grants from Daiichi Sankyo Co., Ltd., Toshihiro Sawai received travel fees from Alexion Pharma. The other authors declare that they have no conflicts of interest.
Research involving human participants
The survey was conducted in accordance with the ethical principles contained within the 1964 Declaration of Helsinki, and the ethical guidelines for epidemiological studies issued by the Ministry of Health, Labour and Welfare, Japan. The survey was approved by the ethics board of Osaka Medical College (approval number: 1823) before the study commenced.
Informed consent
For this type of study, formal consent was not required.
About this article
Cite this article
Ashida, A., Matsumura, H., Sawai, T. et al. Clinical features in a series of 258 Japanese pediatric patients with thrombotic microangiopathy. Clin Exp Nephrol 22, 924–930 (2018). https://doi.org/10.1007/s10157-018-1531-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10157-018-1531-0