Abstract
Background
Anemia associated with high mortality is a common complication of chronic kidney disease (CKD). Target hemoglobin (Hb) levels for CKD treatment remain controversial: Recent guidelines recommend a maximum of 13 g/dL to avoid increased risk of CVD. However, some smaller studies show slower progression of renal function loss with high Hb targets. Recently, darbepoetin alfa targeting Hb 11–13 g/dL was reported to improve renal composite outcome of Japanese patients compared with a low Hb group maintained at 9.0–11.0 g/dL using epoetin alfa (HR 0.66; 95 % CI 0.47–0.93). The high Hb group showed significant reduction of left ventricular mass index and improved quality of life. Sub-analysis revealed greater beneficial effects in non-diabetic stage 5 CKD patients. This randomized controlled trial, PREDICT, aims to confirm the impact of targeting Hb levels of 11–13 g/dL using darbepoetin alfa with reference to a low Hb target of 9–11 g/dL.
Methods
We calculated the number of subjects (N = 440) necessary to detect a statistically significant level of α = 0.05 (two-sided) and statistical power of 80 % for a minimum follow-up period of 2 years on the basis of a previous study.
Results
The study enrolled 498 non-diabetic Japanese patients with eGFR 8–20 mL/min/1.73 m2. The primary outcome is a composite renal endpoint (starting chronic dialysis, transplantation, eGFR 6 mL/min/1.73 m2 or less, 50 % decrease in eGFR). Average follow-up period is 2 years and the study ends in 2016.
Conclusion
PREDICT will determine the optimum target Hb for Japanese patients with non-diabetic CKD.
(ClinicalTrials.gov No. NCT01581073).
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Anemia is a common comorbidity in patients with chronic kidney disease (CKD) [1–3]. Given that anemia is defined by a hemoglobin (Hb) level less than 11 g/dL, 45 % of Japanese patients with CKD have anemia [1]. Anemia is associated with an increased risk of mortality, development of cardiovascular disease (CVD), and progressive loss of renal function in patients with CKD [4, 5].
Correction of anemia in CKD patients using erythropoiesis-stimulating agents (ESA) or iron has been investigated in randomized controlled studies, but the results are inconclusive [6–15]. Randomized controlled trials intentionally targeting Hb levels of 13 g/dL or higher, including the Cardiovascular Risk Reduction by Early Anemia Treatment with Epoetin Beta (CREATE) trial [10], the Correction of Hemoglobin and Outcomes in Renal Insufficiency (CHOIR) trial [11], and the Trial to Reduce Cardiovascular Events With Aranesp Therapy (TREAT) [12], failed to demonstrate beneficial effects and resulted in increased severe adverse events including stroke and CVD. A meta-analysis of 27 trials including 10,452 patients concluded that ESA therapy targeting higher Hb levels leads to increased risk of vascular and fatal events, suggesting that this treatment is harmful for patients with CKD [7]. A meta-analysis of the benefits and harms of darbepoetin alfa used to treat anemia in adults and children with CKD concluded that it reduced the need for blood transfusion but increased the risk of hypertension. Darbepoetin alfa had little or no effect on mortality or quality of life in adult patients with CKD stage 3–5 [8].
However, smaller studies showed improved renal outcome, although the methodology was not as rigorous as in contemporary randomized controlled trials [13–15]. In particular, two randomized controlled studies performed in Japan showed ESA treatment with a higher target Hb of 11.0–13. 0 g/dL reduced renal outcome without increasing the incidence of CV events [13, 15]. This may be due to the low incidence of CVD in Japanese patients and/or targeting a medium level of Hb while avoiding Hb normalization.
In the present randomized controlled study, we will confirm the impact on renal composite outcome of maintaining Hb at 11–13 g/dL using darbepoetin alfa in Japanese patients with non-diabetic advanced CKD in the PREDICT trial (Prevention of end-stage kidney disease by darbepoetin alfa in CKD patients with non-diabetic kidney disease).
Methods
Trial design
This is a multicenter, randomized (1:1), open-label, parallel group study conducted on non-diabetic CKD patients with an eGFR of 8–20 mL/min/1.73 m2. The study was registered to ClinicalTrials.gov (NCT01581073). The study protocol and informed consent form were approved by the institutional review board of each center. All patients received information on the purpose and nature of this study as well as the potential risks and benefits. Thenceforth, written informed consent for participation was obtained from each patient. In addition, this study is being conducted under the health insurance system of Japan, in accordance with the Declaration of Helsinki and the Ethical Guidelines on Clinical Studies of the Ministry of Health, Labor and Welfare of Japan. The study is being performed according to CONSORT 2010 [16].
Participants
The current study enrolled patients aged 20–85 years with CKD undergoing appropriate treatment, who were not on chronic dialysis. Further inclusion criteria were an estimated glomerular filtration rate (eGFR) of 8–20 mL/min/1.73 m2 at least twice within 12 weeks prior to registration; renal anemia with Hb <10 g/dL during the previous 8 weeks; and transferrin saturation (TSAT) >20 % or serum ferritin >100 ng/mL during the previous 8 weeks.
Patients were excluded if they had diabetes, uncontrolled hypertension (>180 mmHg or >110 mmHg), congestive heart failure (NYHA class III and IV), malignancy, hematological disorders, hemorrhagic lesions, malnutrition, continuous hemorrhage from a gastrointestinal ulcer (e.g., duodenal ulcer, ulcerative colitis), anti-neutrophil antibody, acute infection, collagen diseases, or severe allergy (e.g., hypersensitivity to ESA). In addition, patients were excluded when resistance to ESA was suspected in patients treated with epoetin >24,000 U/4 weeks or darbepoetin alfa >90 μg/4 weeks, or the introduction of dialysis or transplant was planned within 6 months after registration. Further exclusion conditions were use of ESA within 3 months before registration, myocardial infarction within 6 months, symptomatic stroke, and pulmonary thrombosis or embolism within 1 year.
Study setting
Patients were enrolled for 3.5 years (from December 2011–June 2014) from 74 institutions across the country. Initially, the enrollment period was one year, but this period was extended due to insufficient accrual of patients and the results of the interim assessment of sample size. Patient follow-up is ongoing and will end in June 2016.
Intervention
Participants were randomly assigned to either the high (11.0–13.0 g/dL) or low (9.0–11.0 g/dL) Hb group. Administration of ESA was initiated within 1 month after randomization and is continued until the final observation or the patient’s death. Patients in the high Hb group have a target Hb of 12.0 g/dL, to maintain Hb at 11.0–13.0 g/dL, with a maximum dosage of 240 μg/month of darbepoetin. If Hb exceeds 13.0 g/dL, darbepoetin is reduced or withheld. Patients in the low Hb group have a target Hb of 10.0 g/dL and are maintained at Hb levels of 9.0–11.0 g/dL. If Hb exceeds 10.0 g/dL, darbepoetin is reduced or stopped. In both groups, blood pressure is maintained at <130/80 mmHg without changing the dosage of angiotensin-converting enzyme (ACE) inhibitors, angiotensin-receptor blockers, renin inhibitor and mineral corticoid receptor blocker during the study period. Carbon sorbents are used without changing the dosage during study period. In addition, iron supplement is administered to maintain serum ferritin ≥100 ng/mL or TAST level ≥20 %, without restriction. Serum lipids are controlled in accordance with clinical practice.
Outcome
The primary endpoint is onset of a composite renal event, consisting of initiation of dialysis, renal transplantation, reaching an eGFR of 6 mL/min/1.73 m2 or less or 50 % reduction in eGFR. The secondary points include onset of a composite CV event, initiation of dialysis, reduction in eGFR (<50 %), all-cause death, change in eGFR, change proteinuria, onset of renal composite outcome in patients who maintained the target Hb level for more than two-thirds of the observational period, onset of stroke, onset of myocardial infarction, and onset of malignancy. A composite CV event consists of CV death, stroke, myocardial infarction, amputation of lower extremities, hospitalization due to heart failure, or hospitalization due to angina. The definition of each event is shown in Table 1.
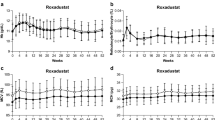
The onset of renal and CV events and maintenance of Hb level are monitored at 12, 24, 36, 48, 60, 72, 84 and 96 weeks and at the completion of this study. The central committee monitored the number of enrolled patients and the mean Hb levels in each group every quarter until the interim assessment. Following the interim assessment, the central committee meets annually. The physicians at each study center evaluate each endpoint. The central committee annually reviews the data submitted from each center, and decisions are corrected if necessary.
Hypertension is defined as a blood pressure of 140/90 mmHg or higher or if a patient is taking antihypertensives. Diabetes is defined as fasting blood glucose ≥126 mg/dL, casual blood glucose ≥200 mg/dL, or blood glucose ≥200 mg/dL 2 h after 75 g oral glucose tolerance test, or HbA1c ≥6.5 %. GFR was estimated by the Japanese equation as follows: GFR = 194 × SCr−1.094 × Age−0.287 (×0.739, if female) [17].
Sample size
Sample size calculations were based on event rates in the high Hb group of a sub-analysis of previous study, in which the event-free rate of the low Hb group was assumed to be 35 % over 2 years of observation, and the hazard ratio of the high Hb group was 0.70 with reference to the low Hb group [15]. Based on these assumptions, 188 patients are needed in each treatment group to detect a statistically significant difference between treatment groups using the log-rank test with α = 0.05 (two-sided) and 1−β = 0.80 for a minimum 2 years of observation. Because of the burden for participants of the high cost of darbepoetin alfa, it was assumed that a certain number of patients would withdraw their consent. Assuming that fewer than 15 % of patients are lost to follow-up, the required sample size was determined to be 220 per group. The 15 % estimate was inaccurate and the final sample size was determined following interim analysis.
Interim assessment for sample size estimation
We performed an interim assessment for sample size re-estimation to obtain the appropriate statistical power, but did not perform an interim assessment of the primary and secondary endpoints. Approximately 2 months before completion of enrollment, using the association between the difference in maintained Hb levels and the hazard ratio for composite renal events that was found in our previous study, the predicted hazard ratio was estimated (using the difference in maintained Hb levels) for the PREDICT trial. Assuming that the difference in maintained Hb levels between the two groups is linearly correlated with the hazard ratio for composite renal events, the sample size was re-estimated.
Based on the results of the interim assessment, the committee recommended a change in the sample size of the study.
Randomization
Patients were enrolled through a web-based registration and follow-up system provided by the data center at the Translational Research Informatics Center, Kobe, Japan. Once the primary physician had obtained patient consent, generally with the support of the clinical research coordinators, access to the system was granted and the physician sent the information required for enrollment. The system automatically evaluated the eligibility of each patient and randomly assigned participants to either the high Hb group or the low Hb group (1:1 allocation). Following randomization, the baseline characteristics of Hb level (<9 vs. ≥9 g/dL), eGFR (<15 mL/min/1.73 m2 vs. ≥15 mL/min/1.73 m2), urinary protein/creatinine ratio (<1.0 g/gCr vs. ≥1.0 g/gCr), and history of ESA use were evenly balanced between the two groups.
Statistical analysis
All patients who have taken darbepoetin at least once will be included in the safety analysis set. The primary efficacy analysis set will be the full analysis set (FAS), based on the intention-to-treat principle. The FAS will include all patients satisfying the following conditions: (1) fulfilled all entry criteria; (2) took the study drug at least once; and (3) were followed up at least once after randomization. The secondary efficacy analysis set will be the per protocol set (PPS), consisting of patients included in the FAS who have no major protocol violations. Patients whose mean Hb for the entire study period does not achieve the target level or the measured Hb achieves the target range for less than half of the observation period are excluded from the PPS.
For the primary renal composite outcome, the two groups will be compared using the log-rank test. Stratified log-rank tests will be performed with allocation factors as stratification factors. The cumulative event rate for each defined event will be estimated by the Kaplan–Meier method for each treatment group. The Cox regression model will be used to estimate the hazard ratios with 95 % confidence intervals for the renal composite event rate with covariates including sex, age, baseline eGFR, baseline Hb, systolic blood pressure and proteinuria. Secondary outcomes measured as time-to-event data will be analyzed using the same methods as for the primary outcome.
The linear mixed effect model, including study drugs, measurement times and other covariates selected after the blind data review, will be used for comparing the trends in the percent change in proteinuria and the reciprocal of the serum creatinine level between treatment groups. Similar analyses for each endpoint will also be applied for the subgroup of each prognostic factor.
Adverse events will be summarized for each treatment group. The cumulative rate of occurrence of all adverse events and drug-related adverse events in each treatment group will be analyzed by Fisher’s exact test. Contingency tables showing the number and percentage of patients within each category of adverse events will also be presented.
Results
We will confirm the effects of targeting an Hb level of 11–13 g/dL using darbepoetin alfa with reference to a control group with a low Hb target of 9–11 g/dL in a randomized control trial, PREDICT. The study has a targeted enrollment of non-diabetic Japanese CKD patients with an eGFR of 8–20 mL/min/1.73 m2. The primary outcome is a composite renal (starting chronic dialysis, transplantation, eGFR 6 mL/min/1.73 m2 or less, 50 % decrease in eGFR).
We planned to enroll 440 patients. In October 2013, when the total number of patients enrolled reached 359, we performed an interim assessment to re-estimate the sample size. Using the association between the difference in maintained Hb levels and the hazard ratio for composite renal events that was found in our previous study, and by measuring the difference in mean Hb levels between both groups at 16 weeks, we estimated the predicted hazard ratio in this study to be 0.733. The result suggested we needed to increase the sample size to 476 patients because a sample of 440 gave 1−β=0.768 with a minimum 2 years of observation. The period for registration was therefore extended to June 2014.
The current study includes 521 patients from 87 participating institutions, enrolled from February 16, 2012 to June 30, 2014. After randomization, 23 patients were ineligible, reducing the total number of eligible patients to 498. The average follow-up period is 2 years and the study ends in June 2016.
Discussion
The PREDICT study asks whether renal outcome will be reduced in non-diabetic patients with advanced CKD by treatment with darbepoetin alfa targeting moderate Hb levels of 11.0–13.0 g/dL, compared with reference control grope with a low Hb target of 9.0–11.0 g/dL. The rationale of PREDICT is as follows.
Effects of diabetes on renal and CV outcome
Patients with diabetes have a higher incidence of CVD than those without, because diabetes is associated with atherosclerosis as well as arteriosclerosis [18, 19]. CV risk is also increased in CKD patients with diabetes. A landmark study, TREAT, asked whether targeting an Hb level of 13.0 g/dL improved CV outcome in diabetic patients with renal anemia [12]. It clearly demonstrated that in diabetic patients with moderately decreased GFR (20–60 mL/min/1.73 m2), a target Hb of 13.0 g/dL and achieved 12.5 g/dL failed to improve CV or renal outcomes. The higher Hb group had significantly fewer CV revascularization events but had significantly higher risk for non-hemorrhagic stroke. In the CHOIR study, approximately 50 % of participants had diabetes (DM), and patients with DM had a greater risk of experiencing a primary endpoint than those without DM (HR 1.30, p = 0.067) [10]. However, the level of Hb did not affect the hazard ratio for the primary CV endpoint in patients with diabetes [20].
Kuriyama et al. demonstrated that patients with CKD treated with epoetinalfa had slower progression of renal failure compared with untreated patients (cumulative survival rates were 48 and 16 %, respectively, p = 0.003) [13]. However, the cumulative survival rate was significantly lower in diabetic than in non-diabetic patients [13]. Tsubakihara et al. reported that the incidence of a composite endpoint consisting of death, end-stage renal disease (ESRD), and doubling of serum creatinine was 39.9 and 32.4 % in the high and low Hb groups, respectively, with no significant difference between the two groups. However, the hazard ratio for the composite renal endpoint in the high Hb group was 0.71 (95 % CI 0.52–0.98, p = 0.035) with reference to the low Hb group, suggesting that maintaining Hb levels at 11.0–13.0 g/dL was beneficial [21]. In a sub-analysis, the benefits of maintaining high Hb were not seen in patients with diabetes.
Overall, the beneficial effects of maintaining high Hb at 11.0–13. 0 g/dL seem to be confined to non-diabetic patients. We therefore excluded patients with diabetes from PREDICT.
Effects of baseline renal function on renal and CV outcome
The large randomized controlled trials, TREAT, CHOIR, and CREATE, enrolled patients with stage 3–4 CKD. In contrast, two Japanese studies that showed beneficial effects of high Hb both included stage 5 patients [13, 15].
In the sub-analysis of a previous study, cumulative renal survival of patients with stage 5 CKD was significantly higher in the high Hb group than in the low Hb group, but there was no difference between the two groups at CKD stage 4 [21].
We therefore enrolled patients with eGFR 8–20 mL/min/1.73 m2 in PREDICT.
Effects of ESA dose on renal and CV outcome
The dosage of ESA used varies among studies. Patients in the high Hb group of CREATE and CHOIR were treated with 5000 U/week and 11,215 U/week of epoetin, respectively [10, 11]. In TREAT, patients in the high Hb group received 176 µg/month of darbepoetin [22].
In a previous study [21], mean weekly doses in the high and low Hb groups were 25–35 µg/week darbepoetin alfa and 3500–4500 IU/week epoetin alfa, respectively; these were relatively small dosages compared to previous randomized controlled trials [10, 11]. We limit the amount of darbepoetin alfa administered to 240 µg/month in PREDICT.
Exception of adverse events in PREDICT
ESA causes several adverse events including hypertension, thrombosis, and malignancy. A meta-analysis revealed a significant increase in the risk of stroke, vascular access thrombosis, and hypertension [8]. In addition, it showed a probable increase in the risk of all-cause death, serious CV events, and end-stage renal disease. In contrast to reports from Western countries, Japanese studies did not find an increase in the risk of severe adverse events [13, 15]. In addition, an observational study, SEASCAN, did not show a difference in incidence of stroke and malignancy in Japanese patients treated with epoetin [23].
Investigation of the safety of ESA in participants is another important objective of PREDICT.
References
Akizawa T, Makino H, Matsuo S, Watanabe T, Imai E, Nitta K, Ohashi Y, Hishida A, Chronic Kidney Disease Japan Cohort Study Group. Management of anemia in chronic kidney disease patients: baseline findings from Chronic Kidney Disease Japan Cohort Study. Clin Exp Nephrol. 2011;15:248–57.
Hsu CY, McCulloch CE, Curhan GC. Epidemiology of anemia associated with chronic renal insufficiency among adults in the United States: results from the Third National Health and Nutrition Examination Survey. J Am Soc Nephrol. 2002;13:504–10.
Astor BC, Muntner P, Levin A, Eustace JA, Coresh J. Association of kidney function with anemia: the Third National Health and Nutrition Examination Survey (1988–1994). Arch Intern Med. 2002;162:1401–8.
Weiner DE, Tighiouart H, Vlagopoulos PT, Griffith JL, Salem DN, Levey AS, Sarnak MJ. Effects of anemia and left ventricular hypertrophy on cardiovascular disease in patients with chronic kidney disease. J Am Soc Nephrol. 2005;16:1803–10.
Al-Ahmad A, Rand WM, Manjunath G, Konstam MA, Salem DN, Levey AS, Sarnak MJ. Reduced kidney function and anemia as risk factors for mortality in patients with left ventricular dysfunction. J Am Coll Cardiol. 2001;38:955–62.
Silverberg DS, Wexler D, Iaina A. The importance of anemia and its correction in the management of severe congestive heart failure. Eur J Heart Fail. 2002;4:681–6.
Palmer SC, Navaneethan SD, Craig JC, Johnson DW, Tonelli M, Garg AX, Pellegrini F, Ravani P, Jardine M, Perkovic V, Graziano G, McGee R, Nicolucci A, Tognoni G, Strippoli GF. Meta-analysis: erythropoiesis-stimulating agents in patients with chronic kidney disease. Ann Intern Med. 2010;153:23–33.
Palmer SC, Saglimbene V, Craig JC, Navaneethan SD, Strippoli GF. Darbepoetin for the anaemia of chronic kidney disease. Cochrane Database Syst Rev. 2014; 3:CD009297. doi:10.1002/14651858.CD009297.pub2.
KDIGO Clinical Practice Guideline for Anemia in Chronic Kidney Disease. Kidney Int Suppl 2012; 2:279–335.
Drüeke TB, Locatelli F, Clyne N, Eckardt KU, Macdougall IC, Tsakiris D, Burger HU, Scherhag A, CREATE Investigators. Normalization of hemoglobin level in patients with chronic kidney disease and anemia. N Engl J Med. 2006;355:2071–84.
Singh AK, Szczech L, Tang KL, Barnhart H, Sapp S, Wolfson M, Reddan D, CHOIR Investigators. Correction of anemia with epoetin alfa in chronic kidney disease. N Engl J Med. 2006;355:2085–98.
Pfeffer MA, Burdmann EA, Chen CY, Cooper ME, de Zeeuw D, Eckardt KU, Feyzi JM, Ivanovich P, Kewalramani R, Levey AS, Lewis EF, McGill JB, McMurray JJ, Parfrey P, Parving HH, Remuzzi G, Singh AK, Solomon SD, Toto R, TREAT Investigators. A trial of darbepoetin alfa in type 2 diabetes and chronic kidney disease. N Engl J Med. 2009;361:2019–32.
Kuriyama S, Tomonari H, Yoshida H, et al. Reversal of anemia by erythropoietin therapy retards the progression of chronic renal failure, especially nondiabetic patients. Nephron. 1997;77:176–85.
Gouva C, Nikolopoulos P, Ioannidis JP, Siamopoulos KC. Treating anemia early in renal failure patients slows the decline of renal function: a randomized controlled trial. Kidney Int. 2004;66:753–60.
Tsubakihara Y, Gejyo F, Nishi S, Iino Y, Watanabe Y, Suzuki M, Saito A, Akiba T, Hirakata H, Akizawa T. High target hemoglobin with erythropoiesis-stimulating agents has advantages in the renal function of non-dialysis chronic kidney disease patients. Ther Apher Dial. 2012;16:529–40.
Schulz KF, Altman DG, Moher D, CONSORT Group. CONSORT 2010 statement: updated guidelines for reporting parallel group randomized trials. Ann Intern Med. 2010;152:726–32.
Mastuo S, Imai E, Horio M, Yasuda Y, Tomita K, Nitta K, Yamagata K, Tomino Y, Yokoyama H, Hishida A. Revised equations for estimating glomerular filtration rate (GFR) from serum creatinine in Japan. Am J Kidney Dis. 2009;53:982–92.
Collins AJ, Foley RN, Chavers B, et al. US Renal Data System 2013 Annual Data Report. Am J Kidney Dis. 2014;63(1 Suppl):A7.
Fox CS, Matsushita K, Woodward M, Bilo HJ, Chalmers J, Heerspink HJ, Lee BJ, Perkins RM, Rossing P, Sairenchi T, Tonelli M, Vassalotti JA, Yamagishi K, Coresh J, De Jong PE, Wen CP, Nelson RG, Kidney Disease Prognosis Consortium. Associations of kidney disease measures with mortality and end-stage renal disease in individuals with and without diabetes: a meta-analysis. Lancet. 2012;380:1662–73.
Szczech LA, Barnhart HX, Sapp S, Felker GM, Hernandez A, Reddan D, Califf RM, Inrig JK, Patel UD, Singh AK. A secondary analysis of the CHOIR trial shows that comorbid conditions differentially affect outcomes during anemia treatment. Kidney Int. 2010;77:239–46.
Tsubakihara Y, Akizawa T, et al. High Hemoglobin Levels Maintained by an Erythropoiesis-stimulating Agent Improve Renal Survival in Patients with Severe Renal Impairment. Ther Dial Aphe. 2015 (in press).
Solomon SD, Uno H, Lewis EF, Eckardt KU, Lin J, Burdmann EA, De Zeeuw D, Ivanovich P, Levey AS, Parfrey P, Remuzzi G, Singh AK, Toto R, Huang F, Rossert J, McMurray JJ, Pfeffer MA, Trial to Reduce Cardiovascular Events with Aranesp Therapy (TREAT) Investigators. Erythropoietic response and outcomes in kidney disease and type 2 diabetes. N Engl J Med. 2010;363:1146–55.
Imai E, Yamamoto R, Suzuki H, Watanabe T. Incidence of symptomatic stroke and cancer in chronic kidney disease patients treated with epoetins. Clin Exp Nephrol. 2010;14:445–52.
Conflict of interest
Employment/Leadership position/Advisory role: Tadao Akizawa (Kyowa Hakko Kirin, Japan Tabaco, Astellas, Nipro), Consultancies: Masaomi Nangaku (Kyowa Hakko Kirin, Chugai), Manuscript fee: Tadao Akizawa (Kyowa Hakko Kirin, Astellas), Honoraria: Enyu Imai (Daiichi Sankyo, Dainippon Sumitomo, Kyowa Hakko Kirin, Chugai, MSD, Sanwa Kagaku), Terumasa Hayashi (Kyowa Hakko Kirin, Chugai), Masaomi Nangaku (Kyowa Hakko Kirin, Chugai), Hideki Hirakata (Chugai, Kyowa Hakko Kirin, Japan Tabaco, Bayer, Torii, Astellas), Ichiei Narita (Mochida, Novartis, Daiichi Sankyo, MSD, Mitsubishi Tanabe), Yoshihara Tsubakihara (Chugai, Kyowa Hakko Kirin, Mitsubishi Tanabe), Tadao Akizawa (Chugai, Bayer, Kyowa Hakko Kirin). Grants received: Shoichi Maruyama (Kyowa Hakko Kirin, Otsuka, Dainippon Sumitomo, Mochida), Masaomi Nangaku (Kyowa Hakko Kirin, Chugai), Ichiei Narita (KUREHA, Chugai, Astellas, Kyowa Hakko Kirin, Genzyme Japan, Daiichi Sankyo, Takeda). Endowed departments by commercial entities; Yoshiharu Tsubakihara (Chugai, Baxter).
Author information
Authors and Affiliations
Corresponding author
About this article
Cite this article
Imai, E., Maruyama, S., Nangaku, M. et al. Rationale and study design of a randomized controlled trial to assess the effects of maintaining hemoglobin levels using darbepoetin alfa on prevention of development of end-stage kidney disease in non-diabetic CKD patients (PREDICT Trial). Clin Exp Nephrol 20, 71–76 (2016). https://doi.org/10.1007/s10157-015-1133-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10157-015-1133-z