Abstract
Background
The primary cause of death of hemodialysis (HD) patients is cardiovascular disease, and increased oxidative stress has been proposed to be involved in the disease pathogenesis. In this study, we examined the effect of olmesartan on oxidative stress induced by angiotensin II, lipopolysaccharide, indoxyl sulfate, advanced oxidation protein products (AOPP) or hydrogen peroxide (H2O2), which are known to be present at higher concentrations in the blood of HD patients, using human umbilical vein endothelial cells (HUVECs).
Methods
Oxidative stress was evaluated by measuring the mean fluorescence intensity of CM-H2DCFCA, an ROS-sensitive fluorescent dye, in HUVECs. HUVECs were incubated with each of the above compounds in the presence or absence of olmesartan. Moreover, these oxidant-stimulated cells were also treated with the reactive oxygen species (ROS) inhibitor N-acetyl-cysteine (NAC), NADPH oxidase inhibitor diphenylene iodonium (DPI) or PKC inhibitor calphostin C. In addition, we investigated the effects of olmesartan on cytotoxicity and vascular endothelial growth factor (VEGF) secretion, which is involved in vascular inflammation in HUVECs induced by AOPP or H2O2.
Results
The treatment of these oxidant-stimulated cells with olmesartan resulted in a significant reduction in intracellular ROS production to an extent that was nearly equivalent to that of NAC, DPI or calphostin C. Furthermore, olmesartan reduced the cytotoxicity and VEGF secretion induced by AOPP or H2O2.
Conclusions
These results demonstrated that the antioxidant activity of olmesartan might contribute to both its vasculoprotective and anti-hypertensive effects.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Angiotensin II (AII) type 1 receptor blockers (ARBs) inhibit the renin–angiotensin system (RAS) and have been shown to be effective for the treatment of hypertension. Independent of their ability to reduce blood pressure (BP), these compounds have also been reported to reduce the progression of nephropathy in patients suffering from diabetes mellitus (DM) and chronic renal failure (CRF) [1, 2]. In addition, these compounds have been shown to play a promising role in reducing the risk of cardiovascular disease (CVD) in these high-risk patients [3]. Although much of the tissue-specific protective effects of ARBs are due to BP reduction, some protection might be due to their antioxidant potential, resulting in reduced oxidative stress. Indeed, Miyata et al. reported that olmesartan, a recently developed ARB, displayed stronger antioxidant effects compared to any other ARB examined in an in vitro study [4, 5]. Moreover, in an in vivo study, olmesartan decreased serum total free radical levels in hemodialysis (HD) patients [6]. We also revealed that the clinical concentration of olmesartan exerts antioxidant properties not only in a clinical trial of HD patients but also in an in vitro study [7]. Furthermore, we demonstrated that the antioxidant property of olmesartan might be related to a renoprotective rather than an antihypertensive effect [8]. Recently, this accumulated evidence has indicated that the management of oxidative stress using olmesartan, which alleviates the production of excessive levels of reactive oxygen species (ROS), results in protective effects of the heart or kidney in CRF patients, particularly HD patients.
AII is the primary effector peptide of the RAS via AII type-1 (AT1) receptor-mediated stimulation of NADPH oxidase and enhancement of ROS production, which in turn contribute to endothelial dysfunction and vascular inflammation [9]. The combination of hypertension and oxidative stress, which are induced by the stimulation of RAS, results in the accelerated progression of atherosclerosis in HD patients [10]. Moreover, blockade of the AT1 receptor in hypertensive patients has been shown to reduce oxidative stress, inflammation and endothelial dysfunction [11]. Thus, olmesartan also appears to exert antioxidant effects and endothelial cell protection via blockade of the AT1 receptor. In addition to AII, there are several risk factors that promote oxidative stress in HD patients, such as the interaction between the dialysis membrane and blood, the infiltration of lipopolysaccharide (LPS) in the dialysate [12], and the accumulation of uremic toxins, such as indoxyl sulfate (IS) and advanced oxidation protein products (AOPP). However, thus far, there has been little examination of the effects of olmesartan on oxidative stress induced by ROS production in endothelial cells under CRF conditions.
Thus, the aim of this study is to examine whether olmesartan inhibits oxidative stress and consequently protects against cell injury in endothelial cells induced by five typical ROS inducers using HUVECs as a model of HD.
Materials and methods
Reagents
Olmesartan was obtained from Daiichi-Sankyo Pharmaceutical (Tokyo, Japan). N-acetylcysteine (NAC) was obtained from Sigma Chemical, Inc. (St. Louis, MO, USA). 5-(and-6)-chloromethyl-2′, 7′-dichlorodihydrofluorescein diacetate (CM-H2DCFDA) was purchased from Molecular Probes (Leiden, Netherlands). HUVECs were purchased from Dainippon Sumitomo Pharma Co., Ltd. (Osaka, Japan). All chemicals were of analytical grade.
Cell culture and treatment conditions
Among endothelial cells, HUVECs are frequently used to study the mechanisms of oxidative stress-induced alterations in endothelial cell function. Thus, we used HUVECs in the present study as a model of human endothelial cells. HUVECs were cultured as previously described [13] and used for experimentation at passages between 3 and 5.
Measurements of ROS in HUVECs
To investigate the effect of several concentrations of ROS inducers, such as AII, LPS, IS, AOPP and hydrogen peroxide (H2O2), on the generation of ROS in HUVECs, we measured the fluorescence intensities of CM-H2DCFDA, which was used as an ROS probe. HUVECs (104 cells/well) were pre-incubated in 96-well plates for 24 h at 37 °C in culture medium. Confluent HUVECs were then incubated in 10 µM CM-H2DCFDA in serum-free medium for 30 min at 37 °C. After the removal of the media from the wells, one of the several compounds in serum-free medium at 37 °C with or without olmesartan or an ROS inhibitor, such as diphenylene iodonium (DPI) or calphostin C, was added to the cells. The degree of fluorescence, which corresponded to intracellular ROS, was determined using a fluorescence microplate reader (CORONA Multi Microplate Reader) equipped with 490 nm excitation and 530 nm emission filters. The mean fluorescence intensity (MFI) ratio is presented as the percentage of the control value after subtraction of the background fluorescence.
Cytotoxicity assays
The time course of cytotoxicity induced by AOPP or H2O2 with or without olmesartan in HUVECs was determined after 0, 6 and 24 h post-treatment in 60-mm culture plates using the Trypan blue dye exclusion assay and Cell Counting Kit-8 assay.
VEGF secretion measurements
VEGF secretion induced by H2O2 or AOPP in HUVECs with or without olmesartan was determined using commercially available enzyme-linked immunosorbent assay kits (Biosource International, Camarillo, CA, USA).
Statistics
Statistical significance was evaluated using two-tailed, unpaired Student’s t tests for comparisons between two means or ANOVA analysis followed by the Tukey–Kramer method for multiple comparisons. These results are expressed as the mean ± SD.
Results
Effect of olmesartan pre-treatment on several oxidants in HUVECs
First, we examined the effect of olmesartan on the oxidative stress induced by angiotensin II (AII), lipopolysaccharide (LPS), indoxyl sulfate (IS), advanced oxidation protein products (AOPP) or hydrogen peroxide (H2O2), which are known to be present at higher concentrations in blood from HD patients. Incubation of HUVECs in each of the above compounds resulted in a significant increase in ROS production (Fig. 1a). In particular, AOPP exerted the highest level of ROS production. Moreover, treatment of these oxidant-stimulated cells with olmesartan resulted in a significant reduction in intracellular ROS production to an extent that was nearly equivalent to that of treatment with the ROS inhibitor NAC (Fig. 1b). The AOPP induced ROS production plateaued by 3 h in HUVECs treated with olmesartan (Fig. 2a). We found that olmesartan exhibited antioxidant effects against IS-induced ROS production in a dose-dependent manner at concentrations of 1–50 μmol/L, including its clinical concentration (Fig. 2b). Similar phenomena were also observed using other stimulants.
Production of ROS induced by various stimulants (a) and inhibition of ROS production using various inhibitors (b). NAC (1 mM) and olmesartan (1 μM) were added 10 min prior to the addition of various stimulants. The values are expressed as the mean ± SD (n = 8). *P < 0.05 compared to control treatment (a) or treatment with the stimulant alone (b)
Mechanism of olmesartan protection via the protein kinase C (PKC) pathway and NADPH oxidase
Recent studies have demonstrated that endothelial cells, such as HUVECs, can produce ROS via PKC and NADPH oxidase [14]. To clarify the ROS production pathway induced by these five stimulants, the effects of inhibitors of PKC and NADPH oxidase, as well as olmesartan, on oxidative stress were examined. These results revealed that incubation of diphenylene iodonium (DPI) or calphostin C in these oxidant-stimulated cells resulted in a significant reduction in intracellular ROS production. Interestingly, the extent of ROS reduction by these inhibitors was nearly equivalent to that of treatment with olmesartan (Fig. 3). These results suggest that all the substances examined in this study may produce ROS via PKC pathway-mediated NADPH oxidase activation and that the antioxidant effect of olmesartan may involve inhibition of NADPH oxidase and the PKC pathway.
Effect of NADPH oxidase and PKC inhibitors on intracellular ROS induced by various stimulants for 3 h in HUVECs. Olmesartan (1 μM), NAC (1 mM), DPI (10 mM) or calphostin C (10 nM) was added 10 min prior to the addition of various stimulants. The values are expressed as the mean ± SD (n = 8). *P < 0.05 compared to treatment with the stimulant alone
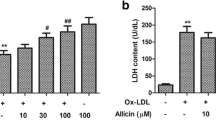
Effect of olmesartan pre-treatment on AOPP- and H2O2-induced cytotoxicity in HUVECs
We found that various stimulants increase ROS production in HUVECs and that this effect was alleviated by olmesartan. Thus, we next investigated whether the high levels of ROS stimulated by AOPP or H2O2 could induce cytotoxicity and whether olmesartan could exert a protective effect on this cytotoxicity in HUVECs. These results revealed that both AOPP and H2O2 induced cytotoxicity in HUVECs and that olmesartan displayed a protective effect against this cytotoxicity in a time-dependent manner (Fig. 4). The finding that ROS production in HUVECs incubated in AOPP plateaued by 3 h suggests that ROS production may be accelerated preceding cellular injury (Fig. 2a). These results suggest that AOPP-induced cellular damage to HUVECs may be due to ROS production via PKC pathway-mediated activation of NADPH oxidase and that the antioxidant effect of olmesartan may involve inhibition of NADPH oxidase and the PKC pathway, resulting in the suppression of cellular damage.
Cytotoxicity induced by H2O2 or AOPP in HUVECs. a Time course of cytotoxicity induced by H2O2 (100 μM) in HUVECs with (filled square) or without (filled triangle) olmesartan treatment. b Time course of cytotoxicity induced by AOPP (1 mg/mL) in HUVECs with (filled square) or without (filled triangle) olmesartan treatment. Olmesartan (1 μM) was added 10 min prior to the addition of AOPP or H2O2. The values are expressed as the mean ± SD (n = 8). *P < 0.05 compared to control treatment
Effect of olmesartan pre-treatment on VEGF secretion in HUVECs
Because VEGF is a proinflammatory factor [15–17], we next examined the effect of olmesartan on VEGF secretion induced by AOPP or H2O2. These results revealed that both AOPP and H2O2 induced VEGF secretion in HUVECs, while treatment with olmesartan for 3 h decreased this stimulant-induced VEGF secretion (Fig. 5).
Discussion
Previously, we demonstrated for the first time that olmesartan at its clinical dose displayed antioxidant activity in HD patients [7]. Because oxidative stress is significantly associated with the progression of renal failure and the development of complications, such as CVD, an antioxidant effect of olmesartan beyond its reduction of BP could be involved in its ability to protect organ function in CRF patients. However, the effects of olmesartan on ROS-induced oxidative stress in endothelial cells have not been extensively examined with respect to organ protection. In this study, we used HUVECs to examine the effect of olmesartan on oxidative stress induced by several stimulants that are known to be present at higher concentrations in blood from HD patients.
In our previous studies, we showed the antioxidant activity of olmesartan in vivo, but this activity had a direct and indirect antioxidant activity, such as modulation via NADPH oxidase activity [7, 8]. Various factors, except for these effects, may be concerned with the complicated antioxidant activity of olmesartan. Since it has been reported that blockade of AT1 receptor leads to the enhancement of the activity of AT2 receptor or ACE2 [18, 19], similar beneficial effects would be also expected by olmesartan under uremic conditions. Further study will be necessary to clarify whether these stimulations are involved in the antioxidant and cytoprotective effects of olmesartan as observed in this study. We recently also demonstrated that other angiotensin II type 1 receptor blockers, including telmisartan, effectively reduced the extent of blood pressure and reduced oxidative stress and were safe and well tolerated by HD patients [20]. Interestingly, the reduction of oxidative stress of olmesartan was slightly higher compared to telmisartan. This effect might be due to its structure and strong binding to AT1 receptor. Finally, this observation also supports the antioxidant potential of olmesartan via the AT1 receptor.
Typically, AII stimulates NADPH oxidase via the AT1 receptor and enhances ROS production in HD patients. Moreover, ROS production induced by AT1 receptor stimulation promotes not only blood vessel contraction, multiplication, hypertrophy and migration of vascular smooth muscle but also inflammation in the blood vessel wall, such as promotion of the expression of pro-inflammatory factors in vascular smooth muscle cells [21, 22]. However, because various factors, except for AII, are associated with an increase in oxidative stress in HD patients, it was necessary to examine the effect of olmesartan on oxidative stress induced by various stimulants. As shown in Fig. 1a, incubation of HUVECs in each stimulant resulted in a significant increase in ROS production in a dose-dependent manner. Under these conditions, olmesartan significantly suppressed ROS production induced by each stimulant (Fig. 1b). Stimulants such as LPS, IS, AOPP and H2O2 might activate the AT1 receptor in several cells. For example, upregulation of the AT1 receptor promotes inflammation and LOX-1 expression-related ROS induction by LPS in cultured cardiomyocytes [23]. High pressure, likely via the induction of H2O2 production, increases the functional availability of AT1 receptors and thus enhances Ang II-induced arteriolar constrictions in skeletal muscle arteries [24]. AOPPs also resulted in a significant increase in the expression of AT1 receptors in PTCs [25]. Furthermore, IS significantly increased AT1 receptor protein expression in mouse proximal renal tubular cells in culture [26]. Thus, the induction of the AT1 receptor by these stimulants might be very important in the elucidation of the mechanism of ROS inhibition by olmesartan.
A component of the signaling pathway of the AT1 receptor to NADPH oxidase has been suggested to involve the PKC pathway [27]. Next, we examined the effect of the NADPH oxidase inhibitor and PKC inhibitor on ROS production induced by various stimulants. The production of ROS was blocked by these inhibitors (Fig. 3). Currently, it is unknown whether the stimulants used in this study, except for Ag II, act on the AT1 receptor. Thus, the effects of the inhibitors examined in this study appear to involve NADPH oxidase via the PKC pathway in the absence of binding to the AT1 receptor. Moreover, the effects of these inhibitors were nearly equivalent to those of olmesartan. These results suggest that all the stimulants examined in this study may induce ROS production via PKC pathway-mediated NADPH oxidase activation. Thus, the antioxidant effect of olmesartan against these stimulants might involve direct or indirect inhibition of NADPH oxidase and the PKC pathway via the AT1 receptor. Currently, the antioxidant activity of ARBs is based on the former pathway, while the latter pathway appears to account for the antioxidant activity of olmesartan. Recently, the expression of RAGE, a scavenger receptor, was enhanced by stimulation of the AT1 receptor and was decreased by the binding of telmesartan, another ARB, to the AT1 receptor [28]. Because CD36 has been suggested to be involved in the endocytosis of AOPP in endothelial cells [29, 30], olmesartan appears to indirectly block the endocytosis of AOPP via activation of NADPH oxidase and the PKC pathway via the AT1 receptor [31, 32]. However, determining the mechanism by which these compounds alter ROS production will require further in vitro and in vivo studies. Moreover, to determine the precise mechanism of the anti-oxidative property of olmesartan, further in vitro or in vivo experiments using knockdown or knockout techniques against NADPH oxidase or PKC are needed.
As previously mentioned above, ROS production increased in HUVECs treated with various stimulants, and these activities were inhibited by olmesartan. It is important to clearly demonstrate the manner in which increased ROS production affected endothelial cells injury to clarify the olmesartan-induced activities of organ protection and CVD pathogenesis prevention in HD patients. Thus, we investigated whether high levels of ROS induced by AOPP or H2O2 could induce cytotoxicity and whether olmesartan could protect against this cytotoxicity in HUVECs. These results revealed that both AOPP and H2O2 induced cytotoxicity in HUVECs and that olmesartan displayed a protective effect against this cytotoxicity (Fig. 4). Although several investigators reported that olmesartan-induced organ protection alleviates the production of inflammatory cytokines by renal proximal tubule epithelial cells and vascular smooth muscle cells [33, 34], no studies have examined the injury effects to endothelial cells, such as HUVECs. Moreover, because activation of NADPH oxidase via the PKC pathway was also related to AOPP-induced ROS production in HUVECs, AOPP-induced endothelial cell injury appears to involve the same pathway via activation of NADPH oxidase. Furthermore, the increase in ROS production reached a plateau by 3 h, and because this plateau occurred at an early time point rather than upon the appearance of cellular injury (Fig. 2a), it is possible that ROS production served as the trigger to induce cell damage. Thus, olmesartan is proposed to protect the vascular endothelium via the regulation of ROS production. Furthermore, olmesartan reduced VEGF secretion-induced vascular inflammation within 3 h (Fig. 5). VEGF generally acts as a proinflammatory cytokine by increasing endothelial permeability and inducing adhesion molecules that bind leukocytes to endothelial cells [21]. These results also suggested that olmesartan-induced inhibition of VEGF secretion from HUVECs might result in decreased vascular inflammation via oxidative stress.
In conclusion, the present findings demonstrated that the antioxidant effect of olmesartan was markedly related to its vascular protective effect rather than its antihypertensive effect. Currently, the number of HD patients exceeds 250,000 individuals, and for half of these patients, the cause of death is CVD. These results suggest a mechanism underlying the prevention of CVD and the foundation of a new treatment strategy for HD patients using olmesartan, which displayed antioxidant activity beyond its reduction in BP.
References
Lewis EJ, Hunsicker LG, Clarke WR, Berl T, Pohl MA, Lewis JB, et al. Renoprotective effect of the angiotensin-receptor antagonist irbesartan in patients with nephropathy due to type 2 diabetes. N Engl J Med. 2001;345(12):851–60.
Haller H, Viberti GC, Mimran A, Remuzzi G, Rabelink AJ, Ritz E, et al. Preventing microalbuminuria in patients with diabetes: rationale and design of the Randomised Olmesartan and Diabetes Microalbuminuria Prevention (ROADMAP) study. J Hypertens. 2006;24(2):403–8.
Akhrass PR, McFarlane SI. Telmisartan and cardioprotection. Vasc Health Risk Manag. 2011;7:677–83.
Miyata T, van Ypersele de Strihou C, Ueda Y, Ichimori K, Inagi R, Onogi H, et al. Angiotensin II receptor antagonists and angiotensin-converting enzyme inhibitors lower in vitro the formation of advanced glycation end products: biochemical mechanisms. J Am Soc Nephrol. 2002;13(10):2478–87.
Nangaku M, Miyata T, Sada T, Mizuno M, Inagi R, Ueda Y, et al. Anti-hypertensive agents inhibit in vivo the formation of advanced glycation end products and improve renal damage in a type 2 diabetic nephropathy rat model. J Am Soc Nephrol. 2003;14(5):1212–22.
Honda H, Hosaka N, Aoshima Y, Hirai Y, Michihata T, Akizawa T. Olmesartan medoxomil is associated with decreased plasma AGEs, pentosidine, and N-(epsilon)-carboxymethyl-lysine levels in hemodialysis patients. Clin Exp Hypertens. 2012;34(1):17–23.
Kadowaki D, Anraku M, Tasaki Y, Kitamura K, Wakamatsu S, Tomita K, et al. Effect of olmesartan on oxidative stress in hemodialysis patients. Hypertens Res. 2007;30(5):395–402.
Kadowaki D, Anraku M, Tasaki Y, Taguchi K, Shimoishi K, Seo H, et al. Evaluation for antioxidant and renoprotective activity of olmesartan using nephrectomy rats. Biol Pharm Bull. 2009;32(12):2041–5.
Griendling KK, Minieri CA, Ollerenshaw JD, Alexander RW. Angiotensin II stimulates NADH and NADPH oxidase activity in cultured vascular smooth muscle cells. Circ Res. 1994;74(6):1141–8.
Weiss D, Kools JJ, Taylor WR. Angiotensin II-induced hypertension accelerates the development of atherosclerosis in apoE-deficient mice. Circulation. 2001;103(3):448–54.
Koh KK, Ahn JY, Han SH, Kim DS, Jin DK, Kim HS, et al. Pleiotropic effects of angiotensin II receptor blocker in hypertensive patients. J Am Coll Cardiol. 2003;42(5):905–10.
Nockher WA, Scherberich JE. Monocyte cell-surface CD14 expression and soluble CD14 antigen in hemodialysis: evidence for chronic exposure to LPS. Kidney Int. 1995;48(5):1469–76.
Li H, Forstermann U. Structure-activity relationship of staurosporine analogs in regulating expression of endothelial nitric-oxide synthase gene. Mol Pharmacol. 2000;57(3):427–35.
Heitzer T, Wenzel U, Hink U, Krollner D, Skatchkov M, Stahl RA, et al. Increased NAD(P)H oxidase-mediated superoxide production in renovascular hypertension: evidence for an involvement of protein kinase C. Kidney Int. 1999;55(1):252–60.
Folkman J. Angiogenesis in cancer, vascular, rheumatoid and other disease. Nat Med. 1995;1(1):27–31.
Marumo T, Schini-Kerth VB, Busse R. Vascular endothelial growth factor activates nuclear factor-kappaB and induces monocyte chemoattractant protein-1 in bovine retinal endothelial cells. Diabetes. 1999;48(5):1131–7.
Ferrara N. Role of vascular endothelial growth factor in the regulation of angiogenesis. Kidney Int. 1999;56(3):794–814.
Iwai M, Chen R, Li Z, Shiuchi T, Suzuki J, Ide A, et al. Deletion of angiotensin II type 2 receptor exaggerated atherosclerosis in apolipoprotein E-null mice. Circulation. 2005;112(11):1636–43.
Ohshima K, Mogi M, Nakaoka H, Iwanami J, Min LJ, Kanno H, et al. Possible role of angiotensin-converting enzyme 2 and activation of angiotensin II type 2 receptor by angiotensin-(1-7) in improvement of vascular remodeling by angiotensin II type 1 receptor blockade. Hypertension. 2014;63(3):e53–9.
Shimada H, Kitamura K, Anraku M, Miyoshi T, Adachi M, Tuyen DG, et al. Effect of telmisartan on ambulatory blood pressure monitoring, plasma brain natriuretic peptide, and oxidative status of serum albumin in hemodialysis patients. Hypertens Res. 2005;28(12):987–94.
Kim I, Moon SO, Kim SH, Kim HJ, Koh YS, Koh GY. Vascular endothelial growth factor expression of intercellular adhesion molecule 1 (ICAM-1), vascular cell adhesion molecule 1 (VCAM-1), and E-selectin through nuclear factor-kappa B activation in endothelial cells. J Biol Chem. 2001;276(10):7614–20.
Jinno T, Iwai M, Li Z, Li JM, Liu HW, Cui TX, et al. Calcium channel blocker azelnidipine enhances vascular protective effects of AT1 receptor blocker olmesartan. Hypertension. 2004;43(2):263–9.
Wang X, Khaidakov M, Ding Z, Mitra S, Lu J, Liu S, et al. Cross-talk between inflammation and angiotensin II: studies based on direct transfection of cardiomyocytes with AT1R and AT2R cDNA. Exp Biol Med (Maywood). 2012;237(12):1394–401.
Bagi Z, Erdei N, Koller A. High intraluminal pressure via H2O2 upregulates arteriolar constrictions to angiotensin II by increasing the functional availability of AT1 receptors. Am J Physiol Heart Circ Physiol. 2008;295(2):H835–41.
Cao W, Xu J, Zhou ZM, Wang GB, Hou FF, Nie J. Advanced oxidation protein products activate intrarenal renin-angiotensin system via a CD36-mediated, redox-dependent pathway. Antioxid Redox Signal. 2013;18(1):19–35.
Sun CY, Chang SC, Wu MS. Uremic toxins induce kidney fibrosis by activating intrarenal renin-angiotensin-aldosterone system associated epithelial-to-mesenchymal transition. PLoS One. 2012;7(3):e34026.
Ross R. Atherosclerosis is an inflammatory disease. Am Heart J. 1999;138(5 Pt 2):S419–20.
Yoshida T, Yamagishi S, Nakamura K, Matsui T, Imaizumi T, Takeuchi M, et al. Telmisartan inhibits AGE-induced C-reactive protein production through downregulation of the receptor for AGE via peroxisome proliferator-activated receptor-gamma activation. Diabetologia. 2006;49(12):3094–9.
Nakamura K, Yamagishi S, Nakamura Y, Takenaka K, Matsui T, Jinnouchi Y, et al. Telmisartan inhibits expression of a receptor for advanced glycation end products (RAGE) in angiotensin-II-exposed endothelial cells and decreases serum levels of soluble RAGE in patients with essential hypertension. Microvasc Res. 2005;70(3):137–41.
Ohgami N, Nagai R, Ikemoto M, Arai H, Kuniyasu A, Horiuchi S, et al. Cd36, a member of the class b scavenger receptor family, as a receptor for advanced glycation end products. J Biol Chem. 2001;276(5):3195–202.
Fujita M, Okuda H, Tsukamoto O, Asano Y, Hirata YL, Kim J, et al. Blockade of angiotensin II receptors reduces the expression of receptors for advanced glycation end products in human endothelial cells. Arterioscler Thromb Vasc Biol. 2006;26(10):e138–42.
Hayek T, Aviram M, Heinrich R, Sakhnini E, Keidar S. Losartan inhibits cellular uptake of oxidized LDL by monocyte-macrophages from hypercholesterolemic patients. Biochem Biophys Res Commun. 2000;273(2):417–20.
Tanifuji C, Suzuki Y, Geot WM, Horikoshi S, Sugaya T, Ruiz-Ortega M, et al. Reactive oxygen species-mediated signaling pathways in angiotensin II-induced MCP-1 expression of proximal tubular cells. Antioxid Redox Signal. 2005;7(9–10):1261–8.
Teng J, Fukuda N, Suzuki R, Takagi H, Ikeda Y, Tahira Y, et al. Inhibitory effect of a novel angiotensin II type 1 receptor antagonist RNH-6270 on growth of vascular smooth muscle cells from spontaneously hypertensive rats: different anti-proliferative effect to angiotensin-converting enzyme inhibitor. J Cardiovasc Pharmacol. 2002;39(2):161–71.
Conflict of interest
All of the authors have declared that there are no competing interests.
Author information
Authors and Affiliations
Corresponding authors
About this article
Cite this article
Kadowaki, D., Anraku, M., Sakaya, M. et al. Olmesartan protects endothelial cells against oxidative stress-mediated cellular injury. Clin Exp Nephrol 19, 1007–1014 (2015). https://doi.org/10.1007/s10157-015-1111-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10157-015-1111-5