Abstract
Background
Pozzi et al. reported the effectiveness of steroid pulse therapy (Pozzi’s regimen) in IgA nephropathy (IgAN). The present study was performed to clarify the predictive factors for IgAN patients treated with Pozzi’s regimen.
Methods
One hundred nine IgAN patients treated by Pozzi’s regimen were observed for up to 112.6 (median 39.7) months, and remission of proteinuria (PR) and disappearance of urinary abnormalities [complete remission (CR)] after Pozzi’s regimen were analyzed. Predictive factors for the glomerular filtration rate (GFR) slopes for up to 5 years were analyzed among 81 patients who were observed for at least 2 years. The outcome of a 50 % increase in sCr was compared between the CR and non-CR groups within 2 years.
Results
Cumulative PR and CR rates increased rapidly until 2 years (54.5 and 46.8 % at 2 years), and then slowly but steadily up to 6 years (72.8 and 66.4 % at 6 years). Baseline characteristics of the CR and non-CR groups within 2 years were similar except for proteinuria. GFR slope was steeper in the non-CR group than in the CR group (−2.44 ± 5.12 vs. −0.32 ± 3.34 ml/min/1.73 m2/year). On multivariate analysis, sex and CR within 2 years were associated with GFR slope. Kaplan-Meier analysis demonstrated a better survival rate in CR group patients without a 50 % increase in sCr (p = 0.024).
Conclusions
Among IgAN patients treated with Pozzi’s regimen, CR within 2 years predicts a good prognosis.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Immunoglobulin A nephropathy (IgAN) is one of the most common causes of glomerulonephritis worldwide, and its prevalence is reported to be higher in the Pacific Rim and Mediterranean areas [1–3]. The pathogenesis of IgAN is still a matter of debate [4, 5]. In Japan, IgAN accounts for around 30 to 40 % of all cases of primary glomerulonephritis [6]. Although IgAN was originally reported as a rather stable type of renal disease [1], its prognosis turned out to be poor, and approximately 40 % of patients ultimately developed end-stage renal disease (ESRD) within 20 years [6, 7]. Thus, IgAN patients are treated by various immunosuppressive therapy regimens when the prognosis is expected to be worse [7–10].
Kobayashi et al. [11] first reported the long-term effect (10 years) of oral corticosteroid therapy for moderate IgAN patients in a case control study. The clinical value of methylprednisolone (mPSL) pulse therapy was demonstrated by Pozzi et al. [12, 13] in a randomized, controlled trial (RCT). However, even with Pozzi’s regimen, renal function continues to decline in some IgAN patients. Locateli et al. showed that the renal survival rate without a 33 % reduction in estimated creatinine clearance (CCr) using the Cockroft and Gault formula [14] decreased as the follow-up period extended [15]. Another RCT with Pozzi’s regimen showed renal survival without a 50 % increase in sCr was 89 % at 5 years and 84 % at 7 years [16]. Thus, a prognostic factor is desired to predict renal outcome after treatment.
In clinical research, systolic hypertension, massive proteinuria, renal impairment, and severe histological findings on renal biopsy have been reported as risk factors for ESRD [8]. In addition, inappropriate lifestyles, including high-salt and high-protein diets, are also associated with ESRD [9]. Of these, proteinuria is one of the best predictive risk factors for ESRD. Reich et al. [17] reported the association of time average proteinuria (TAP) with renal survival in IgAN in a retrospective cohort. However, only a small number of patients received immunosuppressive therapy in this study, and with TAP it seems to be difficult to predict outcome in the early phase after treatment.
Among IgA nephropathy patients treated with Pozzi’s regimen, steroid treatment, histological score, proteinuria reduction at 6 months, and no increase in proteinuria were significantly associated with renal survival. Although proteinuria reduction at 6 months might be useful as a predictive marker, it is often seen that the urinary abnormality gradually improved even after 6 months. Therefore, a further study to predict prognosis in patients treated with Pozzi’s regimen is needed.
The clinical significance of hematuria has recently been highlighted. In a young general population, isolated microscopic hematuria has been reported to be a risk factor for ESRD [18]. In IgA nephropathy patients with minimal [19] or normal range proteinuria [20], microscopic hematuria was a significant risk factor for subsequent proteinuria, hypertension, or renal insufficiency. Hotta et al. [21] also showed that IgAN patients who achieved a disappearance of hematuria and proteinuria, complete remission (CR), had excellent renal outcomes in their retrospective cohort. However, there is no report showing the change in hematuria after Pozzi’s regimen, nor its clinical utility as a prognostic factor.
The present study was performed to study the effectiveness of Pozzi’s regimen, focusing on changes in urinary abnormalities, and to clarify the associations among various clinical parameters, including CR, and renal outcome in our retrospective cohort of IgAN patients.
Materials and methods
Diagnosis and histological grade of IgAN
The diagnosis of IgAN was made by detection of mesangial deposits staining predominantly for IgA on immunofluorescence studies in patients without evidence of systemic lupus erythematosus, Henoch-Schönlein purpura or chronic liver cirrhosis. The histologic lesions of all IgAN patients were assessed according to the guidelines presented by the Special Study Group (IgAN) on Progressive Glomerular Disease in Japan [22, 23]. Glomerular findings and interstitial and vascular findings were scored from grade 1 to 4. In case of grade disagreement, the worst grade was selected. Histological grade was diagnosed by three independent renal biopsy specialists.
Study population
The participants were 109 biopsy-proven IgAN patients in Nagoya University Hospital (n = 58), Tosei General Hospital (n = 28) and Kasugai Municipal Hospital (n = 23). Between January 2001 and December 2009, 957 renal biopsies were performed in three collaborative centers, and 251 patients were diagnosed as having IgAN. Patients who were treated by conservative therapy (118 patients), by tonsillectomy alone (6 patients) or by another immunosuppressive therapy regimen (18 patients) were excluded from the study. Therefore, 109 patients were eligible (Fig. 1). A retrospective cohort study was carried out to validate the renal outcome and identify prognostic predictors. The study protocol was approved by the ethics committees of Nagoya University Hospital and affiliated hospitals.
Treatment protocol
All patients were treated by Pozzi’s regimen, consisting of 3 consecutive days of mPSL pulse therapy, three times at 2-month intervals, in combination with oral corticosteroid of 0.5 mg/kg BW/day on alternate days for 6 months [12, 13]. Almost all patients received intravenous mPSL pulses of 1 g/day, but 20 patients in Kasugai Municipal Hospital received pulses of 0.5 g/day. Tonsillectomy was performed in 54 patients (49.5 %).
Data collection and analysis
The clinical data collected just before the initiation of Pozzi’s regimen were defined as the baseline parameters. Hypertension was defined as systolic blood pressure (BP) ≥ 140 mmHg and/or diastolic BP ≥ 90 mmHg, or the use of antihypertensive medication. Urinary parameters were evaluated at every outpatient clinic visit until remission of proteinuria and hematuria. The sCr level was measured enzymatically, and the data were collected from the medical records just before and 2, 4 and 6 months after Pozzi’s regimen, and then every 6 months until the end of 2010. Estimated GFR (eGFR) was calculated using the Japanese eGFR equation based on age, sex and sCr [24]. Patients were categorized into the tonsillectomy group if they had undergone the procedure by the end of 2010. Protein reduction at 6 months was evaluated by proteinuria (g/gCr) in a spot urine at the beginning of and after 6 months of Pozzi’s regimen.
Study designs
Of the 109 participants treated by Pozzi’s regimen, cumulative remission rates of proteinuria (PR) and disappearance of urinary abnormalities (CR) were analyzed over time after treatment. PR was defined as urinary protein less than 0.2 g/gCr on two consecutive outpatient clinic urinalyses, and CR was defined as both urinary protein less than 0.2 g/gCr and urinary erythrocytes less than 5/high power field in fresh urinary sediment on two consecutive urinalyses.
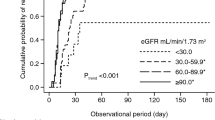
Subsequently, of the 81 patients whose observation period was longer than 2 years, the eGFR slope was calculated by the linear least squares method from eGFR plots during observation periods of up to 5 years and expressed as ml/min/1.73 m2/year [17, 25, 26]. Factors associated with eGFR slope were studied by univariate and multivariate linear regression analyses. The Kaplan-Meier analysis for a 50 % increase in sCr was conducted in the CR and the non-CR groups within 2 years. The correlation between baseline proteinuria and proteinuria reduction at 6 months was analyzed.
Statistical methods
The duration of the observation period is shown as the median with the minimum and maximum range, and all other continuous variables are summarized as means ± standard deviation. Categorical variables are expressed as numbers and proportions. The cumulative remission rates in the PR group and the CR group were estimated using the Kaplan-Meier method. Clinical variables were compared using the unpaired t test, the Mann-Whitney U test, the chi-square test or Fisher’s exact test. The univariate analysis for GFR slope was conducted using the linear regression method with Pearson’s correlation coefficients or Spearman’s rank correlation coefficients. The multiple linear regression analysis was also carried out for the GFR slope. A p value of less than 0.05 was considered significant. All statistical evaluations were performed with IBM SPSS Statistics ver. 19 (Chicago, IL, USA).
Results
Improvement in urinalysis after Pozzi’s regimen of 109 IgAN patients
Table 1 shows the baseline characteristics of all 109 IgAN patients. The mean duration of follow-up was 39.7 (7.8–112.6) months. Before starting Pozzi’s regimen, urinary protein was 1.61 ± 1.46 g/day, and the serum creatinine level was 0.91 ± 0.35 mg/dl. In the present study, sCr was measured using the enzymatic method. The enzymatic method is more accurate, but reports approximately 0.2 mg/dl lower values than those obtained by the Jaffe-kinetic method without offset due to non-creatinine chromogens [27].
The Kaplan-Meier analysis (Fig. 2) showed that the cumulative remission rates increased rapidly until 2 years (53.2 % for PR and 45.0 % for CR) and then slowly up to 6 years (61.5 % for PR and 54.1 % for CR). In Kasugai Municipal Hospital, 20 patients were treated by mPSL pulse therapy at a daily dosage of 0.5 g, but remission rates in the three centers did not show any significant differences (data not shown).
In our study, some outliers compared to Pozzi’s report were included. Of the ten patients with sCr values greater than 1.3 mg/dl using the enzymatic method, those who met the exclusion criteria of sCr values above 1.5 mg/dl using the Jaffe method, 6 (60 %) achieved CR with Pozzi’s regimen. Of the seven patients with proteinuria greater than 3.5 g/day, 4 (57.1 %) achieved CR as well. Regarding adverse events associated with Pozzi’s regimen, only one patient was diagnosed with asymptomatic aseptic necrosis of the femoral head on magnetic resonance imaging (MRI) and required no specific treatment.
Predictive factors of eGFR slope among 81 IgAN patients
Since Kaplan-Meier analysis clearly showed different increases in the rates of cumulative remissions before and after 2 years, 81 patients with a follow-up period of more than 2 years were analyzed in association with the GFR slope.
Of the 81 patients, 35 achieved CR within 2 years. The baseline characteristics of the CR and non-CR groups within 2 years are shown in Table 2. Only proteinuria was significantly lower in the CR group than in the non-CR group (1.69 ± 2.02 g/day vs. 1.83 ± 1.21 g/day, p = 0.009). However, protein reduction at 6 months was not different between the CR and non-CR groups. The GFR slope was steeper in the non-CR group than in the CR group (−2.44 ± 5.12 vs. −0.32 ± 3.34 ml/min/1.73 m2/year), but the difference was not significant (p = 0.067). Neither sCr nor histological grade was significantly different between the two groups. Prescriptions of angiotensin-converting enzyme inhibitor (ACE-I) and/or angiotensin receptor blocker (ARB) and tonsillectomy rates were similar in both groups. The GFR slopes were −0.49 ± 3.35 ml/min/1.73 m2/years in the PR group and −2.64 ± 5.37 ml/min/1.73 m2/years in the non-PR group (p = 0.076). Among 35 IgA nephropathy patients who achieved CR within 2 years, one patient showed proteinuria recurrence and another one hematuria recurrence. The patient with proteinuria recurrence did not get additional immune-suppressive therapy since she had no hematuria. The patient with hematuria recurrence underwent tonsillectomy and achieved CR again. The creatinine levels of these two patients remained stable throughout the following period. No patients developed a recurrence with both proteinuria and hematuria.
On univariate analysis, no parameter was significantly associated with GFR slope, and CR within 2 years showed the lowest p value of 0.067. Protein reduction at 6 months did not correlate with GFR slope (Table 3). Histological grade, tonsillectomy and hematuria remission did not correlate with GFR slope. Next, multivariate analysis was carried out using sex, age, systolic BP, CR, eGFR and histological grade. Sex and CR within 2 years were significant predictors of GFR slope (Table 4).
The clinical impact of CR was further analyzed for the renal outcome of a 50 % increase in sCr. In Kaplan-Meier analysis (Fig. 3), renal outcome was significantly better in the CR group at 2 years (p = 0.024).
Kaplan-Meier curve for renal survival between complete remission (CR) and non-CR groups. Renal survival rates without a 50 % increase in serum creatinine above baseline are shown in CR and non-CR groups. The solid line shows the survival rate of the CR group, and the dotted line shows that of the non-CR group
The clinical value of proteinuria reduction at 6 months was further analyzed in association with baseline proteinuria. There was a significant correlation between baseline proteinuria and proteinuria reduction at 6 months (Fig. 4). In 85 out of 109 patients (78 %), urinary protein excretion decreased after 6 months of therapy, while it increased in 24 patients (22 %). No difference was observed between the baseline characteristics of the two groups (data not shown), indicating that it is difficult to predict the treatment-resistance before starting the treatment.
Discussion
In this retrospective cohort of Japanese IgAN patients, it was demonstrated that CR, defined as complete disappearance of urinary abnormalities, within 2 years was an independent predictor of renal prognosis in IgAN patients. In the present study, CR was achieved in about 60 % of patients within 6 years after Pozzi’s regimen, while the original papers did not mention hematuria at all [12, 13]. To the best of our knowledge, this is the first report demonstrating the usefulness of Pozzi’s regimen to achieve CR.
In the present study, CR within 2 years and sex were independent predictors of eGFR decline on multivariate analysis, and the survival rate without a 50 % increase in sCr was significantly different between the CR and non-CR groups. Strikingly, none of the CR group patients developed the renal outcome of a 50 % increase in sCr up to 106.6 months. Moreover, the eGFR slope of the CR within the 2-year group (−0.32 ± 3.34 ml/min/1.73 m2/year) was even less than the average eGFR slope of the Japanese general population (−0.36 ml/min/1.73 m2/year) [28]. Although the eGFR slope of the CR group tended to better than that of the non-CR group (−2.44 ± 5.12 ml/min/1.73 m2/year), it was not significantly different. Hotta et al. [21] first reported the clinical significance of CR, but it has not been clear when the effectiveness of treatment should be assessed. The present study suggested that CR within 2 years would be a good prognostic marker after treatment.
Male sex was a significant risk factor for eGFR slope in IgAN patients with Pozzi’s regimen. In a nationwide, 10-year, prospective cohort of 2,238 Japanese IgAN patients, a scoring system to predict renal outcome was proposed [29], with male sex as an independent risk factor along with age, family history of ESRD or chronic glomerulonephritis, systolic BP, proteinuria, mild hematuria, hypoproteinemia, low eGFR and histology. This scoring system was also validated in a Norwegian cohort [30]. Although male sex might be a risk factor in IgAN patients, further analysis is necessary.
Pozzi et al. [13] reported that proteinuria reduction at 6 months was a predictor of better renal outcome. However, in the present study, urinary protein reduction at 6 months was not associated with the renal outcome of eGFR slope. Instead, it was significantly correlated with the amount of baseline proteinuria (Fig. 4). This discrepancy may be attributed to the difference in patient profiles, the definition of renal outcomes and the methodology to evaluate proteinuria. The utilities of proteinuria reduction at 6 months as a prognostic factor should be analyzed in a further study.
In the present study, baseline proteinuria was not significantly associated with eGFR slope. Similarly, Pozzi et al. [13] demonstrated a negative association between baseline proteinuria and renal outcome. These results contradicted most previous publications demonstrating that baseline proteinuria was a prognostic factor for renal outcome [8, 10–13, 17]. One plausible interpretation would be that mPSL pulse therapy is so effective that IgAN patients with moderate to severe proteinuria could be effectively treated. Indeed, in seven patients with massive baseline proteinuria (>3.5 g/day), CR was achieved in three (42.9 %) within 2 years, and the mean eGFR slope was −0.29 ml/min/1.73 m2/year, which was even better than the mean value of the 81 patients (−1.52 ml/min/1.73 m2/year). Thus, we could not predict the patient’s prognosis only by the amount of proteinuria before treatment.
Although it is not definitive in our study, CR seems to be a better prognostic factor than PR. On univariate analysis, CR was associated more strongly with GFR slope than PR. No CR group patients (CR within 2 years) reached the renal outcome of a 50 % or greater increase in sCr, while 1 of 42 PR group patients crossed the threshold. However, the eGFR slopes of PR and CR groups exhibited no statistical significance. The clinical significance of CR compared to PR needs further studies in larger cohorts with longer observation period.
In addition, this was the first validation study using a non-Italian cohort. Recently, Pozzi et al. [16] reported an RCT to clarify the additive effect of azathioprine. In that study, 106 IgAN patients were treated according to Pozzi’s regimen, and the primary outcome of a 50 % increase in sCr was observed in 12 patients (11.3 %) during a median follow-up of 4.9 years. On the other hand, in the present study, only eight patients (7.3 %) reached the renal outcome of a 50 % increase in sCr, including two patients who required dialysis therapy. In addition, a decrease in proteinuria was also validated. In the present study, disappearance of proteinuria or PR, which was defined as ≤ 0.2 g/gCr on two consecutive urinalyses, was observed in approximately 70 % of patients, while Pozzi et al. [12, 13] reported that 72 and 26 % of patients in the treatment group improved their proteinuria to less than 1 g/day and 0.5 g/day, respectively, after 1 year. Although this was a retrospective cohort, there were only four dropouts within 2 years, suggesting reliability in the CR and PR rates after Pozzi’s regimen. The present study shows that Pozzi’s regimen is also effective in Japanese IgAN patients.
The present study also demonstrated that Pozzi’s regimen was effective in IgAN patients even in the moderate stage. In the present cohort, 16 patients met the exclusion criteria of the original report by Pozzi et al. with a high sCr or high proteinuria levels at baseline. In ten patients, baseline sCr levels were above 1.3 mg/dl using the enzymatic method, which was identical to above 1.5 mg/dl using the Jaffe method [27]. The amount of proteinuria exceeded 3.5 g/day in seven patients before treatment, including one patient whose sCr was above 1.3 mg/dl at the same time. Even among these 16 advanced patients, 9 patients achieved CR with treatment, resulting in preserved renal function. In the present study, the baseline sCr values of two patients who required dialysis therapy were 2.83 mg/dl and 1.10 mg/dl, respectively, and the latter did not respond to mPSL therapy at all. The indications and limitations of Pozzi’s regimen should be examined in further studies.
In the present study, histological score, hypertension, and administration of ACE-I or ARB [31, 32] were not significantly associated with prognosis on univariate analysis, which was in good agreement with the previous report [13]. Furthermore, tonsillectomy showed a negative association with eGFR slope in this study. Although several reports demonstrated the additive effect of tonsillectomy combined with mPSL pulse therapy [21, 22], it still remains controversial. Xie et al. [33] showed the efficacy of tonsillectomy at 20 years but not at 10 years; thus, this should be further analyzed with a longer observation period.
There are limitations to the present study. Firstly, this was a retrospective analysis, and unknown confounding factors may have affected the result. Secondly, there was no control group without treatment. Lastly, the number of patients who reached the primary outcome was small.
In conclusion, CR, disappearance of proteinuria and hematuria within 2 years are predictors of a better prognosis among IgAN patients treated by Pozzi’s regimen.
References
Berger J, Hinglais N. Les depots intercapillaires d’IgA-IgG. J Urol Nephrol (Paris). 1968;74:694–5.
D’Amico G. The commonest glomerulonephritis in the world IgA nephropathy. Q J Med. 1987;245:709–27.
Donadio James V, Grande Joseph P. IgA nephropathy. N Engl J Med. 2002;347:738–48.
Hiki Y, Odani H, Takahashi M, Yasuda Y, Nishimoto A, Iwase H, et al. Mass spectrometry proves under-O-glycosylation of glomerular IgA1 in IgA nephropathy. Kidney Int. 2001;59:1077–85.
Yasuda Y, Horie A, Odani H, Iwase H, Hiki Y. Application of mass spectrometry to IgA nephropathy: structural and biological analyses of underglycosylated IgA1 molecules. Contrib Nephrol. 2004;141:170–88.
Koyama A, Igarashi M, Kobayashi M, Coworkers of the Research Group on Progressive Renal Diseases. Natural history and risk factors for immunoglobulin A nephropathy in Japan. Am J Kidney Dis. 1997;29:526–32.
D’Amico G. Natural history of idiopathic IgA nephropathy and factors predictive of disease outcome. Semin Nephrol. 2004;24:179–96.
Wakai K, Kawamura T, Endoh M, Kojima M, Tomino Y, Tamakoshi A, et al. A scoring system to predict renal outcome in IgA nephropathy: from a nationwide prospective study. Nephrol Dial Transplant. 2006;21:2800–8.
Wakai K, Kawamura T, Matsuo S, Hotta N, Ohno Y. Risk factors for IgA nephropathy: a case-control study in Japan. Am J Kidney Dis. 1999;33:738–45.
Radford MG Jr, Donadio JV Jr, Bergstralh EJ, Grande JP. Predicting renal outcome in IgA nephropathy. J Am Soc Nephrol. 1997;8:199–207.
Kobayashi Y, Hiki Y, Kokubo T, Horii A, Tateno S. Steroid therapy during the early stage of progressive IgA nephropathy. A 10-year follow-up study. Nephron. 1996;72:237–42.
Pozzi C, Bolasco PG, Fogazzi GB, Andrulli S, Altieri P, Ponticelli C, et al. Corticosteroids in IgA nephropathy: a randomised controlled trial. Lancet. 1999;353:883–7.
Pozzi C, Andrulli S, Del Vecchio L, Melis P, Fogazzi GB, Altieri P, et al. Corticosteroid effectiveness in IgA nephropathy: long-term results of a randomized, controlled trial. J Am Soc Nephrol. 2004;15:157–63.
Cockcroft DW, Gault MH. Prediction of creatinine clearance from serum creatinine. Nephron. 1976;16:31–41.
Locatelli F, Pozzi C, Del Vecchio L, Andrulli S, Bolasco P, Fogazzi G, et al. New therapeutic approaches in primary IgA nephropathy. Adv Nephrol Necker Hosp. 1999;29:73–91.
Pozzi C, Andrulli S, Pani A, Scaini P, Del Vecchio L, Fogazzi G, et al. Addition of azathioprine to corticosteroids does not benefit patients with IgA nephropathy. J Am Soc Nephrol. 2010;21:1783–90.
Reich HN, Troyanov S, Scholey JW, Cattran DC. Toronto glomerulonephritis registry: remission of proteinuria improves prognosis in IgA nephropathy. J Am Soc Nephrol. 2007;18:3177–83.
Vivante A, Afek A, Frenkel-Nir Y, Tzur D, Farfel A, Golan E, et al. Persistent asymptomatic isolated microscopic hematuria in Israeli adolescents and young adults and risk for end-stage renal disease. JAMA. 2011;17(306):729–36.
Szeto CC, Lai FM, To KF, Wong TY, Chow KM, Choi PC, et al. The natural history of immunoglobulin a nephropathy among patients with hematuria and minimal proteinuria. Am J Med. 2001;110:434–7.
Kim BS, Kim YK, Shin YS, Kim YO, Song HC, Kim YS, et al. Natural history and renal pathology in patients with isolated microscopic hematuria. Korean J Intern Med. 2009;24:356–61.
Hotta O, Miyazaki M, Furuta T, Tomioka S, Chiba S, Horigome I, et al. Tonsillectomy and steroid pulse therapy significantly impact on clinical remission in patients with IgA nephropathy. Am J Kidney Dis. 2001;38:736–43.
Komatsu H, Fujimoto S, Hara S, Sato Y, Yamada K, Kitamura K. Effect of tonsillectomy plus steroid pulse therapy on clinical remission of IgA nephropathy: a controlled study. Clin J Am Soc Nephrol. 2008;3:1301–7.
Tomino Y, Sakai H. Special Study Group (IgA Nephropathy) on Progressive glomerular disease. Clinical guidelines for immunoglobulin A (IgA) nephropathy in Japan, second version. Clin Exp Nephrol. 2003;7:93–7.
Matsuo S, Imai E, Horio M, Yasuda Y, Tomita K, Nitta K, et al. Revised equations for estimated GFR from serum creatinine in Japan. Am J Kidney Dis. 2009;53:982–92.
Fujimi-Hayashida A, Ueda S, Yamagishi S, Kaida Y, Ando R, Nakayama Y, et al. Association of asymmetric dimethylarginine with severity of kidney injury and decline in kidney function in IgA nephropathy. Am J Nephrol. 2011;33:1–6.
Ballardie FW, Roberts IS. Controlled prospective trial of prednisolone and cytotoxics in progressive IgA nephropathy. J Am Soc Nephrol. 2002;13:142–8.
Ando M, Minami H, Ando Y, Saka H, Sakai S, Yamamoto M, et al. Multi-institutional validation study of carboplatin dosing formula using adjusted serum creatinine level. Clin Cancer Res. 2000;6:4733–8.
Imai E, Horio M, Yamagata K, Iseki K, Hara S, Ura N, et al. Slower decline of glomerular filtration rate in the Japanese general population: a longitudinal 10-year follow-up study. Hypertens Res. 2008;31:433–41.
Goto M, Wakai K, Kawamura T, Masahiko A, Masayuki E, Yasuhiko T. A scoring system to predict renal outcome in IgA nephropathy: a nationwide 10-year prospective cohort study. Nephrol Dial Transplant. 2009;24:3068–74.
Bjørneklett R, Vikse BE, Bostad L, Iversen BM. Long-term risk of ESRD in IgAN; validation of Japanese prognostic model in a Norwegian cohort. Nephrol Dial Transplant. 2012;27:1485–91
Lv J, Zhang H, Chen Y, Li G, Jiang L, Singh AK, et al. Combination therapy of prednisone and ACE inhibitor versus ACE-inhibitor therapy alone in patients with IgA nephropathy: a randomized controlled trial. Am J Kidney Dis. 2009;53:26–32.
Manno C, Torres DD, Rossini M, Pesce F, Schena FP. Randomized controlled clinical trial of corticosteroids plus ACE-inhibitors with long-term follow-up in proteinuric IgA nephropathy. Nephrol Dial Transplant. 2009;24:3694–701.
Xie Y, Nishi S, Ueno M, Imai N, Sakatsume M, Narita I, et al. The efficacy of tonsillectomy on longterm renal survival in patients with IgA nephropathy. Kidney Int. 2003;63:1861–7.
Acknowledgments
This study was supported in part by a grant from the Study Group on IgA Nephropathy and by a Grant-in-Aid for Progressive Renal Diseases Research, Research on Intractable Disease, from the Ministry of Health, Labour and Welfare of Japan.
Author information
Authors and Affiliations
Corresponding author
About this article
Cite this article
Tatematsu, M., Yasuda, Y., Morita, Y. et al. Complete remission within 2 years predicts a good prognosis after methylprednisolone pulse therapy in patients with IgA nephropathy. Clin Exp Nephrol 16, 883–891 (2012). https://doi.org/10.1007/s10157-012-0644-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10157-012-0644-0