Abstract
Objective
Myeloid-derived suppressor cells (MDSCs) have been identified as immunosuppressive cells in tumor-related inflammation. However, the pathogenesis of MDSCs for autoimmune disease has not been investigated as yet. The aim of this study was to address whether MDSCs contribute to autoimmune organ injury in lupus-prone mice.
Methods
MDSCs were analyzed by flow cytometric staining of CD11b+ GR-1+ in MRL-Fas lpr mice. CD4+ T-cell proliferation assay was performed by coculture with CD11b+ GR-1+ splenocytes. The percentage of immunosuppressive cells was examined during disease progression. Expression of chemokine receptor on immunosuppressive cells was analyzed, and chemotaxis assay was performed.
Results
CD11b+ GR-1low cells had a suppressive effect on CD4+ T-cell proliferation, which was restored by an arginase-1 inhibitor. CD11b+ GR-1low cells increased in percentage during disease progression in kidney and blood. The number of migrated CD11b+ GR-1low cells increased in the presence of monocyte chemoattractant protein-1/CCL2.
Conclusion
We assessed the involvement of CD11b+ GR-1low cells in autoimmune disorder in MRL-Fas lpr mice. These cells regulate immunological responses via CCL2/CCR2 signaling. The regulation of immunosuppressive monocytes may provide novel therapeutic strategy for organ damage in autoimmune diseases.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Myeloid-derived suppressor cells (MDSCs), which show heterogeneous phenotypes, including immature granulocytes, monocytes/macrophages (Mφ), dendritic cells (DCs), and early myeloid progenitors, have been originally identified as immunosuppressive cells in association with tumor expansion. These cells have been reported to express CD11b and GR-1 in mouse models [1–4]. In tumor microenvironment, MDSCs inhibit T-cell activation via arginase (ARG)-1 and nitric oxidase activation, resulting in tumor growth [4]. Moreover, MDSCs play a critical role not only in neoplastic diseases but also in other conditions [5–8]. However, the impacts of MDSCs on autoimmune disorder have not been elucidated.
It has been reported that MDSCs exist in peripheral blood and may have immunosuppressive effects in patients with inflammatory bowel disease [8] and melanoma [9]. These results indicated that MDSCs may regulate the immune response, not only within accumulated organs, but also systemically. The chemokine system plays critical roles in migration and activation in various types of cells. Regarding chemotaxis of MDSCs, recent reports show C–C chemokine receptor 2 (CCR2) regulates the dynamics in tumor environment [10–12].
Autoimmune diseases in MRL/MPJ-lpr/lpr (MRL-Fas lpr) mice resemble human systemic lupus erythematosus (SLE), characterized by dysregulation of both cellular and humoral immunity [13]. In this model, CCR2 has been reported to contribute to the progression of autoimmune kidney injury, followed by the decreased number of macrophages (Mφ) [14]. However, the pathogenesis of MDSCs, especially focused on CCR2 signaling, remains to be investigated. Moreover, it should be elucidated as to whether MDSCs regulate systemic inflammation as well as peripheral autoimmune organ injury in association with CCR2 signaling.
The aim of this study was to investigate the phenotype and function of CD11b+GR-1+ cells in MRL-Fas lpr mice and identify immunosuppressive cells. Moreover, the impact of CCR2 signaling on immunosuppressive cells was examined.
Materials and methods
Mice
MRL-Fas lpr mice were obtained from Charles River Japan Inc., Atsugi, Japan. All procedures employed in the animal experiments complied with the standards set out in the Guideline for the Care and Use of Laboratory Animals in Takara-machi Campus of Kanazawa University.
Antibodies
The following antibodies were used for flow cytometry: fluorescein isothiocyanate (FITC) conjugated rat anti-mouse CD11b antibody, phycoerythrin (PE) conjugated rat anti-mouse Gr-1 antibody, allophycocyanin (APC) conjugated hamster anti-mouse CD11c antibody, APC conjugated rat anti-mouse CD45R/B220 antibody, biotin conjugated rat anti-mouse I-Ak antibody (BD Biosciences, San Diego, CA, USA), APC conjugated rat anti-mouse F4/80 antibody (eBioscience, San Diego, CA, USA).
Immunohistochemical examination
Tissues for immunoperoxidase staining were snap-frozen in OCT (Miles Scientific, Naperville, IL, USA) and stored at −80°C. CD11b+ cells were examined using biotin conjugated anti-mouse CD11b monoclonal antibodies (BD Biosciences). These positive lesions were identified using the avidin–biotin complex technique (DAKO, Glostrup, Denmark).
Cell isolation and separation
A single cell suspension was obtained from spleens, kidneys, and bone marrow, as described previously [15]. Following cell isolation, red blood cells were lysed using fluorescence-activated cell sorter (FACS) lysing solution (BD Biosciences). CD4+ T cells and CD11b+ cells were purified from spleen using magnetic-activated cell sorting (MACS) beads (Miltenyi Biotec., Auburn, CA, USA) according to the manufacture’s protocol. The purity of cells after separation was >90%. For separation of CD11b+ GR-1+ cells, the purified CD11b+ cells were resuspended in FACS buffer [1× phosphate-buffered saline (PBS) supplemented with 2 mM ethylenediaminetetraacetate (EDTA) and 0.5% bovine serum albumin (BSA)] and stained with anti-CD11b antibodies (abs) and anti GR-1 abs. Various myeloid cell populations were sorted by FACSCalibur (BD Biosciences). Cell morphology was examined on May–Giemsa staining (DAKO) in each myeloid cell population.
Flow cytometric analysis
After single cells were collected as described above, cells were suspended in FACS buffer. Then, cell-surface markers were stained with 10% mouse serum blocking. The biotinylated antibodies were visualized with PerCP-Cy5.5 streptavidin (BD Biosciences). FACS data were acquired on FACSCalibur. The percentage of cells expressing cell-surface marker were determined by analyzing a minimum of 50,000 cells using FlowJo software (Tree Star, Palo Alto, CA, USA).
In vitro cell culture experiment
Splenic CD4+ T cells and CD11b+ GR-1+ cells were cocultured as described previously [7]. Briefly, CD4+ T cells and CD11b+ GR-1+ cells were purified from MRL-Fas lpr mice at the age of 12 weeks, as described above. These cells were suspended in Roswell Park Memorial Institute (RPMI) 1640 medium (Invitrogen, Carlsbad, CA, USA), including 100 μg/ml streptomycin and 100 U/ml penicillin. Purified CD11b+ GR-1+ cells were first treated with mitomycin C (Nacalai Tesque Inc., Kyoto, Japan) at 10 μg/ml for 2 h at 37°C in 5% carbon dioxide (CO2) cell culture incubator. CD4+ T cells were stimulated by Biocoat anti-mouse CD3-coated plate (BD Biosciences) at 1.5 × 106 cells/well. CD11b+ GR-1+ cells were added to CD4+ T cells at 1:1 or different ratios. To determine the impact of arginase 1 for CD11b+ GR-1+ cells, 0.5 mM N(omega)-hydroxy-nor-l-arginine (nor-NOHA) (Carbiochem, Gibbstown, NJ, USA) was added in some experiments. After 48 h, 10 μg/well WST-1 (Premix WST-1 Cell Proliferation Assay System; Takara Bio Inc., Tokyo, Japan) was added to each well for proliferation assay, and cells were harvested for 4 h. Absorbance was measured at 450 nm with a reference wavelength of 650 nm. The proliferative activity of the isolated CD11b+ GR-1+ cells was subtracted to determine the activity of CD4+ T cells.
Chemotaxis assay
Isolated CD11b+ GR-1low splenocytes were resuspended at 5 × 106 cell/ml in RPMI 1640 medium with 0.5% BSA. The 60-μl cells were added into 8-μm pore-size chemotaxis chamber (Chemotaxicell 96; Kurabou, Osaka, Japan). The lower chamber of the 96-well plates (BD Pharmingen) was filled with 100 μl of medium containing 10 ng/ml murine recombinant monocyte chemoattractant protein (MCP)-1 (R&D, Minneapolis, MN, USA). The chamber was incubated for 2 h at 37°C in 5% CO2 cell culture incubator. The number of cells that migrated through the filter into the lower chamber was counted using the cell counter of FACScalibur.
RT-PCR analysis
Total RNA was purified from isolated CD11b+ GR-1low splenocytes using RNeasy mini kit (Qiagen, Valencia, CA, USA). Reverse transcription (RT) was performed with SuperScript II (Invitrogen). Multiple CCR expression was analyzed using a multiplex polymerase chain reaction (MPCR) kit for mouse chemokine receptor CCR set-1 (Maxim Biotec Inc., San Francisco, CA, USA) according to the manufacture’s instruction manual.
Statistical analyses
Data represent mean ± SEM. Statistical significance was determined by analysis of variance (ANOVA) and Kruskal–Wallis analyses. Significance was judged at a P value of <0.05.
Results
MRL-Fas lpr mice contained three distinct populations of CD11b+ GR-1+ cells, which showed the different character in morphology and phenotype
To determine whether MDSCs exist in MRL-Fas lpr mice, flow cytometric analysis was performed in 10-week-old animals. CD11b+ GR-1+ cells contained three distinct populations, showing CD11b+ GR-1high, CD11b+ GR-1int, and CD11b+ GR-1low cells (Fig. 1a). These populations comprised 5.9 ± 1.0%, 1.6 ± 0.1%, and 4.6 ± 0.3%, respectively. May–Giemsa stain exhibited that CD11b+ GR-1high cells had lobular-shaped nuclei, whereas CD11b+ GR-1int and CD11b+ GR-1low cells were monocytic in morphology (Fig. 1b). Phenotypic study revealed that CD11b+ GR-1high cells did not express F4/80, CD11c or B220. CD11b+ GR-1int cells expressed F4/80 but did not express CD11c or B220. Part of CD11b+ GR-1low cells expressed F4/80, CD11c and B220 (Fig. 1c). These data suggest that CD11b+ GR-1high cells were granulocyte lineage and that CD11b+ GR-1int cells were F4/80+ macrophage lineage. CD11b+ GR-1low cells contained heterogeneous populations.
Morphology and phenotype of CD11b+GR-1+ cells in spleen of MRL-Fas lpr mice. a Three distinct populations of CD11b+ GR-1+ cells were identified in the spleen of MRL-Fas lpr mice: CD11b+ GR-1high, CD11b+ GR-1int, and CD11b+ GR-1low. b May–Giemsa stain exhibited that CD11b+ GR-1high cells have lobular-shaped nuclei, whereas CD11b+ GR-1int and CD11b+ GR-1low cells are monocytic in morphology. c Phenotypic study revealed that CD11b+ GR-1high cells do not express F4/80, CD11c or B220. CD11b+ GR-1int cells express F4/80 but not CD11c or B220. Some CD11b+ GR-1low cells express F4/80, CD11c, and B220. Splenocytes from MRL-Fas lpr mice at 10 weeks of age was analyzed by flow cytometry
CD11b+ GR-1low cells suppress T cell proliferation via ARG-1 activity
To investigate whether CD11b+ GR-1+ cells from MRL-Fas lpr mice have inhibitory effects on T-cell proliferation, each population of CD11b+ GR-1+ cells was cultured with CD4+ T cells at the ratio of 1:1 in anti-mouse CD3-coated plates (Fig. 2a). CD11b+ GR-1high cells had no effect on CD4+ T-cell proliferation, whereas CD11b+ GR-1int cells significantly induced proliferation of CD4+ T cells compared with CD4+ T cells cultured alone (CD4 only 0.09 ± 0.01, CD4 + CD11b+ GR-1high cells 0.08 ± 0.02, CD4 + CD11b+ GR-1int cells 0.40 ± 0.10). In contrast, CD11b+ GR-1low cells significantly inhibited the proliferation of CD4+ T cells (0.03 ± 0.01) (Fig. 2a). At the increased ratio of CD11b+ GR-1low cells to CD4+ T cells (2:1) the proliferation of CD4+ T cells was completely suppressed (CD4 only 0.38 ± 0.02, CD4 + 2 × CD11b+ GR-1low cells 0.01 ± 0.00) (Fig. 2b). However, no inhibitory effect of CD11b+ GR-1low cells was shown at the ratio of 0.2:1(0.36 ± 0.01) (Fig. 2b). To determine the impact of ARG-1 on inhibitory effects of CD11b+ GR-1low cells, the cultured cells were treated with 0.5 mM nor-NOHA, an ARG-1 inhibitor. The supplementation of nor-NOHA restored T-cell proliferation (0.25 ± 0.04) (Fig. 2b). These results imply that CD11b+ GR-1low cells had the inhibitory effect on CD4+ T-cell proliferation via ARG-1 activation in MRL-Fas lpr mice.
To investigate whether CD11b+ GR-1+ cells from MRL-Fas lpr mice have an inhibitory effect on T-cell proliferation, each population of CD11b+ GR-1+ cells was cocultured with CD4+ T cells at the ratio of 1:1 in anti-mouse-CD3-coated plate. a CD11b+ GR-1high cells had no effect to CD4+ T-cell proliferation, whereas CD11b+ GR-1int cells induced proliferation of CD4+ T cells compared with CD4+ T cells cultured alone. In contrast, CD11b+ GR-1low cells inhibit the proliferation of CD4+ T cells. b At the increased ratio of CD11b+ GR-1low cells to CD4+ T cells (2:1) proliferation of CD4+ T cells was completely suppressed. However, the inhibitory effect of CD11b+ GR-1low cells was not shown at the ratio of 0.2:1. Moreover, supplementation of N(omega)-hydroxy-nor-l-arginine (nor-NOHA), an ARG-1 inhibitor, restored T-cell proliferation. Proliferative activity of the isolated CD11b+ GR-1+ cells was subtracted to determine the activity of CD4+ T cells. # p < 0.01, ++ p < 0.05
Percentage of CD11b+ GR-1low cells changed according to disease activity in MRL-Fas lpr mice
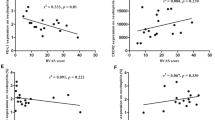
MRL-Fas lpr mice show glomerular, tubular, and perivascular lesions at 22 weeks age (Fig. 3) [16]. To detect the localization of CD11b+ cells in peripheral organs, immunohistochemistry was performed on the spleens and kidneys of 22-week-old animals. In the spleens, CD11b+ cells were detected at perifollicular lesions (Fig. 3a). In the kidneys, CD11b+ cells were observed at perivascular lesions (Fig. 3b) and within glomeruli (Fig. 3c). The percentage of CD11b+ GR-1low cells in spleen, bone marrow, kidney, and peripheral blood was analyzed during disease progression. In the spleen and bone marrow, the percentage of CD11b+ GR-1low cells significantly increased in the early stage of the disease, then decreased according to disease activity (Fig. 3d, e). In spleen, CD11b+ GR-1low cells increased from 3.5 ± 0.1% of all splenocytes at 6 weeks of age to 4.6 ± 0.3% at 10 weeks of age, then decreased to 2.7 ± 0.5% at 22 weeks of age. In bone marrow, CD11b+ GR-1low cells increased from 6.7 ± 1.0% at 6 weeks of age to 10.8 ± 0.9% at 14 weeks of age, then decreased to 8.1 ± 0.3% at 22 weeks of age. In contrast, the percentage of CD11b+ GR-1low cells increased during disease progression in kidney and blood (Fig. 3f, g). The percentage increased from 0.1 ± 0.0% of all kidney cells at 6 weeks of age to 2.0 ± 0.2% at 22 weeks of age, and from 2.2 ± 0.5% at 6 weeks of age to 15.2 ± 2.8% at 22 weeks of age in blood. In MRL++ mice, the frequency of CD11b+ GR-1low cells did not change in these organs.
Localization of CD11b+ cells and the time course of CD11b+ GR-1low cells were examined in MRL-Fas lpr mice. MRL-Fas lpr mice show glomerular hypercellularity, tubular damage (dilatation and casts asterisks), and perivascular cell infiltration (arrowheads) at 22 weeks age (×200). a In the spleens, CD11b+ cells were detected at perifollicular lesions (×100). b In the kidneys, CD11b+ cells were observed at perivascular lesions (×100). c CD11b+ cells also localized within glomeruli (×400). Frozen sections were stained with the indirect avidin-biotinylated peroxidase complex method. d, e In the spleen and bone marrow, the frequency of CD11b+ GR-1low cells was significantly increased in the early stage of the disease, then decreased according to disease activity. f, g In contrast, the frequency of CD11b+ GR-1low cells increased during disease progression in the kidney and blood. v Vessel, # p < 0.01, ++ p < 0.05 compared with 6 weeks
CCR2 signaling contributed to migration of CD11b+ GR-1low cells
To examine whether CCR2 contributes to chemotaxis of CD11b+ GR-1low cells in MRL-Fas lpr mice, the expression of CCR2- and MCP-1/CCL2-induced chemotaxis assay was examined. Multiple chemokine receptor expression analyses revealed that CD11b+ GR-1low cells strongly expressed CCR4 and CCR5 and weakly expressed CCR2 mRNAs (Fig. 4a). In the chemotaxis assay, MCP-1/CCL2 induced chemotaxis of CD11b+ GR-1low cells (CD11b+ GR-1low cells alone; 1125 ± 41/well, MCP-1/CCL2 added; 1434 ± 25/well) (Fig. 4b).
To test the impact of chemokine receptor for myeloid-derived suppressor cell (MDSC) function, chemokine receptor expression and functional assays were performed. a Multiple polymerase chain reaction (PCR) analysis for chemokine receptor revealed that CD11b+ GR-1low cells strongly expressed CCR4 and CCR5 and weakly expressed CCR2 mRNAs. b In the chemotaxis assay, MCP-1/CCL2 induced chemotaxis of CD11b+ GR-1low cells. ++ p < 0.05
Discussion
In various tumor models, the critical role of MDSCs has been reported. However, the impact of MDSCs on inflammatory disease, especially for autoimmune organ disease, has not previously been examined. In this study, proliferation of CD4+ T cells was markedly inhibited by coculture with CD11b+ GR-1low cells and restored by ARG-1 inhibitor. These cells were monocytic in morphology and showed heterogeneous populations in phenotype. In spleen and bone marrow, the percentage of CD11b+ GR-1low cells was increased in the early stage of the disease. In kidney and peripheral blood, the percentage of CD11b+ GR-1low cells increased according to disease activity. CCL2/CCR2 signaling contributed to the migration of CD11b+ GR-1low cells. Taken together, these results suggest that CD11b+ GR-1low cells are immunosuppressive cells and may contribute to autoimmune response in MRL-Fas lpr mice via CCL2/CCR2 signaling.
CD11b+ GR-1+ cells contained three distinct populations in MRL-Fas lpr mice. Based on morphology and cell-surface markers, CD11b+ GR-1high cells are of granulocyte lineage. These cells showed no effects on CD4+ T cells in functional assay. CD11b+ GR-1int cells express F4/80 and activated CD4+ T cell proliferation, indicating this population as Mφ lineage. CD11b+ GR-1low cells had the suppressive effect on CD4+ T cells. Therefore, this subset may be responsible for immunosuppressive cells in MRL-Fas lpr mice. Supporting this notion, some reports exhibited suppressive effects of CD11b+ GR-1low cells in tumor mice models [11, 17]. Moreover, the l-arginine metabolism is one of the mechanisms by which MDSCs suppress T-cell function [4]. In this regard, ARG-1 inhibitor restored CD4+ T cells function, which was cultured with CD11b+ GR-1low cells in our study. In addition, CD11b+ cells were detected in perifollicular lesions of the spleen, indicating that CD11b+ cells interact with T cells. These results may indicate CD11b+ GR-1low cells as MDSCs in MRL-Fas lpr mice. However, recent reports showed CD11b+ GR-1− F4/80+ monocytes, which expressed arginase 1, as immunosuppressive M2 Mφ [18–20]. Moreover, tumor-infiltrating MDSCs have been reported to bear M1 and M2 Mφ characteristics [11]. Therefore, distinct and defined markers between MDSCs and M2 Mφ remain to be determined.
The percentage of CD11b+ GR-1low cells increased in spleen, kidney, and blood in 10-week-old MRL-Fas lpr mice, suggesting these cells contribute to immune modulation. Zhu et al. [7] reported that the percentage of MDSCs in peripheral organs increased after disease induction in experimental autoimmune encephalomyelitis. In alopecia areata mice, injection of MDSCs has been reported to promote hair growth by inhibiting T-cell function [6]. These results, together with our results, indicated that MDSCs play an important role not only in neoplastic diseases but also in inflammatory diseases. In in vitro study, the low expression of CCR2 mRNAs was detected on CD11b+ GR-1low cells. Moreover, MCP-1/CCL2 induced chemotaxis of CD11b+ GR-1low cells. This notion was suggested in recent reports, which revealed that some chemokine receptors, including CCR2, CCR5, and CX3CR1, were expressed on MDSCs and contributed to chemotaxis [10–12].
In conclusion, we assessed the involvement of CD11b+ GR-1low cells, which were responsible for CD4+ T-cell suppression in MRL-Fas lpr mice. Immunosuppressive monocytes regulated immunological responses via CCR2 signaling. Further, regulation of immunosuppressive monocytes may provide a novel therapeutic strategy for organ damage in autoimmune diseases.
References
Serafini P, Borrello I, Bronte V. Myeloid suppressor cells in cancer: recruitment, phenotype, properties, and mechanisms of immune suppression. Semin Cancer Biol. 2006;16:53–65.
Talmadge JE, Donkor M, Scholar E. Inflammatory cell infiltration of tumors: Jekyll or Hyde. Cancer Metastasis Rev. 2007;26:373–400.
Marigo I, Dolcetti L, Serafini P, Zanovello P, Bronte V. Tumor-induced tolerance and immune suppression by myeloid derived suppressor cells. Immunol Rev. 2008;222:162–79.
Rodríguez PC, Ochoa AC. Arginine regulation by myeloid derived suppressor cells and tolerance in cancer: mechanisms and therapeutic perspectives. Immunol Rev. 2008;222:180–91.
Makarenkova VP, Bansal V, Matta BM, Perez LA, Ochoa JB. CD11b+/Gr-1+ myeloid suppressor cells cause T cell dysfunction after traumatic stress. J Immunol. 2006;176:2085–94.
Marhaba R, Vitacolonna M, Hildebrand D, Baniyash M, Freyschmidt-Paul P, Zöller M. The importance of myeloid-derived suppressor cells in the regulation of autoimmune effector cells by a chronic contact eczema. J Immunol. 2007;179:5071–81.
Zhu B, Bando Y, Xiao S, Yang K, Anderson AC, Kuchroo VK, et al. CD11b+Ly-6C(hi) suppressive monocytes in experimental autoimmune encephalomyelitis. J Immunol. 2007;179:5228–37.
Haile LA, Wasielewski RV, Gamrekelashvili J, Krüger C, Bachmann O, Westendorf AM, et al. Myeloid-derived suppressor cells in inflammatory bowel disease: a new immunoregulatory pathway. Gastroenterology. 2008;135:871–81.
Filipazzi P, Valenti R, Huber V, Pilla L, Canese P, Iero M, et al. Identification of a new subset of myeloid suppressor cells in peripheral blood of melanoma patients with modulation by a granulocyte-macrophage colony-stimulation factor-based antitumor vaccine. J Clin Oncol. 2007;25:2546–53.
Huang B, Lei Z, Zhao J, Gong W, Liu J, Chen Z, et al. CCL2/CCR2 pathway mediates recruitment of myeloid suppressor cells to cancers. Cancer Lett. 2007;252:86–92.
Umemura N, Saio M, Suwa T, Kitoh Y, Bai J, Nonaka K, et al. Tumor-infiltrating myeloid-derived suppressor cells are pleiotropic-inflamed monocytes/macrophages that bear M1- and M2-type characteristics. J Leukoc Biol. 2008;83:1136–44.
Sawanobori Y, Ueha S, Kurachi M, Shimaoka T, Talmadge JE, Abe J, et al. Chemokine-mediated rapid turnover of myeloid-derived suppressor cells in tumor-bearing mice. Blood. 2008;111:5457–66.
Kelley VR, Wuthrich RP. Cytokines in the pathogenesis of systemic lupus erythematosus. Semin Nephrol. 1999;19:57–66.
Pérez de Lema G, Maier H, Franz TJ, Escribese M, Chilla S, Segerer S, et al. Chemokine receptor Ccr2 deficiency reduces renal disease and prolongs survival in MRL/lpr lupus-prone mice. J Am Soc Nephrol. 2005;6:3592–601.
Sakai N, Wada T, Yokoyama H, Lipp M, Ueha S, Matsushima K, et al. Secondary lymphoid tissue chemokine (SLC/CCL21)/CCR7 signaling regulates fibrocytes in renal fibrosis. Proc Natl Acad Sci USA. 2006;103:14098–103.
Iwata Y, Wada T, Furuichi K, Sakai N, Matsushima K, Yokoyama H, et al. p38 Mitogen-activated protein kinase contributes to autoimmune renal injury in MRL-Fas lpr mice. J Am Soc Nephrol. 2003;14:57–67.
Gallina G, Dolcetti L, Serafini P, De Santo C, Marigo I, Colombo MP, et al. Tumors induce a subset of inflammatory monocytes with immunosuppressive activity on CD8+ T cells. J Clin Invest. 2006;116:2777–90.
Xiao W, Hong H, Kawakami Y, Lowell CA, Kawakami T. Regulation of myeloproliferation and M2 macrophage programming in mice by Lyn/Hck, SHIP, and Stat5. J Clin Invest. 2008;118:924–34.
Gordon S, Taylor PR. Monocyte and macrophage heterogeneity. Nat Rev Immunol. 2005;5:953–64.
Mantovani A, Sica A, Locati M. Macrophage polarization comes of age. Immunity. 2005;23:344–6.
Acknowledgments
Y I is a recipient of a Grant-in-Aid from the Ministry of Education, Science, Sports, and Culture in Japan. T W is a recipient of a Grant-in-Aid from the Ministry of Education, Science, Sports, and Culture in Japan and Takeda Science Foundation.
Conflict of interest statement
The authors have no confliction of interest.
Author information
Authors and Affiliations
Corresponding author
About this article
Cite this article
Iwata, Y., Furuichi, K., Kitagawa, K. et al. Involvement of CD11b+ GR-1low cells in autoimmune disorder in MRL-Fas lpr mouse. Clin Exp Nephrol 14, 411–417 (2010). https://doi.org/10.1007/s10157-010-0309-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10157-010-0309-9