Abstract
Background
Anemia is common among patients with chronic kidney disease (CKD). The introduction of erythropoietin treatment has changed anemia management, but the therapeutic hemoglobin (Hb) target is still under debate, and clinical evidence for its effect on cardiac functions and QOL is sparse.
Methods
A 16-week dose–response study and a 32-week follow-Up study were combined. After correcting anemia of less than 10 g/dl in pre-dialysis Japanese CKD patients, a higher Hb target (12–13 g/dl) by darbepoetin alfa (DPO) was compared with the conventional Hb target by epoetin alfa (EPO). Outcomes were anemia correction, management of the left ventricular mass index (LVMI) and QOL scores.
Results
No significant difference was seen in Hb at baseline and week 16, but a significant difference was recorded at week 34 (12.34 ± 0.93 g/dl for DPO and 10.43 ± 0.90 g/dl for EPO). In both groups, LVMI decreased similarly until week 16, but the decrease of EPO was retarded, and a significant difference between LVMI was seen only in DPO at week 34 (100.7 ± 16.6 g/m2 for DPO and 110.9 ± 25.2 g/m2 for EPO). Relationships between Hb and LVMI change at week 34 were examined by stratifying Hb into four groups (Hb <10 g/dl, 10 g/dl ≤ Hb <11 g/dl, 11 g/dl ≤ Hb <12 g/dl and 12 g/dl ≤ Hb), and a decrease of LVMI was prominent in the 12 g/dl ≤ Hb group. Correction of anemia to 11 g/dl or more led to improved QOL scores. No safety difference was observed among the treatments.
Conclusions
Targeting a higher Hb around 12 g/dl was more beneficial than targeting conventional Hb in terms of reduction of LVMI and QOL. Further studies to determine the appropriate Hb target are necessary.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Anemia is a common problem among patients with advanced chronic kidney disease (CKD). Prior to the availability of erythropoietic stimulating agents (ESAs), chronic blood transfusions represented the standard of care for treating anemia. Chronic treatment with transfusions carried inherent risks associated with infection, such as viral hepatitis, iron overload and the risk of alloimmunization [1]. With the approval of recombinant erythropoietin (EPO), the care of patients with CKD and anemia dramatically changed, and the necessity of transfusion to treat anemia in this group was greatly diminished. Currently, the objective of anemia treatment with EPO is not just to avoid transfusion, but also to improve the symptoms of anemia, such as shortness of breath and fatigue. However, the optimal hemoglobin (Hb) target applied in EPO therapy is still under debate and is being examined closely by the medical community.
The KDOQI guideline for anemia treatment was updated in 2006 to raise the upper limit of the Hb target, which previously had been set at 12 g/dl [2]. Afterward, negative patient outcomes of the CHOIR study in which a higher Hb target (13.5 g/dl) was compared to conventional treatment (11.3 g/d) were reported [3], and the therapeutic Hb target for patients with CKD became a topic of heated discussion once again [4, 5]. While several observational studies suggested that higher Hb indicated better patient outcomes or good patient health status [6–9], prospective studies such as CHOIR and CREATE [10], to correct anemia higher than the recommended Hb, failed to demonstrate a benefit. The difference might derive from the situations of daily clinical practice and clinical study settings that require strict protocol compliance with closer attention to the specific therapeutic effect of the treatment [4]. In Japan, the therapeutic Hb target for EPO treatment in regular clinical practice for patients with CKD, regardless of renal replacement therapy, is set at around 10 g/dl by the government. There are few reports in which a high Hb target has been applied and its effects examined in a large Asian population, including the Japanese. Additionally, Fukuhara et al. [11] reported that a decline in quality of life (QOL) was associated with an increase in serum creatinine and a decline in hematocrit in CKD patients. Although KDOQI and other guidelines, including European ones [12], recommend that the Hb target level should be 11.0 g/dl or greater in terms of QOL, it has not been well validated in Asian populations. On the other hand, it was reported that normalization of the hematocrit level in Japanese CKD patients led to favorable cardiovascular changes in a small prospective study [13]. Therefore, we report the results of a clinical trial in pre-dialysis CKD patients that compared the therapeutic Hb target of 12–13 g/dl to that of 10–12 g/dl, and investigated its impact on left ventricular mass index (LVMI) reduction and QOL. This is a combined analysis of two consecutive comparative randomized clinical studies comprised of the dose–response and follow-up studies of darbepoetin alfa (DPO) and EPO. Originally, the dose–response study was conducted to examine the dose–response relationship of DPO with Hb in anemia correction. The follow-up study was to evaluate the safety and efficacy of DPO at a higher therapeutic Hb target compared with EPO at the conventional Hb target.
Materials and methods
Study population
The dose–response and follow-up studies were multicenter, randomized, open-label, parallel-group studies conducted from July 2004 through December 2005. Fifty-two medical centers and hospitals in Japan participated in the studies. The studies were conducted in accordance with the Declaration of Helsinki and international guidelines for good clinical practice. The protocols were approved by each local institutional review board prior to implementation.
The dose–response study enrolled adults with anemia (Hb <10 g/dl without administration of EPO in the last 4 weeks) and CKD [creatinine ≥2 mg/dl (177 μmol/l)] who were aged 20–80 years and weighed 40–80 kg, and who were not expected to initiate regular renal replacement therapy within 16 weeks. However, those with uncontrolled hypertension, congestive heart failure [New York Heart Association (NYHA) class III–IV] and known history of symptomatic myocardial, pulmonary and cerebral infarction, unstable angina and obstructive arteriosclerosis (Fontaine’s class II–IV) were excluded together with those with malignancy, major bleeding, recent surgery, transfusion or investigational products within 16 weeks. All patients gave written informed consent prior to study enrollment. Those who completed the dose–response study and were not expected to initiate regular renal replacement therapy within another 32 weeks were asked to enroll in the follow-up study. Those subjects who agreed to participate in the follow-up study were asked to provide additional written informed consent.
Study design
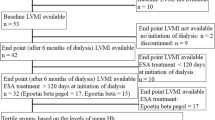
The design of the dose–response and follow-up studies is shown in Fig. 1; the first 16 weeks were allocated to the dose–response study and the latter 32 weeks to the follow-up study. Eligible patients were randomly assigned to receive 30, 60 or 90 μg of DPO subcutaneously every other week or 6,000 IU of EPO subcutaneously once a week in the dose–response study. The dosage of the drug was not changed until Hb reached above 12 g/dl. Administration was suspended if severe adverse events occurred or the rate of Hb rise was over 3 g/dl in 4 weeks as set in the previous similar study [14]. After achieving the lower bound of the therapeutic target, the dosage was adjusted to maintain the target range at a physician’s discretion. Randomization of patients was performed centrally into four treatment groups with dynamic allocation, stratified by Hb, serum creatinine and institution. In this analysis, all groups in the study were integrated to investigate the relationship between QOL and Hb or Hb rise.
In the follow-up study, allocation of DPO and EPO for each patient was not changed from the dose–response study. Therefore, the ratio of patients with DPO to EPO was expected to be about 3:1. Patients treated with DPO were assigned to maintain a target of 12–13 g/dl, whereas those treated with EPO were to maintain a target of 10–12 g/dl. DPO was administered every 2 or 4 weeks subcutaneously, and the maximum dose was limited to 180 μg. The dose of DPO was adjusted to maintain the target range at the discretion of each investigator and selected from the following: 15, 30, 60, 90, 120 and 180 μg. Dose increase per time was limited to the next higher dose. Dosage of EPO was subcutaneous 6,000 IU weekly or 6,000–12,000 IU every 2 weeks, which was the approved dosage on the product label in Japan.
An iron supplement was prescribed as appropriate to keep transferrin saturation above 20% or ferritin above 100 ng/ml.
All patients had a clinical assessment at least every 2 weeks throughout the two trials. Echocardiographic images were obtained at baseline, week 16 and 34 after the initiation of the dose–response study for the assessment of cardiac functions together with electrocardiograms and chest X-rays. With patient information blinded, independent cardiologists excluded those that were incomparable for drawing a comparison for each of the three points. LVMI was measured with two-dimensional echo-guided M-mode echocardiograms, and the calculation used for the body surface correction was the Devereux formula: 0.8 × {1.04 × [(LVDd + IVST + PWT)3 − LVDd3]} + 0.6 (LVDd: left ventricular end-diastolic diameter, IVST: interventricular septal thickness, PWT: left ventricular posterior wall thickness).
For QOL assessments, a self-administered medical outcomes study, the 36-item short-form health survey (SF-36), and a functional assessment of chronic illness therapy (FACIT) fatigue scale, instruments widely employed [3, 10, 11, 15, 16] to measure perceived health status and daily functioning, were conducted at baseline, week 8 and 16 after the initiation of the dose–response study.
Study objectives
The objective of this exploratory combined analysis was to investigate whether the differences of anemia correction and management had an effect on LVMI reduction and QOL in Japan.
Statistical analysis
The chi-square test was applied to compare categorical data, and the Student’s t test was applied to compare means, while analysis of variance was applied to compare serial changes among the groups over time. Analysis of covariance was used to calculate the effects of Hb on the values that demonstrate cardiac functions like LVMI and QOL scores. P < 0.05 was considered significant.
The sample size was originally estimated to investigate the relationship of DPO dosage with Hb rise in the dose–response study.
Results
Patients
Two hundred ten patients were screened, and 171 received at least one treatment in the dose–response study. One hundred forty-three patients completed it, and 116 continued on to the follow-up study. Eighty-four patients accomplished this (Fig. 2). Drop-out rates were similar among the treatment groups in both studies. In the dose–response study, the major reason of withdrawal was initiation of renal replacement therapy [12 out of 28 patients (42.8%)]. In the follow-up study, 11 (34.4%) patients dropped out because of the occurrence of an adverse event and 14 (43.7%) because of initiation of renal replacement therapy.
Patient disposition. Participant flow chart. A total of 171 patients were enrolled in this study; 143 completed the dose–response study, and 84 completed the follow-up study. The major reason for withdrawal was initiation of renal replacement therapy and occurrence of an adverse event. EPO Epoetin alfa, DPO darbepoetin alfa
No major imbalances were observed in the demographics of the 171 patients who received at least one dose in the dose–response study, although the numbers of females in the EPO group and the group of patients with a heavier weight of DPO 60 μg were slightly higher than in the others (Table 1). There was no difference in cardiovascular history and use of anti-hypertensives as well as the ratio of patients with diabetes.
Anemia correction and maintenance
Figure 3 shows mean Hb throughout the studies. In the dose–response study, mean (±SD) Hb of the integrated value across the groups was 8.76 ± 1.00 g/dl at baseline and rose gradually to 10.58 ± 1.32 g/dl at week 8 and 11.25 ± 1.33 g/dl at week 16. There was no difference in baseline values among the treatment groups, and the mean Hb of patients with DPO increased in a dose-dependent manner after initiation. Significant differences were observed in the Hb rate of rise between 90 and 30 μg (P < 0.001), and between 90 and 60 μg (P = 0.001). The Hb rise of patients with EPO was comparable to 60 μg of DPO. In the follow-up study, the mean Hb of DPO and EPO was 10.88 ± 1.23 and 10.21 ± 0.87 g/dl, respectively. The mean Hb of DPO increased slowly, reached 12.31 ± 0.97 g/dl at week 34 and stayed around 12 g/dl, while EPO was kept around 10 g/dl, as the product label in Japan recommended. Hb values after final dosing were 11.75 ± 0.99 g/dl at week 48 and 11.23 ± 0.87 g/dl at week 50 for DPO, and 10.42 ± 1.04 g/dl at week 48 for EPO. No significant change was observed in the mean weekly dose for both treatment groups in the follow-up study (data not shown).
LVMI
After an independent review, the data of 49 patients for whom all three echocardiographs at baseline, week 16 and week 34 had been judged assessable and comparable were subjected to the analysis. There was no significant difference in mean (±SD) Hb between the treatment groups at baseline (9.18 ± 0.62 g/dl for DPO and 9.09 ± 0.85 g/dl for EPO) and week 16 (11.61 ± 1.15 g/dl for DPO and 11.01 ± 0.75 g/dl for EPO), but the difference became significant at week 34 (12.34 ± 0.93 g/dl for DPO and 10.43 ± 0.90 g/dl for EPO), as expected (Fig. 4a). Inverse changes were observed in the mean (±SD) LVMI. The LVMI of both groups decreased similarly until week 16 (118.1 ± 23.5–110.9 ± 24.3 g/m2 for DPO and 119.0 ± 31.7–112.5 ± 27.1 g/m2 for EPO). However, a decrease of LVMI in patients with EPO was retarded, while that of DPO continued to week 34 (100.7 ± 16.6 g/m2 for DPO and 110.9 ± 25.2 g/m2 for EPO) (Fig. 4b). There was a significant difference of LVMI score only in the DPO group between baseline and week 34, and between week 16 and week 34. Since DPO has almost the same pharmacological effects as EPO [17], we considered it appropriate to divide patients regardless of their treatment groups into categories based on their Hb level at week 34, adjusted by baseline, and examine the relationships between Hb and change of LVMI [categories: Hb <10 g/dl (n = 5), 10 g/dl ≤ Hb <11 g/dl (n = 5), 11 g/dl ≤ Hb <12 g/dl (n = 14), 12 g/dl ≤ Hb (n = 25)]. A significant decrease was observed in 11 g/dl ≤ Hb <12 g/dl (P = 0.004) and 12 g/dl ≤ Hb (P < 0.001) compared to that of baseline (Fig. 5). Although the numbers of the lower Hb subsets were limited, significant correlation was demonstrated by linear regression analysis (P = 0.004) (data not shown). No significant change was detected in electrocardiograms and the chest-thoracic ratio measured from chest X-rays. The incidences of patients who initiated renal replacement therapy were similar in both groups in the follow-up study. Furthermore, the number of patients who used anti-hypertensives such as ARB or ACEi was 31 (88.6%) for the DPO group and 13 (92.9%) for the EPO group. At the start of the study, the numbers of these patients were 30 (85.7%) and 12 (85.7%), respectively, and the ratio was nearly the same throughout the study.
Quality of life assessment
All 171 patients who received at least one treatment filled out the questionnaire. One hundred sixty-three and 143 patients repeated it at week 8 and 16, respectively. Means of most domains of the SF-36 and FACIT fatigue score in week 8 and 16 rose higher than baseline. The difference was significant (P < 0.05) in four (RP, role-physical; GH, general health; VT, vitality; FF, FACIT fatigue) and 2 (GH and FF) items at week 8 and 16, respectively (Fig. 6). Baseline to week 8 was prominent, especially for vitality among the SF-36 domains. The correlation between change of vitality and Hb at week 8 was examined by stratifying Hb into three categories: Hb <10 g/dl (n = 47), 10 g/dl ≤ Hb <11 g/dl (n = 47) and 11 g/dl ≤ Hb (n = 69). The result adjusted by sex, age, weight and baseline value demonstrated a significant increase in subsets 10 g/dl ≤ Hb < 11g/dl (P = 0.005) and 11 g/dl ≤ Hb (P < 0.001) compared to that of baseline (Fig. 7). However, significant correlation was not observed among the three subsets.
Safety
With regard to patient safety, adverse events observed in the two studies were those commonly seen in this patient population. No safety difference for adverse events with the occurrence frequency of ≥5% was reported between DPO and EPO (Fig. 8). The incidence of pruritus was similar in both products, although there was a report of an increase in the DPO treatment [18]. Headache was reported only in the DPO group. Death and antibody formation with DPO or EPO were not reported in our studies.
Discussion
Presently, use of epoetins, regardless of conventional EPO or the new long-acting DPO, is the routine treatment for patients with chronic anemia, especially for those with CKD, as more than 80% of the patients on hemodialysis therapy receive the treatment [19]. Currently, the purpose of anemia treatment by epoetins is not just to avoid transfusion, but also to improve QOL. Moreover, an association of higher hematocrit values with lower hospitalization and mortality in hemodialysis patients was indicated [6].
Silverberg et al. [20] reported that the use of epoetins in patients with chronic heart failure, targeting above 12 g/dl, improved not only anemia, but also the NYHA class and number of hospitalizations. Hayashi et al. [13] also concluded that from the perspective of left ventricular hypertrophy regression, normalization of the hematocrit was more effective than partial correction in Japanese CKD patients.
In this analysis, we examined the effect of anemia treatment on QOL and LVMI in Japanese patients with CKD not on dialysis. In Japan, the therapeutic Hb target for CKD patients, whether or not on dialysis, is set at around 10 g/dl for EPO, and treatment suspension is recommended if the Hb value exceeds 12 g/dl. Our result indicates that, at least for pre-dialysis CKD patients, a conventional target higher than the recommenced worldwide guidelines is beneficial. Continuous reduction of the LVMI score was observed only in the DPO group whose Hb target was set higher than the conventional one, and the decrease of LVMI was prominent in the 12 ≤ Hb group. Also, improvement of QOL was demonstrated in our study, as observed in other reports [10, 15, 16, 21]. Although the KDOQI guideline for anemia treatment states that it lacks sufficient evidence to recommend maintaining 13 g/dl or higher, it was updated in 2006 to lift the upper side of the Hb target [2]. Recently, however, the CHOIR study revealed that targeting 13.5 g/dl was more harmful than 11.3 g/dl in pre-dialysis patients with CKD [3]. Also, the CREATE study did not demonstrate that early anemia correction targeting over 13 g/dl reduced the risk of cardiovascular events [10]. Following the publication of these studies, the guideline was revised in 2007 to reinstitute the upper limit target value of 12 g/dl [22]. In our studies, CKD patients with serious complications were excluded, while the CHOIR study included many patients with severe complications such as myocardial infarction. It suggests that caution is needed to apply a therapeutic Hb target higher than 12 g/dl to patients with a history of serious complications, especially cardiac. In the dose–response study, we enrolled patients whose Hb was less than 10 g/dl. In contrast, patients enrolled in the CREATE study had much less anemia than ours, and the mean Hb was above 11 g/dl. Early anemia correction seems to contribute to improving QOL, but the effect on cardiac functions might be obscured if patients are not too anemic at the commencement of the treatment. The effect on renal functions should be discussed further.
Our results indicate that anemia correction and maintenance up to 12 g/dl are a reasonable target for pre-dialysis CKD patients without serious complications. Even after the publications of the CHOIR and CREATE studies, it was decided to continue a much larger study, TREAT, in which targeting 13 g/dl in CKD patients with diabetes was compared to a placebo to examine patient outcome, including composite of death and hard endpoints [23, 24]. It might be appropriate to maintain the therapeutic target on a subnormal level (around 12 g/dl) until the results of this largest trial come out. With regards to the CHOIR trial, the secondary analysis was additionally published, and it suggests that the detrimental outcome of a higher target may be associated with the inability to achieve the hemoglobin target with the use of a high EPO dose [25]. Although no deaths were reported in our study, the relationship should be investigated in future studies.
There are still certain limitations to our study, and to apply the results to the general population of renally impaired patients requires caution. For many CKD patients without severe complications, twice-a-month clinical assessments might be unrealistic in daily clinical practice. In that sense, a long-acting epoetin like DPO may play an important role in actual clinical settings, especially in countries like Japan, where self-injection of EPO is not officially authorized. Further studies for generalization are warranted.
In summary, we examined the effect of anemia correction and management, comparing groups targeting around 12 g/dl with 10 g/dl in pre-dialysis patients with CKD without severe complications. Targeting around 12 g/dl was more beneficial than 10 g/dl in terms of decreased LVMI and QOL. This indicates that higher Hb may be a more appropriate target for pre-dialysis Japanese CKD patients.
References
Vella JP, O’Neill D, Atkins N, Donohoe JF, Walshe JJ. Sensitization to human leukocyte antigen before and after the introduction of erythropoietin. Nephrol Dial Transpl. 1998;13:2027–32.
National Kidney Foundation. KDOQI clinical practice guidelines and clinical practice recommendations for anemia in chronic kidney disease in adults. Am J Kidney Dis. 2006;47 Suppl 3:S16–85.
Singh AK, Szczech L, Tang KL, et al. Correction of anemia with epoetin alfa in chronic kidney disease. N Engl J Med. 2006;355:2085–98.
Roger SD, Levin A. Epoetin trials: randomized controlled trials don’t always mimic observational data. Nephrol Dial Transpl. 2007;22:684–6.
Strippoli GFM, Tognoni G, Navaneethan SD, Nicolucci A, Craig JC. Haemoglobin targets: we were wrong, time to move on. Lancet. 2007;369:346–50.
Li S, Collins AJ. Association of hematocrit value with cardiovascular morbidity and mortality in incident hemodialysis patients. Kidney Int. 2004;65:626–33.
Pisoni RL, Bragg-Gresham JL, Young EW, et al. Anemia management and outcomes from 12 countries in the dialysis outcomes and practice patterns study (DOPPS). Am J Kidney Dis. 2004;44:94–111.
Amaral S, Hwang W, Fivush B, et al. Association of mortality and hospitalization with achievement of adult hemoglobin targets in adolescents maintained on hemodialysis. J Am Soc Nephrol. 2006;17:2878–85.
Regidor DL, Kopple JD, Kovesdy CP, et al. Associations between changes in hemoglobin and administered erythropoiesis-stimulating agent and survival in hemodialysis patients. J Am Soc Nephrol. 2006;17:1181–91.
Drueke TB, Locatelli F, Clyne N, et al. Normalization of hemoglobin level in patients with chronic kidney disease and anemia. N Engl J Med. 2006;355:2071–84.
Fukuhara S, Yamazaki S, Marumo F, et al. Health-related quality of life of predialysis patients with chronic renal failure. Nephron Clin Pract. 2007;105:c1–8.
Locatelli F, Aljama P, Barany P, et al.: Revised European best practice guidelines for the management of anaemia in patients with chronic renal failure. Nephrol Dial Transpl. 2004;19 Suppl 2:ii1–47.
Hayashi T, Suzuki A, Shoji T, et al. Cardiovascular effect of normalizing the hematocrit level during erythropoietin therapy in predialysis patients with chronic renal failure. Am J Kidney Dis. 2000;35:250–6.
Macdougall IC, Matcham J, Gray SJ, et al. Correction of anaemia with darbepoetin alfa in patients with chronic kidney disease receiving dialysis. Nephrol Dial Transpl. 2003;18:576–81.
Parfrey PS, Foley RN, Wittreich BH, et al. Double-blind comparison of full and partial anemia correction in incident hemodialysis patients without symptomatic heart disease. J Am Soc Nephrol. 2005;16:2180–9.
Rossert J, Levin A, Roger SD, et al. Effect of early correction of anemia on the progression of CKD. Am J Kidney Dis. 2006;47:738–50.
Mac dougall IC, Gray SJ, Elston O, et al. Pharmacokinetics of novel erythropoiesis stimulating protein compared with epoetin alfa in dialysis patients. J Am Soc Nephrol. 1999;10(11):2392–5.
Vanrenterghem Y, Barany P, Mann JFE, et al. Randomized trial of darbepoetin alfa for treatment of renal anemia at a reduced dose frequency compared with rHuEPO in dialysis patients. Kidney Int. 2002;62:2167–75.
Locatelli F, Pisoni RL, Combe C, et al. Anaemia in haemodialysis patients of five European countries: association with morbidity and mortality in the dialysis outcomes and practice patterns study (DOPPS). Nephrol Dial Transpl. 2004;19:121–32.
Silverberg DS, Wexler D, Blum M, et al. The effect of correction of anaemia in diabetics and non-diabetics with severe resistant congestive heart failure and chronic renal failure by subcutaneous erythropoietin and intravenous iron. Nephrol Dial Transpl. 2003;18:141–6.
Ritz E, Laville M, Bilous RW, et al. Target level for hemoglobin correction in patients with diabetes and CKD: primary results of the anemia correction in diabetes (ACORD) Study. Am J Kidney Dis. 2007;49:194–207.
National Kidney Foundation. KDOQI clinical practice guideline and clinical practice recommendations for anemia in chronic kidney disease: update of hemoglobin target. Am J Kidney Dis. 2007;50:471–530.
Mix TC, Brenner RM, Cooper ME, et al. Trial to reduce cardiovascular events with aranesp therapy (TREAT): evolving the management of cardiovascular risk in patients with chronic kidney disease. Am Heart J. 2005;149:408–13.
Pfeffer MA, for the TREAT executive committee. An Ongoing Study of Anemia Correction in Chronic Kidney Disease. N Engl J Med. 2007;356:959–61.
Szczech L, Barnhart H, Inrig J, et al. Secondary analysis of the CHOIR trial epoetin-alfa dose and achieved hemoglobin outcomes. Kidney Int. 2008. doi:10.1038/ki.2008.295.
Acknowledgment
The dose–response and follow-up studies were sponsored by Kirin Pharma Company, Ltd.
Author information
Authors and Affiliations
Corresponding author
About this article
Cite this article
Hirakata, H., Tsubakihara, Y., Gejyo, F. et al. Maintaining high hemoglobin levels improved the left ventricular mass index and quality of life scores in pre-dialysis Japanese chronic kidney disease patients. Clin Exp Nephrol 14, 28–35 (2010). https://doi.org/10.1007/s10157-009-0212-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10157-009-0212-4