Abstract
Work on wearable kidneys has evolved around the technology of hemodialysis or hemofiltration, which call for continuous anticoagulation of the extracoporeal circulation and are encumbered with potential immunologic and non-immunologic complications of continuous blood–artificial membrane interactions. A peritoneal-based automated wearable artificial kidney (AWAK) requires no extracorporeal circulation and is therefore “bloodless.” Because AWAK is designed to continuously regenerate and reuse the spent dialysate in perpetuity, it is also “waterless.” A sorbent-based assembly regenerates both the aqueous and the protein components (AqC and PrC) of the spent dialysate, producing a novel, autologous protein-containing dialysate. The regenerated AqC has the same composition as the commercially available peritoneal dialysate, but contains bicarbonate instead of lactate and has a more physiological pH. The regenerated PrC is recycled back into the peritoneal cavity, thereby ameliorating or eliminating protein loss. Depending on the steady-state protein concentrations that can be achieved (under the condition of continuous dialysate regeneration and recycling), the PrC also has the potential of both augmenting ultrafiltration and mediating the removal of protein-bound toxins. Additional sorbents can be incorporated into AWAK for the removal of middle molecular weight uremic toxins. At a regeneration rate of 4 l/h, AWAK provides a dialysate flow of 96 l/day (8–12 times the current rate). Round-the-clock dialysis and ultrafiltration provide steady-state metabolic-biochemical and fluid balance regulation, thereby eliminating “shocks” of abrupt changes in these parameters that characterize the current dialytic modalities. Dialysis-on-the-go, made possible by AWAK’s “wearability” and automation, frees end-stage renal failure patients from the servitude that is demanded by the current dialytic regimentations.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
There are three basic functional characteristics of the natural kidney that are not duplicated by the available artificial kidneys. First, the natural kidney provides continuous, round-the-clock metabolic and fluid regulation; second, it excretes, in addition to small molecular weight, water-soluble toxins, also middle molecular weight and protein-bound toxins; and third it functions “automatically,” and thereby imposes no restriction on the freedom of an individual’s living activities (Table 1).
In terms of metabolic and fluid regulation, the natural kidney removes metabolic wastes, such as urea, continuously as they are generated. Thus, blood urea, for example, is maintained at a low and steady level (Fig. 1, normal subjects). The natural kidney also regulates, at all times, the fluid volume of, and its distribution in, the body. In hemodialysis [the predominant form of therapy used in patients with end-stage renal disease (ESRD) in the USA], on the other hand, the urea and fluid that are accumulated over 2–3 days are rapidly removed within 4 h. In place of the normal steady-state level, the blood urea (Fig. 1, HD patients), as does the fluid volume, fluctuates in a seesaw pattern, a labile state for which the body is evolutionally ill prepared. It is not often realized that a 12-h weekly hemodialysis leaves an ESRD patient azotemic, uremic and fluid over-loaded for the remaining 156 h (93%) of the week. Similar observations can be made for peritoneal dialysis, in its various formats that are currently practiced, although the degree of fluctuations is less because of a more “continuous” pattern of dialysis.
In normal subjects with natural kidneys, urea is excreted as it is formed. Thus, mean blood urea level is maintained at a steady-state low level (horizontal continuous line). In hemodialysis (HD) patients, urea is removed during dialytic treatments (assuming equal interdialytic intervals) and accumulates between treatments, giving rise to a see-saw pattern of blood urea levels
Quantitative and qualitative removal of uremic toxins constitute the second major functional difference between the natural kidney and the artificial kidneys (Table 1). The European Uremic Toxin Work Group has categorized uremic toxins into three groups: (1) water-soluble, low molecular-weight solutes (MW < 500 D), (2) middle molecules (MW from 555 to 32,000 D); and (3) protein-bound solutes, most of which have MW less than 500 D [1]. Unlike the natural kidney, none of the current artificial kidneys has the capability of removing significant amounts of the middle molecular-weight and the protein-bound solutes.
The third, and we consider the most important point in Table 1, is that none of the current dialytic therapies accords patients the freedom to live a “normal life.” In practical terms, being on dialysis is like having received a sentence that markedly restricts an individual’s choice in all aspects of living. While much effort has been spent on the science and the technology of ESRD treatment, far fewer thoughts and efforts have been given to free patients from the servitude imposed by the available dialytic modalities.
These considerations have led us to the concept of a peritoneal-based automated wearable artificial kidney (AWAK).
AWAK: conceptual background
We set our goal to “functionally clone” a natural kidney with three basic properties: operates on a 24/7 basis, has the potential of removing middle molecules and protein-bound solutes, in addition to small molecular-weight solutes, and works automatically to provide dialysis-on-the-go, thereby maximizing a patient’s freedom for normal living activities.
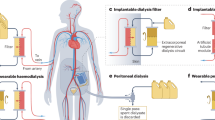
Our initial approach towards a wearable kidney was like those of most current workers in the field [2–4], i.e., based on some form of a miniaturized system of blood-cleansing outside the body [5]. The requirement for extracorporeal circulation on a life-long basis did not appeal to us as an ideal long-term strategy. The extracorporeal circulation would require, given our current technology, continuous anticoagulation and a complex monitoring system, with the additional concern for known and yet unknown consequences of immunological and non-immunological blood–artificial surface interactions. Other possible complications would include membrane fouling [6] and exsanguinations, either through occult bleeding (in continuously anti-coagulated patients) or accidental disruption of the blood circuit. There is also the possibility that continuous extracorporeal circulation may negatively affect the longevity of the limited vascular access sites. Of the two hemofiltration-based wearable kidneys reported, both clotted within a week in face of aggressive heparinization [7, 8].
We therefore, focused on a wearable, peritoneal-based system [9–12], which accomplishes dialysis through the autologous peritoneal membrane and requires no extracorporeal circulation. More importantly, chronic ambulatory peritoneal dialysis has an established successful and safe record for long-term “wearability” and is currently the most promising route towards the development of an AWAK.
The nuts-and-bolts of AWAK
Figure 2 provides a schematic of the basic components of AWAK. Dialysate flows into and out of the patient’s peritoneal cavity either in a conventional “inflow–outflow” pattern using a single-lumen catheter or in a continuous “flow-through” pattern using a single double-lumen catheter or two single-lumen catheters as shown in Fig. 2. AWAK, with its high dialysate regeneration rate (see below), is suitable for single-catheter tidal peritoneal dialysis (TPD), which can eliminate the pain, currently experienced by some patients at the initiation of dialysate inflow or at the end of dialysate outflow or both [13, 14]. The reserve volume in TPD is also anticipated to facilitate rapid dialysate outflow.
A small fraction of the spent dialysate (adjusted to the amount of fluid a patient needs to excrete) is stored in a bladder reservoir, e.g., an artificial bag, or the fluid may be diverted into the natural bladder [7] for intermittent emptying. The bulk of the spent dialysate flows through a sorbent assembly consisting of a fibrin/debris trap, a carbon filter and sorbents designed and engineered to regenerate both the ultrafiltrate and the proteins of the spent dialysate, yielding a fresh protein-containing dialysate. The proportionate protein concentrations in the peritoneal spent dialysate are similar to those in the serum (see below and Fig. 4), but are quantitatively about 80- to 100-fold more dilute. The range of protein concentrations that can be attained with continuous cycles of regeneration, is currently not known.
The enrichment motif adds to the regenerated dialysate, potassium, calcium, magnesium (removed by the sorbent assembly) and glucose (for regulating ultrafiltreation). The replenished fresh dialysate, after passing through a sterilizing filter and a gas removal module, is recycled back into the peritoneal cavity. A user-friendly “disconnect–connect” mechanism that allows contamination-proof removal and replacement of the sorbent assembly, the enrichment motif and the bladder reservoir completes the major components of the system.
AWAK: proof of concepts
Continuous flow-through peritoneal dialysis is potentially more efficient than the conventional inflow/outflow peritoneal dialysis [15, 16]. Clinical feasibility of flow-thru peritoneal dialysis has been demonstrated using either a single-double lumen catheter [17] or two single lumen catheters [18]. Using a modified REDY® sorbent cartridge, the feasibility of conducting peritoneal dialysis based on sorbent regeneration of spent peritoneal dialysate has been demonstrated [19]. Ninety successful peritoneal dialyses, each of 4–24-h duration, were conducted in 20 male patients, using a single-lumen catheter and either a conventional in-and-out, or a TPD, dialysate flow pattern. One patient was maintained on this sorbent regeneration system for 2 months. Based on the TPD mode of dialysate delivery, it was demonstrated that with a 1–1.5-l reserve volume and rapid cycles of 0.5 l of tidal volume, an exchange rate of 9 l/h could be attained, yielding an urea clearance of 31.5±1.5 ml/min. REDY® sorbent cartridges have been used successfully in hemodialysate regeneration since 1973 [20].
In the laboratory we have successfully regenerated, ex-vivo, spent peritoneal dialysate into fresh dialysate using commercially available REDY® sorbent cartridges [21]. Spent dialysate was first passed through a hemofilter to produce a protein-free ultrafiltrate, which was then passed through a conventional sorbent cartridge and reconstituted with potassium, calcium, magnesium and glucose. The chemical composition of the regenerated dialysate was similar to that of a commercially available peritoneal dialysate (Table 2) with two notable improvements. The regenerated dialysate contained bicarbonate as an anion and had a more physiological pH of 6.5–7.0—properties akin to second-generation peritoneal dialysis solutions such as the Physioneal (Baxter Health Care) [22]. With continuous cycles of regeneration, the lactate anion can be completely replaced by bicarbonate, with an anticipated further elevation in pH towards 7.4.
In addition to regenerating the ultrafiltrate, AWAK is also designed and constructed to regenerate the proteins in the spent peritoneal dialysate, thereby producing an autologous protein-containing peritoneal dialysate. This opens up the possibility of removing protein-bound uremic toxins and the treatment of intoxications from drugs that are highly protein-bound, e.g., digoxin and salicylates. In children with salicylate intoxication, three exchanges of peritoneal dialysate containing 5% albumin removed 574 mg of salicylate in 9 h. Over the same period of time, only 128 mg of salicylate were excreted by the kidneys [23].
We have demonstrated that peritoneal proteins concentrated into a 6% solution bind digoxin, carbamazipine or theophylline, in a manner similar to commercially available albumin preparations (diluted down to 6%) and that this binding capacity was not affected by a sorbent-regenerative protocol, consisting of sequential shaking with zirconium phosphate, hydrated zirconium oxide and activated carbon [24]. The composition of the peritoneal proteins is qualitatively identical to that in the serum proteins (see below and Fig. 4) and can therefore bind ligands not bound by albumin. Aluminum, for example, is bound by peritoneal proteins, but not by albumin (Fig. 3, before [25]). This protein-bound aluminum can be extracted by shaking with hydrated zirconium oxide and the regenerated peritoneal proteins were able to bind aluminum again, with no loss of activity (Fig. 3, after). On the other hand, albumin treated in a similar fashion continued to exhibit no aluminum-binding capacity.
Percent of aluminum that is protein-bound in peritoneal dialysate containing 6% peritoneal proteins (open bars) or 6% commercially available human albumin (filled bars). Seventy-one percent of aluminum was bound by peritoneal proteins before treatment with regenerative sorbents, and this capacity remained the same (75%) after treatment with sorbents. Albumin does not bind aluminum either before and after identical sorbent-regenerative process
We have also demonstrated that with filter–sterilization, the regenerated dialysate is rendered culture negative and pyrogen free, and can be infused into patients [26]. Peterson and associates have reported that the carbon in the purification filter, the first layer in the early generations of REDY® sorbent cartridges, removed bacteria and bacterial endotoxins from spent dialysate [27]. In a water purification method using a combination of alumina and zirconia, Levy claimed the advantage of “reductions in the level of bacterial contamination, particularly contamination by coliform and pseudomonal bacteria” [28]. Others have demonstrated the removal of pyrogenic lipopolysaccharides using colloidal zirconia adsorbents [29]. The bacteria-removing capability of the sorbent cartridge is also suggested by the observation that in unsterilized REDY cartridges, bacteria grew in different layers of the cartridge with decreasing frequency from the bottom layer (urease, where contamination was, most likely, originated) upwards [30]. Using sterilized REDY® sorbent cartridges coupled with sterilizing filters, ultrafiltrate in hemofiltration has been successfully regenerated for direct infusion back into patients [31, 32]. The continuous removal of bacteria and pyrogens by sterile sorbent assembly and sterilizing filters (Fig. 2), and the round-the-clock dialysate exchanges and the use of contamination-proof connectology have the potential of reducing infectious and pyrogenic complications in patients treated with AWAK.
AWAK: potential advantages (Table 3)
“Bloodless” and “waterless”
A peritoneal dialysis-based AWAK has the advantage of requiring no extracorporeal blood circulation and is therefore “bloodless.” In addition, the membrane involved is autologous (the patient’s own peritoneum), rather than an artificial, non-self membrane or surface. Since the spent dialysate is continuously regenerated and reused in perpetuity, AWAK is also “waterless.” This dispenses with the need for disposing large quantities of potentially hazardous spent dialysate and is also anticipated to reduce the amount of other disposables. Future development will include the regeneration and reuse of the spent sorbent assemblies.
A marked increase in small solute toxin clearance and the maintenance of a steady-state metabolic and fluid regulation
The clearance of water-soluble metabolic wastes, e.g., urea, is directly related to the peritoneal dialysate exchange rate (see Fig. 2 in [15]). In the current inflow–outflow practice of peritoneal dialysis, the strategy for increasing the daily amount of fresh dialysate circulating through the peritoneal cavity consists of increasing either the volume of each exchange or the number of exchanges in chronic ambulatory peritoneal dialysis (CAPD). Increasing the volume of each exchange (and therefore the dwell volume) can cause abdominal distention, back-pain and hernias. The chore of more frequent exchanges in CAPD can be ameliorated by transferring patients to automated peritoneal dialysis (APD) using machine-operated exchanges. However, often a less than optimal amount of dialysate is used for the purpose of cost control. AWAK, through continuous regeneration of spent dialysate, can provide relatively large quantities of fresh dialysate round-the-clock. A flow rate of 4 l/h or 96 l/day (has the potential of going up to 24 l/h [20]) would represent an 8- to 12-fold increase over the current dialysate exchange rate of 8–12 l per 24 h. Thus, blood urea is expected to be maintained at stable and close to normal levels. At a relatively high level of dialysate flow rate, it is also anticipated that a much smaller dwell-volume (reserve volume, in the case of tidal peritoneal dialysis) would be sufficient, e.g., 0.5–1.5 l, in place of the conventional 2–3 l.
The anticipated glucose-sparing effect by the oncotic pressure of the regenerated and concentrated peritoneal proteins in the dialysate (see below) and the round-the-clock dialysate exchanges may facilitate the regulation of fluid removal even in the high transporters. Fluid “excretion” into the bladder reservoir (Fig. 2) can be continuous, intermittent or otherwise programmed. Net ultrafiltration from the patient can be regulated by the addition of glucose from the enrichment motif (Fig. 2) into the regenerated dialysate, and its amount can be adjusted to mediate “diuresis” in fluid over-loaded patients, maintenance of fluid balance in euvolemic patients and “anuria” in hypovlemic patients. Net exchange between the vascular/interstitial fluid and peritoneal fluid compartments would, of course, depend upon a multiplicity of factors, including the relative osmotic and oncotic pressures of the two compartments and the permeability characteristics of the patient’s peritoneum membrane.
The maintenance of a steady-state metabolic and biochemical control and the ability to regulate fluid balance on a continuous basis would reduce or eliminate the “shocks” that characterize the current dialytic modalities [33]. The anticipated greater efficiency in water-soluble, small molecular-weight solute clearance and fluid regulation, in combination with the potential of removing protein-bound and middle molecule uremic toxins, may reduce or eliminate the need for phosphate-binders, erythropoietin and medications for the management of hypertension.
Potential advantages of an aulogous protein-containing dialysate
The recovery of proteins in the regenerated dialysate is expected to reduce or eliminate protein loss, a major disadvantage in current peritoneal dialysis practice. Since proteins are the physiological colloidal oncotic agents that trans-locates fluid into, and retains it in, the vascular system, the protein-containing dialysate generated by AWAK may exert a glucose-sparing effect in the regulation of ultrafiltration. Icodextrin (Extraneal™), a recent advance in augmenting ultrafiltration in peritoneal dialysis, also exerts its effect through a colloidal oncotic pressure [34]. Its use is recommended at one exchange per day. The transperitoneally absorbed icodextrin is metabolized by alpha amylase into oligosaccharides, including maltose, maltotriose, maltotetraose, and eventually glucose. Following a 12-h dwell time, a 150 g of icodextrin (2 l) led to a median plasma peak level of 2.2 g/l (icodextrin plus its metabolites), returning to baseline levels in approximately 1 week (Prod Info Extraneal™, 2002b—Product Information: Extraneal™, icodextrin. Baxter Healthcare Corp., Deerfield, IL, 2002b). Skin hypersensitivity reactions, including generalized rash and exfoliative and psoriasiform eruptions, have been reported in 2.5% of peritoneal dialysis patients using icodextrin solutions [35]. Icodextrin-associated sterile peritonitis is another reported complication that was attributed to peptidoglycan content in the solution. However, the complication is still reported in patients treated with icodextrin solution considered to contain “safe” levels of this agent [36]. Since the regenerated proteins in AWAK are autologous in origin, it can be used on a continuous basis and are not expected to cause sensitizing/immunological reactions. Protein-containing dialysate has an additional theoretical advantage. It has been reported that the longevity of human peritoneal mesothelial cells cultured in 4.25% glucose peritoneal dialysis fluid could be extended by the maintenance of physiological pH, and further augmented by the addition of albumin [37].
As mentioned earlier, the efficacy of albumin-added peritoneal dialysate in salicylate removal has been demonstrated in both experimental studies [38] and in children with salicylate intoxication [23]. More recently, the same principle has been used in the molecular adsorbent recirculation system (MARS) for the removal of albumin-bound toxins in liver failure [39]. In current peritoneal dialysis practice, the clearance of protein-bound toxins, e.g., p-cresol, is mainly dependent on the residual renal function [40]. The possibility that AWAK may remove such toxins, thereby providing a form of “tubular” secretory function of the native kidney, would be expected to be of particular importance in peritoneal dialysis patients who have declining or who have lost all residual renal function.
It is important to point out that AWAK regenerates a combination of autologous proteins rather than albumin only. Figure 4 shows that the proteins in the spent peritoneal dialysate are qualitatively identical to that in the serum. As pointed out earlier, the advantage of a protein combination over albumin-only dialysate is the ability of the former to bind aluminum (Fig. 3) and possibly other toxic agents. In addition to salicylate poisoning, the protein-containing dialysate of AWAK has the potential of removing other protein-bound poisons, administered inadvertently, e.g., amanita phalloides (mushroom) poisoning [41], or intentionally, e.g., sarin poisoning [42] or in chemical warfare. Under such acute circumstances, the initial addition of commercial albumin to the peritoneal dialysate would be required until autologous peritoneal protein concentrations are built up with repeated cycles of regeneration (see below).
Figure 4 shows the proportionate distribution of peritoneal proteins in the spent dialysate is qualitatively similar to those in the serum, including a monoclonal spike (arrows), when present. It is thus possible to selectively remove such undesirable macromolecules from the spent dialysate prior to recycling the regenerated dialysate back into the peritoneal cavity. This form of continuous, intermittent or otherwise programmed “dialysate-pheresis” can remove pathogenetic macromolecules, e.g., immunoglobulins, autoantibodies, lipoproteins and immune complexes.
Our primary objective in regenerating and recycling the peritoneal proteins is to ameliorate or eliminate protein loss. Other potential advantages discussed above will depend on a number of currently undefined factors, e.g., the protein concentrations that can be attained, when dialysate is continuously regenerated and recycled.
Comprehensive removal of uremic toxins
The much higher efficiency of AWAK in the clearance of low molecular-weight uremic toxins and its possible potential in clearing protein-bound toxins have been addressed. The middle molecules, of which 22 have been reported with MW ranging between 555 D (methionine-enkephalin) and 32,000 D (interlukin-1β), are mainly peptides and low molecular-weight proteins. AWAK may selectively remove these molecules directly by “dialysate-pheresis” or by the use of customized sorbents. Activated carbon and a host of novel sorbents, currently used mainly in blood- or plasma-contacting devices [43, 44], can be used with greater safety in dialysate-contacting AWAK.
The multifunctional enrichment motif
The main function of the enrichment motif, as mentioned earlier, is to re-constitute the regenerated dialysate with potassium, calcium, magnesium and glucose. These cations in the spent dialysate are completely removed by the sorbent assembly. They are then added back to the regenerated dialysate, each at a concentration prescribed by the managing physician. By manipulating the concentration in the regenerated dialysate, it is possible to bring about a negative, neutral or positive balance of a given cation.
The enrichment motif can be programmed to add dry and sterile glucose to the regenerated dialysate on a “need-basis’ for regulating ultrafiltration. The elimination of the need for heat-sterilization and storage of glucose in solution is expected to minimize the generation of advanced glycation end products [45]. As mentioned earlier, the glucose requirement for ultrafiltration may also be reduced by the continuous presence in the dialysate of oncotic pressure-generating proteins.
The enrichment motif can also serve as a convenient route for the administration of nutrients, micronutrients, vitamins and other beneficial supplements. AWAK also has the potential to function as an artificial gut providing continuous or programmed nutritional support in patients, in whom complete gut rest is a desired therapeutic strategy.
Thus, like the natural kidney, AWAK not only removes uremic toxins and other noxious agents, but it also adds beneficial agents. Along this line, AWAK can function as artificial glands for hormone “secretion.” For example, in conjunction with a peritoneal fluid glucose monitor calibrated to reflect blood/interstitial fluid glucose levels, insulin administration can be programmed in a physiological feed-back-loop fashion. AWAK can also be programmed to deliver, painlessly, other hormones. Although infrequently practiced, the intraperitoneal route is an effective mode for administering erythropoietin [46]. Adsorption of erythropoietin (and recombinant human growth hormone) to dialysis bags and tubing is minimal, <7% [47]. Intraperitoneal administration of therapeutic agents is particularly favored in children in whom subcutaneous administration is frightening and distressing [48]. In peritoneal dialysis patients non-compliance rates in self-administration of subcutaneous erythropoietin in adults ranged between 35 and 55%, while that for subcutaneous recombinant human growth hormone administration in children ranged between 50 and 91% [48].
Examples of other potential applications for the enrichment motif include extended and programmed treatment of chronic sepsis and, possibly, neoplasm.
Automation and dialysis-on-the-go
Automation and dialysis-on-the-go would achieve our major objective of allowing ESRD patients the freedom to pursue normal living activities, unencumbered by restrictions and chores demanded by the current dialysis treatments. We anticipate, once established, a patient needs only to be seen at monthly intervals, and possibly at longer intervals with time, as patient gains expertise in the management of his/her AWAK. This 24/7 mode of treatment is expected to further enhance the known benefits of “frequent dialysis” and is likely to improve dialytic mortality and morbidity rates. AWAK is the ultimate response to the exhortation for “longer, gentler dialysis sessions” [33].
AWAK may lead to cost reductions. Healthy and fully rehabilitated patients will not only reduce hospitalizations and needs for costly mediations, but also convert tax-consumers to tax generators. Unlike hemodialysis, AWAK eliminates the need for the purchase, construction and maintenance of physical facilities and equipment and is expected to result in a marked reduction in professional personnel. Compare to the current peritoneal dialysis practice, AWAK requires relatively little storage space for supplies. The operative simplicity, the anticipated minimal demand for professional intervention and the absence of requirement for water are qualities that can make AWAK a suitable device for the management of large scale disasters (natural or intentional), e.g., earthquake, war or sabotage.
AWAK: potential challenges (Table 4) and solutions
Long-term use of zoconium-based sorbent system
Zirconium (Zr) is widely distributed in nature and is found in all biological systems, frequently in an appreciable amount [49, 50]. It exhibits most of the characteristics of an essential trace metal [50]. Experimental and clinical studies support the general consensus that Zr compounds are biocompatible and exhibit low toxicity [49–52]. Decades of wide spread and increasing use of Zr compounds in medical practice have so far not been associated with clear evidence for Zr toxicities. Examples for successful medical applications include Zr-containing deodorant sticks, aerosol antiperspirants and poison-oak lotions [53], as well as life-long, internal placement of Zr-containing implants in dental restorative practice [54], in total knee [55] and hip [56] replacement, and in middle-ear ossicular chain reconstruction surgery [57]. Sorbent hemodialysis, using Zr-based hemodialysate regenerating cartridges, has been in use for the treatment of acute renal failure and end-stage renal failure patients since 1973 [20]. The amount of Zr translocated into a patient during a 4-h sorbent-based hemodialysis treatment has been estimated to range from 2.5 to 8.2 μmoles, or a maximum amount of 0.76 mg [58]. This is a fraction of the estimated daily Zr intake of 4.15 mg in normal subjects [50]. Available evidence suggests normal Zr excretion is kidney-independent and is accomplished through the hepatic-biliary pathway. Thus, the body has a relatively large margin of safety in maintaining zirconium balance. Nevertheless, we intend to vigilantly monitor AWAK treatment for possible adverse reactions from zirconium exposure. We are also working towards a more secure anchorage of the zirconium compounds within our newly designed and engineered sorbent assembly.
Distraction of a wearable device
Once the convenience and the efficiency of the AWAK are taken for granted, patients are likely to focus on the audio- and visual-intrusiveness of the device and the need to carry a predicted weight of about 4 pounds. These disadvantages are expected to resolve with the development of progressively newer models. The high efficiency of the device will allow temporary interruption in treatment for special situations when the device would be considered intrusive or inconvenient. During the sleep hours, the patient can “hook” on to a heavier, noise-proof, bedside system.
Need for interval replacement of components
Components that require replacement include the sorbent assembly, the enrichment motif, the bladder reservoir and batteries. The sorbent cartridge needs to be replaced every 4–8 h (depending on the weight a patient is comfortable carrying); the longer functioning units weigh more. The sorbent assembly and the enrichment motif can be replaced as a single unit. The bladder reservoir can be replaced at longer intervals, but requires emptying when full. Possession of more than one battery pack will be recommended. If only one battery pack is purchased, it can be recharged during the sleep hours, while the AWAK is powered through wall-sockets.
Peritoneal membrane dysfunction
The patient may contract infection of the peritoneal cavity, and the peritoneal membrane may become dysfunctional or non-functional, temporarily or permanently. Factors that may reduce infectious complications in the AWAK have been discussed earlier. The physiological pH and the presence of bicarbonate (in place of lactate or acetate) are known to improve the preservation of the function and the integrity of the peritoneal membrane. High-transporting peritoneum is the major contemporary obstacle to maintaining patients on peritoneal dialysis. AWAK with dialysate recycling at a relatively high flow rate and the potential of protein-mediated oncotic pressure may improve the management of these patients. As mentioned earlier the capability of adding fresh glucose into the regenerated dialysate on a “need-basis” for immediate use without storage will contribute to minimize the generation of glucose degradation products and their deleterious effects on the peritoneum.
AWAK: the preferred form of treatment modality for ESRD patients?
The advantages of the peritoneal-based AWAK may make it a preferred form of dialytic therapy. It also has the potential of becoming the preferred form of ESRD therapy. Both the number of patients on the waiting list for kidney transplantation and the wait time for deceased donor kidneys have continued to increase [59]. AWAK, with its anticipated improvements in uremic and fluid management, may provide the quality-of-life equivalent to an average functioning kidney transplant. However, in contrast to kidney transplantation, patients treated with AWAK do not need anti-rejection treatment and additional medications to ameliorate the side effects of these agents. Moreover, most dialysis patients are older in age—55.5% of the US dialysis patients on 31 December 2004 were over the age of 60 years [59] (Table D.6)—and are likely to prefer non-surgical therapies. Since the continued expansion of the transplant waiting list and the increase in wait time for deceased donor kidneys disproportionately affect the older patients [59], AWAK can potentially ameliorate the escalating pressure of the shortage in kidney donors.
References
Vanholder R, De Smet R, Glorieux G, et al. Review on uremic toxins: classification, concentration, and interindividual variability. Kidney Int. 2003;63(5):1934–43.
Gura V, Beizai M, Ezon C, Polaschegg HD. Continuous renal replacement therapy for end-stage renal disease. The wearable artificial kidney (WAK). Contrib Nephrol. 2005;149:325–33.
Nissenson AR, Ronco C, Pergamit G, Edelstein M, Watts R. The human nephron filter: toward a continuously functioning, implantable artificial nephron system. Blood Purif. 2005;23(4):269–74.
Saito A, Aung T, Sekiguchi K, et al. Present status and perspectives of bioartificial kidneys. J Artif Organs. 2006;9(3):130–5.
Lande AJ, Roberts M, Pecker EA. In search of a 24 hrs/day, 7 days/week wearable hemodialyzer. Trans Am Soc Artif Intern Organs. 1977;23:185–90.
Yamamoto K, Hiwatari M, Kohori F, Sakai K, Fukuda M, Hiyoshi T. Membrane fouling and dialysate flow pattern in an internal filtration-enhancing dialyzer. J Artif Organs. 2005;8(3):198–205.
Murisasco A, Reynier JP, Ragon A, et al. Continuous arterio-venous hemofiltration in a wearable device to treat end-stage renal disease. ASAIO Trans. 1986;32(1):567–71.
Neff MS, Sadjadi S, Slifkin R. A wearable artificial glorerulus. ASAIO Trans. 1979;25:71–3.
Lee DBN, Roberts M. A peritoneal-based wearable dialysis system. Continuous dialysis using a protein-containing dialysate In: Agarwal S, ed. Scientific Proceedings, South-Asian Nephrology Congress at New Millennium and International CME-2000. New Delhi, 2000:94–9.
Roberts M, Lee DBN. A proposed peritoneal-based wearable artificial kidney. Home Hemodialysis Int. 1999;3:65–7.
Roberts M, Lee DBN. Wearable artificial kidneys. A peritoneal-dialysis approach. Dialysis and Transplantation. 2006;36:780–2.
Roberts M, Niu PC, Lee DBN. Regeneration of peritoneal dialysate (PD): a step towards a continuous wearable artificial kidney (CWAK). J Am Soc Nephrol. 1991;2(3):367.
Vychytil A, Horl WH. The role of tidal peritoneal dialysis in modern practice: A European perspective. Kidney Int Suppl. 2006(103):S96–103.
Fernando SK, Finkelstein FO. Tidal PD: its role in the current practice of peritoneal dialysis. Kidney Int Suppl 2006(103):S91–5.
Roberts M, Ash SR, Lee DB. Innovative peritoneal dialysis: flow-thru and dialysate regeneration. ASAIO J. 1999;45(5):372–8.
Villarroel F. Kinetics of intermittent and continuous peritoneal dialysis. J Dial. 1977;1(4):333–47.
Lange K, Treser G, Mangalat J. Automatic continuous high flow rate peritoneal dialysis. Arch Klin Med. 1968;214(3):201–6.
Lee DB, Brown DL, Baker LR, Littlejohns DW, Roberts PD. Haematological complications of chlorate poisoning. Br Med J. 1970;2(5700):31–2.
Blumenkrantz MJ, Gordon A, Roberts M, Lewin AJ, Pecker EA, Moran JK, Coburn JW, Maxwell MH. Applications of the Redy sorbent system to hemodialysis and peritoneal dialysis. Artif Organs. 1979;3(3):230–6.
Hansen S. Sorbent dialysis in the third millennium. Nephrol News Issues 2006;20(1):43–5.
Capparelli AW, Roberts M, Lee DBN. Towards a wearable artificial kidney for continuous dialysis: ex-vivo sorbent regeneration of filtered peritoneal dialysate during intermittent peritoneal dialysis. J Am Soc Nephr. 1993;4:399A.
Hoff CM. In vitro biocompatibility performance of Physioneal. Kidney Int Suppl. 2003(88):S57–74.
Etteldorf JN, Dobbins WT, Summitt RL, Rainwater WT, Fischer RL. Intermittent peritoneal dialysis using 5 per cent albumin in the treatment of salicylate intoxication in children. J Pediatr. 1961;58:226–36.
Roberts M, Dinovo EC, Yanagawa N, Lee DBN. Can peritoneal proteins be regenerated and reused for binding toxins? J Am Soc Nephrol. 1999;10:228A.
Roberts M, Paul W, Yanagawa N, Corry DB, Lee DBN. Peritoneal dialysis of protein-bound toxins: feasibility of regeneration of spent dialysis proteins. Perit Dial Int. 1999;19(Suppl 1):S22.
Roberts M, Capparelli AW, Wong C, Lee DBN. Development of a wearable artificial kidney based upon sorbent regeneration of peritoneal dialysate. Perit Dial Int. 1995;15(Suppl 4):S88.
Petersen NJ, Carson LA, Favero MS, Marshall JH Jr, Aguero SM. Removal of bacteria and bacterial endotoxin from dialysis fluids by the media in a sorbent cartridge. Trans Am Soc Artif Intern Organs. 1979;25:402–3.
Levy E. Method of reducing contaminants in drinking water In: USPaT Office, ed. United States Patent Application Publication. USA, 2003.
Karl DW, Magnusson JC, Carr PW, Flickinger MC. Preliminary assessment of removal of pyrogenic lipopolysaccharides with colloidal zirconia adsorbents. Enzyme Microb Technol. 1991;13(9):708–15.
Sonderstrup J. On bacteriological problems in the REDY dialysis system. Scand J Urol Nephrol 1976(30 Suppl):19–22.
Murisasco A, Baz M, Boobes Y, Bertocchio P, el Mehdi M, Durand C, Reynier JP, Ragon A. A continuous hemofiltration system using sorbents for hemofiltrate regeneration. Clin Nephrol. 1986;26(Suppl 1):S53–7.
Shapiro WB, Schilb TP, Porush JG. Sorbent recycling of ultrafiltrate in man–a 45-week crossover study. Clin Nephrol. 1986;26(Suppl 1):S47–52.
Twardowski ZJ. Short, thrice-weekly hemodialysis is inadequate regardless of small molecule clearance. Int J Artif Organs. 2004;27(6):452–66.
Frampton JE, Plosker GL. Icodextrin: a review of its use in peritoneal dialysis. Drugs. 2003;63(19):2079–105.
Garcia-Lopez E, Lindholm B, Tranaeus A. Biocompatibility of new peritoneal dialysis solutions: clinical experience. Perit Dial Int. 2000;20(Suppl 5):S48–56.
Rozenberg R, Magen E, Weissgarten J, Korzets Z. Icodextrin-induced sterile peritonitis: the Israeli experience. Perit Dial Int. 2006;26(3):402–5.
Lai KN, Ho SK, Leung J, Tang SC, Chan TM, Li FK. Increased survival of mesothelial cells from the peritoneum in peritoneal dialysis fluid. Cell Biol Int. 2001;25(5):445–50.
Etteldorf JN, Montalvo JM, Kaplan S, Sheffield JA. Intermittent peritoneal dialysis in the treatment of experimental salicylate intoxication. J Pediatr. 1960;56:1–10.
Chiu A, Fan ST. MARS in the treatment of liver failure: controversies and evidence. Int J Artif Organs. 2006;29(7):660–7.
Bammens B, Evenepoel P, Verbeke K, Vanrenterghem Y. Removal of middle molecules and protein-bound solutes by peritoneal dialysis and relation with uremic symptoms. Kidney Int. 2003;64(6):2238–43.
Faybik P, Hetz H, Baker A, Bittermann C, Berlakovich G, Werba A, Krenn CG, Steltzer H. Extracorporeal albumin dialysis in patients with Amanita phalloides poisoning. Liver Int. 2003;23(Suppl 3):28–33.
Yokoyama K, Ogura Y, Kishimoto M, et al. Blood purification for severe sarin poisoning after the Tokyo subway attack. Jama. 1995;274(5):379.
Ash SR, Sullivan TA, Carr DJ. Sorbent suspensions vs. sorbent columns for extracorporeal detoxification in hepatic failure. Ther Apher Dial. 2006;10(2):145–53.
Winchester JF, Amerling R, Harbord N, Capponi V, Ronco C. The potential application of sorbents in peritoneal dialysis. Contrib Nephrol. 2006;150:336–43.
Tauer A, Zhang X, Schaub TP, Zimmeck T, Niwa T, Passlick-Deetjen J, Pischetsrieder M. Formation of advanced glycation end products during CAPD. Am J Kidney Dis. 2003;41(3 Suppl 1):S57–60.
Reddingius RE, de Boer AW, Schroder CH, Willems JL, Monnens LA. Increase of the bioavailability of intraperitoneal erythropoietin in children on peritoneal dialysis by administration in small dialysis bags. Perit Dial Int. 1997;17(5):467–70.
Schroder CH, Swinkels LM, Reddingius RE, Sweep FG, Willems HL, Monnens LA. Adsorption of erythropoietin and growth hormone to peritoneal dialysis bags and tubing. Perit Dial Int. 2001;21(1):90–2.
Schroder CH. The management of anemia in pediatric peritoneal dialysis patients. Guidelines by an ad hoc European committee. Pediatr Nephrol. 2003;18(8):805–9.
Ghosh S, Sharma A, Talukder G. Zirconium. An abnormal trace element in biology. Biol Trace Elem Res. 1992;35(3):247–71.
Schroeder HA, Balassa JJ. Abnormal trace metals in man: zirconium. J Chronic Dis. 1966;19(5):573–86.
Piconi C, Maccauro G. Zirconia as a ceramic biomaterial. Biomaterials. 1999;20(1):1–25.
Sollazzo V, Palmieri A, Pezzetti F, Bignozzi CA, Argazzi R, Massari L, Brunelli G, Carinci F. Genetic effect of zirconium oxide coating on osteoblast-like cells. J Biomed Mater Res B Appl Biomater 2007.
Laden K. Introduction ahd history of antiperspirants and deodorants. In: Laden K, Felger CB, eds. Antiperspirants and deodorants. New York: Marcel Decker, 1988:1–13.
Chang PP, Henegbarth EA, Lang LA. Maxillary zirconia implant fixed partial dentures opposing an acrylic resin implant fixed complete denture: a two-year clinical report. J Prosthet Dent. 2007;97(6):321–30.
Tsukamoto R, Chen S, Asano T, Ogino M, Shoji H, Nakamura T, Clarke IC. Improved wear performance with crosslinked UHMWPE and zirconia implants in knee simulation. Acta Orthop. 2006;77(3):505–11.
Lappalainen R, Santavirta SS. Potential of coatings in total hip replacement. Clin Orthop Relat Res. 2005(430):72–9.
Schadel A, Thun G, Stork L, Metzler R. Immunodiffusion and immunohistochemical investigations on the reactivity of oxide ceramic middle-ear implants. ORL J Otorhinolaryngol Relat Spec. 1993;55(4):216–21.
Odell RA. Sorbent dialysis. In: Nissenson AR, Fine RN, Gentile DE, eds. Clinical dialysis, 2nd edition. Connecticut: Appleton and Lange, 1990:712–9.
U.S. Renal Data System, USRDS 2006 Annual Data Report: Atlas of End-Stage Renal Disease in the United States. Bethesda, MD: National Institutes of Health, National Institute of Diabetes and Digestive and Kidney Diseases.
Author information
Authors and Affiliations
Corresponding author
About this article
Cite this article
Lee, D.B.N., Roberts, M. A peritoneal-based automated wearable artificial kidney. Clin Exp Nephrol 12, 171–180 (2008). https://doi.org/10.1007/s10157-008-0050-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10157-008-0050-9