Abstract
The endotoxin activity assay (EAA) is a FDA-approved blood endotoxin assay that is reported as a useful tool for the diagnosis of gram-negative bacterial infection. However, discrepancies between the results of the EAA and those of the limulus amebocyte lysate (LAL) assay have been reported. Thus, we verified these methods. Blood was incubated with anti-endotoxin antibody, the resultant polymorphonuclear activation to produce oxidants was measured and the EAA level calculated. As a reference endotoxin assay, we used an endotoxin-specific LAL assay. Significant increases in plasma LAL assay levels were observed only in patients with sepsis caused by gram-negative bacterial infections, whereas higher EAA levels were observed in almost all the sepsis cases and the SIRS cases, especially those with acute pancreatitis. Graded amounts of LPS (1–10,000 pg/ml) were spiked into normal blood to obtain dose–response curves: a good dose–response curve, from 1 to 1,000 pg/ml, was obtained for the LAL assay. A good dose–response curve was barely obtained for the EAA; the lowest detection limit seemed to be 1,000 pg/ml. Addition of methylprednisolone decreased the EAA levels. Interleukin-8 (IL-8) induced elevation in EAA levels when IL-8 was added to volunteers’ blood samples. Overall, the EAA kit could not measure clinically relevant doses of endotoxin. Because IL-8 induced an increase in EAA level, it is suggested that the EAA level reflects the primed state of polymorphonuclear leukocytes.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
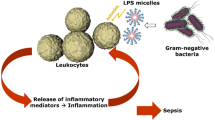
Endotoxins are lipopolysaccharides (LPS) and cell-wall constituents of gram-negative bacilli. When liberated into the body from lysed bacteria in sepsis situations, endotoxins act upon macrophages to induce the release of inflammatory mediators, which can in turn give rise to endotoxin shock and multiple organ failure. The role of endotoxins in sepsis has long been a subject of discussion and debate, and it has been a common practice to quantify the plasma endotoxin level using the endotoxin-specific limulus amebocyte lysate (LAL) assay in Japan. This test contributed to the establishment of the concept that endotoxemia is only associated with bacterial infections [1–3]. As the β-d-glucan or glucan-like activity [4] reacts in the factor G-mediated cascade of LAL, a glucan-specific limulus test has been developed in Japan for the diagnosis of deep fungal infection [5], and this test was recently approved by the US FDA [6].
As an endotoxin-specific LAL assay, subpicograms of plasma endotoxin can now be measured using the national health insurance-covered turbidimetric kinetic assay method [7, 8]; this assay was used in the present study and is more sensitive than the previously used synthetic chromogenic substrate assay method [9]. The structural requirements of the lipid A portion of LPS in the activation of clotting enzyme from the amebocyte lysate were investigated in detail by Takada et al. [10], providing theoretical grounds for the ability of the limulus test to truly quantify endotoxin, and the precise structure of lipid A, which induces the activation of the limulus cascade, was elucidated.
At our Advanced Critical Care and Emergency Center, the determination of plasma endotoxin levels is usually performed using the turbidimetric kinetic assay. We have also attempted to use the endotoxin activity assay (EAA) to secure important information for diagnosis and treatment. The EAA is a chemiluminescent immunodiagnostic test for the detection of endotoxin in the plasma [11, 12]. This test has many steps, i.e., the formation of a complex of LPS and anti-LPS murine IgM antibody, complement activation, and the adherence of C3b to CR1 and CR3 on the surface of polymorphonuclear leukocytes (PMN) to prim the PMN. The primed PMN are then activated by complement-opsonized zymosan to release oxidants.
Recently, discrepancies between the results of the EAA and those of the LAL assay have been reported [13, 14]. We previously experienced a case with a low EAA value in a patient who had been treated with a steroid [15]. In this study, we examined the possibility that the EAA results may reflect a factor other than the blood endotoxin level.
Patients and methods
Patients
Sepsis was diagnosed in accordance with the diagnostic criteria proposed by the Members of the American College of Chest Physicians/Society of Critical Care Medicine Consensus Committee [16]. The study population consisted of 44 patients who were admitted emergently or with newly developed sepsis at this institution between April 2008 and November 2009 (Table 1). The chief physician for the 44 cases treated at this center was the first author of this paper, and all these cases were enrolled in the present study. All the specimens that were tested had been collected at the time of diagnosis. Before collecting the blood samples from each patient, the informed consent of the patient’s family and the approval of the ethics committee of the Iwate Medical University were obtained (Approval No. H19-1). Among the patients who were diagnosed as having an infection, those failing to meet the diagnostic criteria for sepsis were excluded from this study.
EAA
The EAA (Spectral Diagnostics, Toronto, Canada) was performed according to the manufacturer’s instructions (Fig. 1). Each blood sample was collected in a sterile Vacutainer tube (BD Bioscience, San Jose, CA, USA) containing EDTA anti-coagulant. Five hundred milliliters of blood was then added to an aliquot tube (empty tube) and an LPS MAX tube. In the LPS-MAX tube, 2.3 ng of Escherichia coli O55:B5 LPS had been previously added, according to the manufacturer’s instructions. After incubation for 10 min at 37 °C, 40 ml blood from the aliquot tube was added to tube 1 and to tube 2, and 40 ml blood from the LPS-MAX tube was added to tube 3. Previously, lyophilized reagents containing luminol, complement-opsonized zymosan (in all the tubes), and anti-LPS monoclonal antibody (in tubes 2 and 3) were reconstituted with Hanks’ balanced salt solution (1 ml). The three tubes were incubated for 15 min at 37 °C with constant shaking; then, light emission was monitored using a temperature-controlled (37 °C) photon-counting luminometer (Berthold 953; Henry Troemner, Thorofare, NJ, USA) to detect oxidants produced by activated PMN. Tube 1 reflected the baseline neutrophil activation in the absence of exogenous immune complexes. Tube 2 contained a specific anti-LPS murine IgM antibody that primes neutrophil activity in proportion to the concentration of LPS in the blood. Finally, tube 3 contained specific anti-LPS murine IgM antibody and an excess of LPS, so that the chemiluminescence would reflect the maximum response of an individual patient’s sample. The EAA level was calculated using the formula shown in Fig. 1. The EAA levels were graded into three categories: low EAA level, <0.40; mid-EAA level, 0.40–0.59; high-EAA level, ≥0.60. The values of normal volunteers reportedly correspond to a low EAA level (<0.40) [12].
Illustrated procedure for endotoxin activity assay (EAA). Blood is collected into an EDTA-containing blood collection tube; 500 μl blood is poured into an aliquot tube and an LPS MAX tube, in which excess lipopolysaccharide (LPS) was added in advance. Tubes are incubated for 10 min, at 37 °C with shaking. Then, 40 μl blood in an aliquot tube is poured into tubes 1 and 2; 40 μl blood in the LPS MAX tube is poured into tube 3. An anti-LPS monoclonal antibody (tubes 2 and 3), complement-opsonized zymosan (tubes 1, 2, 3), and luminol (tubes 1, 2, 3) were added to these tubes previously and dissolved using a solvent (Hanks’ balanced salt solution). Tubes are then incubated for 15 min and photons counted using a luminometer. EAA level was calculated using the formula shown. All testing was done in duplicate; mean values were used in this study
LAL assay
The endotoxin-specific turbidimetric kinetic assay (Wako Pure Chemical Industries, Osaka, Japan), designed specifically for the detection of endotoxin by the addition of an excess amount of β-d-glucan, was used [7, 8]. Endotoxin-free tips (BioClean tips; Wako) were used to handle the samples. Heparinized blood was centrifuged in a countertop centrifuge at 3,000 rpm for at least 40 s to spin down the erythrocytes, and the resultant supernatant was used as platelet-rich plasma (PRP). The PRP was diluted tenfold with the pretreatment solution (0.02 % Triton X100 in water; Wako), then heated at 70 °C for 10 min followed by cooling on crushed ice to obtain the pretreated sample. This dilution and heating procedure inactivates the enhancing and inhibiting activities of the limulus assay, which are also factors relevant to the coagulation pathway in the plasma [17]. The LAL reagent (Endotoxin Single Test Wako; Wako) was dissolved in 200 μl of this pretreated sample and was used for the assay, which was conducted using a Toxinometer MT-5500 (Wako). The gelation time was defined as the length of time from the start of the assay until the dimming of the transmitted light to a point corresponding to an 8 % reduction. The concentration of endotoxin was calculated using a calibration curve constructed using standard LPS solutions (derived from E. coli O111:B4; Sigma-Aldrich). The maximum reaction time of this apparatus was set at 200 min, and the apparatus was capable of measuring about 0.04 pg/ml LPS. The minimum detection limit was dependent on the lot of the reagent. Because the endotoxin content of plasma diluted ten times was measured, the measurement limit of the plasma endotoxin was ultimately about 0.4 pg/ml. The cutoff value for endotoxemia was set at 1.1 pg/ml [2].
Endotoxin detection in the EAA test tubes
As an aliquot tube, tube 1, tube 2, and tube 3 must be endotoxin free; therefore, these tubes were tested for any trace of endotoxin. One milliliter of endotoxin-free water (<0.04 pg/ml) or endotoxin extracting solution (Wako) was added to each of these tubes, mixed in a vortex mixer, and assayed using the LAL assay. Endotoxin contamination was confirmed by adding polymyxin B (10 μg/ml) or anti-activated factor C monoclonal antibody (clone no. T8617A; Immunology Institute, Tokyo, Japan). Polymyxin B is a well-known inhibitor of LPS activities [18]. The monoclonal antibody was made using spleen cells from mice immunized with a complex of factor C and LPS (E. coli O111:B4) [19]. The antibody inhibits the limulus cascade reaction by binding with factor C. The limulus reagent was dissolved with polymyxin B or the monoclonal antibody, and the test samples were added to the mixture. The endotoxin levels were then measured using a Toxinometer. The final concentrations of polymyxin B and the antibody were 10 and 20 μg/ml, respectively.
Effect on EAA levels of adding polymyxin B to whole blood: Polymyxin B (Sigma-Aldrich) was added at a dose between 0.1 and 10,000 pg/ml to whole blood (previously incubated for 30 min) obtained from healthy subjects, and the blood was incubated for 30 min. The EAA level of the resultant mixtures was then compared with that of the control whole blood to explore the influence of polymyxin B on the EAA levels.
Preparation of dose–response curves for the two methods
Serially diluted LPS (E. coli O111, B4) were used to spike whole blood obtained from healthy subjects. An EAA was then performed, and the plasma endotoxin contents were also measured using the LAL assay.
Effect on EAA levels of adding a steroid to whole blood
Blood from healthy volunteers was incubated for 2 h at 37 °C in the presence or absence of methylprednisolone (Solu-Medrol; Pfizer), and the EAA levels of the resultant mixtures were measured.
Effect on EAA levels of adding interleukin-8 (IL-8) to whole blood: Human recombinant IL-8 (Wako) was added at doses of 4, 20, or 100 ng/ml to whole blood from healthy subjects, and the resultant mixture was incubated for up to 1 h. The EAA levels of the mixtures were compared with that of the control whole blood to explore the influence of IL-8 on the EAA levels.
Statistics
Any differences with P < 0.05 found during a statistical analysis of the data using the Student’s t test and Bonferroni test were considered significant.
Results
Comparison of LAL assay and EAA levels in patients with sepsis and those with SIRS
The EAA levels in the patients with sepsis were not significantly higher than those in the patients with systemic inflammatory response syndrome (SIRS) (Fig. 2). When the sepsis group was divided into three groups according to the causative pathogens, no significant differences in the levels were noted among the three groups. When the values were compared among the SIRS cases, the plasma EAA levels were significantly higher among the cases with acute pancreatitis and were lower among the cases with intensive burns and trauma. On the other hand, the LAL assay levels were significant higher only in the gram-negative infection group, compared with the other groups (Fig. 3). As expected based on the aforementioned data, no correlations between the EAA and LAL assay levels were found in the sepsis and SIRS groups (Fig. 4).
Box plot of EAA levels in sepsis group, systemic inflammatory response syndrome (SIRS) group, and non-SIRS group. Sepsis group was divided into three groups: gram-negative infections, gram-positive infections, and suspected sepsis cases (source of infection unknown). SIRS group was divided into four groups: acute pancreatitis, severe burns, trauma, and others. Asterisk indicates statistical significance (P < 0.05) between two groups (Bonferroni test)
Box plot of limulus amebocyte lysate (LAL) assay levels determined using the turbidimetric kinetic assay in sepsis, SIRS, and non-SIRS groups. Sepsis and SIRS groups were divided into groups as described for Fig. 2. Asterisk indicates statistical significance (P < 0.05) between two groups (Bonferroni test)
Endotoxin detection in the EAA test tubes
Endotoxin was detected in the three tubes included in the EAA kit that was tested. In the aliquot tube, the endotoxin level was less than the detection limit (<0.05 pg/ml). These tubes were evidently contaminated with endotoxin, as the endotoxin levels in the tubes were reduced by the addition of polymyxin B (Table 2). About 99 % of the limulus activity found in tube 2 was decreased by the addition of the anti-factor C monoclonal antibody to tube 2. Meanwhile, in a control experiment, almost 100 % of the limulus activity of 10 pg of LPS was inhibited by the addition of the antibody. Endotoxin was not detected (less than the detection limit, i.e., <0.05 pg/ml) in the blood collection tube (BD sterile Vacutainer tube containing EDTA anti-coagulant).
Preparation of dose–response curves
When LPS was used to spike a volunteer’s blood sample, the corresponding amounts of LPS (about 60–80 % of the limulus activity of added LPS) was recovered when the LAL assay was used, and a good correlation curve was obtained (Fig. 5). However, no such results were observed when the measurements were conducted using the EAA, and an EAA level that was significantly higher than the control level was only noted when as much as 1,000 pg/ml LPS was added (Fig. 6).
Dose–response curve for EAA using a whole blood sample spiked with LPS. Serially diluted LPS (1–10,000 pg/ml Escherichia coli O111, B4, Sigma, in 10 μl physiological saline) or physiological saline was spiked into 1 ml whole blood obtained from healthy subjects; EAA assay was soon performed. Three experiments with different blood samples used an EAA kit (lot no. 09EK005C). Mean ± SD is depicted
Dose–response curve for LAL assay using LAL assay levels for same blood samples as in experiment shown in Fig. 5. LAL assay levels in saline-spiked bloods were <0.4 pg/ml. Mean ± SD is depicted
Effect on EAA level of adding a steroid to whole blood
The EAA levels decreased noticeably following the addition of methylprednisolone (120 μg/ml) in the presence or absence of LPS (1,000 pg/ml) (Table 3). However, the LAL levels were not affected by the addition of methylprednisolone (data not shown).
Effect on EAA level of adding IL-8 to whole blood
IL-8 was added to whole blood samples from three volunteers and the samples were incubated for up to 1 h. The EAA levels were then examined. As shown in Fig. 7, the light emissions of tube 2, and tube 4, but not that of tube 1, tended to be increased by the addition of IL-8, and resultant EAA levels were elevated by the addition of IL-8 in a dose-dependent manner.
Effect of interleukin-8 (IL-8) on EAA level using blood samples from three volunteers. IL-8 or phosphate-buffered saline (PBS(−)) at 10 μl was added to 1 ml blood; mixture was vigorously mixed and incubated for 60 min and EAA was then performed in duplicate (EAA kit, lot no. 10EK0014L). Endotoxin content in 100 ng IL-8 solution was less than detection limit (<0.04 pg). Means (±SD) of light emission of tubes 1, 2, and 3 are depicted as circles, squares, and triangles, respectively (a). Mean EAA levels are shown in b. *P < 0.005 versus PBS(−) control (Student’s t test, two-tailed, paired). **P < 0.05 versus PBS(−) control (Student’s t test, one-tailed, paired)
Discussion
In this study, we verified whether the EAA truly measures the plasma endotoxin level. First, we compared the endotoxin levels determined using the LAL assay and the EAA in patients with sepsis or SIRS; we have found that the EAA levels were elevated in patients with sepsis or SIRS, especially those with pancreatitis (Fig. 2), although high LAL assay levels were only found in patients with gram-negative sepsis (Fig. 3). Therefore, no correlations between the EAA and LAL assay levels were seen for patients with sepsis or for those with SIRS (Fig. 4), as previously reported [13, 14].
Of note, the EAA level in a normal volunteer was as high as 0.4. We suspected that the high EAA level even in the normal volunteer might have been caused by endotoxin contamination in the tubes attached to the EAA kit. We detected as much as 30 pg endotoxin in the tubes (Table 2). The endotoxin contamination was confirmed using inhibitory experiments with polymyxin B and anti-factor C monoclonal antibody. Next, we investigated the influence of polymyxin B by adding it to tube 1 and to tube 2 before performing the EAA. As a result, polymyxin B scarcely decreased the EAA levels in the volunteer’s blood (data not shown). Thus, we concluded that endotoxin contamination did not influence the EAA levels even in the normal volunteer’s blood sample.
According to the original paper by Romaschin et al. [11] concerning the EAA, good dose–response curves for whole blood samples were obtained for doses of 20, 50, 100, 200, 400, and 800 pg/ml of LPS, and the significant reactivity level of LPS in the EAA seemed to be more than 20 pg/ml. Therefore, we confirmed the dose–response curve for the EAA after the addition of graded amounts of LPS to volunteers’ blood samples. Surprisingly, the curve unexpectedly differed from that described in the original paper [11]. In our result, the lowest detection limit was 1000 pg/ml in three volunteers’ blood sample (Fig. 6). The result was confirmed by another lot of kit (data not shown). We could not explain the discrepancy between the present results and those of the original paper, although the assay procedures were slightly different [11]. Regardless, the detection limit (20 pg/ml) of the original method may not be sufficient to measure endotoxin levels in the blood, because patients with plasma endotoxin content <20 pg/ml are occasionally encountered (Figs. 3, 4) [1–3, 15, 17]. As the detection limit of the EAA, which was used in the present study, seemed to be 1,000 pg/ml endotoxin, the amount of endotoxin contamination is unlikely to influence the EAA values.
In tube 2, anti-LPS monoclonal antibody and complement-opsonized zymosan were added, whereas only complement-opsonized zymosan was added to tube 1 according to the description in the instruction manual. If a human is carrying an antibody against mouse IgM protein, immune complex formation as a result of the human anti-mouse IgM antibody (HAMA-IgM) and the mouse IgM protein will also occur in tube 2. Humans have been reported to carry HAMA-IgM [20], and we also confirmed the presence of HAMA-IgM in human plasmas (data not shown). Thus, the EAA level may rise because of the presence of HAMA-IgM. Therefore, the presence of HAMA-IgM should be compensated for by adding murine IgM protein, which has no reactivity with human proteins and LPS, to tube 1.
The aforementioned data strongly suggest that the EAA does not reflect the endotoxin content in blood samples. The EAA has many steps, i.e., immune complex formation, complement activation, binding of the complement component to the PMN, priming of the PMN, and activation of the PMN. Other than immune complex formation, which of these steps has the largest influence on oxidant formation? These steps can be influenced by pharmacological treatments and the physiological states of patients. A clinical dose of methylprednisolone intensively reduced the EAA value (Table 3). Glucocorticoids are known to act on PMN to reduce oxidant production [21]. Thus, a factor that interferes with PMN activation suggested influencing the EAA level.
The levels of inflammatory cytokines, such as TNF-α, IL-6, and IL-8, are elevated in patients with sepsis [1, 22], and these cytokines are known to induce PMN to enter a primed state characterized by the enhanced responsiveness to subsequent stimuli [23]. Therefore, we investigated the effect of the addition of IL-8 on the EAA level. As shown in Fig. 7, the values of tube 2 and tube 3 were increased by the addition of IL-8 in a dose-dependent manner. The value of tube 1 was barely increased by the addition of IL-8, and the calculated EAA level was gradually increased by the addition of IL-8. The reason why IL-8 is capable of elevating the EAA level is likely the absence of complement-opsonized zymosan in tube 1. However, according to the instruction manual, complement-opsonized zymosan should be added to both tube 1 and tube 2. Anyway, obviously IL-8, but not endotoxin, induces an elevation in the EAA level. We also confirmed that TNF-α increased EAA level in volunteer’s blood (data not shown). Thus, the priming of PMN by inflammatory cytokines is a key process to enhance EAA level in patient with infections.
In this study, we reported relatively high EAA values in patients with acute pancreatitis, although the LAL assay levels were within the cutoff value (Figs. 2, 3). As enhanced PMN function and a high IL-8 level have been reported in patients with acute pancreatitis [24, 25], the high EAA level suggested to be associated with the priming of the PMN by IL-8. On the other hand, the EAA levels in patients with severe burns and trauma were relatively low upon admission to our emergency center. In these acute phases of injury, PMN function reported to be sporadically reduced [26, 27].
The EAA is an FDA-approved assay method for measuring blood endotoxin levels, and this assay system is reportedly used in the United States and Europe. However, we could not measure a clinically relevant amount of endotoxin in human blood by the EAA kit. It was suggested that the EAA kit is, rather, a method of measuring the degree of priming of PMN.
References
Endo S, Inada K, Inoue Y, Kuwata Y, Suzuki M, Yamashita H, et al. Two types of septic shock classified by the plasma levels of cytokines and endotoxin. Circ Shock. 1992;38:264–74.
Yaegashi Y, Inada K, Sato N, Kojika M, Endo S. Highly sensitive endotoxin assay for the diagnosis of sepsis. Jpn J Crit Care Endotoxemia. 2003;7:25–8 (in Japanese).
Kojika M, Sato N, Yaegashi Y, Suzuki Y, Suzuki K, Nakae H, et al. Endotoxin adsorption therapy for septic shock using polymyxin B-immobilized fibers (PMX): evaluation by high-sensitivity endotoxin assay and measurement of the cytokine production capacity. Ther Apher Dial. 2006;10:12–8.
Yajima Y, Fukuda I, Otsuki M, Suzuki H, Mori K, Goto Y. Non-septic endotoxemia in cirrhotic patients. Gastroenterol Jpn. 1989;24:262–9.
Obayashi T, Kawai T, Yoshida M, Mori T, Goto Hyasuoka A, et al. Plasma (1 → 3)-β-d-glucan measurement in diagnosis of invasive deep mycosis and fungal febrile episodes. Lancet. 1995;345:17–20.
Fungitell® Assay. Web site of Associates of Cape Cod. http://www.acciusa.com/clinical/fungitell/index.html.
Oishi H, Takaoka A, Hatayama Y. Automated limulus amebocyte lysate (LAL) test for endotoxin assay using a new Toxinometer ET-201. J Parenter Sci Technol. 1981;39:194–200.
Kambayashi J, Yokota M, Sakon M, et al. A novel endotoxin-specific assay by turbidimetry with Limulus amoebocyte lysate containing β-glucan. J Biochem Biophys Methods. 1991;22:93–100.
Obayashi T, Tamura H, Tanaka S, Ohki M, Takahashi S, Arai M, et al. A new chromogenic endotoxin-specific assay using recombined limulus coagulation enzymes and its clinical applications. Clin Chim Acta. 1985;149:55–65.
Takada H, Kotani S, Tanaka S, Ogawa T, Takahashi I, Tsujimoto M, et al. Structural requirements of lipid A species in activation of clotting enzymes from the horseshoe crab, and the human complement cascade. Eur J Biochem. 1988;175:573–80.
Romaschin AD, Harris DM, Ribeiro MB, Paice J, Foster DM, Walker PM, et al. A rapid assay of endotoxin in whole blood using autologous neutrophil dependent chemiluminescence. J Immunol Method. 1998;212:169–85.
Marshall JC, Walker PM, Foster DM, Harris D, Ribeiro M, Paice R, et al. Measurement of endotoxin activity in critically ill patients using whole blood neutrophil dependent chemiluminescence. Crit Care. 2002;6:342–8.
Adachi K, Shimaoka H, Nishi S. Clinical usefulness of newly developed whole blood endotoxin activity assay (EAA). ICU & CCU 2007;31:445–52 (in Japanese).
Kuwata A, Satake Y, Inoue K, Tokuda Y, Yamashita T, Fujita N. A study of the effectiveness for new endotoxin activity assay (EAA). Jpn J Crit Care Endotoxemia 2007;1:18–33 (in Japanese).
Matsumoto N, Takahashi G, Kojika M, Shozushima T, Oikawa H, Suzuki Y, et al. A study on the influence of steroids on the results of endotoxin activity assay (EAA). Jpn J Crit Care Endotoxemia 2010;14:134–9 (in Japanese).
ACCP/SCMCC Consensus Conference Committee: Definitions for sepsis and organ failure and guidelines for the use of innovative therapies in sepsis. Chest 1992;101:1644-55/Crit Care Med. 1992;20:864–74.
Inada K, Endo S, Takahashi K, Suzuki M, Narita T, Yoshida T, et al. Establishment of a new perchloric acid treatment method to allow detection of the total endotoxin content in human plasma by the Limulus test and clinical application. Microbiol Immunol. 1991;35:303–14.
Inada K. Complement activating property of protein-rich endotoxin (OEP) of Pseudomonas aeruginosa. II. Complement activating property of the lipopolysaccharide portion and the inhibition by polymyxin B. Jpn J Exp Med. 1980;50:107–15.
Yoshida M, Inada K, Endo S, Yamashita H, Iwanari H, Sekiguchi K, et al. An assay method of (1,3)-β-d-glucan to diagnose invasive mycosis. A utilization of monoclonal antibody to the activated factor C in blood coagulation system of horseshoe crab. In: Suzuki S, Suzuki M, editors. Fungal cells in biodefense mechanism. Tokyo: Saikon; 1996. p. 265–71.
Oei AL, Sweep FC, Geurts-Moespot A, van Tienoven D, von Mensdorff-Pouilly S, Thomas CMG, et al. Human anti-mouse IgM and IgG responses in ovarian cancer patients after radioimmunotherapy with 90Y-muHMFG1. Anticancer Res. 2008;28:2721–5.
Goldstein IM, Roos ZD, Weissmann AG, Kaplan HB. Influence of corticosteroids on human polymorphonuclear leukocyte function in vitro. Reduction of lysosomal enzyme release and superoxide production. Inflammation. 1976;1:305–15.
Endo S, Inada K, Ceska M, Takakuwa T, Yamada Y, Nakae H, et al. Plasma interleukin 8 and polymorphonuclear leukocyte elastase concentrations in patients with septic shock. J Inflamm. 1995;45:136–42.
Elbim C, Bailly S, Chollet-Martin S, Hakimu J, Gougerot-Pocidalo MA. Differential priming effects of proinflammatory cytokines on human neutrophil oxidative burst in response to bacterial N-formyl peptides. Infect Immun. 1994;62:2195–201.
Widdison AL, Cunningham S. Immune function early in acute pancreatitis. Br J Surg. 1996;83:633–6.
Gross V, Andreesen R, Leser H-G, Ceska M, Liehl E, Lausen M, et al. Interleukin-8 and neutrophil activation in acute pancreatitis. Eur J Clin Invest. 1992;22:200–3.
Zallen G, Moore EE, Johnson JL, Tamura DY, Shames B, Walter L, et al. Postinjury suppression of human neutrophil cytokine production results from the stabilization of inhibitory kappa b. Shock. 1999;11:77–81.
Rosenthal J, Thurman GW, Cusack N, Peterson VM, Malech HL, Ambruso DR. Neutrophils from patients after burn injury express a deficiency of the oxidase components p47-phox and p67-phox. Blood. 1996;88:4321–9.
Acknowledgments
This paper received special research grants for development of characteristic education by the Promotion and Mutual Aid Corporation for Private Schools of Japan, and Ministry of Education, Culture, Sports, Science and Technology of Japan. We wish to thank Kayo Kishi for technical assistance.
Conflict of interest
None to declare.
Author information
Authors and Affiliations
Corresponding author
About this article
Cite this article
Matsumoto, N., Takahashi, G., Kojika, M. et al. Interleukin-8 induces an elevation in the endotoxin activity assay (EAA) level: does the EAA truly measure the endotoxin level?. J Infect Chemother 19, 825–832 (2013). https://doi.org/10.1007/s10156-013-0567-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10156-013-0567-z