Abstract
Recent studies demonstrated that mortality associated with methicillin-resistant Staphylococcus aureus (MRSA) bacteremia was high when vancomycin was used to treat infections with strains that had a high vancomycin minimum inhibitory concentration (MIC). This study compared several characteristics of vancomycin MIC 2 μg/ml strains isolated from bacteremia with those isolated from infections other than bacteremia. A total of 128 episodes of MRSA bacteremia between 2005 and 2008 were followed-up, and compared with 631 MRSA infections other than bacteremia. The isolation of strains with a 2 μg/ml MIC accounted for 32.0% of isolates from MRSA bacteremia, whereas strains with a 2 μg/ml MIC comprised 9.0% of MRSA isolated from other sites (p < 0.001). The incidence of pneumonia as the source of infection was significantly higher in patients with bacteremia from strains with a 2 μg/ml MIC than in those with ≤1 μg/ml MIC. Prior vancomycin use did not correlate with the isolation of 2 μg/ml strains. The efficacy of glycopeptides as 1st line therapy in patients infected with 2 μg/ml strains was significantly lower than that for patients infected with ≤1 μg/ml strains (30.0 vs. 78.8%, p < 0.001) in bacteremia. In the analysis of infections other than bacteremia, efficacy did not reveal a significant difference according to MIC (69.0 vs. 79.6%, p = 0.109). In bacteremia, mortality was 65.8% in patients with 2 μg/ml strains and 19.5% in patients with ≤1 μg/ml strains (p < 0.001), whereas there was no significant difference in mortality from infections other than bacteremia (10.7 vs. 7.8%, p = 0.617). In multivariate analysis, bacteremia with 2 μg/ml strains, intensive care unit (ICU) stay, and liver cirrhosis were independent risk factors for death in patients with bacteremia, and initial appropriate therapy lowered the risk. Several characteristics such as a higher incidence than at other infection sites, a high incidence of pneumonia as a source of infection, a low success rate of vancomycin therapy, and poor prognosis were confirmed in 2 μg/ml MIC MRSA isolated from bacteremia; however, a low success rate of vancomycin and poor prognosis were not apparent in 2 μg/ml MIC MRSA strains isolated from infections other than bacteremia.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
There is growing concern that vancomycin may provide suboptimal therapy for severe methicillin-resistant Staphylococcus aureus (MRSA) infections [1, 2]. Although there are conflicting results [3], the recent minimum inhibitory concentration (MIC) creep in vancomycin has prompted guidelines to recommend a vancomycin target trough of 15–20 μg/ml [4]. A reduction in the efficacy of vancomycin against MRSA strains with a high MIC (1–2 μg/ml) has been described in observational studies [5, 6], suggesting that subtle changes in the MIC may explain the clinical failure. Soriano et al. [7] described that independent predictors of mortality in multivariate analysis in patients with MRSA bacteremia included the receipt of empirical vancomycin and having an isolate with a vancomycin MIC of 2 μg/ml (odds ratio [OR] 6.39). The purpose of the present study was to evaluate further the clinical characteristics of the 2 μg/ml strains in patients with bacteremia, compared with the characteristics in those with other infection sites.
Methods
Blood culture was performed using BacT-ALERT 3D (Sysmex-biomerieux, Tokyo, Japan). Isolates were identified and susceptibility determined according to standard techniques, using the Auto-Scan W/A and Comb Panel (Siemens). Methicillin susceptibility was determined by microdilution using Clinical Laboratory Standards Institute methods [8]. One hundred and twenty-eight episodes of MRSA bacteremia were recorded between January 2005 and June 2008 at a single center, and the isolated strains were stored at −20°C. To identify MRSA strains of vancomycin MIC 2 μg/ml, a standard E test was performed according to the instructions in the manufacturer’s manual (Sysmex-biomerieux). Briefly, several colonies were suspended in Mueller-Hinton broth (Nissui Pharmaceutical, Tokyo, Japan) to obtain an inoculum equivalent to a 0.5 McFarland standard. One hundred microliters of inoculum was evenly streaked onto a 90-mm BHIA (BBL; Becton Dickinson, Mountain View, MD, USA) plate and allowed to dry. Vancomycin E test strips (Sysmex-biomerieux) were applied to the surface of the agar, and the plates were incubated at 35°C in air for 24 h. Zones were read at complete inhibition, with care, to visualize hazy growth and microcolonies [9].
To compare with the clinical features of MRSA vancomycin MIC 2 μg/ml strains isolated from bacteremia, we evaluated 631 MRSA strains isolated from infection sites other than blood in the same period. These MRSA strains included 227 strains from respiratory tract infections, 205 strains from skin and soft tissue infections (incisional surgical site infections; 148 strains), 92 strains from intraabdominal infections, 58 strains from urinary tract infections, and 49 strains from other infections.
The following data were obtained as risk factors for mortality in all patients: age, sex, preexisting comorbidities, need for mechanical ventilation, need for hemodialysis, intensive care unit (ICU) stay, receipt of prior glycopeptide, receipt of prior anti-pseudomonas antibiotics, implant infection, current administration of steroids for >30 days, current administration of immunosuppressants, current administration of anticancer drugs, source of bacteremia, history of hospitalization within 6 months, presence of shock when blood samples were obtained for culture, use of linezolid (1st or 2nd choice), initial appropriate therapy (anti-MRSA drug use) within 24 h, and MRSA bacteremia with strains of vancomycin MIC 2 μg/ml. Comorbidity was defined as a disease or therapy that could predispose patients to infection, such as the following; diabetes, liver cirrhosis, renal failure, alcoholism, active neoplastic disease, receipt of a solid organ or bone marrow transplant, neutropenia, chronic obstructive pulmonary disease, or severe cardiac disease with systematic heart failure.
Empirical treatment was defined as an antibiotic administered before the definitive microbiological testing result was obtained, and it was considered to be appropriate when the isolated MRSA strain was sensitive. The mortality and clinical efficacy of vancomycin or linezolid for MRSA bacteremia caused by the strain of vancomycin MIC 2 μg/ml were compared with those for MRSA bacteremia caused by strains of vancomycin MIC ≤1 μg/ml. Mortality was defined as death from any cause at 28 days. The dosage of vancomycin was adjusted to obtain a trough serum concentration of 15–20 μg/ml after 3 days of administration. The study concerning MRSA bacteremia was approved by the ethics committee at Hyogo College of Medicine. Informed consent was not required because all procedures were routine.
Statistical analysis was performed as follows; categorical variables were compared by the χ2 test with Yates’ correction or Fisher’s exact test when necessary, by using Microsoft Excel 2003. The variables selected by univariate analysis (p < 0.2) were subjected to multivariate analysis using a stepwise logistic regression model. SPSS version 16.0 (Tokyo, Japan) was used to perform these analyses. The level of statistical significance was set at p < 0.05.
Results
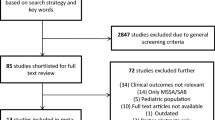
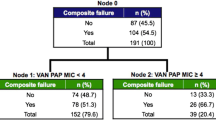
The MIC of vancomycin was 2.0 μg/ml for 41 strains (32.0%), 1 μg/ml for 85 strains (66.4%), and 0.5 μg/ml for 2 strains (1.6%) in MRSA isolated from blood cultures; however, in MRSA isolated from other materials, 2 μg/ml MIC strains accounted for only 8.9%, and there was a significant difference (p < 0.001, Table 1). The geometric mean MIC for vancomycin in MRSA isolated from blood culture was higher than that in MRSA from other materials (blood 1.235 vs. other materials 0.952, 1.3-fold).
Table 2 shows the primary diseases in patients with episodes of MRSA bacteremia according to the vancomycin MIC. There was no significant difference between groups. As the source of bacteremia, the incidence of pneumonia was significantly higher in patients with strains of 2 μg/ml MIC than in those with strains of ≤1 μg/ml MIC (Table 3). In patients with MRSA infections other than bacteremia, the percentages of each infection site were similar in patients infected with 2 μg/ml strains and in those infected with ≤1 μg/ml strains (Table 4).
In the patients with MRSA bacteremia, and in the patients with infections other than bacteremia, prior vancomycin use did not correlate with the isolation of 2 μg/ml strains in either of the groups (Tables 5, 6). Antibiotics selected as 1st line therapy for patients with MRSA bacteremia were comparable in patients with 2 μg/ml MIC strains and those with ≤1 μg/ml MIC strains (Table 7). In bacteremia patients administered glycopeptides as 1st line therapy, the clinical efficacy for strains with a vancomycin MIC of 2 μg/ml was significantly lower than that for strains with a vancomycin MIC of ≤1 μg/ml (30.0 vs. 78.8%, p < 0.001) (Table 8). In the analysis of the efficacy of glycopeptides as 1st line therapy for infections other than bacteremia, there was no significant difference between infections with 2 and ≤1 μg/ml MIC strains (p = 0.109) (Table 9).
In the analysis of each infection site, the efficacy of glycopeptides as 1st line therapy was 71.0% in infections with MIC ≤1 μg/ml strains and 53.3% in infections with MIC 2 μg/ml strains in the pulmonary tract (p = 0.253), 91.2 and 83.3% in skin and soft tissue, 80.0 and 71.0% in the intraabdominal region, 81.1 and 100% in the urinary tract, and 63.3 and 50.0% in other areas. Infections other than pulmonary tract infections were not submitted to statistical analysis because of the low numbers in the data. The efficacy of linezolid was comparable in infections other than bacteremia (80.1 and 73.7%, respectively, Table 9).
Mortality was documented in 65.8 and 19.5% of episodes due to strains with vancomycin MICs of 2 and ≤1 μg/ml, respectively, in patients with bacteremia (p < 0.001). In patients with MRSA infections other than bacteremia, mortality was 45/575 (7.8%) in those with ≤1 μg/ml MIC strains and 6/56 (10.7%) in those with 2 μg/ml MIC strains (p = 0.617).
To elucidate the role of vancomycin MIC in mortality, univariate and multivariate analyses were performed, using death at 28 days as a dependent variable. In univariate analysis, episodes involving strains with a 2 μg/ml MIC, liver cirrhosis, ICU stay, and pneumonia as a source were associated with mortality. Independent predictors associated with mortality in the multivariate analysis included having an isolate with a vancomycin MIC of 2 μg/ml, liver cirrhosis, and ICU stay, and initial appropriate therapy lowered the risk (odds ratio [OR] 0.22; 95% confidence interval [CI] 0.06–0.91) (Table 10).
Discussion
The incidence of strains with vancomycin MIC 2 μg/ml has varied considerably among several studies [3, 10–12]. As reasons for this inconsistency, an increase of these strains could be caused by either the extensive use of vancomycin or the dissemination of clones with less sensitivity to vancomycin. Moise et al. [13] demonstrated that MRSA bloodstream isolates from patients recently treated with vancomycin showed reduced susceptibility and increased tolerance to vancomycin in vitro. In the present study, however, vancomycin use did not affect the isolation of 2 μg/ml strains. It is important to clearly distinguish MIC creep from the increased occurrence of specific epidemic clones with elevated vancomycin MIC values. From another point of view, the proportion of 2 μg/ml strains among strains isolated from bacteremia in the present study was significantly higher than that in strains isolated from other infections (32.0 vs. 8.9%, p < 0.001). As an explanation, refractory infections caused by 2 μg/ml strains might subsequently develop systemic infections, such as bacteremia. Interestingly, the incidence of pneumonia as a source of infection in bacteremia due to 2 μg/ml strains was significantly higher than that in bacteremia due to ≤1 μg/ml strains. Only 20–30% of the vancomycin serum concentration is achieved in lung tissue, thus requiring even higher doses to treat pneumonia.
As reported by other investigators [2, 5, 7], the present study has suggested that the vancomycin MIC has an important impact on antibiotic efficacy and on mortality in patients with bacteremia due to MRSA. In patients administered glycopeptides, there was a significant difference in clinical efficacy between infections caused by MIC ≤1 μg/ml strains and those caused by MIC 2 μg/ml strains. In the analysis of infection sites other than blood, however, there was no significant difference in clinical efficacy. Because of the low number of 2 μg/ml strains in infections other than bacteremia, insignificant difference of the efficacy of glycopeptides between pulmonary infections caused by MIC ≤1 μg/ml strains and MIC 2 μg/ml strains may not be worth evaluating. Mortality was significantly higher in patients with MRSA bacteremia infected with 2 μg/ml strains than in those infected with ≤1 μg/ml strains; however, there was no significant difference in mortality from infections other than bacteremia. Factors independently associated with mortality in patients with bacteremia in a regression model included bacteremia with MRSA strains with a vancomycin MIC of 2 μg/ml, liver cirrhosis, and ICU stay, and initial appropriate therapy lowered the risk.
Considering the current problems with vancomycin treatment, it is necessary to clarify whether new anti-staphylococcal agents, such as linezolid, daptomycin, or tigecycline, are superior to vancomycin when the strain has a vancomycin MIC >1 μg/ml. Thickening of the cell wall observed in vancomycin-intermediate S. aureus prevents the passage of vancomycin through a thickened peptidoglycan layer [14]. Camargo et al. [15] observed a strong correlation between the presence of a thickened cell wall and daptomycin resistance. In contrast, Mitsutaka et al. [16] demonstrated that the linezolid MIC showed no correlation with VCM resistance and they suspected that linezolid would be effective to treat infections that are poorly responsive to vancomycin. In our study, the clinical efficacy of linezolid use did not reveal a significant difference according to the MIC value in patients with bacteremia and other infections. As linezolid was mainly used as 2nd line therapy in bacteremia in our study, further study is necessary to confirm its efficacy in the treatment of MRSA infections with a vancomycin MIC of ≥2 μg/ml.
In conclusion, several characteristics such as a higher incidence than at other infection sites, a high incidence of pneumonia as a source of infection, a low success rate of vancomycin therapy, and poor prognosis were confirmed in 2 μg/ml MIC MRSA isolated from bacteremia; however, such features were not apparent in infections other than bacteremia.
References
Moise PA, Schentag JJ. Vancomycin treatment failures in Staphylococcus aureus lower respiratory tract infections. Int J Antimicrob Agents. 2000;16(Suppl 1):S31–4.
Howden BP, Ward PB, Charles PG, Korman TM, Fuller A, du Cros P, et al. Treatment outcomes for serious infections caused by methicillin-resistant Staphylococcus aureus with reduced vancomycin susceptibility. Clin Infect Dis. 2004;38:521–8.
Alos JI, Garcia-Canas A, Garcia-Hierro P, Rodriguez-Salvanes F. Vancomycin MICs did not creep in Staphylococcus aureus isolates from 2002 to 2006 in a setting with low vancomycin usage. J Antimicrob Chemother. 2008;62:773–5.
Gemmell CG, Edwards DI, Fraise AP, Gould FK, Ridgway GL, Warren RE. Guidelines for prophylaxis and treatment of methicillin-resistant Staphylococcus aureus (MRSA) infections in the UK. J Antimicrob Chemother. 2006;57:589–608.
Moise PA, Sakoulas G, Forrest A, Schentag JJ. Vancomycin in vitro bactericidal activity and its relationship to efficacy in clearance of methicillin-resistant Staphylococcus aureus bacteremia. Antimicrob Agents Chemother. 2007;51:2582–6.
Sakoulas G, Moise-Broder PA, Schentag J, Forrest A, Moellering RC Jr, Eliopoulos GM. Relationship of MIC and bactericidal activity to efficacy of vancomycin for treatment of methicillin-resistant Staphylococcus aureus bacteremia. J Clin Microbiol. 2004;42:2398–402.
Soriano A, Marco F, Martinez JA, Pisos E, Almela M, Dimova VP, et al. Influence of vancomycin minimum inhibitory concentration on the treatment of methicillin-resistant Staphylococcus aureus bacteremia. Clin Infect Dis. 2008;46:193–200.
Clinical and Laboratory Standards Institute. Performance standards for antimicrobial disk susceptibility tests; approved standards. 9th ed. M2-M9. Wayne: Clinical and Laboratory Standards Institute; 2006.
Walsh TR, Bolmstrom A, Qwarnstrom A, Ho P, Wootton M, Howe RA, et al. Evaluation of current methods for detection of staphylococci with reduced susceptibility to glycopeptides. J Clin Microbiol. 2001;39:2439–44.
Steinkraus G, White R, Friedrich L. Vancomycin MIC creep in non-vancomycin-intermediate Staphylococcus aureus (VISA), vancomycin-susceptible clinical methicillin-resistant S. aureus (MRSA) blood isolates from 2001-05. J Antimicrob Chemother. 2007;60:788–94.
Sader HS, Fey PD, Fish DN, Limaye AP, Pankey G, Rahal J, et al. Evaluation of vancomycin and daptomycin potency trends (“MIC creep”) against methicillin-resistant Staphylococcus aureus collected in nine United States medical centers over five years (2002–2006). Antimicrob Agents Chemother. 2009;53:4127–32.
Sakoulas G, Moellering RC Jr. Increasing antibiotic resistance among methicillin-resistant Staphylococcus aureus strains. Clin Infect Dis. 2008;46:S360–7.
Moise PA, Smyth DS, EI-Fawal N, Robinson D, Holden PN, Forrest A, et al. Microbiological effects of prior vancomycin use in patients with methicillin-resistant Staphylococcus aureus bacteremia. J Antimicrob Chemother. 2008;61:85–90.
Cui L, Murakami H, Kuwahara-Arai K, Hanaki H, Hiramatsu K. Contribution of a thickened cell wall and its glutamine nonamidated component to the vancomycin resistance expressed by Staphylococcus aureus Mu50. Antimicrob Agents Chemother. 2000;44:2276–85.
Camargo IL, Neoh HM, Cui L, Hiramatsu K. Serial daptomycin selection generates daptomycin-nonsusceptible Staphylococcus aureus strains with a heterogeneous vancomycin-intermediate phenotype. Antimicrob Agents Chemother. 2008;52:4289–99.
Mitsutaka K, Tajima Y, Ito T, Yamashiro Y, Hiramatsu K. Use of a sensitive chemiluminescence-based assay to evaluate the metabolic suppression activity of linezolid on methicillin-resistant Staphylococcus aureus showing reduced susceptibility to vancomycin. J Microbiol Biotechnol. 2009;19:734–41.
Author information
Authors and Affiliations
Corresponding author
About this article
Cite this article
Takesue, Y., Nakajima, K., Takahashi, Y. et al. Clinical characteristics of vancomycin minimum inhibitory concentration of 2 μg/ml methicillin-resistant Staphylococcus aureus strains isolated from patients with bacteremia. J Infect Chemother 17, 52–57 (2011). https://doi.org/10.1007/s10156-010-0086-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10156-010-0086-0