Abstract
Background
The surgical treatment of rectovaginal fistula (RVF) remains challenging and there is a lack of data to demonstrate the best, single procedure. The aim of this study was to assess the results of different surgical operations for rectovaginal fistula.
Methods
Patients with RVF who underwent surgical repair between 1992 and 2017 at a single, tertiary care center were included. Twenty different procedures were performed including: primary closure, closure with sphincter repair, flap repairs, plug/fibrin/mesh repair, examination under anesthesia (EUA) ± seton placement, abdominal resections with and without diversion and ileostomy takedown, gracilis muscle transposition, fistulotomy/ligation of intersphincteric fistula tract. All patients with RVF due to diverticulitis and patients without complete data from paper charting were excluded. Success was defined based on the absence of symptoms related to RVF and absence of diverting stoma at 6 months.
Results
One hundred twenty-four women were analyzed. The median age was 45 (range 18–84) years. Median follow-up time from the last procedure was 6 months (range 0–203 months).
The total number of patients considered successfully treated at the end of their treatment was 91 (91/124, 73.4%). When considering all procedures (n = 255), the success rate for flap procedures was 57.9% (22/38), followed by abdominal resections with and without proximal diversion and ileostomy takedown (16/29, 55.2%) and primary closure with sphincter repair (17/32, 53.1%) while fistula plug, and fibrin glue had among the lowest success rates (4/22, 18.2%). The highest success rate was observed among patients whose RVF etiology was due to malignancy (11/16, 68.8%) followed by unknown (8/14, 57%) and iatrogenic (21/48, 43.8%) causes.
Conclusions
Local procedures such as mucosal flap or primary closure and sphincteroplasty are associated with a high success rate should be considered in patients with low-lying, simple RVF. Abdominal resections with and without proximal diversions and ileostomy takedown have a relatively high success rate in selected patients. The low success rate of fibrin glue and fistula plugs demonstrates their low efficacy in RVF; thus, these procedures should be avoided in the treatment algorithm.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Rectovaginal fistula (RVF) remains a challenging condition for colorectal surgeons and a significant physical and psychosocial burden to the patients. The challenging nature of this disease mostly relates to high failure rates after surgical interventions [1]. To achieve successful treatment outcome, a number of variables needs to be taken into account including the etiology, size, and location of the RVF [2]. Furthermore, there is a lack of large cohort data to establish the best surgical treatment.
American Society of Colon and Rectal Surgeons (ASCRS) in their Clinical Practice Guidelines recommends using endorectal advancement flap with or without sphincteroplasty as the procedure of choice for most simple RVF; however, this is based on low-quality evidence [3]. The treatment of complex RVFs is more complicated and often based on an individual’s anatomy, presenting symptoms and number of previous operations. Due to high failure rates, often associated with stoma creation, many surgeons adopted the step-up approach. This algorithm consists of local, conservative treatments such as rectal or vaginal advancement flaps, fistula plug [4] or fibrin glue [5] with more aggressive and complex procedures such as gracilis or Martius flap interposition or abdominal operations reserved for patients who fail the initial treatment [6, 7].
Although most patients with RVF are treated at specialized, tertiary referral centers, the complexity and relative rarity of this condition have not allowed surgeons to determine the best surgical approach for this condition. The aim of our study was to assess the results of surgical repairs of RVF at a large, tertiary referral center.
Materials and methods
Patients
Institutional Review Board approval was obtained prior to data collection. Patients who underwent RVF repair between 1992 and 2017 at a tertiary, academic, referral center were included. Retrospective analysis of a prospectively maintained database was performed based on the collected demographics, specific features of the RVFs, and variables related to the surgical procedures (Table 1). The etiology of RVFs was categorized into eight different groups including: obstetric, malignancy, inflammatory bowel disease (IBD), iatrogenic, rectal ulceration, others including chronic constipation, neovagina creation, unknown etiologies patients with RVFs due to unknown causes and non-IBD colitis of unknown etiology, and patients with multiple etiologies. Iatrogenic etiology was further subdivided into post-surgery, post-chemoradiation/radiation, and other iatrogenic causes. Inclusion criteria were patients > 18 years old with a diagnosis of RVF based on clinical symptoms and physical examination. Exclusion criteria were patients < 18 years old, those with RVFs due to diverticular disease, and patients with incomplete RVF repair paper chart documentation (Fig. 1). All patients were evaluated in the colorectal surgery clinic prior to surgery. Patients with RVF due to IBD were evaluated whether they were on 5-ASA or biologic medications treatment.
Types of RVF
Based on the ASCRS Clinical Practice guidelines, RVFs were classified as low/high and simple/complex. Low RVFs were those with the tract between the distal anal canal (dentate line or below) and the vaginal fourchette. High RVFs were defined as the ones with a tract communicating the upper vagina (at the level of the cervix) with the rectum. The location of the fistula was based on the operative description for each patient. Additionally, simple RVFs were defined as a low, small-diameter (< 2.5 cm) fistula communicating the anal canal and vagina resulting from obstetrical injury or infection. Complex RVFs involved a higher communication between the rectum and vagina, or a larger opening (> 2.5 cm) that was iatrogenic or due to radiation, cancer, or IBD [3].
Surgical procedures
All procedures were performed by colorectal surgeons. Twenty different procedures were performed (Table 2). The results were analyzed individually in terms of success, which was defined based on the absence of RVF symptoms and absence of diverting stoma at the 6 month follow-up visit. Patients who underwent abdominoperineal resection, received permanent stomas and/or failed the RVF repair at the 6-month follow-up visit were considered failures. Definitive procedures were considered surgeries with an attempt to fix RVF without an anticipated need for further surgical treatment.
Statistical analysis
Patient demographics and outcomes were analyzed using the appropriate statistical methods to determine differences between the procedures, etiologies, and patient outcomes. A significance level of 0.05 was used for all tests (α = 0.05). All statistical analyses were performed using SAS software 9.4.
Descriptive statistics were computed to summarize the frequency of each procedure and the demographic variables. The statistical analysis included patients’ demographic factors i.e., age, smoking status, location of RVF and its complexity.
Results
A total of 166 female patients were initially included in the study. One hundred sixty-six patients underwent 302 procedures. Among 166 patients, only 124 patients (74.7%) had complete data regarding their RVF procedure. The remaining 42 patients (25.3%) had incomplete data in their paper charts, and therefore, were not included in the final analysis (Fig. 1). Among the 124 patients analyzed, the median age was 45 (range 18–84) years. Twenty-five patients (20.2%) were smokers, and 70 patients (56.4%) were non-smokers. Smoking was not significantly associated with success rate of RVF surgery when comparing smokers to non-smokers (p = 0.567). The median number of procedures per patient was 1 (range 1–13 procedures) with 67 patients (54.0%) undergoing only 1 procedure and 57 patients (46.0%) undergoing 2 or more procedures. Most commonly, patients underwent multiple simultaneous procedures (28/124, 22.5%), but in terms of the most common definitive procedure, primary closure using absorbable sutures ± sphincter repair was the most performed operation (44/255, 17.3%) followed by advancement flap repair (38/255, 15%) and abdominal resections with or without proximal diversions and ileostomy takedowns (29/255, 11.4%) (Table 2). Seventy-eight patients (78/124, 62.9%) had undergone a prior RVF repair at another institution. Patients who initially had examination under anesthesia (EUA), incision and drainage (I&D) ± seton placement and patients who had multiple procedures performed were more likely to undergo additional procedures later. The total number of patients who were considered successfully treated at the end of their treatment was 91 (91/124, 73.4%), regardless of whether they underwent one or multiple procedures.
The most common etiology of RVF was found to be obstetric (43/124, 34.7%) followed by IBD (28/124, 22.6%) and iatrogenic (24/124, 19.4%). Sixty-nine patients (69/124, 55.7%) presented with low RVFs and 35 patients (35/124, 28.2%) presented with high RVFs. The remaining 20 (20/124, 16.1%) could not be classified based on the available data. Median follow-up time from the last procedure was 6 months (range 0–203 months).
Success rate by type of surgery
A total of 255 procedures were evaluated. Among the 255 procedures, 95 (95/255, 37.3%) operations were considered successful, and 153 (153/255, 60%) procedures failed. There were 7 (7/255, 2.7%) procedures with unknown outcome. The most successful outcome was after advancement flap procedures (22/38, 57.9%), followed by abdominal resections with or without proximal diversions and ileostomy takedown (16/29, 55.2%) and primary closure with sphincter repair (17/32, 53.1%). Patients who had gracilis muscle transposition or fistulotomy or ligation of intersphincteric fistula tract (LIFT) had a higher success rate; however, the number of analyzed patients was low (Table 3). When compared to abdominal resections with or without proximal diversions and ileostomy takedown, patients who had multiple simultaneous procedures had a lower success rate (OR 0.218, CI 95% 0.082–0.556, p = 0.002). Local procedures including fistula plugs, fibrin glue and mesh repairs also had a lower success rate than those who had abdominal resections with or without proximal diversions and ileostomy takedown (OR 0.18, CI 95% 0.047–0.594, p = 0.007). Lastly, patients who had EUA, I&D of an abscess and seton placement had lower success rates than those who had abdominal resections with or without proximal diversions and ileostomy takedown (OR- 0.125, CI 95% 0.042–0.342, p < 0.001); however, these procedures were intended to control perianal sepsis rather than serve as a definitive repair. Success rates of other surgical treatments were not statistically different when compared to abdominal resections with or without proximal diversions and ileostomy takedown.
When considering the definitive procedure for each patient, 91 (73.4%) out of 124 patients had successful treatments, 26 patients (26/124, 21.0%) had treatments that failed, and 7 patients (7/124, 5.6%) had unknown results. Among the ultimate, 180 definitive procedures, flap procedures had the highest success rate (91.3%), followed by abdominal resections with or without proximal diversions and ileostomy takedown (88.9%), and primary closure with sphincter repair (81%).
Success rate by location
Patients with complex, low RVF had significantly lower success rates than patients with simple, low RVF (OR 0.33, 95% CI 0.16–0.67, p = 0.002). The success rate of patients with simple, high RVFs and complex, high RVFs was not significantly different than that of patients with simple, low RVF (Table 4).
Success rate by etiology
The highest success rate was observed among patients whose RVF etiology was malignancy (68.6%) followed by unknown (57.0%) and iatrogenic (43.8%) (Table 5). Additionally, patients with malignant etiology had higher success rate than patients with RVF due to IBD or obstetric etiology (Table 5); however, when comparing two groups with different etiologies, the confidence intervals are wide due to low number of patients in each group (Table 6). Patients with obstetric, IBD, unknown, and other etiologies had a significantly higher rate of undergoing > 3 procedures than those with malignant etiology (Tables 6, 7).
Success rate for IBD patients
Patients diagnosed with IBD had a significantly lower success rate than patients without a diagnosis of IBD (Table 8). However, there was no significant difference in success rate for IBD patients who were or were not on anti-inflammatory or biologics treatment (OR-0.696, 95%CI 0.12–3.4, p = 0.66).
Discussion
RVF treatment continues to be challenging as the anatomy of the individual patient and the fistula itself are often the foremost factors in determining the procedure of choice. Historically, the recommendation was to perform less invasive procedures first and to try more complex and potentially morbid procedures in failed cases [8]. Since the publication by Corte et al. of 79 patients undergoing 286 RVF procedures, the case could be made that upfront large abdominal operation with proximal diversion may be a better option [1]. However, Gottgens et al. [9] demonstrated the disappointing quality of published studies on operative techniques for RVF in their systematic review and found that none of the studies were randomized, the closure rates varied between 0 and > 80% and the poor quality of studies did not allow performance of a meta-analysis.
Our study, including 124 patients with RVFs undergoing 255 procedures demonstrates a 37.3% overall success rate for all procedures, defined as complete healing and absence of diverting stoma at 6 months. This rate is lower than previous reports [10,11,12] with success rates ranging from 43 [13] to 100% [14], vastly depending on different etiologies and techniques used in each report. However, when considering the overall, complete healing for the last, definitive procedure, a 73.4% success rate was achieved, demonstrating the high likelihood of successful repair at the end of treatment for RVF patients. When analyzing each procedure type in our study, the success rates ranged from 15.1% after EUA, I&D ± seton placement to 57.9% and 55.2% after flap repairs and abdominal resections with or without proximal diversions and ileostomy takedown, respectively. With a relatively high success rate, our results support the findings by Corte et al. emphasizing the possible importance of upfront bowel resection with primary diversion in selected patients.
Pinto et al. [10] evaluated the predictors of outcome in 184 RVF procedures and demonstrated an overall success rate of 60% and 88% after multiple procedures, concluding that most RVFs can be successfully treated with subsequent operations. Their report demonstrates the complicated nature and the non-uniform distribution of RVF etiologies in different outcome analyses; however, it supports our findings of 73.4% success at the end of RVF treatment. The difficulty of identifying a particular etiology as a prognostic factor of success has also been replicated in our study. The most commonly observed cause of RVF in our study was obstetric and the success rate for subsequent repair of these cases was 43.4%. Additionally, patients with obstetric etiology had higher success rate than patients with RVF due to IBD and similar to iatrogenic causes. Patients with obstetric had significantly higher rate of undergoing > 3 procedures to achieve successful results than those with malignant etiology. In a recent study by Ryoo et al. [15], the authors found that a RVF due to radiation therapy and previous pelvic operation were poor prognostic factors, whereas low fistula, sphincter defect, obstetrical etiology were good prognostic factors for successful closure. Pinto et al. [10] looked at the predictors of outcome following RVF repair and found that only Crohn’s disease and smoking history are strongly associated with recurrence. Furthermore, the demographic information, location, use of immunosuppression, number of vaginal deliveries and presence of fecal diversion did not affect outcomes in their study. In our study, both post-radiation iatrogenic etiology and IBD had only a 25% success rate which supports the findings by Pinto et al.; however, we did not perform a predictive model analysis. Smoking status was not significantly associated with the end result in our study.
Fibrin glue, fistula plug
Historically, the majority of surgeons used the step-up approach; however, more recently Corte et al. [1] reported a very low success rates of minor procedures such as setons, fibrin glue, fistula plug, advancement flaps (5%, 11%, and 12%, respectively). We had slightly higher success rates, but still a very low closure rate with these minimally invasive procedures. When compared to previous results regarding the fistula plug and fibrin glue insertion, our success rate of 18.2% was significantly lower than most studies (10–78%) [11]. Therefore, we believe that fibrin glue and fistula plug must be abandoned.
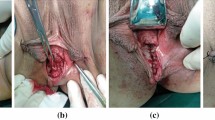
Primary closure/closure with sphincter repair
The transperineal closure technique is based on developing the plane and dissecting through the rectovaginal septum with subsequent closure of the fistula openings. It is important to note that RVF in cases of obstetrical trauma can present with a sphincter injury. Sphincter defects should be closed using the overlapping sphincteroplasty technique to prevent incontinence and to further buttress the repair as recommended by the guidelines [16]. In our study, the success rate of primary closure was 41.7%, whereas primary closure with sphincter repair was 53.1%. Previous studies demonstrated higher success rates [9]; however, systematic reviews and results of this procedure are limited due to a small number of cases and a lack of appropriate follow-up to determine the long-term closure rates.
Advancement flaps
The most commonly performed local procedures for RVF remain rectal or vaginal advancement flaps. Systematic review of the available data regarding management of RVF demonstrates an average success rate of 60% in advancement flaps, but as high as 90% in some studies [9]. Our success rate of 57.9% supports the previously reported data and ASCRS recommendations, further emphasizing that flap procedures can be considered in selected, simple, low-lying RVF as the initial operation [3, 17]. Additionally, Devesa et al. reported the success rate of endorectal advancement flaps for simple RVF to be 100% [18], whereas Ruffolo et al. [12] reported that the closure rate in RVF due to Crohn’s disease after rectal advancement flap was 69%, further supporting the fact that the success rate is often multifactorial and dependent on RVF etiology [17].
Abdominal resection and diverting ostomy
More recent studies have demonstrated improved healing rates with abdominal resection and diverting ostomy [1]. Our results demonstrate a relatively high success rate of 55% in patients undergoing resection and diverting ostomy for all abdominal resections and 88.9% when considered a final, definitive operation. Diverting ostomy can be beneficial in healing RVFs after repeated failures of local procedures and is necessary in cases where a large abdominal resection is performed in a form of an ultra-low anterior resection. Corte et al. [1] also calculated that proposing a major procedure upfront is an independent prognostic factor for success. In our analysis, abdominal resection with and without primary diversion and ileostomy takedown as the definitive procedure was found to be successful in 88.9%, suggesting that this procedure can be attempted earlier or even as the initial operation.
Gracilis muscle transposition/Martius procedure
Interposition graft procedures have been included in this analysis; however, the number of cases is very low to derive any significant conclusions. The available success rate results of both gracilis muscle interposition and Martius flap techniques range from 60 to 95% [9]. The adverse effect of these procedures on sexual activity is controversial [7, 19].
Miscellaneous techniques
Fistulotomy and LIFT procedures were also included in the study; however, the low number of cases did not allow us to draw significant conclusions. It is important to note that performing multiple simultaneous procedures has a low success rate which suggests the need for a staged approach or more aggressive operation upfront.
RVF due to IBD
We evaluated whether IBD and administration of anti-inflammatory or biologic drugs contributed to the success rate of each procedure and found that the presence of IBD significantly contributed to the success rate. Twenty-one of the patients with IBD were taking anti-inflammatory or biologic drugs; however, it did not affect the success rate of RVF closure. Although surgery is the mainstay of treatment in RVF related to Crohn’s disease, medical therapy plays a role and is usually the first step, together with the drainage of local sepsis prior to definitive RVF surgery. Our study supports the findings that RVF due to IBD are more complex, and associated with a low treatment success rate, but should still be treated in the same surgical fashion as non-IBD RVF after the disease is medically controlled and the perianal sepsis has resolved.
The limitations of our study include its retrospective design, short follow-up, a lack of case matching when comparing different procedure outcomes and non-uniform data collection. The inability to evaluate cross-application of individual operation to certain patient populations is also considered a limitation. Furthermore, our analysis includes a period prior and after the introduction of biologic agents in the late 90s and when the results of ACCENT 1 trial were published in 2002 [20]. Finally, given the number of interventions performed we tried to group them to better analyze the outcome giving rise to very heterogeneous groups such as one of the patients undergoing abdominal operations.
Conclusions
Local procedures including endorectal advancement flap operations should still be considered in patients with low-lying, simple RVF undergoing first repair. Our study demonstrates that upfront diverting ostomy with abdominal resection can be offered in selected RVF patients as the initial procedure with a relatively high success rate. The low success rate of fibrin glue and fistula plugs demonstrates that these techniques should be abandoned. RVF is a complex pathology often requiring multiple procedures, but despite the number of performed procedures in each patient, majority of RVF heals. This emphasizes the need for the operating surgeon to be familiar with multiple operations. Lastly, IBD contributes to lower success rate of RVF procedures; however, patients with IBD should be treated the same way as non-IBD patients after control of perianal sepsis.
References
Corte H, Maggiori L, Treton X, Lefevre JH, Ferron M, Panis Y (2015) Rectovaginal fistula: what is the optimal strategy?: an analysis of 79 patients undergoing 286 procedures. Ann Surg 262(5):855–860 (discussion 860–861)
Rivadeneira DE, Ruffo B, Amrani S, Salinas C (2007) Rectovaginal fistulas: current surgical management. Clin Colon Rectal Surg 20(2):96–101
Vogel JD, Johnson EK, Morris AM, Paquette IM, Saclarides TJ, Feingold DL et al (2016) Clinical practice guideline for the management of anorectal abscess, fistula-in-ano, and rectovaginal fistula. Dis Colon Rectum 59(12):1117–1133
Champagne BJ, O’Connor LM, Ferguson M, Orangio GR, Schertzer ME, Armstrong DN (2006) Efficacy of anal fistula plug in closure of cryptoglandular fistulas: long-term follow-up. Dis Colon Rectum 49(12):1817–1821
Grimaud J-C, Munoz-Bongrand N, Siproudhis L, Abramowitz L, Sénéjoux A, Vitton V et al (2010) Fibrin glue is effective healing perianal fistulas in patients with Crohn’s disease. Gastroenterology 138(7):2275–2281 (2281.e1)
Pitel S, Lefevre JH, Parc Y, Chafai N, Shields C, Tiret E (2011) Martius advancement flap for low rectovaginal fistula: short- and long-term results. Colorectal Dis Off J Assoc Coloproctol G B Irel 13(6):e112-115
Lefèvre JH, Bretagnol F, Maggiori L, Alves A, Ferron M, Panis Y (2009) Operative results and quality of life after gracilis muscle transposition for recurrent rectovaginal fistula. Dis Colon Rectum 52(7):1290–1295
Kniery KR, Johnson EK, Steele SR (2015) Operative considerations for rectovaginal fistulas. World J Gastrointest Surg 7(8):133–137
Göttgens KW, Smeets RR, Stassen LP, Beets G, Breukink SO (2014) The disappointing quality of published studies on operative techniques for rectovaginal fistulas: a blueprint for a prospective multi-institutional study. Dis Colon Rectum 57(7):888–898
Pinto RA, Peterson TV, Shawki S, Davila GW, Wexner SD (2010) Are there predictors of outcome following rectovaginal fistula repair? Dis Colon Rectum 53(9):1240–1247
Akiba RT, Rodrigues FG, da Silva G (2016) Management of complex perineal fistula disease. Clin Colon Rectal Surg 29(2):92–100. https://doi.org/10.1055/s-0036-1580631
Ruffolo C, Penninckx F, Van Assche G, Vermeire S, Rutgeerts P, Coremans G et al (2009) Outcome of surgery for rectovaginal fistula due to Crohn’s disease. Br J Surg 96(10):1190–1195
Hannaway CD, Hull TL (2008) Current considerations in the management of rectovaginal fistula from Crohn’s disease. Colorectal Dis Off J Assoc Coloproctology G B Irel. 10(8):747–755 (discussion 755–756)
Sonoda T, Hull T, Piedmonte MR, Fazio VW (2002) Outcomes of primary repair of anorectal and rectovaginal fistulas using the endorectal advancement flap. Dis Colon Rectum 45(12):1622–1628
Rahman MS, Al-Suleiman SA, El-Yahia AR, Rahman J (2003) Surgical treatment of rectovaginal fistula of obstetric origin: a review of 15 years’ experience in a teaching hospital. J Obstet Gynaecol J Inst Obstet Gynaecol 23(6):607–610
Aigmueller T, Umek W, Elenskaia K, Frudinger A, Pfeifer J, Helmer H et al (2013) Guidelines for the management of third and fourth degree perineal tears after vaginal birth from the Austrian urogynecology working group. Int Urogynecol J 24(4):553–558
Lowry AC, Thorson AG, Rothenberger DA, Goldberg SM (1988) Repair of simple rectovaginal fistulas. Influence of previous repairs. Dis Colon Rectum 31(9):676–678
Devesa JM, Devesa M, Velasco GR, Vicente R, García-Moreno F, Rey A et al (2007) Benign rectovaginal fistulas: management and results of a personal series. Tech Coloproctology 11(2):128–134
Chen X, Liao D, Luo C, Yu J, Zhang Z, Liu G et al (2013) Prospective study of gracilis muscle repair of complex rectovaginal fistula and rectourethral fistula. Zhonghua Wei Chang Wai Ke Za Zhi Chin J Gastrointest Surg 16(1):52–55
Hanauer SB, Feagan BG, Lichtenstein GR, Mayer LF, Schreiber S, Colombel JF et al (2002) Maintenance infliximab for Crohn’s disease: the ACCENT I randomised trial. Lancet Lond Engl 359(9317):1541–1549
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. Material preparation, data collection and analysis were performed by Dr. A, Dr. G, Dr. S, and Dr. P. The first draft of the manuscript was written by Dr. S and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
All procedures performed in the study involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
Informed consent
For this type of study, formal informed consent is not required.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Studniarek, A., Abcarian, A., Pan, J. et al. What is the best method of rectovaginal fistula repair? A 25-year single-center experience. Tech Coloproctol 25, 1037–1044 (2021). https://doi.org/10.1007/s10151-021-02475-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10151-021-02475-y