Abstract
Background
Stoma rods are used traditionally to prevent retraction of loop stomas into the abdominal cavity. However, there is very little evidence to support or refute their use. The aim of the present systematic review and metaanalysis was to assess the current data on stoma rods in loop stomas. The primary outcomes were stoma necrosis and stoma retraction.
Methods
A systematic review and metaanalyses were conducted using the preferred reporting items for systematic reviews and metaanalysis guidelines (PRISMA). The study protocol was registered prospectively on PROSPERO. An electronic search was performed by two reviewers independently using predefined search strategy and Medline. Bibliographies of selected studies were screened for additional references. RevMan was used to generate forest plots and calculate odds ratios and 95% confidence intervals (CIs).
Results
In total, five studies were identified that met inclusion criteria, including four randomized controlled trials. Three studies examined only ileostomies, while one included both colostomies and ileostomies, and one only examined colostomies. In total, 561 patients underwent a stoma with a rod compared to 443 without. There was a higher rate of dermatitis (rod 29.86% vs no rod 16% OR 2.65; 95% CI 1.79–3.93) and stoma necrosis (rod 7% vs no rod 1.15% OR 5.58; 95% CI 1.85–16.84) in the rod group, but there was no significant difference in stoma retraction (rod 2.28% vs no rod 3.45%; OR 0.7; 95% CI 0.32–1.54).
Conclusions
Stoma rods do not reduce the incidence of stoma retraction and instead lead to increased rates of dermatitis and stoma necrosis.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Loop stomas are commonly created in colorectal surgery to divert the faecal stream. This may be a defunctioning loop ileostomy to protect a downstream colorectal anastomosis and reduce the risk of a clinically significant leak [1]. Less commonly, a loop colostomy is performed for this indication. Other indications for loop stoma formation are to divert in the setting of obstruction, either in the acute setting or with unresectable distal disease, for pelvic floor conditions and for severe perineal disease. One problem with loop stomas is their tendency to retract and the stoma rod has traditionally been used to reduce this risk. The aim of this systematic review and metaanalysis was to objectively assess the stoma rod to see if it improved outcomes.
The stoma rod was first introduced in 1888, and improved stoma care by preventing easily retracting stomas as at the time stomas were brought to skin level without suturing [2]. The main rationale for rod use is to reduce the risk of stoma retraction. However, as stoma techniques advanced with sutured techniques, the advent of the Brook ileostomy in the 1950s, and a better understanding of stoma care, the need for the rod is now more questionable [3].
Stomas themselves are not without complications, despite frequently being performed as a prophylactic measure to reduce perioperative risk of a clinically significant leak [4]. Beyond the psychological effects of stoma formation, there are multiple physical complications that are well described including include parastomal hernias, stoma retraction, stoma necrosis, and dermatitis.
The rates of stoma complications between those with and without a rod are unclear. Furthermore, patient-reported outcome measures (PROMs) are increasingly recognised, as critical outcomes we should be considering in clinical trials [5]. The impact of the stoma rod on the patient experience and quality of life is not well known.
This systematic review and metaanalysis sought to determine whether a stoma rod reduces complication rates in loop stomas. Furthermore, the study aimed to determine whether use of a stoma rod impacted on patient’s quality of life and whether there is an evidence-based rationale for the routine use of a stoma rod.
Materials and methods
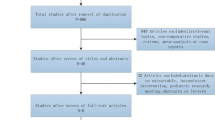
A systematic review was performed using a predefined search strategy using online electronic databases Pubmed and EMBASE. Two independent reviewers (HM and AP) performed the search and data extraction. The review was conducting in keeping with the preferred reporting items for systematic reviews and metaanalyses (PRISMA) statement and the review was registered online at PROSPERO (registration number CRD 42018095423). The literature was reviewed systematically by searching in Pubmed and Embase for studies published between 1 January 2000 and 7 May 2018 (Fig. 1).
The search strategy included the following domains of Medical Subject Heading (MeSH) terms: ‘stoma AND rod’, ‘stoma AND bar’, ‘ileostomy AND rod’, ‘ileostomy AND bar’, ‘colostomy AND rod’, ‘colostomy AND bar’, ‘surgical stoma AND rod’, ‘surgical stoma AND bar’, ‘loop ileostomy AND rod’, ‘loop ileostomy AND bar’, ‘loop colostomy AND rod’, and ‘loop colostomy AND bar’.
Randomized controlled trials (RCTs) and prospective cohort studies comparing ileostomy and/or colostomy with and without rod were included. Animal studies and studies not published in English were excluded. Two authors (HM and AP) screened the titles and abstracts independently for eligibility. Disagreements were resolved by discussion and consensus achieved. Primary and secondary outcomes were extracted from the full text. All studies were assessed for risk of bias using the Oxford Centre for Evidence-Based Medicine (CEBM) Critical Appraisal Skill Programme Checklists for randomized trials and observational cohort studies.
Statistical analysis was performed using an analysis of variance and random effects model in RevMan Version 5, and forest plots were constructed using outcomes of interest and odds ratios and 95% confidence intervals calculated.
Results
The search strategy retrieved 178 articles, of which 5 were included in the final analysis, including 4 RCT [6,7,8,9,10] (Table 1). Results of the methodological quality assessment are reported in Table S1 (supporting information). All studies were prospective. In three studies [6,7,8], the assignment of patients was randomized and a centralized computer randomization was performed in two of them [6, 8]. Because both surgeons and patients were able to distinguish between patients with or without a stoma rod, the studies could not be described as blinded. In all studies, missing data were verified. Aside from the use or not of the stoma rod, groups were treated equally. Losses to follow-up were less then 20% in all included studies. In the one observational cohort study, the rate of stoma rod usage decreased significantly over the course of the study period from 91.4% in 2003 to 10% in 2010 [9].
Study population
In total, 1058 patients were included in the analysis. Characteristics of patients included are given in Table 1. There was no difference in patient baseline characteristics between those in which a rod was used vs not used within each individual study, but there were differences in mean age and Body Mass Index (BMI) across the studies. One study was conducted on patients with ulcerative colitis [7] (Table 2). Of the five studies, three included only patients with ileostomy [5, 7, 10], one only patients with colostomy [8], and one both patients with ileostomy and colostomy [9].
Quality assessment of included studies
Critical appraisal of studies based on Centre for Evidence-Based Medicine (CEBM) criteria for RCTs and observational cohort studies was performed to assess for the risk of bias (Supplementary Table 1). All included studies were of sufficient quality to allow metaanalysis.
Duration of stoma rod
In two studies, it was not specified how long the rod has been left in [6, 9]. In two studies, the rod was removed on the 7–8th day after surgery [7, 10], while in the RCT performed by Franklyn et al., the rod was left in place until the 10–14th day after surgery [8].
Indications for stoma
The indications for stoma formation were heterogenous across the studies. Uchino et al. looked only at ileostomy formation for ileal pouch–anal anastomosis (IPAA) for ulcerative colitis [7]. Overall, inflammatory bowel disease (IBD) and cancer were the two most common indications for ileostomy, with a diverse range of other indications also represented (Table 2). Comparison of indications for stoma between rod and no rod group was reported in four out of five studies (not reported in Ref. [10]), with no significant difference in any study.
Stoma retraction
Stoma retraction was recorded as an outcome in all five studies (n = 1047 patients total) [6,7,8,9,10]. The incidence of stoma retraction overall was 2.87% (n = 30). Comparing those with a stoma rod to those without, there was no significant difference [rod n = 12, 2.28%; no rod n = 18, 3.45%; OR 0.7 (95% CI 0.32–1.54)] (Fig. 2). Interestingly, in the cohort study which saw a significant decrease in stoma rod usage over the study period, there was no difference across years in stoma retraction [9].
Stoma necrosis
The incidence of stoma necrosis or ischaemia was reported in four of five studies (n = 718) [6, 8,9,10]. There was a significantly higher rate of stoma necrosis in the group that had a rod compared with no rod [rod 7% (n = 26); no rod 1.15% (n = 4); OR 5.58 (95% CI 1.85–16.84)] (Fig. 3). Franklyn et al. also reported skin necrosis separately, which occurred in one patient with a stoma rod but none without [8].
Peristomal dermatitis
The rate of peristomal dermatitis was explicitly recorded in two studies (n = 689) [7, 9]. In these studies, there was a significantly increased risk of dermatitis in the group that used a rod [(rod 29.86% (n = 103); no rod 16% (n = 55); OR 2.65 (95% CI 1.79–3.93)]. Frankyln et al. reported on “skin necrosis” instead, with one case in the rod group and none in the group with no rod [8].
Mucocutaneous separation
Two studies reported on mucocutaneous separation [8, 9]. There was no significant difference in mucocutaneous separation between the two groups [rod 7.72% (n = 23); no rod 3.86% (n = 11); OR 2.06 (95% CI 0.98–4.32)].
Parastomal abscess
There was no significant difference in parastomal abscess [8, 9]. Again, only two studies reported on parastomal abscess [rod 1.67% (n = 5); no rod 0.7% (n = 2); OR 2.46 (95% CI 0.47–12.9)]. Incisional surgical site infection rather than parastomal abscess was recorded by Uchino et al., who also found no difference between groups [7].
Length of stay
Three studies reported length of stay (LOS), and sufficient data was available in two of three studies for inclusion in the metaanalysis. There was no significant difference in LOS between patients that did and did not have a stoma rod.
Quality of life
Zindel et al. conducted a quality-of-life assessment with a validated tool, the Stoma Quality-of-Life Scale (SQOLS)pre and post-surgery [6]. Postoperative measures were recorded at both 2 weeks and 3 months. There was no difference in SQOLS between those who had a rod and those who did not. Those with stoma retraction had a significantly worse SQOLS. No other study included quality of life or patient-reported outcome measures.
Other outcome measures
Zindel et al. included a composite score the Stoma-Specific Morbidity Score (SSMS). There was no difference based on presence of a stoma rod, but patients with a higher BMI did have a higher SSMS. Zindel et al. also recorded the amount of time taken by stoma nurses to instruct patients, and found no difference between groups [6].
Discussion
This systematic review and metaanalysis demonstrates that routine use of the stoma rod should be avoided. In particular, there is evidence of increased local stoma complications, such as dermatitis and stoma necrosis. Use of a stoma rod does not appear to protect against stoma retraction. Given that the aim of a stoma is often to reduce complications, adding a device that increases complications is counter intuitive [11, 12]. The aim of the rod is to prevent retraction [13]. However, this metaanalysis shows that it does not reduce the rate of stoma retraction.
There are multiple techniques described for the formation of a stoma rod. These include traditional hard plastic bridge devices and softer tubing, e.g., Foley catheter, to make a soft ring rod [14, 15]. Theoretically, these may have a lower complication rate. However, given the low rate of complications without a rod, the need for this is debatable. In essence, rods should only be used for selected cases and when using a rod a soft plastic ring rod instead of a traditional rod should be considered.
There are anecdotal reports of difficulty fitting stoma appliances with rods, which may in theory delay the time when the patient is able to manage the stoma independently. For example, Speirs et al. reported that bridging a stoma makes it more difficult to fit a stoma appliance and, therefore, increases the risk of soiling. This is difficult to capture and measure, and only one study used a formal quality-of-life tool and an assessment of time taken by the stoma nurse to instruct the patient. There was no difference found in the study by Zindel et al., but numbers were low and there is a possibility of a type 2 error [6]. Further RCTs should include rigorous assessment of PROMs that capture the patient experience and patient-reported outcomes.
Limitations
Limitations of this systematic review include the paucity of trials on this topic, and the differential reporting of results, making only smaller numbers available for each outcome. It is possible that there is a type 2 error in the results, particularly given the low incidence of the primary endpoints of stoma necrosis and retraction. In addition, the review was unable to discern outcomes in subgroups of patients, e.g., the very obese, as there were insufficient data reported from included trials. This review also did not focus on studies which compared different types of stoma rod, and there was limited reporting of the length of time the rod was left in situ.
Conclusions
Stomas can be associated with morbidity [16]. The stoma rod does not provide a proven benefit in formation of a loop stoma, and higher rates of stoma necrosis and dermatitis are associated with rod use.
References
Dehni N, Schlegel RD, Cunningham C, Guiguet M, Tiret E, Parc R (1998) Influence of a defunctioning stoma on leakage rates after low colorectal anastomosis and colonic J pouch-anal anastomosis. Br J Surg 85(8):1114–1117
Doughty DB (2008) History of ostomy surgery. J Wound Ostomy Cont Nurs 35(1):34–38
Brooke B (1952) The management of an ileostomy including its complications. Lancet 2:102–104
Malik T, Lee MJ, Harikrishnan AB (2018) The incidence of stoma related morbidity—a systematic review of randomised controlled trials. Ann R Coll Surg Engl 100(7):501–508
McNair AGK, Whistance RN, Forsythe RO, Rees J, Jones JE, Pullyblank AM, Avery KNL, Brookes ST, Thomas MG, Sylvester PA, Russell A, Oliver A, Morton D, Kennedy R, Jayne DG, Huxtable R, Hackett R, Dutton SJ, Coleman M, Card M, Brown J, Blazeby JM (2015) Synthesis and summary of patient-reported outcome measures to inform the development of a core outcome set in colorectal cancer surgery. Colorectal Dis 17(11):O217–O229
Zindel J, Gygax C, Studer P, Kauper M, Candinas D, Banz V, Brügger LE (2017) A sustaining rod increases necrosis of loop ileostomies: a randomized controlled trial. Int J Colorectal Dis 32(6):875–881
Uchino M, Ikeuchi H, Bando T, Chohno T, Sasaki H, Horio Y (2017) Is an ostomy rod useful for bridging the retraction during the creation of a loop ileostomy? A randomized control trial. World J Surg 41(8):2128–2135
Franklyn J, Varghese G, Mittal R, Rebekah G, Jesudason MR, Perakath B (2017) A prospective randomized controlled trial comparing early postoperative complications in patients undergoing loop colostomy with and without a stomarod. Colorectal Dis 19(7):675–680
Whiteley I, Russell M, Nassar N, Gladman MA (2016) Outcomes of support rod usage in loop stoma formation. Int J Colorectal Dis 31(6):1189–1195
Speirs M, Leung E, Hughes D, Robertson I, Donnelly L, Mackenzie I, Macdonald A (2006) Ileostomy rod—is it a bridge too far? Colorectal Dis 8(6):484–487
Pisarska M, Gajewska N, Małczak P, Wysocki M, Witowski J, Torbicz G, Major P, Mizera M, Dembiński M, Migaczewski M, Budzyński A, Pędziwiatr M (2018) Defunctioning ileostomy reduces leakage rate in rectal cancer surgery—systematic review and meta-analysis. Oncotarget 9(29):20816–20825. https://doi.org/10.18632/oncotarget.25015 (eCollection 2018 Apr 17)
Wu X, Lin G, Qiu H, Xiao Y, Wu B, Zhong M (2018) Loop ostomy following laparoscopic low anterior resection for rectal cancer after neoadjuvant chemoradiotherapy. Eur J Med Res 23(1):24. https://doi.org/10.1186/s40001-018-0325-x
Oh HK, Han EC, Song YS, Seo MS, Ryoo SB, Jeong SY, Park KJ (2015) Is the use of a support bridge beneficial for preventing stomal retraction after loop ileostomy? A prospective nonrandomized study. J Wound Ostomy Cont Nurs 42(4):368–373
Dziki Ł, Mik M, Trzciński R, Buczyński J, Darnikowska J, Spychalski M, Wierzbicka A, Dziki A (2015) Evaluation of the early results of a loop stoma with a plastic rod in comparison to a loop stoma made with a skin bridge. Pol Przegl Chir 87(1):31–34. https://doi.org/10.1515/pjs-2015-0014
Goldstein ET, Williamson PR (1993) A more functional loop ileostomy rod. Dis Colon Rectum 36(3):297–298
Shabbir J, Britton DC (2010) Stoma complications: a literature overview. Colorectal Dis 12(10):958–964
Funding
None.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
As this was a systematic review and metaanalyses of existing studies ethical approval was not required.
Informed consent
For this type of study formal consent is not required.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Mohan, H.M., Pasquali, A., O’Neill, B. et al. Stoma rods in abdominal surgery: a systematic review and metaanalyses. Tech Coloproctol 23, 201–206 (2019). https://doi.org/10.1007/s10151-019-01935-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10151-019-01935-w