Abstract
Background
Surgical site infections (SSI) are costly complications that may cause significant morbidity and increase the cost of care, particularly in colorectal surgery. Microbial sealants (MS) are a new class of wound barriers aimed at decreasing SSI; however, there is only evidence of benefit in clean class 1 procedures. Based on its success in class 1 procedures, we hypothesized that a microbial sealant could reduce the rate of SSI by half for clean-contaminated colorectal procedures (class 2).
Methods
This was a single institution, multihospital, prospective, randomized study approved by the institutional review board. The primary objective was to determine the rate of SSI when microbial sealant (InteguSeal© Kimberly-Clark) is used compared to control (no microbial sealant). Data collected included: open versus laparoscopy, age, body mass index (BMI), diabetes and morbidity [American Society of Anesthesiologists (ASA) class], hospital readmission, reoperation and wound dehiscence. Enrolled subjects received the same preoperative mechanical bowel preparation with oral antibiotics, operative skin preparation (Chloraprep), Surgical Care Improvement Project guidelines implementation), and postoperative care glycemic control for diabetics.
Results
A total of 100 subjects were recruited over 15 months (MS-50; no MS-50). The overall incidence of SSI was 12 %, 14 % (7/50) in the MS versus 10 % (5/50) in the no MS group (p = 0.545). SSI incidence with and without microbial sealant was not significantly different in either the open or the laparoscopic subgroup. Laparoscopy decreased absolute risk of SSI by 16 %. Secondary data (age, BMI, diabetes, ASA) and tertiary data (readmission, reoperation, wound dehiscence) were positively correlated with SSI.
Conclusions
Microbial sealant as employed in this study did not appear to offer any benefit in a class 2 (clean contaminated) operative procedure when perioperative care is standardized. The relative benefit of laparoscopy was also confirmed but unaffected by use of the microbial sealant.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Surgical site infections (SSI) are serious operative complications that occur in approximately 2 % of all surgical procedures [1] and result in 1 million additional inpatient days at a cost of 1.6 billion dollars per year in the USA [2]. The American College of Surgeons NSQIP data 1992–2002 reveals the cost of SSI is $25,546 per event or about $32,714 adjusted for today’s inflation rate [3]. The 2005 Healthcare Cost and Utilization Project [2] reports that over half of the total patients discharged with SSI come after colon and rectal surgery. In fact, up to 25 % of elective colorectal procedures develop SSI [4] and prolong hospital stay 4 days [2]. The major SSI expense occurs after discharge because 80 % of SSI present in the outpatient time period. This is also the reason readmission for SSI is triple the rate of patients discharge with SSI [2]. In addition to increasing healthcare cost, SSI exacerbates comorbidities and increases the rate of long-term incisional hernia [5].
Mechanical bowel preparation with oral antibiotics, abdominal skin preparation, prophylactic intravenous (IV) antibiotics, laparoscopy and postoperative glycemic control in diabetics have been shown to reduce the risk of developing SSI. In addition to skin preparation, the addition of wound barriers may also lower the incidence of SSI by theoretically providing a physical barrier to bacterial contamination of the wound during surgery. The use of intraoperative wound barriers, such as the ALEXIS O-ring wound retractor, does decrease the rate of SSI [6]. However, the efficacy of preoperative wound barriers, such as iodine-impregnated adhesive drapes, remains unclear [7, 8].
A new class of wound barriers is the microbial sealants. Microbial sealant is a liquid applied to the area of incision, after skin preparation and just before incision. Microbial sealants have reduced the incidence and relative risk of SSI by 35 % in clean class 1 procedures such as cardiac surgery, open elective inguinal hernia repair and elective spine surgery [9–14]. We proposed to perform the first study assessing the role of a skin microbial sealant for reducing the rate of superficial and deep wound SSI in a blended case mix of open and laparoscopic clean-contaminated procedures.
Materials and methods
The primary objective was to determine whether the microbial sealant InteguSeal© (Kimberly-Clark, Irving, TX, USA) could reduce the incidence of SSI for elective clean-contaminated abdominal colorectal procedures compared to control (no microbial sealant). Kimberly-Clark donated the InteguSeal© for this study. Based upon internal quality reports, the average blended SSI rate for laparoscopic and open colectomy at our institution is approximately 17 % or about mid-range for reported SSI rates (9.4–25 %) for colorectal procedures. We powered this study with the assumption that InteguSeal© would lower the incidence of superficial and deep wound SSI by 50 % based on our institutions blended rate of wound SSI for colectomy. Based on the Cohen’s d statistical table [15], for a 0.95 powered study to detect a 50 % change in the rate of SSI, we need a population of approximately 105. We collected the following data: open versus laparoscopy, age, body mass index (BMI), diabetes, morbidity (American Society of Anesthesiologists (ASA) class), hospital readmission and wound dehiscence.
This study was approved by the institutional review board and conducted in accordance with United States Food and Drug Administration regulatory guidelines and ethical standards (Helsinki Declaration). Study design was a single institution, multihospital, prospective and randomized. Consenting patients were blinded from the use (or nonuse) of InteguSeal©. Randomization was achieved via sealed envelopes containing either ‘InteguSeal©’ or ‘Control.’ Control is ‘no use’ of InteguSeal©.
Inclusion criteria are elective laparoscopic or open procedures including: segmental colectomy, total abdominal colectomy, ileorectal anastomosis, total proctocolectomy, low anterior resection, Hartmann’s resection, ileal pouch anal anastomosis and small bowel resection. The laparoscopic procedures were ‘pure laparoscopic’ and not hand assist. Laparoscopic cases converted to open were included in the latter group for statistical analysis. Exclusion criteria were as follows: participants under 18 years of age, pregnancy (positive human chorionic gonadotropin test), history of hypersensitivity to cyanoacrylate–formaldehyde–acetone, emergent surgery, laparotomy within 60 days, planned re-laparotomy within 60 days, sepsis, neutropenia, previous abdominal wound infection, serum creatinine > 3 mg/dL, chemotherapy or radiation within one month, steroids > 10 mg prednisone daily, Remicade within 2 weeks and human immunodeficiency virus with CD4 < 200.
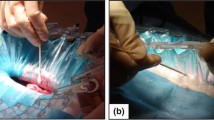
Enrolled subjects were to receive the same preoperative (mechanical bowel preparation with oral antibiotics), operative (Chloraprep and Surgical Care Improvement Project (SCIP)guidelines) and postoperative care (glycemic control for diabetics). The night before surgery patients receive mechanical bowel preparation with Miralax 8.3 oz or 238 g (polyethylene glycol) in 64 oz of Gatorade. Oral antibiotics neomycin 1 g at 3, 4 and 10 pm and metronidazole 500 mg at 10 am, 4 and 10 pm were also given with mechanical bowel preparation. The bowel preparation protocol is standardized across all patients whether they join the study or not. This allows for subjects to consent for this study in the outpatient office setting or just prior to surgery. Enrolled subjects were randomized to either receive InteguSeal© or not (control). When applied, the InteguSeal© was applied to the entire anterior abdominal wall and allowed to solidify for 2 min and all skin incisions were made through the layer of InteguSeal©. Patients received parenteral ceftriaxone 1–2 g and metronidazole 500 mg within 1 h of surgery and continued 6 h for a 24 h period. Abdomen preparation, prior to sealant application, consisted of hair removal by clippers and Chloraprep (2 % chlorhexidine gluconate, 70 % isopropyl alcohol). SCIP [16] and a standardized enhanced recovery protocol were implemented for all patients [17]. Dressings were removed the first postoperative morning and left undressed. Patients were monitored daily for SSI and follow-up occurred at 4 weeks to assure capture of any outpatient recognized infection. Standard wound care was used at the discretion of the managing surgeon if a SSI developed.
Wound classification includes incisional SSI (superficial to fascia) and deep incisional SSI (deep to fascia) [18]. Incisional SSI occurs within 30 days of surgery with symptoms of heat, erythema, tenderness, swelling, positive organism cultured and/or purulent discharge (excluding stitch abscess). Deep incisional SSI is defined as a superficial SSI with wound fascia dehiscence.
The statistical significance of microbial sealant is best determined with a Chi-square test for independence. This study data are categorical and not interval, either a patient developed SSI or they did not. Therefore, the Chi-square 2 × 2 contingency table may be used to test the null hypothesis. Table 1 illustrates the Chi-square contingency table comparing microbial sealant use to no microbial sealant (control).
Significance is determined by use of the shortcut Chi-square formula for 2 × 2 tables: x 2 = [n (ad − bc)2]/[(a + c) (b + d) (a + b) (c + d)], whereas n is the total population
The null hypothesis is accepted if x 2 < 3.841 and rejected if x 2 > 3.841 if the distribution α is 0.05. Microbial sealant would be considered statistically significant if the shortcut Chi-square formula is greater than 3.841. SSI ratios allow for categorical comparison but are not used to determine statistical significance.
Results
A total of 100 subjects were enrolled during the study period over 15 months. Table 2 is the Chi-square 2 × 2 contingency table for the entire population of clean-contaminated colorectal procedures. Table 2 illustrates patients who developed SSI with microbial sealant and without microbial sealant (control).
The shortcut Chi-square formula for Table 2: [100 (7 × 45 − 5 × 43)2]/[(7 + 43) (5 + 45) (7 + 5) (43 + 45)] = 0.545
The null hypothesis is accepted, and microbial sealant does not significantly reduce SSI in clean-contaminated colorectal procedures compared to no microbial sealant.
A total of 57 out of 100 procedures were completed purely laparoscopic. Table 3 is the Chi-square 2 × 2 contingency table for laparoscopic clean-contaminated colorectal procedures.
The shortcut Chi-square formula for Table 3: [57 (2 × 27 − 0 × 28)2]/[(2 + 28) (0 + 27) (2 + 0) (28 + 27)] = 1.87
The null hypothesis is accepted, and microbial sealant does not significantly reduce SSI in pure laparoscopic clean-contaminated colorectal procedures compared to no microbial sealant.
A total of 42 out of 100 procedures were completed open or laparoscopic converted to open. Table 4 is the Chi-square 2 × 2 contingency table for open clean-contaminated colorectal procedures.
The shortcut Chi-square formula for Table 4: [42 (5 × 19 − 5 × 13)2]/[(5 + 13) (5 + 19) (5 + 5) (13 + 19)] = 0.293
The null hypothesis is accepted, and microbial sealant does not significantly reduce SSI in open clean-contaminated colorectal procedures compared to no microbial sealant.
Certain patient characteristics influence the risk of developing SSI. Table 5 categorizes patient characteristics based on age, sex, ASA, diabetes and BMI. Older patients with increased morbidity (higher ASA) and diabetics and overweight patients tended to have a higher incidence of SSI. Table 5 also categorizes outcomes such as readmission, ileus/SBO, wound dehiscence, leak/abscess and mortality. The SSI ratio shows that 1/3 of hospital readmissions had SSI. All wound dehiscence had SSI.
Discussion
Clean-contaminated colorectal surgery procedures are ideal to test the efficacy of microbial sealant for class 2 procedures. SSI occurs in 9–24 % of abdominal colorectal procedures versus 2–9 % for abdominal non-colorectal surgery. The primary endpoint of this study was to determine whether microbial sealant helps prevent SSI for clean-contaminated colorectal procedures. These data are consistent with our typical mix of laparoscopic and open colectomy. We powered this study to detect a 50 % change in the rate of SSI from the historical 17 % SSI at our institution. Our study population had SSI rate of 12 % which is somewhat less powered than we anticipated, but enough to determine statistical significance. Table 2 clearly shows microbial sealant is of no benefit for preventing SSI in this wound class.
Although we have proven microbial sealant not useful in clean-contaminated procedures, other methods are beneficial. SCIP IV antibiotics such as cefazolin/metronidazole, ciprofloxacin/metronidazole or ertapenem have been shown to decrease SSI more than other types or combinations of antibiotics [19]. Preoperative bowel preparation with a combination of oral non-absorbable antibiotics such as neomycin and erythromycin base has also been shown to decrease SSI [20–24]. These non-absorbable antibiotics do not increase the incidence of postoperative Clostridium difficile colitis [25]. Chlorhexidine–alcohol should be used instead povidone–iodine [26] as should an ALEXIS O-ring wound retractor for bowel extraction [6]. A subcutaneous drain eliminates dead-space fluid collections which can become infected. These drains have been shown to decrease SSI in obese patients [27]. Patients with diabetes benefit from perioperative blood glucose monitoring and control [28].
Perhaps the most powerful deterrent of SSI, as confirmed by this study, is the completion of a clean-contaminated procedure using pure laparoscopy [29]. In our study, open operations were associated with SSI over seven times that of minimally invasive colectomy. Fortunately, the use of minimally invasive colectomy is increasing. Laparoscopic colectomy for benign disease increased from 6.2 % in 2001–2003 to 11.8 % in 2005–2007, while those for colon cancer have increased by a larger percentage, 2.3–8.9 % [30]. This should decrease overall SSI rate more than any other factor in the near future.
Conclusions
The data presented failed to demonstrate a benefit for the routine addition of a microbial skin sealant to our standard perioperative care plan for open and laparoscopic colectomy. Further work is required to identify simple, cost-effective methods of reducing wound SSI in colectomy.
References
Raymond DP, Pelletier SJ, Crabtree TD, Schulman AM, Pruett TL, Sawyer RG (2001) Surgical infection and the aging population. Am Surg 67:827–833
de Lissovoy G, Fraeman K, Hutchins V, Murphy D, Song D, Vaughn BB (2009) Surgical site infection: incidence and impact on hospital utilization and treatment costs. Am J Infect Control 37:387–397
Smith RL, Bohl JK, McElearney ST et al (2004) Wound infection after elective colorectal resection. Ann Surg 239:599–605 discussion 605–607
Murray BW, Cipher DJ, Pham T, Anthony T (2011) The impact of surgical site infection on the development of incisional hernia and small bowel obstruction in colorectal surgery. Am J Surg 202:558–560
Cheng KP, Roslani AC, Sehha N et al (2012) ALEXIS O-ring wound retractor vs. conventional wound protection for the prevention of surgical site infections in colorectal resections. Colorectal Dis 14:e346–e351
Webster J, Alghamdi AA (2007) Use of plastic adhesive drapes during surgery for preventing surgical site infection. Cochrane Database Syst Rev 17:CD006353
Kramer A, Assadian O, Lademann J (2010) Prevention of postoperative wound infections by covering the surgical field with iodine-impregnated incision drape (Ioban 2). GMS Krankenhhyg Interdiszip 21:5
Dohmen PM, Gabbieri D, Weymann A, Linneweber J, Geyer T, Konertz W (2011) A retrospective non-randomized study on the impact of INTEGUSEAL, a preoperative microbial skin sealant, on the rate of surgical site infections after cardiac surgery. Int J Infect Dis 15:e395–e400
Iyer A, Gilfillan I, Thakur S, Sharma S (2011) Reduction of surgical site infection using a microbial sealant: a randomized trial. J Thorac Cardiovasc Surg 142:438–442
Dohmen PM, Gabbieri D, Weymann A, Linneweber J, Konertz W (2009) Reduction in surgical site infection in patients treated with microbial sealant prior to coronary artery bypass graft surgery: a case–control study. J Hosp Infect 72:119–126
von Eckardstein AS, Lim CH, Dohmen PM (2011) A randomized trial of a skin sealant to reduce the risk of incision contamination in cardiac surgery. Ann Thorac Surg 92:632–637
Towfigh S, Cheadle WG, Lowry SF, Malangoni MA, Wilson SE (2008) Significant reduction in incidence of wound contamination by skin flora through use of microbial sealant. Arch Surg 143:885–891 discussion 891
Dromzee E, Tribot-Laspière Q, Bachy M, Zakine S, Mary P, Vialle R (2012) Efficacy of integuseal for surgical skin preparation in children and adolescents undergoing scoliosis correction. Spine (Phila Pa 1976) 37:E1331–E1335
Kenny, David A (1987) Statistics for the social and behavioral sciences. Boston. Chapter 13, page 215, in: Little, Brown. ISBN 0-316-48915-8
Rosenberger LH, Politano AD, Sawyer RG (2011) The surgical care improvement project and prevention of post-operative infection, including surgical site infection. Surg Infect (Larchmt) 12:163–168
Adamina M, Kehlet H, Tomlinson GA, Senagore AJ, Delaney CP (2011) Enhanced recovery pathways optimize health outcomes and resource utilization: a meta-analysis of randomized controlled trials in colorectal surgery. Surgery 149:830–840
Horan TC, Gaynes RP, Martone WJ, Jarvis WR, Emori TG (1992) CDC definitions of nosocomial surgical site infections, 1992: a modification of CDC definitions of surgical wound infections. Infect Control Hosp Epidemiol 13:606–608
Hendren S, Fritze D, Banerjee M (2013) Antibiotic choice is independently associated with risk of surgical site infection after colectomy: a population-based cohort study. Ann Surg 257:469–475
Bellows CF, Mills KT, Kelly TN, Gagliardi G (2011) Combination of oral non-absorbable and intravenous antibiotics versus intravenous antibiotics alone in the prevention of surgical site infections after colorectal surgery: a meta-analysis of randomized controlled trials. Tech Coloproctol 15:385–395
Cannon JA, Altom LK, Deierhoi RJ et al (2012) Preoperative oral antibiotics reduce surgical site infection following elective colorectal resections. Dis Colon Rectum 55:1160–1166
Deierhoi RJ, Dawes LG, Vick C, Itani KM, Hawn MT (2013) Choice of intravenous antibiotic prophylaxis for colorectal surgery does matter. J Am Coll Surg 217:763–769
Fry DE (2011) Colon preparation and surgical site infection. Am J Surg 202:225–232
Englesbe MJ, Brooks L, Kubus J (2010) A statewide assessment of surgical site infection following colectomy: the role of oral antibiotics. Ann Surg 252:514–519 discussion 519–520
Krapohl GL, Phillips LR, Campbell DA Jr (2011) Bowel preparation for colectomy and risk of Clostridium difficile infection. Dis Colon Rectum 54:810–817
Darouiche RO, Wall MJ Jr, Itani KM et al (2010) Chlorhexidine-alcohol versus povidone-iodine for surgical-site antisepsis. N Engl J Med 362:18–26
Fujii T, Tabe Y, Yajima R (2011) Effects of subcutaneous drain for the prevention of incisional SSI in high-risk patients undergoing colorectal surgery. Int J Colorectal Dis 26:1151–1155
Sehgal R, Berg A, Figueroa R et al (2011) Risk factors for surgical site infections after colorectal resection in diabetic patients. J Am Coll Surg 212:29–34
Kiran RP, El-Gazzaz GH, Vogel JD, Remzi FH (2010) Laparoscopic approach significantly reduces surgical site infections after colorectal surgery: data from national surgical quality improvement program. J Am Coll Surg 211:232–238
Rea JD, Cone MM, Diggs BS, Deveney KE, Lu KC, Herzig DO (2011) Utilization of laparoscopic colectomy in the United States before and after the clinical outcomes of surgical therapy study group trial. Ann Surg 254:281–288
Conflict of interest
The microbial sealant InteguSeal© was generously provided free of charge by Kimberly-Clark, Inc.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Doorly, M., Choi, J., Floyd, A. et al. Microbial sealants do not decrease surgical site infection for clean-contaminated colorectal procedures. Tech Coloproctol 19, 281–285 (2015). https://doi.org/10.1007/s10151-015-1286-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10151-015-1286-5