Abstract
Background
Although surgery is the gold standard treatment for anal fissure, the main concern remains its side effects and complications. Botulinum toxin injection and lateral internal sphincterotomy are technical options for patients suffering from chronic anal fissure. However, little is known about the efficacy of these two techniques. The aim of this meta-analysis was to compare the outcomes of botulinum toxin injection versus lateral internal sphincterotomy for chronic anal fissure.
Methods
Original studies in English were searched from the MEDLINE database, PubMed, Web of Science, and the Cochrane Library database. Randomized control trials that compared botulinum toxin injection with lateral internal sphincterotomy were identified. Data were independently extracted for each study, and a meta-analysis was performed using fixed and random effects models.
Results
Four hundred and eighty-nine patients from seven trials met the inclusion criteria. Patients undergoing lateral internal sphincterotomy had a higher-healing and incontinence rate. No statistically significant differences were noted in total complications between botulinum toxin injection and lateral internal sphincterotomy. Patients treated with lateral internal sphincterotomy had a significantly lower recurrence rate than the patients treated with botulinum toxin injection.
Conclusions
Our meta-analysis shows that lateral internal sphincterotomy was superior to botulinum toxin injection in terms of healing rate and lower recurrence rate. Botox, however, is safe associated with a lower rate of incontinence and could be used in certain situations. Further studies with a long-term follow-up are required to confirm our observations.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Anal fissure is a common disease responsible for substantial morbidity in people who are otherwise healthy [1]. Many conservative or surgical treatments have been proposed even if the clinical management of chronic anal fissures is still controversial despite several reviews [2]. Surgical procedures, such as anal dilatation, posterior midline sphincterotomy, and lateral internal sphincterotomy (LIS), have been the gold standard treatment for anal fissure [3]. However, all surgical techniques may be accompanied by significant postoperative complications, such as pain, bleeding, incontinence, and recurrence. It has been found that patients undergoing lateral internal sphincterotomy had better relief of symptoms as well as a shorter hospital stay [4]. Recently, less invasive treatment options such as botulinum toxin injection (Botox), topical nitrates, and calcium antagonists have been proposed. Chemical sphincterotomy (CS) using botulinum toxin has been reported to be associated with a lower recurrence rate and fewer side effects than CS using nitrates [5, 6]. To establish the better technique, a meta-analysis was performed by comparing botulinum toxin injection with lateral internal sphincterotomy for chronic anal fissure with regard to postoperative outcomes.
Materials and methods
Data sources
Randomized controlled trials (RCTs) that compared botulinum toxin injection with lateral internal sphincterotomy for chronic anal fissure were included in this meta-analysis. We used studies published from 1996 to August 31, 2013. A comprehensive search was performed in the MEDLINE database, PubMed, Web of Science, and the Cochrane Library database using the following search terms: “botulinum toxin,” “botulinum toxin injection,” “sphincterotomy,” “lateral internal sphincterotomy,” “anal fissure,” and “fissure-in-ano” combined with “randomized trials”. To identify all RCTs, we also included the reference list of the trials. Two independent observers (Huasheng Wang and Yijia Lin) separately identified and extracted the data.
Inclusion and exclusion criteria
Studies were included if they met the following criteria: randomized trials; comparison between botulinum toxin injection and lateral internal sphincterotomy; and published full article. All studies were published in an English language format. The reference list of all trials that met the inclusion criteria and reference list of review articles were checked for more relevant articles. For estimation of the recurrence rate of anal fissure treated with botulinum toxin, clinical trials with a follow-up for at least 6 months were included. For duplicate publications, the most complete report was selected. Trials investigating the effects of botulinum toxin in children were excluded. Retrospective trials and studies without data for retrieval publications were excluded. Unpublished trials were not included (Fig. 1).
Methodological quality
The Jadad scoring system, which evaluates studies based on appropriate randomization, proper blinding, and an adequate description of withdrawals and dropouts, was used to assess the quality of RCTs. The study was considered to be of high quality if the quality score was ≥3.
Statistical analysis
Data analysis was performed using RevMan5.0 (The Cochrane Collaboration, Oxford, UK). For continuous variables, weighted mean difference (WMD) was calculated with a 95 % confidence interval (CI), and the odds ratio (OR) with a 95 % CI was calculated for all dichotomous variables. If mean values were not available for continuous outcomes, median values were used for meta-analysis. The standard deviation (SD) was calculated according to the guidelines of “The handbook Cochrane Collaboration.” The random effect model and the fixed effect model were used to calculate the overall effect of the combined outcomes. Heterogeneity was explored using the χ 2 test, with significance set at p < 0.05. If heterogeneity was present, only the random effects model results were reported. Heterogeneity was, respectively, qualified as low, moderate, or high for I 2 values of 25, 50, and 75 %. The forest plot was then used to display the results from the meta-analysis.
Results
Four hundred and eighty-nine patients from seven randomized controlled trials were qualified for the meta-analysis [7–13]. Patient characteristics extracted from these trials and quality scores are presented in Table 1. Table 2 displays the number of studies reporting on each outcome, the total number of patients in both Botox and LIS groups, the summary statistic, 95 % CIs, the calculated p values, and a test of heterogeneity between the studies.
Healing
Since data from six trials suggested that there were no significant heterogeneity among trials regarding healing (χ 2 = 4.36, df = 5, p = 0.50, I 2 = 0 %), we used the fixed effect model. We observed a significant difference in the healing rate and hence concluded LIS is superior to Botox (OR 0.15; 95 % CI 0.08, 0.27; Z = 6.26; p < 0.00001; Fig. 2a).
Complications
There was a significant heterogeneity among trials regarding total complications (χ 2 = 20.28, df = 5, p = 0.001, I 2 = 75 %). In the random models, there were no significant difference in the total complications between the Botox and LIS groups (OR 0.55; 95 % CI 0.15, 1.94; Z = 0.93; p = 0.35; Fig. 2b).
Incontinence
No significant heterogeneity was observed among trials regarding incontinence (χ 2 = 5.24, df = 5, p = 0.53, I 2 = 0 %). In the fixed models, a significant difference was found in the incontinence between Botox and LIS group (OR 0.12; 95 % CI 0.05, 0.26; Z = 5.34; p < 0.00001; Fig. 2c). Hence, our results show Botox is better than LIS as regards incontinence.
Recurrence rate
All of the trials presented data on recurrence. There was no significant heterogeneity among trials regarding recurrence (χ 2 = 6.26, df = 6, p = 0.39, I 2 = 4 %). In the fixed models, the LIS group appeared to have a significantly lower recurrence rate than the Botox group (OR 5.97; 95 % CI 3.51, 10.17; Z = 6.58; p < 0.00001; Fig. 2d).
Discussion
Lateral internal sphincterotomy has been widely accepted as the treatment of choice for CAF [14]. However, the drawback of this surgery is potential fecal incontinence and complications such as bleeding, pain, anal abscess, or fistula [15]. Since Botox was introduced as a potential treatment for anal fissures [16], many studies have suggested encouraging results for the role of Botox in the treatment of anal fissures [17–20]. However, due to different results and unclear conclusions, controversy still exists on whether Botox is bound to replace LIS as the first-line treatment for CAF.
This meta-analysis showed that even though LIS is associated with a better healing rate and recurrence rate, Botox is superior to LIS in overall complication rates and incontinence rate. Thus, some advantages Botox offers to CAF patients include a good tolerance of the procedure, an outpatient setting, and a low risk of incontinence.
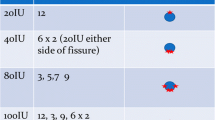
The results of this meta-analysis are in line with research from Sajid et al. and Shao et al. [21, 22]. However, our meta-analysis has some limitations. First, not only were various doses of botulinum toxin used in these studies, but various definitions of CAF were found; this suggests variability in methodology across studies and may impact interpretation of the measured pooled effect or z statistic. Secondly, none of the studies were double blinded. It is, hence, unavoidable that heterogeneity exists among studies in terms of the sample size and surgeon’s experience. Thirdly, the results of the studies included in this meta-analysis were not consistent. The total complication rate varied from 0 to 64 % among the trials, while the incontinence rate varied from 0 to 48 %. Fourthly, although the Botox group may be associated with lower rates of incontinence and LIS group appeared to have a lower recurrence rate, the long-term follow-up data are limited which makes this determination uncertain. Finally, no multicentre randomized trial was found among these studies.
Conclusions
This meta-analysis suggests that in regard to healing rate and recurrence rate, Botox is inferior to LIS for CAF. Botox may therefore be used as a first-line treatment for patients who refuse surgery, who have had previous sphincter surgery, or who are at a particular risk of incontinence with sphincterotomy [7]. In further studies, large-scale, high-quality, multicenter trials based on commonly accepted end points with a long-term follow-up are required to confirm our observations.
References
Sajid MS, Whitehouse PA, Sains P, Baig MK (2013) Systematic review of the use of topical diltiazem compared with glyceryltrinitrate for the nonoperative management of chronic anal fissure. Colorectal Dis 15:19–26
Altomare DF, Binda GA, Canuti S, Landolfi V, Trompetto M, Villani RD (2013) The management of patients with primary chronic anal fissure: a position paper. Tech Coloproctol 15:135–141
Liratzopoulos N, Efremidou EI, Papageorgiou MS et al (2006) Lateral subcutaneous internal sphincterotomy in the treatment of chronic anal fissure: our experience. J Gastrointestin Liver Dis 15:143–147
Madalinski MH, Slawek J, Zbytek B et al (2001) Topical nitrates and the higher doses of botulinum toxin for chronic anal fissure. Hepatogastroenterology 48:977–999
Lysy J, Israelit-Yatzkan Y, Sestiery-Ittah M, Weksler-Zangen S, Keret D, Goldin E (2001) Topical nitrates potentiate the effect of botulinum toxin in the treatment of patients with refractory anal fissure. Gut 48:221–224
Massoud BW, Mehrdad V, Baharak T, Alireza Z (2005) Botulinum toxin injection versus internal anal sphincterotomy for the treatment of chronic anal fissure. Ann Saudi Med 25:140–142
Iswariah H, Stephens J, Rieger N, Rodda D, Hewett P (2005) Randomized prospective controlled trial of lateral internal sphincterotomy versus injection of botulinum toxin for the treatment of idiopathic fissure in ano. ANZ J Surg 75:553–555
Valizadeh N, Jalaly NY, Hassanzadeh M et al (2012) Botulinum toxin injection versus lateral internal sphincterotomy for the treatment of chronic anal fissure: randomized prospective controlled trial. Langenbecks Arch Surg 397:1093–1098
Nasr M, Ezzat H, Elsebae M (2010) Botulinum toxin injection versus lateral internal sphincterotomy in the treatment of chronic anal fissure: a randomized controlled trial. World J Surg 34:2730–2734
Mentes BB, Irkörucu O, Akin M, Leventoglu S, Tatlicioglu E (2003) Comparison of botulinum toxin injection and lateral internal sphincterotomy for the treatment of chronic anal fissure. Dis Colon Rectum 46:232–237
Abd Elhady HM, Othman IH, Hablus MA, Ismail TA, Aboryia MH, Selim MF (2009) Long-term prospective randomised clinical and manometric comparison between surgical and chemical sphincterotomy for treatment of chronic anal fissure. S Afr J Surg 47:112–114
Arroyo Sebastian A, Perez F, Serrano P, Candela F, Lacueva J, Calpena R (2005) Surgical versus chemical (botulinum toxin) sphincterotomy for chronic anal fissure: long term results of a prospective randomized clinical and manometric study. Am J Surg 189:429–434
Poh A, Tan KY, Seow-Choen F (2010) Innovations in chronic anal fissure treatment: a systematic review. World J Gastrointest Surg 2:231–241
Ram E, Alper D, Stein GY, Bramnik Z, Dreznik Z (2005) Internal anal sphincter function following lateral internal sphincterotomy for anal fissure: a long-term manometric study. Ann Surg 242:208–211
Maria G, Cassetta E, Gui D, Brisinda G, Bentivoglio AR, Albanese A (1999) A comparison of botulinum toxin and saline for the treatment of chronic anal fissure. N Engl J Med 338:217–220
Vanella S, Brisinda G, Marniga G, Crocco A, Bianco G, Maria G (2012) Botulinum toxin for chronic anal fissure after biliopancreatic diversion for morbid obesity. World J Gastroenterol 18:1021–1027
Maria G, Brisinda G, Bentivoglio AR, Cassetta E, Gui D, Albanese A (1998) Botulinum toxin injections in the internal anal sphincter for the treatment of chronic anal fissure: long-term results after two different dosage regimens. Ann Surg 228:664–669
Brisinda G, Maria G, Bentivoglio AR, Cassetta E, Gui D, Albanese A (1999) A comparison of injections of botulinum toxin and topical nitroglycerin ointment for the treatment of chronic anal fissure. N Engl J Med 341:624
Giral A, Memisoglu K, Gultekin Y et al (2004) Botulinum toxin injection versus lateral internal sphincterotomy in the treatment of chronic anal fissure: a non-randomized controlled trial. BMC Gastroenterol 4:7
Sajid MS, Hunte S, Hippolyte S, Kiri VA, Maringe C, Baig MK (2008) Comparison of surgical vs chemical sphincterotomy using botulinum toxin for the treatment of chronic anal fissure: a meta-analysis. Colorectal Dis 10:547–552
Shao WJ, Li GC, Zhang ZH, Yang BL, Sun GD, Chen YQ (2008) Systematic review and meta-analysis of randomized controlled trials comparing stapled haemorrhoidopexy with conventional haemorrhoidectomy. Br J Surg 95:147–160
Yiannakopoulou E (2012) Botulinum toxin and anal fissure: efficacy and safety systematic review. Int J Colorectal Dis 27:1–9
Conflict of interest
None.
Author information
Authors and Affiliations
Corresponding author
Additional information
H.-L. Chen, X.-B. Woo, and H.-S. Wang are the co-first authors in this study.
Rights and permissions
About this article
Cite this article
Chen, HL., Woo, XB., Wang, HS. et al. Botulinum toxin injection versus lateral internal sphincterotomy for chronic anal fissure: a meta-analysis of randomized control trials. Tech Coloproctol 18, 693–698 (2014). https://doi.org/10.1007/s10151-014-1121-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10151-014-1121-4