Abstract
Background
The potential for malignancy in rectal polyps increases with the size of the polyp, and unexpected malignancy is reported in up to 39 % of large rectal adenomas. Transanal endoscopic microsurgery (TEM) offers the possibility of an en bloc full-thickness excision for lesions in the rectum. We present our results with TEM in the removal of giant polyps equal or greater than 4 cm in diameter.
Methods
In the period between 1998 and 2012, TEM was performed in 39 patients with rectal polyps measuring at least 4 cm in diameter. Transrectal ultrasound and/or magnetic resonance imaging of the rectum was used when cancer was suspected.
Results
The polyp was removed with en bloc full-thickness excision in 77 % (n = 30). The preoperative diagnosis was benign rectal adenoma in 89.7 % (n = 35). The median size of the polyps was 30 cm2 (range 16–100 cm2). Postoperative complications included bleeding in 4 patients (10.3 %). Histological examination showed unexpected cancer in 4 patients (10.3 %). TEM was curative in 2 of these patients, and the other 2 underwent further surgery. Recurrences occurred in 10 patients (25.6 %) and consisted of 5 adenomas and 5 adenocarcinomas. In 5 patients, these recurrences were treated with endoscopic removal or re-TEM. The remaining 5 underwent total mesorectal excision and/or chemotherapy.
Conclusions
Full-thickness TEM provides a safe and efficient treatment for excision of giant polyps. In case of unexpected cancer, TEM can be curative. Local recurrence can be often treated with a second TEM procedure.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Colorectal adenomas are considered as premalignant lesions, which precede the occurrence of rectal cancer [1]. Several factors such as the histological structure of the adenoma and size of the lesion increase the risk of the polyp developing into cancer [2]. In addition, occurrence of adenocarcinoma in polyps preoperatively assessed as benign adenomas is reported in up to 39 % of cases, despite preoperative diagnostic examinations consisting of transrectal ultrasound (TRUS) and histological evaluation of the biopsied material [3–5].
The definition of a large or giant rectal polyp is controversial and ranges from 2 to 5 cm in diameter. Moreover, many studies report on either the length or the width of the polyp, and not on both the parameters or the total size measured in cm2 [3, 4, 6]. It can therefore be difficult to determine the optimal treatment for these lesions of the rectum.
Endoscopic snare excision is an efficient technique for the removal of small colorectal polyps. However, when it comes to larger polyps, snare excision can become more difficult and other surgical techniques may be required. Conventional radical surgery is associated with procedure-related morbidity and mortality, while local treatments such as endoscopic mucosal resection (EMR), endoscopic submucosal dissection (ESD), transanal excision (TAE), and transanal endoscopic microsurgery (TEM) are preferred. TEM was primarily developed by Buess et al. [7] as a procedure for local excision of adenomas of the rectum. It has since also won the field in the treatment of early rectal cancers [8]. TEM allows for polyps to be removed by submucosal or en bloc dissection with a full-thickness rectal wall excision, which is preferred in the case of findings of incidental adenocarcinoma.
The aim of this study was to evaluate our experience with TEM in removal of giant polyps of the rectum.
Materials and methods
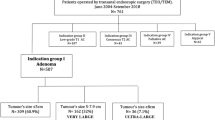
We performed a retrospective analysis of patients with rectal polyps measuring at least 4 × 4 cm, measured at pathological examination. In the period between March 1998 and March 2012, 386 TEM procedures were performed in our institution (Fig. 1). Of these, TEM was performed in 42 patients (10.9 %) with polyps measuring 4 × 4 cm or greater. Three patients who underwent conversion to conventional surgery at the start of the TEM procedures were excluded from this study. The size of the polyps in these patients was 4 × 4 cm, 7 × 5 cm, and 7.5 × 9 cm. All these patients were operated on at the beginning of our surgical experience with TEM procedure. The size and thickness of the polyps had an influence on the decision to convert when the treatment of giant polyps with TEM was still a novelty at our institution. A majority (95 %) of the 39 included patients were operated on after the year 2000, which is why experience may have played a role in determining the conversion to laparotomy. The preoperative workup prior to the TEM procedure included clinical evaluation, complete colonoscopy to exclude synchronous colonic tumors, and rigid rectoscopy to locate lesions and to measure the distance from the anal verge (AV). Multiple biopsies were taken from the lesion for histological assessment. TRUS for the assessment for the level of invasion and/or magnetic resonance imaging (MR) of the rectum for detecting potential lymph node metastases was used when cancer was suspected. The suspicion of cancer was primarily made by clinical findings (digital and endoscopic examination, e.g., fixation of the polyp and if attempted submucosal lifting failed), histological evaluation (e.g., submucosal invasion), and, if TRUS showed irregularity of the borders, hypo-echoic masses with loss of normal echo layer pattern and the presence of rounded unechoic lymph nodes.
In patients with adenocarcinoma, the decision to use TEM was made after a multidisciplinary team (MDT) conference and thoracoabdominal computed tomography (CT) scanning to exclude distant metastases, and serum carcinoembryonic antigen assays were measured before the final decision. In accordance with the guidelines from the Danish Colorectal Cancer Group (DCCG), TEM for rectal cancer without neoadjuvant treatment was only performed in T1sm1 lesions and in T1sm2–3 or T2 lesions if the patient had an increased risk of morbidity and mortality or a short expected lifetime [9].
If the post-TEM histology showed a benign rectal adenoma, the patients were followed up at regular intervals with flexible instruments 3 months after TEM, and colonoscopy a year after TEM (clean colon). If the colonoscopy showed a clean colon, the time interval between the follow-up colonoscopies was 3 years. After two clean colon colonoscopies, the follow-up colonoscopy time interval was 5 years. If the post-TEM histology showed malignancy, the patients were followed up with rectoscopy every 3 months in the first postoperative year, colonoscopy 3 months after the operation (clean colon), and then at the 3rd and 5th year postoperatively. Thoracoabdominal CT was performed at the first and 3rd year postoperatively. The follow-up regime was in accordance with the guidelines of the Danish Colorectal Cancer Group (DCCG) [9]. Data were collected retrospectively from the patient’s charts and included patient and tumor characteristics, procedural details, peri- and postoperative complications, histological data, 30-day mortality, and follow-up. Local recurrences were defined as histological findings on clinical or endoscopic examination in the rectum, at or near the previous TEM site.
Results
Patient and tumor characteristics are shown in Table 1.
Procedural details and complications
Procedural details are shown in Table 2. In total, there were 39 patients (10.1 %) included in this study, with a median age of 74 years (range 49–94 years) who underwent TEM for polyps measuring 4 × 4 cm or larger (Fig. 2). The preoperative histological diagnosis was benign rectal adenoma in 89.7 % (n = 35) and adenocarcinoma in 10.3 % (n = 4). None of the patients received neoadjuvant chemo- or radiation therapy. The tumor was removed with en bloc full-thickness excision in 76.9 % of the patients (n = 30). Partial-thickness excision was not used when the lesion was suspected of malignancy, especially above the sphincter and sometimes with minimal margins. The defect created by the TEM procedure was closed intraoperatively using a 3–0 monofilament running suture and silver clips in 35 patients (89.7 %). In 4 patients, with polyps located at 1–6 cm from the anal verge, the defect was not sutured.
Intraoperative complications occurred in one patient (2.6 %), and intraoperative bleeding was requiring intervention (n = 1). Hemostasis was achieved by placing Spongostan® (Curamedical BV, Assendelft, Netherlands) in the rectum. The patient had an uneventful postoperative course and was discharged after 2 days. We had an unexpected peritoneal perforation which was sutured during the procedure in one patient in our series. However, a peritoneal opening should not be considered as an intraoperative complication anymore today [10]. None of the procedures were converted to open surgery, and the 30-day mortality was nil. Median length of hospital stay was 1 day (range 1–6 days).
Postoperative complications occurred in 4 patients (10.3 %). The polyps in these 4 patients were removed with full-thickness excision. Two patients developed postoperative bleeding requiring intervention. One patient was treated with cauterization at the suture line with flexible sigmoidoscopy under mild sedation, and in the other, bleeding was controlled with the application of with 3 pieces of Spongostan® (Curamedical BV, Assendelft, Netherlands) and packing with a naked gauza roll which is left in situ for 24 h. These 2 patients were discharged later without any further complications. There was a deterioration of the fecal continence in 2 patients with polyps located 2 and 8 cm from the anal verge. These 2 patients were treated conservatively with a fiber-rich diet and pelvic floor muscle training, and continence function returned to baseline after 12 and 18 months, respectively. One of the well-known complications, rectal stenosis, did not occur in any of our patients.
Histological examination
As shown in Table 3, histological examination revealed that a majority of the excised lesions were adenomas (76.9 %, n = 30). There were 4 patients with unexpected malignancy (11.4 %), resulting in a total of 8 patients (20.5 %) with adenocarcinoma (Table 4). There was no lymphovascular invasion in these TEM specimens, and all of them were graded as low risk [11]. Two of the 8 patients underwent further treatment with radical surgery. One had a stage II cancer (T3) staged according to the American Joint Committee on Cancer (AJCC) staging system. This patient underwent radical surgery with low anterior resection (LAR) 5 weeks after TEM, and the final histological evaluation after total mesorectal excision (TME) showed T3N0 adenocarcinoma with 12 harvested lymph nodes. The other patient underwent LAR at another hospital, and the final pathological exam showed no residual tumor (T0N0M0); the number of the harvested lymph nodes was 15 (Table 4). These 2 patients who underwent radical surgery were alive without recurrent disease 45 and 37 months, respectively, after surgery. The rest had stage I cancer. Five of these patients did not receive further treatment as they had clear resection margins. Two of them, who staged as T2 and had severe comorbidities, were not considered to be candidates for further therapy.
Follow-up and recurrences
The patients had a median follow-up of 28 months (range 3–136 months). During that time, local recurrence occurred in 10 patients (26.3 %) (Table 5). Although TEM showed that 9 out of these 10 patients had an adenoma as a histological diagnosis following TEM, the final histological examination of the recurrences showed adenocarcinoma in 5 out of these 10 patients. Three of the patients with adenocarcinoma recurrence underwent TME as a salvage surgery: One patient underwent neoadjuvant radiation therapy and LAR. Final histological examination showed T3N1M0 adenocarcinoma with one metastatic lymph node out of a total of 9. One patient underwent APR, and the final histological examination showed T2N0M0 adenocarcinoma. One patient with T4N2M0 rectal cancer recurrence underwent APR. She refused any further treatment. Two patients with adenocarcinoma recurrences underwent palliative therapy: One patient, an 82-year-old man, had several comorbidities thus preventing major surgery, with unclear resection margins after TEM. The patient refused further follow-up after TEM and was referred to palliative chemotherapy after the recurrence was discovered, but died before treatment. The staging of his recurrence is unknown, as he refused both examination and surgical treatment for his recurrent disease. The other patient, a 78-year-old woman, developed a T4N2 adenocarcinoma recurrence, as evaluated on the pelvic MRI. She underwent re-excision of the recurrent polyp and palliative chemotherapy.
All 5 patients with benign recurrences could be treated with endoscopic removal, or with a re-TEM.
One patient, an 80-year-old woman, refused further follow-up after the TEM operation. Nineteen patients (48.7 %) died during the observation period due to causes not related to their rectal disease.
Discussion
Giant polyps represent a challenge when it comes to choosing the best treatment for the patient. Endoscopic snare excision is an excellent choice for treating small polyps. However, as the size of the polyp increases, this technique becomes more challenging and other techniques may be required. Local treatments preferred in the removal of giant rectal lesions are EMR, ESD, TAE, and TEM. TEM offers full-thickness en bloc resections for lesions in the rectum, while with EMR, the polyps are excised submucosally. An intact en bloc resection provided by resection with TEM is important in order to make a correct histological assessment of the excised polyp, which determines the further treatment plan for the patient and the follow-up program [12]. A patient with a giant polyp in our series evaluated as an adenoma preoperatively was found to have a T3 cancer with unclear resection margins. Final pathological examination following LAR showed again T3 tumor without nodal metastasis. Therefore, it is crucial to resect the whole adenoma, full-thickness with free margins. Excision of an adenoma without any suspicion of malignancy should be performed by flexible sigmoidoscopy, not TEM. All patients with giant polyps have potential malignancy and need to have a R0 resection. In our series, 30 patients had a full-thickness excision (76.9 %). The other studies examining TEM in the treatment of large and giant adenomas report full-thickness excision in 52–100 % of the cases [4, 5, 13, 14].
The size of the polyps can make it difficult to achieve clear resection margins. Our results of 17.9 % positive resection margins are comparable with other studies on the subject, which report R1 resection in 9.7–30.7 % of patients [3, 4, 13, 14], but the resection margin in some specimens could not be evaluated by the pathologist. The thermal damage due to cautery or ultrasound instruments may cause difficulties in evaluating the resection margins. Recurrence associated with R1 resections is commonly high-grade recurrence [4, 10]. Indeed, 29.4 % of our patients who did not have histological margin clearance developed recurrences, and the total recurrence rate was 26.3 % (n = 10). Five out of 10 recurrences were cancerous, even though 90 % of them had a benign TEM histology. Furthermore, unexpected cancer in lesions that appear as benign is not uncommon [2–5, 13, 15, 16]. It is therefore of great importance to create a wide resection margin (>10 mm) when performing local excision with TEM, but it can be difficult to achieve acceptable free margins in giant polyps. In addition to R1 resections, a large size of the polyp is associated with higher recurrence rates [4, 12].
Other studies on large or giant polyps report recurrence rates up to 22.6 % [3, 4, 6, 8, 12–15, 17]. However, the size of the polyps included in our study is considerably larger than in the studies mentioned, with a median size of 30 cm2 (range 16–100 cm2). Only 2 reports described giant polyps larger than 5 cm with a median size of 37 cm2 (range 14–74 cm2) and 33.4 cm2 (range 0.5–196 cm2) [3, 13]. The controversies regarding the definition of a giant polyp make it difficult to interpret and compare the outcomes of different studies in the literature.
An incomplete resection margin may moreover require further surgical treatment if adenocarcinoma cells are discovered in the preoperatively assessed benign polyp. Incidental carcinoma is found in up to 39.1 % of adenomas [1–4, 13, 15, 18] despite the use of preoperative diagnostic tools such as TRUS and serum tumor markers [3, 4]. All giant polyps should be biopsied before the final decision about treatment is made, but a benign biopsy result does not rule out adenocarcinoma as the biopsy can miss the cancerous component of the polyp due to the large volume. The advantage of TEM is that it provides an en bloc full-thickness excision and can therefore be used as a big biopsy when the clinical evaluation does not correlate with the preoperative histological assessment. In the case of incidental adenocarcinoma with T1 staging without poor prognostic factors, or in T2 staging in selected patients, the TEM resection is considered sufficient due to the risks associated with abdominal surgery and other patient-related factors. When the T staging is more advanced (≥T2) or in presence of poor prognostic factors, the patient can undergo early salvage surgery without compromising the oncological outcome [19, 20]. In our study, 4 patients (10.2 %) were diagnosed with cancer preoperatively. In 3 of these 4 patients, the TEM was curative, and the 4th patient was not physically fit to undergo major surgery. Adenocarcinoma was found in 4 other patients, with 11.4 % (4/35) rate of unexpected carcinoma in our study.
An alternative to TEM in the treatment of giant polyps is, as mentioned above, EMR, which in studies by Barendse et al. [15, 17] have been found to be associated with fewer complications than TEM. However the polyps treated with TEM were generally larger than those treated with EMR, and the excision of larger polyps is associated with more complications [3, 13, 15]. Barendse et al. [15] report on two different techniques for two completely different kinds of patients. First, patients with EMR had significantly smaller polyps than patients in the TEM series, and there were more adenocarcinomas in the TEM series which demonstrates a clear bias due to the evident selection of patients. Furthermore, incomplete resection and recurrence are a concern in treatment with EMR, especially when excision is made in a piecemeal fashion, and the early recurrence rate is significantly higher after a single treatment with EMR compared with TEM. Another treatment modality for rectal polyps is ESD, but it is a technically demanding procedure. A study by Repici et al of ESD for rectal tumors larger than 3 cm showed that the en bloc resection rate was 90 %, and the rate of curative resection (R0) was 80 %, which is comparable with the results of TEM [20]. Similar studies on ESD for rectal tumors have shown similar rates of en bloc resection and curative resection rates [21–23]. However, if the biopsies show submucosal invasion or diagnostic modalities show >T1 and if submucosal lifting failed when attempting ESD or EMR, TEM should provide safe and efficient treatment for the excision of giant polyps. The new diagnostic tools such as crystal violet chromoendoscopy and magnify/zoom endoscopy can offer targeted biopsies and better evaluation of early neoplastic lesions. In this way, for the treatment of giant rectal polyps, we have the possibility to choose the procedure best suited to the features of the single case (size, shape, spreading of the lesion).
The most frequent complication after excision of large polyps with TEM is hemorrhage, which is easily manageable. We report a perioperative complication rate of 5.1 % and postoperative complications in 4 patients (10.2 %), which is comparable with similar studies in the literature [1–4, 6, 13–15, 17]. Fifty percent of the recurrences in our study could be managed with endoscopic excision, or with a re-TEM.
Limitations of this study are its retrospective nature, along with the small number of patients included. The size of the polyps varies considerably in studies available on the subject. Therefore, in order to evaluate the outcome of TEM in treatment of giant polyps of the rectum, there is a need for further studies with polyp size inclusion criteria larger than in previous studies, along with a consensus about the definition of a giant polyp.
Conclusions
TEM, if performed en bloc and full-thickness, provides a safe and efficient treatment for excision of giant rectal polyps, with low morbidity. However, the treatment should be tailored to individual patients, ESD, EMR, or TEM, depending on the features of the single case. In the case of unexpected cancer, TEM can be curative, whereas with other local treatments, further treatment is required. Local recurrence of benign disease can be treated with local endoscopic excision or with a re-TEM in the majority of cases.
References
Winawer SJ, Zauber AG, Ho MN et al (1993) Prevention of colorectal cancer by colonoscopic polypectomy. The National Polyp Study Group. N Engl J Med 329:1977–1981
Winburn GB (1998) Surgical resection of villous adenomas of the rectum. Am Surg 64:1170–1172
Schäfer H, Baldus SE, Hölscher AH (2006) Giant adenomas of the rectum: complete resection by transanal endoscopic microsurgery (TEM). Int J Colorectal Dis 21:533–537
Allaix ME, Arezzo A, Cassoni P, Famiglietti F, Morino M (2012) Recurrence after transanal endoscopic microsurgery for large rectal adenomas. Surg Endosc 26:2594–2600
Chiavellati L, D’Elia G, Zerilli M, Tremiterra S, Stips SL (1994) Management of large malignant rectal polyps with transanal endoscopic microsurgery. Is there anything better for the patient? Eur J Surg Oncol 20:658–666
Said S, Stippel D (1995) Transanal endoscopicmicrosrugery in large, sessile adenomas of the rectum. A 10-year experience. Surg Endosc 9:1106–1112
Buess G, Huterer F, Theiss J et al (1984) A system for a transanal endoscopic rectum operation. Chirurg 55:677–680
Baatrup G, Breum B, Qvist N et al (2009) Transanal endoscopic microsurgery in 143 consecutive patients with rectal adenocarcinoma: results from a Danish multicenter study. Colorectal Dis 11:270–275
Danish Colorectal Cancer Group (DCCG) Guidelines 4th edition 2009. http://www.dccg.dk/10_English/0010_English.html
Morino M, Allaix ME, Famiglietti F, Caldart M, Arezzo A (2013) Does peritoneal perforation affect short- and long-term outcomes after transanal endoscopic microsurgery? Surg Endosc 27:181–188
Hermanek P (1989) Colorectal carcinoma: histopathological diagnosis and staging. Baillieres Clin Gastroenterol 3:511–529
McCloud JM, Waymont N, Pahwa N et al (2006) Factors predicting early recurrence after transanal endoscopic excision for rectal adenoma. Colorectal Dis 8:581–585
Scala A, Gravante G, Dastur N et al (2012) Transanal endoscopic microsurgery in small, large, and giant rectal adenomas. Arch Surg 20:1–8
Mörschel M, Heintz A, Bussman M, Junginger T (1998) Follow-up after transanal endoscopic microsurgery or transanal excision of large benign rectal polyps. Arch Surg 383:320–324
Barendse RM, van der Broek FJ, van Schooten J et al (2012) Endoscopic mucosal resection vs transanal endoscopic microsurgery for the treatment of large rectal adenomas. Colorectal Dis 14:e191–e196
Hurlstone DP, Sanders DS, Cross SS et al (2005) A prospective analysis of extended endoscopic mucosal resection for large rectal villous adenomas: an alternative technique to transanal endoscopic microsurgery. Colorectal Dis 7:339–344
Barendse RM, van der Broek FJ, Dekker E et al (2011) Systematic review of endoscopic mucosal resection versus transanal endoscopic microsurgery for large rectal adenomas. Endoscopy 43:941–955
Dell’Abate P, Iosca A, Galimberti A et al (2001) Endoscopic treatment of colorectal benign-appearing lesions 3 cm or larger. Dis Colon Rectum 44:112–118
Levic K, Bulut O, Hesselfeldt P, Bülow S (2012) The outcome of rectal cancer after early salvage TME following TEM compared with primary TME: a case-matched study. Tech Coloproctol 17:397–403
Hahnloser D, Wolff BG, Larson DW et al (2005) Immediate radical resection after local excision of rectal cancer: an oncologic compromise? Dis Colon Rectum 48:429–437
Repici A, Hassan C, Pagano N et al (2013) High efficacy of endoscopic submucosal dissection for rectal laterally spreading tumors larger than 3 cm. Gastrointest Endosc 77:96–101
Saito Y, Otake Y, Sakamoto T et al (2013) Indications for and technical aspects of colorectal endoscopic submucosal dissection. Gut Liver 7:263–269
Choi YS, Lee JB, Lee EJ et al (2013) Can endoscopic submucosal dissection technique be an alternative treatment option for a difficult giant (≥30 mm) pedunculated colorectal polyp? Dis Colon Rectum 56:660–666
Acknowledgments
The authors are indebted to Ian N. Mitchell RN for his review of this manuscript.
Conflict of interest
None.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Levic, K., Bulut, O. & Hesselfeldt, P. Transanal endoscopic microsurgery for giant polyps of the rectum. Tech Coloproctol 18, 521–527 (2014). https://doi.org/10.1007/s10151-013-1069-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10151-013-1069-9