Abstract
Background
Case reports of healthy patients experiencing total perioperative visual loss (POVL) after elective laparoscopic surgery, including colorectal resection, are appearing increasingly frequently in the literature. We reviewed the literature exploring the relationship between patient positioning and intraocular pressure (IOP) across all surgical specialties. This was then applied to the potential risk of developing POVL in patients undergoing laparoscopic colorectal surgery.
Methods
A systematic review of the relevant literature was performed to identify all studies exploring the relationship between intraocular pressure and patient positioning.
Results
Eight relevant studies on both elective patients and healthy non-anaesthetised volunteers in the spinal, neurosurgical and urological fields were identified which explore the changes in IOP according to patient positioning. These all reported significant rises in IOP in both head-down positioning and prone positioning, and the strongest effects were seen in those patients placed in combined head-down and prone position (such as prone jackknife). Rises in IOP were time-dependent in all studies.
Conclusions
Patients undergoing laparoscopic colorectal surgery in a prolonged head-down position are likely to experience raised IOP and thus are at risk of POVL. Those having a laparoscopic abdominoperineal excision with prone positioning for the perineal component are probably those in the greatest danger. Surgeons need to be aware of this under-recognised but potentially catastrophic complication.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Perioperative visual loss (POVL) in the setting of non-ocular surgery is a rare and devastating complication that has been documented after almost every type of operation. In a large cohort study of over 5.6 million operations in the USA, the incidence of POVL ranged from 0.12 per 10,000 after appendicectomy to 8.64 per 10,000 after cardiac procedures, with the risk after colorectal resection quoted as 1.24 per 10,000 (95 % CI 0.97–1.59) [1]. To put this into context, 20,035 Finished Consultant Episodes relating to colorectal resection were documented in the UK in 2008/2009 [2], suggesting that each year in the UK at least 2 patients will experience post-operative unexpected and irreversible blindness. With the rapid growth of laparoscopic surgery over the last two decades, case reports of healthy patients who unexpectedly develop partial or full blindness after elective laparoscopic surgery are appearing with increasing frequency. Cases have been reported after prostatectomy [3, 4], nephrectomy [5], inguinal hernia [6] and now colorectal resection [7]. It is not clear whether laparoscopic surgery confers any increased risk of this complication, but the extended use of head-down and prone positioning and may place the patient at increased risk.
The etiology of POVL is multifactorial and related to a complex interaction between patient, anaesthetic and surgical factors. The two most common types of POVL are anterior ischaemic optic neuropathy (AION) and posterior ischaemic optic neuropathy (PION) [8]. In these conditions, ocular perfusion is reduced. Ocular perfusion pressure is dependent on the difference between mean arterial pressure and intraocular pressure (IOP). Consequently, profound intraoperative hypotension is implicated in the development of PION and AION, and it accounts for a higher rate of POVL after spinal surgery, especially after major blood loss. However, elevation of the IOP also has the potential to deleteriously affect ocular perfusion. This may be one mechanism by which POVL develops in laparoscopic procedures.
The proportion of elective colorectal surgery undertaken laparoscopically has increased dramatically over the past decade and continues to rise each year [2]. This surgical approach is often associated with steep Trendelenburg (head-down) positioning for prolonged periods of time in order to keep the small bowel away from the operative field. The extent and duration of head-down positioning can be even more notable during the early part of a surgeon’s learning curve. Moreover, abdominoperineal resection (APER) for patients with low rectal cancer is being increasing performed in the prone jackknife position after the prolonged head-down positioning of the abdominal part of the operation. This position may further compromise the patient.
The aim of this review was to examine the literature regarding the effects of head-down and prone positioning on IOP and to draw some conclusions about the possible implications of this.
Materials and methods
Search criteria
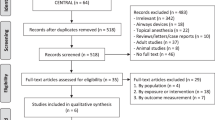
An electronic systematic search of MEDLINE, EMBASE, ISI Web of Science (including Science Citation Index and Conference Proceedings) and the Cochrane Central Register of Controlled Trials (CENTRAL) was performed for studies exploring the effects of patient positioning on intraocular pressure (IOP). The search terms used included ‘patient positioning’, ‘on-table position’, ‘head-down’, ‘Trendelenburg’, ‘reverse Trendelenburg’, ‘body inclination’, ‘prone’, ‘perioperative visual loss’, ‘intraocular pressure’, ‘ocular complications’, visual acuity’, ‘blindness’ singly or in combination. Please refer to Table 1 and Fig. 1 for more details of the study selection process. A manual search of reference lists in recent reviews and papers accepted for this study was also undertaken.
Initially, duplicate references were removed and abstracts evaluated against the inclusion criteria. Full text articles were obtained for all potentially relevant studies, and these were further assessed for suitability.
To be included, studies had to (1) give data on the actual values of intraocular pressure measurement and (2) give clear indication of the patient (or healthy volunteer) positioning at the time. No limitations on publication date or subject age were applied. Only English language studies were accepted. Controlled trials, prospective cohort studies and retrospective reviews were all eligible for inclusion. Case reports and reviews were included for background or discussion information but not for data analysis.
Data extraction
Data were extracted independently by 2 authors, and discrepancies in outcome extraction were resolved by re-examination of the relevant study until consensus was achieved. The information extracted about the study included: year of publication, setting, study design, type of operation undertaken (if appropriate), intraocular pressures, patient (or healthy volunteer) positioning at the time of pressure measurement and time-related factors in the measurement and positioning process.
Statistical analysis
Any continuous data on IOP changes amenable to pooling across multiple studies were expressed as mean ± standard deviation.
Results
Both head-down and prone jackknife positioning result in a number of well-documented physiological changes, in particular increases in IOP. However, no studies could be identified which directly quantified the effects of positioning on IOP in patients undergoing laparoscopic colorectal surgery. Nevertheless, extrapolations may be made from research in other specialities (urology, spinal and neurosurgery) which have explored the effect of patient positioning on IOP.
Intraocular pressure in the supine head-down position
Awad et al. [9] explored the effects of steep Trendelenburg positioning (25 degrees of head-down) on IOP in 33 patients undergoing robotic radical prostatectomy. Similarly, Molloy investigated a cohort of 37 patients undergoing laparoscopic prostatectomy, colonic and gynaecological surgery [3]. Both studies identified a significant rise in IOP which was strongly time-dependent. Awad et al. found a rise of 13.3 ± 0.6 mmHg after a median of 142.5 min, whilst the rise in the Molloy et al. study was 20.4 ± 10.3 mmHg.
Intraocular pressure in the prone position
Research by Lam et al. [10] showed that IOP increased from 14.1 to 20.0 mmHg after 8 min when healthy awake volunteers were moved from supine position to prone. Cheng et al. [11] undertook a similar study in anaesthetised patients undergoing elective spinal surgery in the prone position. Again, an increase in IOP was demonstrated from a supine baseline of 19 ± 1 to 40 ± 2 mmHg after a mean of 320 ± 107 min, but it was conceded that perioperative interventions and anaesthesia might have played a role in these results. An additional patient study by Hunt et al. [12] found broadly similar results.
Grant et al. [13] performed a study to determine whether the effects of head-down positioning could be ameliorated by positioning the subject in a slight head-up position. Ten healthy awake volunteers were placed prone for 5 h, then in a second session prone with a 4-degree reverse Trendelenburg (head-up) position for 5 h. As in previous studies, the IOP increased in the prone compared to baseline supine position. Values rose significantly over the 5 h up to a maximum of 154 % of baseline. Elevating the head of the bed by 4-degrees only minimally affected these readings.
Intraocular pressure in combined prone and head-down position
Ozcan et al. [14] compared the effect of two different operating tables on IOP in various different patient positions, including prone head-down position. Ten healthy volunteers attended twice and lay on each operating table in a preset sequence of positions each for 5 min with IOP measured at each stage. No significant difference was found between the two tables, but prone head-down position had a significantly higher IOP than all other positions, at 158 % of baseline values despite subjects only adopting this position for 5 min.
A second healthy volunteer study was performed by Walick et al. [15] in which 20 subjects were randomised to lie in either the flat prone position or the prone Trendelenburg position (−7-degrees of head-down tilt) for 1 h. Both groups had significantly higher IOP readings than baseline, and those in the head-down position had statistically significantly higher readings than those in flat prone. The later group reached a mean peak IOP of 37.5 ± 4.6 mmHg after 60 min. The authors concluded that the effects of prone and Trendelenburg positioning were additive.
All studies identified and presented above were deemed too heterogenous in design to be pooled together in any meta-analysis, largely due to the variable angles of head-down inclination, durations of positioning and subject types involved.
Discussion
A recent e-communication from the Association of Coloproctologists of Great Britain and Ireland (ACPGBI) was issued on the subject of patient positioning whilst under general anaesthetic, which included discussion of the possible ocular consequences arising from poor positioning [16, 17]. These complications included direct trauma to the eye by local foreign objects, or pressure upon the globe and its surroundings due to the table or headrest used. No mention is made of the role of intrinsic IOP in POVL and how patient positioning can affect this.
It can be seen from the above evidence that most laparoscopic colorectal resections involving head-down positioning will be at risk of elevated IOP and as such this adds to the risk of unexpected visual loss in this group of patients. Those undergoing laparoscopic-assisted APER may be a group at significantly higher risk if the prone position is used for the perineal dissection. Surgeons performing these operations should be aware of this potential issue and be prepared to take avoiding measures which may involve a period of flattening the patient out during long operations and limiting the head-down positioning of patients to the times where it is absolutely necessary.
The patients most likely to suffer from POVL are probably those with established glaucoma. This condition, which increases with age [18], affects 2 % of the population over 40 years old [19] and remains undiagnosed in half of those affected. In all the studies reported above, patients with pre-existing eye conditions such as glaucoma were excluded. This makes it impossible to confirm whether the pressure rises seen would be more profound or damaging in patients with an intrinsically higher baseline IOP, although we feel that this is highly likely to be the case. In glaucoma, the integrity of the optic nerve is already compromised, and the sensitivity of the nerve to pressure-related damage is increased. This is particularly the case in the elderly in whom vascular occlusion is more common. This group of elderly glaucoma sufferers would therefore appear to be the group at highest risk of POVL.
The potential vascular-occlusive effects of elevated IOP are more likely to affect those patients experiencing a period of reduced ocular perfusion pressure due to hypotension. This may be the result of hypotensive anaesthesia or an acute intraoperative hypotensive episode due to surgical misadventure. Should either of these occur during a long laparoscopic operation both the anaesthetist and surgeon should take note and be prepared to flatten out the patient for a period of time.
Conclusions
What is not yet clear is the exact nature of the relationship between the degree and duration of patient tilt and IOP—accurate quantitative research exploring these variables in this specific cohort of patients undergoing these colorectal operations is needed. This research may lead to the production of guidelines outlining that the maximum recommended period patients should spend in certain positions on the theatre table. Until this point, we suggest surgeons take note of these emerging case reports and the already available evidence regarding the effect of patient positioning on IOP.
References
Shen Y, Drum M, Roth S (2009) The prevalence of perioperative visual loss in the United States: a 10-year study from 1996 to 2005 of spinal, orthopaedic, cardiac, and general surgery. Anaesth Analg 109:1534–1545
NICE implementation uptake report: Laparoscopic surgery for the treatment of colorectal cancer. NICE technology appraisal 105
Molloy BL (2011) Implications for postoperative visual loss: steep Trendelenburg position and effects on intraocular pressure. AANA J 79:115–121
Weber ED, Colyer MH, Lesser RL, Subramanian PS (2007) Posterior ischemic optic neuropathy after minimally invasive prostatectomy. J Neuro-Opthalmol 27:285–287
Metwalli AR, Davis RG, Donovan JF (2004) Visual impairment after laparoscopic donor nephrectomy. J Endourol 18:888–890
Stoffelns BM (2009) Decreased visual acuity and loss of field of vision after inguinal hernia surgery (German). Der Opthalmologie 106:448–451
Mizrahi H, Hugkulstone CE, Vyakarnam P, Parker MC (2011) Bilateral ischaemic optic neuropathy following laparoscopic proctocolectomy: a case report. Ann R Coll Surg Engl 93:E53–E54
Berg KT, Harrison AR, Lee MS (2010) Perioperative visual loss in ocular and nonocular surgery. Clin Opthal 4:531–546
Awad H, Santilli S, Ohr M et al (2009) The effects of steep trendelenburg positioning on intraocular pressure during robotic radical prostatectomy. Anesth Analg 109:473–478
Lam AK, Douthwaite WA (1997) Does the change of anterior chamber depth or/and episcleral venous pressure cause intraocular pressure change in postural variation? Optom Vis Sci 74:664–667
Cheng MA, Todorov A, Tempelhoff R, McHugh T, Crowder CM, Lauryssen C (2001) The effect of prone positioning on intraocular pressure in anesthetized patients. Anesthesiology 95:1351–1355
Hunt K, Bajekal R, Calder I, Meacher R, Eliahoo J, Acheson JF (2004) Changes in intraocular pressure in anaesthetized prone patients. J Neurosurg Anaesthesiol 16:287–290
Grant GP, Szirth BC, Bennet HL et al (2010) Effects of prone and reverse trendelenburg positioning on ocular parameters. Anesthesiology 112:57–65
Ozcan MS, Praetel C, Bhatti T, Gravenstein N, Mahla ME, Seubert CN (2004) The effect of body inclination during prone positioning on intraocular pressure in awake volunteers: a comparison of two operating tables. Anesth Analg 99:1152–1158
Walick KS, Kragh JE, Ward JA, Crawford JJ (2007) Changes in intraocular pressure due to surgical positioning. Spine 32:2591–2595
Hazards of patient positioning for surgery (2011) Retrieved 3 Sept 2011, from http://www.acpgbi.org.uk/news/anaesthesia
Knight DJW, Mahajan RP (2004) Patient positioning in anaesthesia. Continuing education in Anaesthesia. Critical Care Pain 4:160–163
Rudnicka AR, Mt-Isa S, Owen CG, Cook DG, Ashby D (2006) Variations in primary open-angle glaucoma prevalence by age, gender, and race: a Bayesian meta-analysis. Invest Ophthalmol Vis Sci 47:4254–4261
Tielsch JM, Sommer A, Katz J, Royall RM, Quigley HA, Javitt J (1991) Racial variations in the prevalence of primary open-angle glaucoma. The Baltimore Eye Survey. JAMA 266:369–374
Conflict of interest
None declared.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Pinkney, T.D., King, A.J., Walter, C. et al. Raised intraocular pressure (IOP) and perioperative visual loss in laparoscopic colorectal surgery: a catastrophe waiting to happen? A systematic review of evidence from other surgical specialities. Tech Coloproctol 16, 331–335 (2012). https://doi.org/10.1007/s10151-012-0879-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10151-012-0879-5