Abstract
Background
The aim of this study was to systematically analyse the clinical trials on the effectiveness of transanal haemorrhoidal de-arterialisation (THD) and stapled haemorrhoidopexy (SH) in the management of haemorrhoidal disease (HD).
Methods
Clinical trials on the effectiveness of THD and SH in the management of HD were analysed systematically using RevMan®, and combined outcomes were expressed as risk ratio (RR) and mean difference (MD).
Results
Three randomised, controlled trials encompassing 150 patients were analysed systematically. There were 80 THD patients and 70 SH patients. There was no significant heterogeneity (P = 0.40) among included trials. Therefore, in the fixed effects model, THD and SH were statistically equivalent in terms of treatment success rate (P = 0.19), operation time (P = 0.55), postoperative complications (P = 0.11) and recurrence (P = 0.46) of HD. THD was associated with significantly less postoperative pain (MD, −2.00; 95% CI, −2.06, −1.94; z = 63.59; P < 0.00001) compared to SH.
Conclusions
Both THD and SH are equally effective and can be attempted for the management of HD. However, THD is associated with significantly lesser postoperative pain and therefore may be considered a preferred procedure. This conclusion is based only on treating 150 patients by THD or SH in three moderate-quality randomised trials. A major, multicenter, randomised trial is required to validate this conclusion and investigate other variables like hospital stay, cost-effectiveness and health-related quality of life measurement.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Haemorrhoidal disease (HD) is the most common type of anorectal disorder seen in the proctology clinic [1]. The incidence of rectal bleeding as a consequence of colorectal pathologies is about 20% per year in Western nations and is mostly due to the HD. The prevalence of HD ranges from 4.4 to 86% [1–4]. Multicenter, randomised, clinical trials have demonstrated that conventional haemorrhoidectomy including the Milligan–Morgan and Ferguson methods and their modifications are associated with numerous complications. The major complications include sphincter dysfunction in up to 25% of patients, pain severe enough to prevent patients from working for up to 3 weeks in 75%, bleeding in 5–15% and up to 30% risk of recurrent disease [4]. Rubber band ligation [5] has been proven to be effective in the treatment for internal haemorrhoids but virtually ineffective for treating fourth-degree HD. The suture technique revived by Farag [6] and its modifications [7, 8] have failed to gain widespread acceptance because they are directed mainly at reduction in blood flow to haemorrhoidal cushions, which is associated with initial painful congestion followed by gradual shrinkage of prolapsed haemorrhoids. Similarly, injection sclerotherapy, photocoagulation and cryosurgery have been found to be effective but with low success rates and high recurrence rates [9–13]. Stapled haemorrhoidopexy (SH) has been reported to be a viable and highly effective alternative compared to other invasive approaches for the management of HD [14–17]. However, a recently published Cochrane Review of 23 randomised controlled trials [18] concluded that SH was not superior to conventional haemorrhoidectomy and its modifications. SH has also been reported to be an expensive procedure, and it is associated with a higher incidence of severe postoperative pain and anal stricture formation than other invasive techniques [19]. Because of a variable success rate, significant postoperative complications and a higher incidence of long-term recurrence following the use of these modalities for the management of HD, efforts are constantly being made to develop an effective and minimally invasive technique to treat haemorrhoids. In 1995, a new technique for the surgical treatment [20, 21] of haemorrhoids called haemorrhoidal artery ligation or transanal haemorrhoidal de-arterialisation (THD) was introduced. This procedure eliminates haemorrhoidal symptoms by ligating the terminal haemorrhoidal branches of the superior haemorrhoidal artery with the help of a specially designed proctoscope (anoscope) coupled with a Doppler probe to aid location of the vessels. Vessel ligation results in the decongestion of haemorrhoidal tissue. This decreased tension allows regeneration of connective tissue within the anal cushions. This in turn facilitates the shrinkage of the piles, reduction in the prolapse and alleviation of symptoms. Since 1995, THD has been evaluated in many case series [1, 4, 22–33] and three randomised controlled trials [34–36]. Currently, both PPH and THD are being investigated quite extensively to evaluate their clinical success to treat HD in terms of postoperative pain, relief of symptoms and recurrence rate. The aim of this review is to systematically analyse the clinical trials on the effectiveness of THD and SH in the management of HD by using the principles of meta-analysis.
Materials and methods
Relevant prospective randomised, controlled trials (irrespective of type, language, blinding, sample size or publication status) on the use of THD versus SH for the management of HD of any grade published before May 2011 were included in this review. The Cochrane Colorectal Cancer Group (CCCG) Controlled Trial Register, the Cochrane Central Register of Controlled Trials (CENTRAL) in the Cochrane Library, Medline, EMBASE and Science Citation Index Expanded were searched until May 2011 using the medical subject headings (MeSH) “haemorrhoids”, “prolapsing haemorrhoids”, and “haemorrhoidal disease” in combination with “surgical treatment”, “stapled haemorrhoidopexy”, “procedure for prolapse and haemorrhoids”, “transanal haemorrhoidal de-arterialisation”, “haemorrhoidal artery ligation” and “anopexy coupled with Doppler probe”. The “related article” function was used to widen the search criteria. All abstracts, comparative studies, non-randomised trials and citations scanned were reviewed in order to get the maximum results from a comprehensive literature search. A filter for identifying relevant studies recommended by the Cochrane Collaboration [37] was used to filter out irrelevant studies in Medline and Embase. The references from the included studies were searched to identify additional trials. Two authors independently identified the relevant studies for inclusion, extracted the data related to the outcomes and secured data on the Microsoft Excel spread sheet. Any conflict about data was resolved by mutual agreement among the authors. The software package RevMan 5.0.1 [38] provided by the Cochrane Collaboration was used for the statistical analysis. The risk ratio (RR) with a 95% confidence interval (CI) was calculated for binary data variables. Summated outcome of the continuous variables was expressed as mean difference (MD). If the standard deviation was not available, then it was calculated according to the guidelines of the Cochrane Collaboration [37]. This process involved the assumptions that both groups had the same variance, which may not have been true, and variance was estimated either from the range or from the P-value. The estimate of the difference between both techniques was pooled, depending upon the effect weights in results determined by each trial estimate variance. The random effects model [39] and the fixed effect model [40] were used to calculate the combined outcome in case of both binary and continuous variables. In case of heterogeneity, only the results of the random effects model were reported. Heterogeneity was explored using the χ2 test, with significance set at P < 0.05, and was quantified [41] using I 2, with a maximum value of 30 per cent identifying low heterogeneity [37]. The Mantel–Haenszel method was used for the calculation of RR under the fixed effect model, and the DerSimonian/Laired method was used for the calculation of RR under the random effect model [42]. In a sensitivity analysis, 0.5 was added to each cell frequency for trials in which no event occurred in either the treatment or control group, according to the method recommended by Deeks et al. [43]. The estimate of the difference between both techniques was pooled depending upon the effect weights in results determined by each trial estimate variance. The forest plot was used for the graphical display of the results from the meta-analysis. The square around the estimate stood for the accuracy of the estimation (sample size), and the horizontal line represented the 95% CI.
Results
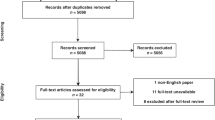
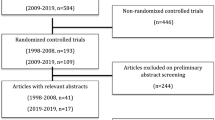
The PRISMA flow chart to explain the study methodology, literature search and trial selection is given in Fig. 1. Three randomised, controlled trials [34–36], encompassing 150 patients, who underwent THD or SH for HD of any degree were retrieved from the electronic databases. Eighty patients underwent THD and 70 patients underwent SH. Variables used to achieve a combined outcome are given in Table 1.
Methodological quality of included studies
The methodological quality of the included trials was initially assessed by the published guideline of Jadad et al. and Chalmers et al. [44, 45]. All trials were of moderate strength according to these criteria. Based on the quality of included randomised controlled trials, the strength and summary of evidence was further evaluated by GradePro® [46], a statistical tool provided by the Cochrane Collaboration (Fig. 2). The Mantel–Haenszel fixed effect model was used to compute robustness and susceptibility to any outlier among these trials. The allocation concealment and blinding of investigator or assessor were not clearly reported in most of the trials evaluating surgical procedures. Therefore, qualitatively, the results of this review may be considered relatively weak, but realistically, they may be considered moderate-quality evidence. There was no statistically significant heterogeneity (clinical and methodological diversity) among trials.
Treatment success rate
There was no heterogeneity [χ2 = 0.90, df = 2, (P = 0.64); I 2 = 0%] among trials. Therefore, in the fixed effects model, treatment success rate following THD was higher compared to SH but statistically (RR, 0.92; 95% CI, 0.81, 1.04; z = 1.31; P = 0.19; Fig. 3), it was not significant. Therefore, both techniques may be considered equally effective in the management of HD.
Operative time
Two trials [35, 36] contributed to the combined calculation of this outcome. There was no heterogeneity [χ2 = 0.13, df = 1, (P = 0.72); I 2 = 0%] among trials. Therefore, in the fixed effects model, the operation time for THD was shorter compared to SH, but statistically (MD, −2.20; 95% CI, −9.36, 4.97; z = 0.60; P = 0.55; Fig. 4), it was not significant.
Postoperative complications
There was no heterogeneity [χ2 = 0.45, df = 2, (P = 0.80); I 2 = 0%] among trials. By using the fixed effects model, THD was associated with fewer postoperative complications compared to the SH, but statistically (RR, 0.48; 95% CI, 0.20, 1.18; z = 1.80; P = 0.11; Fig. 5), this was not significant. Therefore, both techniques may be considered equally effective in the management of HD.
Postoperative pain
There was no heterogeneity [χ2 = 0.52, df = 2, (P = 0.77); I 2 = 0%] among trials. Postoperative pain following THD was significantly lower compared to SH (MD, −2.00; 95% CI, −2.06, −1.94; z = 63.61; P < 0.00001; Fig. 6) using the fixed effects model.
Recurrence of haemorrhoids
There was no heterogeneity [χ2 = 1.95, df = 2, (P = 0.38); I 2 = 0%] among trials. Therefore, in the fixed effects model, THD was associated with a higher incidence of HD recurrence as compared to SH, but statistically (RR, 1.33; 95% CI, 0.62, 2.84; z = 0.74; P = 0.46; Fig. 7), it was not significant. Both techniques may be considered equally effective in the management of HD.
Discussion
Based on this review of three randomised, controlled trials conducted on 150 patients with symptomatic HD, THD is as effective as SH in terms of treatment success rate, operation time, postoperative complications and incidence of HD recurrence. In addition, THD is also associated with significantly less postoperative pain compared to SH. On the evaluation of published case series each with more than 100 patients undergoing THD, the authors found this outcome was comparable to SH for treatment success rate, relief of symptoms and recurrence. There were 14 reported case series [1, 4, 22–33] on THD (Table 2) encompassing 2,902 patients. The reported relief of symptoms after THD varied from 71 to 96%. The disease cure rate was reported to be between 80 and 96%. The isolated symptom control rate was 70–97.5% for pain, 88–91% for rectal bleeding and 92–94% for prolapse. A recently published systematic review of 17 articles including a total of 1,996 patients reported a wide range of operative times for THD (5–50 min). In the majority of cases, the procedure could be performed as a day-case procedure. The overall recurrence rate was 9.0% for prolapse, 7.8% for bleeding and 4.7% for pain at defecation. The recurrence rate at 1 year or more was 10.8% for prolapse, 9.7% for bleeding and 8.7% for pain at defecation. When reported as a function of the haemorrhoidal grade, the recurrence rate was higher for fourth-degree haemorrhoids (range, 11.1–59.3%) [47]. A randomised trial [48] comparing THD with conventional haemorrhoidectomy concluded that the advantages of THD were the following: day-case procedure, less pain, early return to work and minimally invasive. No comparison of THD with rubber band ligation in the management of HD has been reported. However, one would assume that THD is superior to rubber band ligation because of a lower recurrence rate (approximately 18% vs. 85%) [49], a higher cure rate [49] and less postoperative pain [50].
There are several limitations to this review. First, the study by Ramirez et al. [36] is published as an abstract only. It had substantial influence on the combined risk ratio and effect weight of the meta-analysis (39.5%). Considering it is a relatively low-quality randomised trial investigating THD, SH and CH, it may be considered a potential source of contamination of the overall outcome. Second, the quality of included trials was not necessarily high due to the lack of adequate randomisation technique, allocation concealment, single or double blinding, intention-to-treat analysis and power of the study calculations, which are potential sources of higher degree of bias. Third, there were significant differences about inclusion (e.g. degree of haemorrhoids, presence of external haemorrhoids and presence of peri-anal skin tags) and exclusion criteria among included trials. Fourth, varying degrees of differences also exist among included trials concerning the definitions of “treatment success rate”, “symptom relief rate” and “measurement scales for postoperative pain”. Fifth, studies recruiting a very small number of patients in this review may not have been large enough to make possible the identification of small differences between THD and SH. Lastly, because there was no difference in primary outcomes (treatment success rate, postoperative pain, postoperative complications, operative time and recurrence rate) between the two techniques, type of investigated variable in included trials should have been made after taking into account the importance of other outcomes such as overall mortality, length of hospital stay, measurement of health-related quality of life and cost analysis.
Conclusions
To the best of our knowledge, this is the first meta-analysis exploring the role of THD in the management of HD. Although the conclusion of this review based upon the strength of the evidence may be considered weak, we believe this article will pave the way for further investigation of THD in the form of a major, multicenter, randomised, controlled trial. Meanwhile, this review may provide some evidence to help colorectal surgeons in decision making about the type and technique of surgical intervention for the management of HD.
References
Dal Monte PP, Tagariello C, Saragò M et al (2007) Transanal haemorrhoidal dearterialisation: nonexcisional surgery for the treatment of haemorrhoidal disease. Tech Coloproctol 11:333–338
Jayaraman S, Colquhoun PH, Malthaner RA (2007) Stapled hemorrhoidopexy is associated with a higher long-term recurrence rate of internal hemorrhoids compared with conventional excisional hemorrhoid surgery. Dis Colon Rectum 50:1297–1305
Carapeti EA, Kamm MA, McDonald PJ, Phillips RK (1998) Double-blind randomised controlled trial of effect of metronidazole on pain after day-case haemorrhoidectomy. Lancet 351:169–172
Ortiz H, Marzo J, Armendariz P (2002) Randomized clinical trial of stapled haemorrhoidopexy versus conventional diathermy haemorrhoidectomy. Br J Surg 89(11):1376–1381
Wrobleski DE, Corman ML, Veidenheimer MC, Coller JAL (1980) Long-term evaluation of rubber ring ligation in hemorrhoidal disease. Dis Colon Rectum 23:478–482
Farag EA (1978) Pile suture: a new technique for treatment of haemorrhoids. Br J Surg 65:293–295
Awojobi OA (1983) Modified pile suture in the outpatient treatment of haemorrhoids: a preliminary report. Dis Colon Rectum 26:96–97
Serdev N (1990) The surgical treatment of haemorrhoids: their suturing ligation without excision. Khirusgiia 43:65–68
Schulte T, Fändrich F, Kahlke V (2008) Life-threatening rectal necrosis after injection sclerotherapy for haemorrhoids. Int J Colorectal Dis 23:725–726
Marques CF, Nahas SC, Nahas CS, Sobrado CW Jr, Habr-Gama A, Kiss DR (2006) Early results of the treatment of internal hemorrhoid disease by infrared coagulation and elastic banding: a prospective randomized cross-over trial. Tech Coloproctol 10:312–317
Ricci MP, Matos D, Saad SS (2008) Rubber band ligation and infrared photocoagulation for the outpatient treatment of hemorrhoidal disease. Acta Cir Bras 23:102–106
Gupta PJ (2007) Infra red photocoagulation of early grades of hemorrhoids—5-year follow-up study. Bratisl Lek Listy 108:223–226
Tajana A, Chiurazzi D, De Lorenzi I (1995) Infrared photocoagulation, cryosurgery and laser surgery in hemorrhoidal disease. Ann Ital Chir 66:775–782
Longo A (1998) Treatment of haemorrhoidal disease by reduction of mucosa and haemorrhoidal prolapse with circular suturing device: a new procedure. In: Proceedings of the 6th world congress of endoscopic surgery, Monduzzi Editore, Bologna, pp 777–784
Ortiz H, Marzo J, Armendáriz P, De Miguel M (2005) Stapled hemorrhoidopexy vs. diathermy excision for fourth-degree hemorrhoids: a randomized, clinical trial and review of the literature. Dis Colon Rectum 48:809–815
Sakr MF, Moussa MM (2010) LigaSure hemorrhoidectomy versus stapled hemorrhoidopexy: a prospective, randomized clinical trial. Dis Colon Rectum 53:1161–1167
Gravié JF, Lehur PA, Huten N et al (2005) Stapled hemorrhoidopexy versus milligan-morgan hemorrhoidectomy: a prospective, randomized, multicenter trial with 2-year postoperative follow up. Ann Surg 242:29–35
Jayaraman S, Colquhoun PH, Malthane R et al (2006) Stapled versus conventional surgery for haemorrhoids. Cochrane Database Syst Rev (4):CD005393. doi:10.1002/14651858.CD005393.pub2
Seow-Choen F (2001) Stapled haemorrhoidectomy: pain or gain. Br J Surg 88:1–3
Morinaga K, Hasuda K, Ikeda T (1995) A novel therapy for internal hemorrhoids: ligation of the hemorrhoidal artery with a newly devised instrument (Moricorn) in conjunction with a Doppler flowmeter. Am J Gastroenterol 90:610–613
Sohn N, Aronoff JS, Cohen FS, Wernstein MA (2001) Transanal hemorrhoidal dearterialization is an alternative to operative hemorrhoidectomy. Am J Surg 182:515–519
Faucheron JL, Poncet G, Voirin D, Badic B, Gangner Y (2011) Doppler-guided hemorrhoidal artery ligation and rectoanal repair (HAL-RAR) for the treatment of grade IV hemorrhoids: long-term results in 100 consecutive patients. Dis Colon Rectum 54:226–231
Ratto C, Donisi L, Parello A et al (2010) Evaluation of transanal hemorrhoidal dearterialization as a minimally invasive therapeutic approach to hemorrhoids. Dis Colon Rectum 53:803–811
Theodoropoulos GE, Sevrisarianos N, Papaconstantinou J et al (2010) Doppler-guided haemorrhoidal artery ligation, rectoanal repair, sutured haemorrhoidopexy and minimal mucocutaneous excision for grades III-IV haemorrhoids: a multicenter prospective study of safety and efficacy. Colorectal Dis 12:125–134
Pol RA, van der Zwet WC, Hoornenborg D et al (2010) Results of 244 consecutive patients with hemorrhoids treated with Doppler-guided hemorrhoidal artery ligation. Dig Surg 27:279–284
Infantino A, Bellomo R, Dal Monte PP et al (2010) Transanal haemorrhoidal artery echodoppler ligation and anopexy (THD) is effective for II and III degree haemorrhoids: a prospective multicentric study. Colorectal Dis 12:804–809
Wilkerson PM, Strbac M, Reece-Smith H, Middleton SBL (2009) Doppler-guided haemorrhoidal artery ligation: long-term outcome and patient satisfaction. Colorectal Dis 11:394–400
Greenberg R, Karin E, Avital S, Skornick Y, Werbin N (2006) First 100 cases with Doppler-guided hemorrhoidal artery ligation. Dis Colon Rectum 49:485–489
Scheyer M, Antonietti E, Rollinger G, Mall H, Arnold SL (2006) Doppler-guided hemorrhoidal artery ligation. Am J Surg 191:89–93
Narro JL (2004) Hemorrhoid therapy with Doppler guided hemorrhoidal artery ligation via proctoscope KM-25. A new alternative to hemorrhoidectomy and rubber band ligation? Zentralbl Chir 129:208–210
Lienert M, Ulrich B (2004) Doppler-guided ligation of the hemorrhoidal arteries. Report of experiences with 248 patients. Dtsch Med Wochenschr 129:947–950
Tagariello C, Dal Monte PP, Saragò M (2004) Doppler-guided transanal haemorrhoidal dearterialisation. Chir Ital 56:693–697
Arnold S, Antonietti E, Rollinger G, Scheyer M (2002) Doppler ultrasound assisted hemorrhoid artery ligation. A new therapy in symptomatic hemorrhoids. Chirurg 73:269–273
Festen S, van Hoogstraten MJ, van Geloven AA, Gerhards MF (2009) Treatment of grade III and IV haemorrhoidal disease with PPH or THD. A randomized trial on postoperative complications and short-term results. Int J Colorectal Dis 24:1401–1405
Giordano P, Nastro P, Davies A, Gravante G (2011) Prospective evaluation of stapled haemorrhoidopexy versus transanal haemorrhoidal dearterialisation for stage II and III haemorrhoids: three-year outcomes. Tech Coloproctol 15:67–73
Ramirez JM, Gracia JA, Aguilella V et al (2005) Surgical management of symptomatic haemorrhoids: to cut, to hang or to strangulate? A prospective randomized controlled trial. Colorectal Dis 7:52
Higgins JPT, Green S (eds) (2011) Cochrane handbook for systematic reviews of interventions version 5.0.0 (updated February 2008). The Cochrane Collaboration, 2008; http://www.cochrane-handbook.org. Accessed 15 April 2008
Review Manager (RevMan) (2008) [Computer program]. Version 5.0. The Nordic Cochrane Centre, The Cochrane Collaboration, Copenhagen
DerSimonian R, Laird N (1986) Meta-analysis in clinical trials. Control Clin Trials 7:177–188
DeMets DL (1987) Methods for combining randomized clinical trials: strengths and limitations. Stat Med 6:341–350
Higgins JP, Thompson SG (2002) Quantifying heterogeneity in a meta-analysis. Stat Med 21:1539–1558
Egger M, Smith GD, Altman DG (2006) Systematic reviews in healthcare. BMJ Publishing, London
Deeks JJ, Altman DG, Bradburn MJ (2001) Statistical methods for examining heterogeneity and combining results from several studies in meta-analysis. Systemic reviews in health care: meta-analysis in context, 2nd edn. BMJ Publication group, London
Jadad AR, Moore RA, Carroll D et al (1996) Assessing the quality of reports of randomized clinical trials: is blinding necessary? Control Clin Trials 17:1–12
Chalmers TC, Smith H Jr, Blackburn B et al (1981) A method for assessing the quality of a randomized control trial. Control Clin Trials 2:31–49
http://ims.cochrane.org/revman/other-resources/gradepro/download. Accessed 30 April 2011
Giordano P, Overton J, Madeddu F, Zaman S, Gravante G (2009) Transanal hemorrhoidal dearterialization: a systematic review. Dis Colon Rectum 52:1665–1671
Bursics A, Morvay K, Kupcsulik P, Flautner L (2004) Comparison of early and 1-year follow-up results of conventional hemorrhoidectomy and hemorrhoid artery ligation: a randomized study. Int J Colorectal Dis 19:176–180
Lewis AAM, Rogers HS, Leighton M (1983) Trial of maximal anal dilatation, cryotherapy and elastic band ligation as alternatives to haemorrhoidectomy in the treatment of large prolapsing haemorrhoids. Br J Surg 70:54–56
Shanmugam V, Hakeem A, Campbell KL et al (2005) Rubber band ligation versus excisional haemorrhoidectomy for haemorrhoids. Cochrane Database Syst Rev (1):CD005034. doi:10.1002/14651858.CD005034.pub2
Conflict of interest
None to declare.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Sajid, M.S., Parampalli, U., Whitehouse, P. et al. A systematic review comparing transanal haemorrhoidal de-arterialisation to stapled haemorrhoidopexy in the management of haemorrhoidal disease. Tech Coloproctol 16, 1–8 (2012). https://doi.org/10.1007/s10151-011-0796-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10151-011-0796-z