Abstract
Aim
The aim of this experimental study is the assessment of the effects of the immediate post-operative intraperitoneal administration of 5-fluorouracil and irinotecan on the healing process of large bowel anastomoses in rats.
Materials and methods
Sixty male Wistar rats were divided into 4 groups of 15 rats each. The rats underwent large bowel resection and anastomosis, followed by the intraperitoneal administration of normal saline (group 1), 5-fluorouracil (group 2), irinotecan (group 3) or the combination of 5-fluorouracil and irinotecan (group 4). All animals were killed on the eighth post-operative day. During post-mortem examination, the anastomoses were assessed macroscopically for a possible anastomotic leak and the extent of adhesion formation. Subsequently, the anastomotic bursting pressure was measured, and the anastomoses were assessed histologically.
Results
No anastomotic dehiscence was observed in the rats of group 1. In groups 2 and 3, we observed 3 anastomotic leaks in each group, and in group 4, we observed 5 leaks (P = 0.111). The mean bursting pressure of the anastomoses in group 1 was significantly higher compared to groups 2, 3 and 4 (P < 0.001). The least inflammatory cell infiltration score was observed in group 1 (P < 0.001). The lowest neoangiogenesis score was observed in group 2 and the highest in group 4. The collagen formation in group 1 was significantly higher compared to the other 3 groups (P < 0.001). Similar results were observed for the fibroblast activity, where group 1 revealed significantly higher fibroblast scores compared to groups 2, 3 and 4 (P < 0.001). Finally, groups 2, 3 and 4 showed significantly lower hydroxyproline levels compared to the control group (P < 0.001).
Conclusion
The immediate, post-operative intraperitoneal administration of 5-fluorouracil or irinotecan had a negative effect on the healing process of the large bowel anastomoses in rats. The negative effects of the combination of 5-fluorouracil and irinotecan were statistically more significant compared to the single use of 5-fluorouracil or irinotecan.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
It has been proven that intraperitoneal administration of chemotherapeutic agents destroys possible micrometastases, as well as cancer cells, that disseminate intraoperatively, and which can cause local recurrence, peritoneal carcinomatosis or liver metastases. Nevertheless, the intraperitoneal administration of agents can impair the healing process of the anastomoses [1–5].
Aim of this study was to assess the effects of the intraperitoneal administration of combined 5-fluorouracil with irinotecan on the healing process of large bowel anastomoses in rats.
Materials and methods
Sixty male Wistar rats were used for this study. All principles of laboratory animal care were followed. The animals were weighed on the day of the operation and before sacrifice. During surgery, a 1-cm colonic segment was resected 10 cm distally of the ileocecal valve. After the resection, an end-to-end anastomosis was performed using 8 interrupted sutures (6/0 polypropylene).
Before the operation, the rats were randomized in four groups. The drug dosages and frequency of administration were guided by internationally accepted treatment regimens of these drugs. Group 1 (control group): The rats received intraperitoneal normal saline (3 ml) intraoperatively, as well as on the first post-operative day. Group 2 (5-FU group): The rats received intraperitoneal 5-FU (20 mg/kg BW) intraoperatively, as well as on the first post-operative day. Group 3 (irinotecan group): The rats received intraperitoneal irinotecan (3 mg/kg BW) intraoperatively. Group 4 (combination group): The rats received intraperitoneal 5-FU (20 mg/kg BW) and irinotecan (3 mg/kg BW) intraoperatively. On the first post-operative day, they received intraperitoneal 5-FU (20 mg/kg BW).
Sacrifice and macroscopic assessment
All animals were killed on the eighth post-operative day, using intraperitoneal pentothal (300 mg/kg BW). Immediately after the killing, the anastomosis was assessed macroscopically for the presence or not of an anastomotic leak. The presence of abscesses at the anastomotic site and the extent of adhesions were also recorded. All observations were performed in a blind fashion by two examiners. The extent of adhesions was assessed using the scale of van der Hamm et al. [1] as follows: 0 = no adhesions, 1 = minimal adhesions, e.g. between anastomosis and the omentum, 3 = moderate adhesions, e.g. between anastomosis and a small bowel loop, 4 = extensive adhesions with the formation of perianastomotic abscess.
Bursting pressure and histological assessment
After sacrifice, a 5-cm segment of the transverse colon with the anastomosis at the centre was carefully resected along with the adhesions that had been formed. After this bowel segment was washed, the bursting pressure (meaning the pressure at which any leakage of saline or gross rupture of the bowel was noted) was measured, using a three-way catheter. Following the bursting pressure measurement, a 1-cm segment of the bowel with the anastomosis in the middle was resected. That segment was incised longitudinally and divided into two equal parts. The first part was placed in 4% formalin solution and was sent for histological evaluation, using the scale of Ehrlich and Hunt from 0 to 4, as modified by Philips et al. [2]. The grading was as follows: 0 = no evidence, 1 = occasional evidence, 2 = light scattering, 3 = abundant evidence and 4 = confluent cells or fibres. The histological assessment included inflammatory cell infiltration (white blood cell count), neoangiogenesis (new blood vessel development), fibroblast activity and collagen deposition. All histological assessments were carried out in a blind fashion by an experienced histopathologist. The second segment was used for the measurement of hydroxyproline. The process of the hydroxyproline measurement is described in relevant literature.
Statistical analysis
Continuous variables were summarized using means with 95% confidence intervals and medians with ranges from minimum to maximum. Plots were used for the graphical presentation of the results. For the analysis of the anastomotic leaks, the Fisher’s exact test and the χ2 test were employed. Differences amongst groups, with respect to non-normally distributed parameters, were tested using the Kruskal–Wallis test, whereas pairwise differences were compared using the Mann–Whitney test, at a Bonferroni-adjusted significance level. All reported P values were two-tailed with P < 0.05 considered as significant. The Bonferroni correction used with the Mann–Whitney test increased the statistical threshold at a P value of 0.008. All analyses were conducted using SPSS 12.0.
Results
None of the animals died before the 8th post-operative day. The anastomotic leak frequency is presented in Fig. 1 (P = 0.111).
Adhesion formation
Group 1 was the only group with anastomoses free of adhesions (33%). Neither did we observe any perianastomotic abscesses in the control group. The adhesion scores of all groups are presented in Table 1.
Bursting pressure
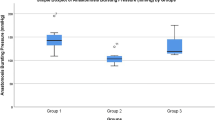
We observed statistically significant differences in the bursting pressures of the four groups (Kruskal–Wallis, P < 0.001). The lowest mean bursting pressure was observed in group 4 (110.2 mmHg) and the highest in the control group (270.87 mmHg). The bursting pressures of the anastomoses that leaked or dehisced before killing were valued as zero. These anastomoses were not included in the comparisons and the statistical calculations. The descriptive values of the bursting pressures in the four groups are presented in Fig. 2.
Bursting pressures (mmHg) in all four groups. Kruskal–Wallis test: P < 0.001. Pairwise group comparison using the Mann–Whitney test with the Bonferroni correction: 1 versus 2 (P < 0.001), 1 versus 3 (P < 0.001), 1 versus 4 (P < 0.001), 2 versus 3 (P > 0.200), 2 versus 4 (P = 0.003), 3 versus 4 (P = 0.003)
Histological assessment/hydroxyproline
Signs of intestinal damage such as mucositis were not reported by the histopathologist during the anastomotic assessment. The control group showed the lowest mean inflammatory score (1.2) and the highest mean fibroblast activity and mean collagen deposition scores (3.47 and 2.87, respectively), as well as significantly increased hydroxyproline concentrations (P < 0.001). Table 2 presents descriptive values of all four histological parameters and the hydroxyproline concentration levels with their statistical comparison results.
Discussion
Peritoneal carcinomatosis is not uncommon in patients with colorectal cancer and has been reported to have a poor prognosis in the past. Since 1990, studies on cytoreductive surgery followed by early post-operative intraperitoneal chemotherapy (EPIC) or hyperthermic intraperitoneal chemotherapy (HIPEC) have prompted new treatment options for selected patients with advanced colorectal cancer [4–6]. The immediate post-operative, intraperitoneal administration of cytostatic drugs achieves high concentrations of these drugs in the peritoneum as well as in the liver, avoiding the side effects of systemic administration. Intraperitoneal chemotherapy has been associated with marked toxicity in the form of lethargy, weight loss and bacterial translocation [7]. Extensive surgical resection of macroscopic tumour is often followed by the construction of multiple bowel anastomoses. Immediate intraperitoneal chemotherapy puts the intestinal healing under increased risk. Various surgical complications have been described following intraperitoneal chemotherapy, the commonest being anastomotic leakage. Leakage rates up to 20% have been reported depending on anastomotic site, resection size and individual risks [7–10].
The combination of 5-FU with newer chemotherapeutic agents seems to improve the patient response rate to chemotherapy and thus results to an even better survival rate. The anastomotic dehiscence rate is possibly the most important indicator of anastomotic healing failure. Zacharakis et al. [9] observed anastomotic dehiscence in 30% of rats under 5-FU treatment, compared to 0% in the control group. The negative effect of 5-FU on the anastomotic bursting pressure has been shown by Kanellos et al. [10]. They have found significant bursting pressure decreases on anastomoses under the intraperitoneal influence of 5-FU and Leucovorin. In our experiment, the presence of intraperitoneal irinotecan or 5-FU significantly decreased the mechanical strength of the anastomoses, whereas the bursting pressures were further decreased when the two agents were combined (group 4 vs. control, P < 0.001).
The microscopic assessment of the anastomotic healing usually finds place by assessing histological parameters, such as inflammatory reaction, neoangiogenesis and collagen formation. It is known that chemotherapy agents affect the healing process by increasing the inflammatory reaction at the wound site. 5-FU has been found to increase inflammatory reaction at the anastomotic site. Furthermore, 5-FU decreases the fibroblast reproduction rate and their concentration [10–12]. Our study has shown 5-FU to negatively affect the anastomotic healing by increasing the inflammatory reaction, reducing neocollagen and fibroblasts and minimally reducing neoangiogenesis at the anastomotic site. Irinotecan had similar effects. It significantly increased the inflammatory reaction (P < 0.001), and it significantly reduced the neocollagen formation (P < 0.001), the fibroblast concentration (P < 0.001) and the hydroxyproline concentration (P < 0.001) when compared to the control group. The combined effects of the two agents were once again more detrimental on the anastomotic healing compared to when the agents were used as monotherapy. Inflammatory reaction in group 4 (5-FU and irinotecan) was significantly increased compared to all other groups. Neoangiogenesis was increased, but no significant results were found. The collagen formation, fibroblast concentration and hydroxyproline concentration were reduced compared to all groups, whereas the comparison with the control group was statistically significant.
In conclusion, the immediate, post-operative intraperitoneal administration of 5-fluorouracil or irinotecan had a negative effect on the healing process of the large bowel anastomoses in rats, with statistically significant results. Nevertheless, the negative effects of the combination of these two agents were statistically more significant compared to the single use of 5-FU or irinotecan.
References
van der Hamm AC, Kort WJ, Weijma IM, van der Ingh HF, Jeekel J (1991) Effect of fibrin sealant on the healing of colonic anastomosis in the rat. Br J Surg 78:49–53
Ehrlich HP, Hunt TK (1969) The effects of cortisone and anabolic steroids on the tensile strength of healing wounds. Ann Surg 170:203–206
Guglielmi A, Sobrero A (2007) Second-line therapy for advanced colorectal cancer. Gastrointest Cancer Res 1:57–63
Cao C, Yan T, Black D, Morris D (2009) A systematic review and meta-analysis of cytoreductive surgery with perioperative intraperitoneal chemotherapy for peritoneal carcinomatosis of colorectal origin. Ann Surg Oncol 16:2152–2165
Kusamura S, Younan R, Baratti D, Costanzo P, Favaro M, Gavazzi C, Deraco M (2006) Cytoreductive surgery followed by intraperitoneal hyperthermic perfusion: analysis of morbidity and mortality in 209 peritoneal surface malignancies treated with closed abdomen technique. Cancer 106:1144–1153
Pelz JOW, Doerfer J, Decker M, Dimmler A, Hohenberger W, Meyer T (2007) Hyperthermic intraperitoneal chemoperfusion (HIPEC) decrease wound strength of colonic anastomosis in a rat model. Int J Colorectal Dis 22:941–947
Fuchs C, Mitchell EP, Hoff PM (2006) Irinotecan in the treatment of colorectal cancer. Cancer Treat Rev 32:491–503
Rothenberg ML, Meropol NJ, Poplin EA, van Cutsem E, Wadler S (2001) Mortality associated with irinotecan plus bolus fluorouracil/leucovorin: summary findings of an independent panel. J Clin Oncol 19:3801–3807
Zacharakis E, Dimitriades H, Pramateftakis MG, Lambrou I, Zacharakis E, Zaraboukas T, Koliakos G, Kanellos I, Betsis D (2008) Effect of IGF-I on healing of colonic anastomoses. J Surg Res 144:138–144
Kanellos I, Kazantzidou D, Evangelou I, Galovatsea K, Zaraboukas T, Dadoukis I (1998) Healing of colonic anastomoses after immediate and delayed administration of 5-fluorouracil plus folinic acid. Eur Surg Res 30:312–317
Kuzu MA, Kuzu I, Koksoy C, Akyol FH, Uzal D, Kale IT, Orhan D, Terzi C (1998) Histological evaluation of colonic anastomotic healing in the rat following preoperative 5-fluorouracil, fractionated irradiation and combined treatment. Int J Colorectal Dis 13:235–240
Ibrahim Canter H, Konas E, Bozdogan O, Vargel I, Ozbatir B, Oner F, Erk Y (2007) Effect of slow-release 5-fluorouracil on capsule formation around silicone breast implants: an experimental study with mice. Aesthetic Plast Surg 31:674–679
Conflict of interest
The authors certify that they have no conflict of interest related to the publication of this article.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Pramateftakis, M.G., Kanellos, D., Mantzoros, I. et al. Intraperitoneally administered irinotecan with 5-fluorouracil impair wound healing of colonic anastomoses in a rat model: an experimental study. Tech Coloproctol 15 (Suppl 1), 121–125 (2011). https://doi.org/10.1007/s10151-011-0755-8
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10151-011-0755-8