Abstract
Background
This study investigated the clinical outcomes of stent placement for malignant extrinsic ureteral obstruction (MUO) and predictive factors for stent failure.
Methods
We retrospectively analyzed clinical data for 91 patients with radiologically significant hydronephrosis due to MUO who underwent successful stent placement. In total, 132 ureters were stented for the decompression. Factors related to stent failure were analyzed with a Cox proportional hazards model.
Results
Stent failure occurred in 25 ureters in 20 patients. The median interval to failure was 63 days. The multivariate analysis showed that the significant predictors of stent failure were bladder invasion and severe hydronephrosis before the stent insertion. The patients were divided into three groups based on these two factors: low-risk (neither factor; 85 patients), intermediate-risk (one factor; 37), and high-risk (both factors; 10). The median stent failure-free survival rate at 3 months was 94.8% in the low-risk, 71.8% in the intermediate-risk and 55.6% in the high-risk group, respectively. Of the ureters with stent failure, there was successful re-replacement of internal stents in 3 low-risk, 6 intermediate-risk and no high-risk ureters. Replacement by nephrostomy was done in 2 low-risk, 5 intermediate-risk and 7 high-risk ureters.
Conclusion
The patients considered at low-risk could be managed without stent failure by internal stenting. However, the patients at high-risk may require the consideration of nephrostomy or other alternatives as the initial treatment. Our stratification model may allow better risk stratification for patients with regard to ureteral stenting, helping to identify patients for whom ureteral stenting is indicated.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Malignant extrinsic ureteral obstruction (MUO) can result from extrinsic compression by a primary lesion, metastases, retroperitoneal lymphadenopathy, or direct tumor seeding [1] and is commonly a late sign in patients with advanced malignancy. The reported median survival of patients with MUO ranges from 3 to 7 months [2]. Because these patients generally have a poor prognosis [3], the management of MUO can be difficult. If untreated, ureteral obstruction can lead to renal failure and even death [4]. However, there is evidence that palliative urinary diversion prevents the deterioration of renal failure and may result in improved survival [5]. It is usually possible to drain the upper urinary tracts adequately using various types of ureteral internal stents, percutaneous nephrostomy (PCN) catheters, or extra-anatomic stents in order to provide symptomatic relief and maintain renal function. However, as yet there have been no definitive published guidelines on the management of MUO, and it is often difficult to identify the most beneficial strategy for a patient and their potentially short life expectancy [4]. The indication for ureteral stent placement in MUO and the outcomes of using ureteral stents remain unclear. The aim of this study, therefore, was to investigate clinical outcomes following the placement of ureteral stents for MUO and to identify the predictive factors for stent failure, with a view to establishing a way to identify patients for whom ureteral stenting would be indicated. We did this by reviewing the experience of our institution in the treatment of MUO.
Patients and methods
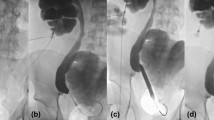
This study was approved by the ethics committee at our institution and the methods were conducted in accordance with the approved guidelines. We retrospectively reviewed clinical and laboratory data for patients with radiologically significant hydronephrosis due to MUO, demonstrated by ultrasonography (US) and computed tomography (CT), who underwent successful ureteral stent placement for decompression of the MUO at our institution between May 2005 and November 2017. Patients with direct ureteral obstruction caused by urolithiasis and those with urinary stones that could affect stent management were excluded from analysis. If the patients with MUO demonstrated obstructive pyelonephritis at the time of consultation to our department, we inserted a single-J ureteral catheter or a PCN catheter to drain the renal pelvis, and then replaced the double-J catheter as the ureteral stent after the pyelonephritis improved. A total of 91 patients met these criteria; their characteristics and types of malignancy are shown in Table 1. The most common malignancy was cervical cancer. The stents for these 91 patients were placed retrogradely in 130 ureters and antegradely in 2, with one stent inserted per ureter without dilation of the obstructive lesion. We used 6-Fr double-J polyurethane stents. The models used were Endo-Sof AQ (Cook Urological, Spencer, IN, USA), White Universa (Cook Urological), or INLAY (C. R. Bard Inc., Murray Hill, NJ, USA), with the choice at the attending urologist’s discretion. Any changes in the type of stent were also made according to the urologist’s judgment, and the treatment policy after stent placement was left to the discretion of the attending physicians of each department. The start of the observation period was defined as the date of the initial ureteral stent placement. The stents were generally exchanged every 2–4 months, and removal was considered if routine follow-up CT or US demonstrated that the cause of the obstruction had definitely disappeared because of the cancer therapy, including systemic or local treatment. Antibiotics were administered at the time of stent replacement. Once the double-J catheter was inserted, palliative treatment without any obstruction was performed for urinary tract infections. Stent failure was defined as the necessity for another alternative form of urinary diversion (including PCN or an external ureteral stent) for one of the following reasons: an inability to replace the ureteral stent; increasing serum creatinine levels; complication by obstructive pyelonephritis; or the presence of a recurrent stent obstruction [2, 6,7,8]. The severity of hydronephrosis was evaluated by US according to the grading system of the Society for Fetal Urology. Performance status (PS) was evaluated according to the Eastern Cooperative Oncology Group grades. The presence or absence of bladder invasion or peritonitis carcinomatosa was judged by endoscopy and from image data and surgical findings, even if these conditions could not be confirmed by cytological or histopathological examination.
Univariate and multivariate analyses using a Cox proportional regression hazard model (with stepwise forward procedure) were used to evaluate the clinical and radiological variables that were significant predictors of stent failure-free survival during the follow-up period, and adjusted hazard ratios were generated. The following variables were included in the analysis: age, sex, hydronephrosis grade, serum creatinine level before the stent insertion, PS, bladder invasion, type of malignancy, peritonitis carcinomatosa, treatment history (tumor recurrence), no cancer treatment after ureteral stenting (best supportive care), and the level of the obstruction. The survival time to stent failure or death was measured from the time of the initial stent insertion. The Kaplan–Meier method was used for the survival analysis. Patients who died without stent failure were censored at the time of death without stent failure. Statistical significance was set at p < 0.05 for all analyses.
Results
Table 2 presents the characteristics of the 132 ureters in which ureteral stents were successfully inserted. The median follow-up interval after the initial stent insertion was 161 days (range 4–3234 days). The median number of stent changes was 1 (range 0–31). Of the 91 patients, 59 received cancer treatment (including chemotherapy, radiotherapy, or an operation); this resulted in the removal of the stent from 18 ureters of 11 patients. The periodic exchange of stents continued in 24 ureters of 17 patients. In total, 61 ureters of 44 patients were effectively managed by ureteral internal stenting without stent failure until the patient’s death. Three patients (four ureters) were lost to follow-up. No major complications were associated with stent replacement other than transient macrohematuria after stenting.
Stent failure occurred in 25 ureters (18.5%) of 20 patients. The median interval from the first stent insertion to failure was 63 days (range 1–468 days). There was no difference in the occurrence of stent failure among each double-J stent used in this study. For 23 of these ureters (18 patients), the reason for the failure was increasing serum creatinine levels, the presence of a recurrent stent obstruction, or complication by obstructive pyelonephritis. The other stent failures included one ureter that required washing in a renal pelvis because of bleeding and one ureter (in a different patient) in which the ureteral stent could not be replaced. For nine ureters (eight patients) with stent failure, replacement was performed by PCN; in the other 16 ureters, the stents were replaced with external single-J stents. As a result, there was successful re-replacement of internal ureteral stents in 11 ureters and replacement by PCN in three ureters.
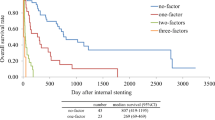
According to the univariate analysis, the significant predictors of stent failure were the presence of bladder invasion, severe hydronephrosis before the stent insertion (grade 3 or 4), the presence of peritonitis carcinomatosa, and gastric cancer as the primary disease (Table 2). However, the Cox regression multivariate analysis identified just two significant predictors of stent failure: the presence of bladder invasion, and severe hydronephrosis before the stent insertion (Table 2). As Ishioka et al. [9] and Cordeiro et al. [10] reported, we used these two risk factors to create a risk stratification model: low-risk (neither factor present), intermediate-risk (one of the factors present), and high-risk (both factors present). We divided the total of 132 ureters into these three risk groups (resulting in 85 low-risk ureters, 37 intermediate-risk, and 10 high-risk) and compared stent failure-free survival between the groups using Kaplan–Meier analysis (Fig. 1). Stent failure occurred at a frequency of 5.9% in low-risk, 35.1% in intermediate-risk, 70% in high-risk group (Table 3). Effective management was done by ureteral internal stenting without stent failure until the patient’s death at a frequency of 53.3% in low-risk, 35.1% in intermediate-risk, 10.0% in high-risk group. This showed a significant difference; the median stent failure-free survival rate at 3 and 6 months was 94.8% and 92.1% in the low-risk group, 71.8% and 62.8% in the intermediate group, and 55.6% and 29.6% in the high-risk group. As shown in Table 3, of the 25 ureters with stent failure, there was successful re-replacement of internal ureteral stents in the 9 ureters (resulting in 3 low-risk ureters, 6 intermediate-risk and no high-risk) and replacement by PCN was done in 14 ureters (resulting in 2 low-risk ureters, 5 intermediate -risk and 7 high-risk).
Discussion
The optimal management of MUO requires the preservation of renal function and treatment of the underlying malignant disease, but consideration of these requirements can be problematic because of the potentially short survival period. It is also important to take into consideration quality of life (QOL) issues related to the invasive procedures and the risks of complications, as well as the expectations of the patients and their families. Although there has been extensive debate on the risks and benefits of the insertion of ureteral stents and placement of nephrostomy tubes to relieve upper urinary tract obstruction, it is not clear which modality provides the most benefit and for which patients [5]. Individual treatment decisions should be made for each patient using a multidisciplinary approach that involves the patient, their family, and members of the treatment team [11]. Although ureteral stents and PCN each have their own advantages and disadvantages, a previous comparison of these methods found no statistically significant difference between them in median survival time or in related complications [12]. Ureteral stents often cannot be inserted because of ureteral deformity or compression, and successful stent placement across an obstructed ureteral segment does not necessarily guarantee adequate urine drainage [6]. The reported success rate for PCN (96–100%) is higher than that for retrograde stent insertion (around 85%) [5]. However, the incidence of insertion failure is markedly higher for patients with MUO, ranging from 15.0 to 27.5% [13]. Patients with “JJ” stents have significantly more irritative urinary symptoms and a higher likelihood of local discomfort than patients with nephrostomy tubes [14]. However, PCN is an invasive intervention that is offered in the palliative care setting [12]. The nephrostomy tube and bag for the external drainage can be burdensome, restricting physical activity and negatively impacting the patient’s QOL [4]. In addition, the long-term management of PCN catheters is cumbersome and associated with an inferior QOL compared with that with ureteral stents [15]. The prognosis, QOL, and complications are important considerations when deciding whether to choose a ureteral stent or PCN7. Stent failure is also considered to be a significant problem with ureteral stents, even when their insertion is successful. Broadly, stent failure is defined as any ureteral unit that requires additional procedures after its initial placement to manage the patient’s symptoms or because of the lack of alleviation by the stent of the patient’s chief complaint [16], due to the exacerbation of occlusion and stent encrustation accompanying disease progression and cancer treatment. Pavlovic et al. described stent failure as a prognostic factor for mortality and likely to be a sign of cancer progression in the patients with MUO [4]. When stent failure occurs and requires PCN, the PCN intervention will reduce the patient’s QOL, although it will improve the symptoms associated with stent failure. In this study, therefore, we investigated the clinical outcomes of stent placement to determine the predictive factors of stent failure.
Previous studies have reported a wide range of stent failure rates from 16 to 53% [4,5,6,7, 11, 14, 17], but these studies differed from each other in patient background, sample size, stent design, and etiology of the malignancies. In our study, the stent failure rate was 19.2%, which was consistent with the previous studies. Several factors have been reported as predictors of stent failure, including serum creatinine level before the ureteral stenting [17,18,19,20], the degree of hydronephrosis [6, 8, 19], gastrointestinal cancer as the primary disease6, poor preoperative PS [6, 20], and the presence of a mid or lower ureteral obstruction [20]; however, perspectives on these have not yet been unified. In this study, serum creatinine level before stent insertion was found not to be predictive of stent failure. However, it was thought to be the cause of acute postrenal failures observed in five of seven patients with serum creatinine levels more than 4 mg/ml before stent insertion, resulting in rapid normalization of the serum creatinine level after unilateral or bilateral ureteral stenting. Ganatra et al. reported that invasion into the bladder observed on cystoscopy had a significant predictive value for progression to PCN [2] and that patients with direct invasion had a threefold greater likelihood of stent failure, resulting in 56% conversion to PCN [2]. Another study advocated primary PCN for patients with urological cancer [21]. A further study reported bladder invasion, PS, and the degree of hydronephrosis were potential independent predictors of insertion failure [13]. We divided our patients with successful ureteral stents placement for MUO into three groups using our risk classification based on the presence of bladder invasion and/or severe hydronephrosis before the stent insertion. These groups differed significantly in stent failure-free survival. In the low-risk group patients, there could be a high possibility that MUO could be successfully managed using 6-Fr double-J polyurethane stents without experiencing stent failure and the necessity of considering using PCN catheters from the beginning. However, in the high-risk group patients, stent failure occurred earlier and at a higher rate, eventually leading to the introduction of PCN without successful re-replacement of internal ureteral stents using a 6-Fr double-J polyurethane stent. Therefore, because only few patients in the high-risk group benefitted from the 6-Fr double-J polyurethane stents used as the initial treatment in this study, it may be better to select PCN catheters or other alternatives for drainage. Recently, resonance stents have been shown to have compression resistance superior to that of polymeric ureteral stents [13], and a recent report demonstrated that resonance stents have higher efficiency than polymeric ureteral stents to withstand extrinsic compression [22]. Compared with polymeric ureteral stents, metal stents preserve patency under a greater degree of extrinsic compression and have longer indwelling times, thereby necessitating fewer stent changes (up to 12 months) [23]. Chow et al. concluded that resonance stents should be offered as an option for internal drainage [24]. Therefore, metal stents may be more useful than polymeric ureteral stents for patients in the high-risk group in our stratification model.
The present study had some limitations. The small sample size may have prevented the determination of precise statistical significance. In addition, a retrospective examination using several kinds of stent by several urologists at a single institution may have resulted in an inadequate assessment of the effects of previously reported significant factors for stent failure. In this study, we targeted only MUO patients who underwent successful stent placement. The patients who failed to insert a ureteral stent were not analyzed. The degrees of hydronephrosis and bladder invasion were reported to be independent predictive factors for ureteral stent insertion failure. Therefore, the selection bias may be applied to the patients considered at high-risk in our classification. The stent insertion failure regarding MUO management also needs to be considered. We believe that a further large-scale study is needed to confirm our findings and to establish clear guidelines for the management of MUO.
In conclusion, bladder invasion and severe hydronephrosis before ureteral stent insertion may be significant predictors of stent failure in patients who had radiologically significant hydronephrosis due to MUO. The stent failure-free survival rate at 6 months was more than 90% for the patients without either of these two risk factors but less than 30% for the patients with both risk factors. Our stratification model may allow better risk stratification for patients with regard to ureteral stenting, helping to identify patients for whom ureteral stenting is indicated. Patients in the high-risk group should be informed of the poor expected outcomes even when ureteral stenting is successful so they can choose whether to receive a ureteral stent or a nephrostomy, in consultation with family members or the clinician.
References
Elsamra SE, Leavitt DA, Motato HA et al (2015) Stenting for malignant ureteral obstruction: Tandem, metal or metal-mesh stents. Int J Urol 22:629–636
Ganatra AM, Loughlin KR (2005) The management of malignant ureteral obstruction treated with ureteral stents. J Urol 174:2125–2128
Fiuk J, Bao Y, Calleary JG et al (2015) The use of internal stents in chronic ureteral obstruction. J Urol 193:1092–1100. https://doi.org/10.1016/j.juro.2014.10.123. (Epub 2014 Nov)
Pavlovic K, Lange D, Chew BH (2016) Stents for malignant ureteral obstruction. Asian J Urol 3:142–149
Sountoulides P, Mykoniatis I, Dimasis N (2014) Palliative management of malignant upper urinary tract obstruction. Hippokratia 18:292–297
Kamiyama Y, Matsuura S, Kato M et al (2011) Stent failure in the management of malignant extrinsic ureteral obstruction: Risk factors. Int J Urol 18:379–382
Izumi K, Mizokami A, Maeda Y et al (2011) Current outcome of patients with ureteral stents for the management of malignant ureteral obstruction. J Urol 185:556–561
Yossepowitch O, Lifshitz DA, Dekel Y et al (2001) Predicting the success of retrograde stenting for managing ureteral obstruction. J Urol 66:1746–1749
Ishioka J, Kageyama Y, Inoue M et al (2008) Prognostic model for predicting survival after palliative urinary diversion for ureteral obstruction: analysis of 140 cases. J Urol 180:618–621
Cordeiro MD, Coelho RF, Chade DC et al (2016) A prognostic model for survival after palliative urinary diversion for malignant ureteric obstruction: a prospective study of 208 patients. BJU Int 117:266–271
Hsu L, Li H, Pucheril D et al (2016) Use of percutaneous nephrostomy and ureteral stenting in management of ureteral obstruction. World J Nephrol 5:172–181
Alawneh A, Tuqan W, Innabi A et al (2016) Clinical factors associated with a short survival time after percutaneous nephrostomy for ureteric obstruction in cancer patients: an updated model. J Pain Symptom Manage 251:255–261
Wang JY, Zhang HL, Zhu Y, (2016) Predicting the failure of retrograde ureteral stent insertion for managing malignant ureteral obstruction in outpatients. Oncol Lett 11:879–883
Shekarriz B, Shekarriz H, Upadhyay J et al (1999) Outcome of palliative urinary diversion in the treatment of advanced malignancies. Cancer 85:998–1003
Chung SY, Stein RJ, Landsittel D et al (2004) 15-Year experience with the management of extrinsic ureteral obstruction with indwelling ureteral stents. J Urol 172:592–595
Fiuk J, Bao Y, Calleary JG et al (2015) The use of internal stents in chronic ureteral obstruction. J Urol 193:1092–1100
McCullough TC, May NR, Metro MJ et al (2008) Serum creatinine predicts success in retrograde ureteral stent placement in patients with pelvic malignancies. Urology 72:370–373
Wenzler DL, Kim SP, Rosevear HM et al (2008) Success of ureteral stents for intrinsic ureteral obstruction. J Endourol 22:295–299
Yu SH, Ryu JG, Jeong SH et al (2013) Predicting factors for stent failure-free survival in patients with a malignant ureteral obstruction managed with ureteral stents. Korean J Urol 54:316–321
Zadra JA, Jewett MA, Keresteci AG et al (1987) Nonoperative urinary diversion for malignant ureteral obstruction. Cancer 60:1353–1357
Kallidonis PS, Georgiopoulos IS, Kyriazis ID et al (2015) The full metallic double-pigtail ureteral stent: Review of the clinical outcome and current status. Indian J Urol 31:8–14
Baumgarten AS, Hakky TS, Carrion RE et al (2014) A single-institution experience with metallic ureteral stents: a cost-effective method of managing deficiencies in ureteral drainage. Int Braz J Urol 40:225–231
Ficko Z, Hyams ES (2018) Complications of upper tract drainage. In: Samir S, Taneja MD, Ojas Shah MD (eds) Complications of urologic surgery, 5th edn. Elsevier, New York, pp 218–225
Chow PM, Chiang IN, Chen CY et al (2015) Malignant ureteral obstruction: Functional duration of metallic versus polymeric ureteral stents. PLoS One 10:e0135566
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
There are no conflicts of interest to declare.
About this article
Cite this article
Matsuura, H., Arase, S. & Hori, Y. Ureteral stents for malignant extrinsic ureteral obstruction: outcomes and factors predicting stent failure. Int J Clin Oncol 24, 306–312 (2019). https://doi.org/10.1007/s10147-018-1348-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10147-018-1348-6