Abstract
Background
The Japanese Children’s Cancer Group (JCCG) Neuroblastoma Committee (JNBSG) conducted a phase II clinical trial for high-risk neuroblastoma treatment. We report the result of the protocol treatment and associated genomic aberration studies.
Methods
JN-H-07 was a single-arm, late phase II trial for high-risk neuroblastoma treatment with open enrollment from June 2007 to February 2009. Eligible patients underwent five courses of induction chemotherapy followed by high-dose chemotherapy with hematopoietic stem cell rescue. Surgery for the primary tumor was scheduled after three or four courses of induction chemotherapy. Radiotherapy was administered to the primary tumor site and to any bone metastases present at the end of induction chemotherapy.
Results
The estimated 3-year progression-free and overall survival rates of the 50 patients enrolled were 36.5 ± 7.0 and 69.5 ± 6.6%, respectively. High-dose chemotherapy caused severe toxicity including three treatment-related deaths. In response to this, the high-dose chemotherapy regimen was modified during the trial by infusing melphalan before administering carboplatin and etoposide. The modified high-dose chemotherapy regimen was less toxic. Univariate analysis revealed that patients younger than 547 days and patients whose tumor showed a whole chromosomal gains / losses pattern had a significantly poor prognosis. Notably, the progression-free survival of cases with MYCN amplification were not inferior to those without MYCN amplification.
Conclusions
The outcome of patients treated with the JN-H-07 protocol showed improvement over the results reported by previous studies conducted in Japan. Molecular and genetic profiling may enable a more precise stratification of the high-risk cohort.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Neuroblastoma is the most frequently encountered childhood extracranial solid tumor and originates in the sympathoadrenal lineage derived from the neural crest [1]. Despite the development of multimodal treatment including induction chemotherapy, surgical resection, high-dose chemotherapy with hematopoietic stem cell rescue (HDC), and radiotherapy, the prognosis of patients with advanced neuroblastoma remains poor [2, 3].
In Japan, clinical studies on patients with International Neuroblastoma Staging System (INSS) stage 4 neuroblastomas has been conducted based on uniform treatment protocols [4, 5]. JANB-85 consisted of six cycles of induction chemotherapy followed by either high-dose chemotherapy with autologous hematopoietic stem cell transplantation (HDC) or repeated courses of conservative chemotherapy. The overall survival rate (OS) was 34.4% at 5 years after diagnosis. In the JANB-91 study, the induction chemotherapy regimen was intensified for MYCN-amplified stage 4 patients and followed by HDC. The 5-year OS was 34.0% for patients with MYCN-amplified tumors and 38.9% for those without MYCN amplification. However, the trial design of these studies has been questioned, since stopping criteria and selection of treatment were dependent on the treating institutions.
The present article reports the result of the first prospective clinical trial for high-risk neuroblastoma treatment conducted by the Japanese Children’s Cancer Group (JCCG) Neuroblastoma Committee (JNBSG) of the in accordance with the rules of Good Clinical Practice. The aim of the study was to verify the efficacy and safety of induction chemotherapy followed by HDC using the drug combinations contained in JANB85, which were also widely used in Japan at the time the study was conceived.
Methods
Study design and patients
JN-H-07 was a multicenter, prospective, single-arm late phase II trial assessing the efficacy and safety of a multimodal treatment that had been widely used for high-risk neuroblastomas in Japan. The study was open for patient registration from June 2007 to February 2009. Children over 12 months old and younger than 18 years of age who had a previously untreated high-risk neuroblastoma were recruited. The inclusion criteria were an INSS stage 2A/2B or stage 3 tumor with MYCN amplification, a stage 3 MYCN-non-amplified tumor with unfavorable histology defined by the international neuroblastoma pathology classification (INPC) over 547 days of age, and a stage 4 tumor aged 365–547 days associated with one of the following: MYCN amplification, DNA index = 1 or unfavorable histology (INPC) or a stage 4 tumor over 547 days in age. The study was approved by each local institutional review board and undertaken in accordance with the principles of the Declaration of Helsinki and the rules of Good Clinical Practice. Informed written consent was obtained from all the patients or their guardians. The primary endpoint was 3-year progression-free survival (PFS). The secondary endpoint was 3-year overall survival and standardized incidence ratio (SIR) of adverse effects.
Diagnosis
A diagnostic biopsy of either the primary tumor or metastatic lesions was mandatory for confirming the histopathological diagnosis and pathological central review. Tumors categorized as either a neuroblastoma or a ganglioneuroblastoma according to INPC were defined as neuroblastomas in this study.
Procedures
Treatment consisted of five cycles of induction chemotherapy followed by HDC with peripheral blood stem cells (PBSC) as a consolidation therapy. Surgical removal of the primary tumor was scheduled after three or four courses of induction chemotherapy. HDC was followed by radiotherapy administered to the primary tumor site. For patients with stage 3 disease without MYCN amplification, HDC was substituted by an additional course of the induction chemotherapy. Details of the protocol treatment are shown in Fig. 1. Initially, HDC consisted of melphalan on days − 5 and −4, etoposide and carboplatin on days − 7, − 6, − 5, − 4 (07MEC). During the trial, the HDC regimen 07MEC was modified in response to the frequent occurrence of severe capillary leak syndrome. Since the simultaneous administration of melphalan and the other two reagents was likely to be the cause of capillary leak, the melphalan infusion was advanced by four days to days - 9 and - 8 (09MEC). No patients received isotretinoin or anti-GD2 antibody immunotherapy as consolidation therapy.
For primary tumor resection, removal of all visible and palpable lesions was recommended while leaving adjacent organs as intact as possible. Incomplete resection was accepted in cases with vascular involvement. Lymph nodes with apparent tumor involvement were dissected, whereas extensive dissection of sentinel lymph nodes was discouraged.
Local extrabeam radiotherapy was administered to the tumor bed in all the patients using 4–20 MV high energy X ray. The clinical target volume included the primary tumor bed and sites of lymph node metastases evident at diagnosis. A fractionated dose of 19.8 Gy was given in eleven equal fractions (1.8 Gy per fraction), with an additional boost dose of 10.8 Gy in six fractions for gross residual diseases. Bone metastases with 123I-MIBG (meta-iodobenzylguanidine) uptake at the end of induction chemotherapy were subjected to a dose of 19.8 Gy in eleven equal fractions.
Response to the protocol treatment was evaluated using the original RECIST criteria [6]. A progressive disease was defined by the fulfillment of one of the following conditions based on imaging studies: (1) the sum of the longest diameter of all the target lesions exceeded 20% of the smallest measurements recorded since the commencement of treatment; (2) enlargement of nontarget lesions was apparent; (3) a novel lesion had emerged. Those that showed progressive disease or an apparent relapse during the induction chemotherapy were reported as an event.
Microarray-based comparative genomic hybridization (Array CGH)
Genomic signature analyses of tumor samples were carried out using microarray-based comparative genomic hybridization (Array CGH). Copy number alterations in nuclear DNA were examined using a 4 × 44 k whole-genome array (Agilent Technologies G4413A). DNA (500 ng) derived from the tumor was used for labeling. The protocol for DNA digestion, labeling, purification, and hybridization to the arrays followed the manufacturers’ instructions (Agilent Technologies).
Statistical analysis
Since 3-year PFS was 34 ± 4% (mean ± SE) in the CCG-3891 study [7], we set our 3-year PFS at 30% under the null hypothesis and 45% as the expected probability. Sample size was calculated using 37 subjects with a one-sided alpha error rate of 0.1 and a power of 0.8. Hence, the planned sample size was 40 and the accrual period was 2 years. Each survival function was estimated by the Kaplan–Meier method with confidence intervals (CI) using Greenwood’s formula and complementary log–log transformation. When the lower limit of the 80% CI for 3-year PFS exceeded 30%, we considered the primary endpoint to have been met. The 95% CI for 3-year OS was also estimated. The PFS curves were also estimated in subgroups for MYCN status (amplified / non-amplified). To evaluate the effect of prognostic factors on PFS and OS, hazard ratios with 95% CIs were estimated by Cox proportional hazards regression. We planned interim monitoring not for efficacy but for safety using the Bayesian method. If the posterior probability with regard to the incidence rate of severe adverse events exceeding 30% was greater than 97.5%, an independent data monitoring committee discussed whether the trial should be continued.
Results
Patients
Between June 2007 and February 2009, a total of 50 patients were enrolled. All patients were eligible for the study and constituted the intention-to-treat sample. The database was locked on April 16, 2014. The characteristics of the study population are summarized in Table 1. During the protocol treatment, 11 patients were excluded from the protocol study due to deviation. Of these, six were withdrawals resulting from parental refusal or the physician’s decision, two were excluded due to treatment-related side effects, and three due to an unsuccessful PBSC harvest. The remaining thirty-nine patients completed the protocol treatment (Fig. 2).
Treatment outcomes
At the latest follow-up, 17 patients were alive without progression or recurrence. Progression during protocol treatment was reported in four cases, which became evident after one, two, three, and three cycles of induction chemotherapy, respectively. Ultimately, thirty patients experienced progression or recurrence. The time to progression/recurrence ranged from 2 to 46 months from enrollment (average 15.5 months). Of these patients, fourteen were alive at the latest follow-up, whereas the remaining sixteen died of the disease. Three patients died of treatment-related toxicity, the details of which are described below. The average follow-up period for the patients without progression or recurrence was 64.6 months. The estimated 3-year PFS of the 50 patients was 36.5 ± 7.0%, and the 3-year OS was 69.5 ± 6.6% (Fig. 3).
Adverse effects
Grade 4 hematological adverse effects were reported after every induction chemotherapy cycle (total number of cycles: 228) given per protocol. Non-hematological adverse effects following induction chemotherapy were reported in three cases (one of liver dysfunction, one of meningitis, and one of hypomagnesaemia). The rate of grade 4 non-hematological adverse effects was 0.013 per induction chemotherapy cycle. These adverse effects were improved following adequate treatment, including the bacterial meningitis, which had been properly treated with antibiotics, and did not interfere with the protocol treatment. Among the 29 cases that underwent HDC, 21 were treated with 07MEC, whereas eight were treated with 09MEC. Fourteen cases reportedly encountered some kind of grade 4 non-hematological toxicity (rate of grade 4 non-hematological adverse effects: 0.48). Grade 4 liver dysfunction was observed in nine cases treated with 07MEC, but in none treated with 09MEC. Other major grade 4 toxicities were as follows: hyperamilasemia (n = 6), capillary leak syndrome (n = 3), cardiovascular toxicity (n = 2), neuronal toxicity (n = 2), and one case each of renal failure, encephalopathy, pleural effusion, nausea, diarrhea, hyponatremia, and hypercreatinemia. Among these, hyponatremia was the only grade 4 non-hematologic toxicity observed in patients treated with 09MEC, whereas others were caused by 07MEC. Treatment-related death was documented in three cases, again, all of which occurred after 07MEC. Two of these resulted from severe capillary leak syndrome, and one from acute renal failure.
Surgical outcomes
The primary tumor was ultimately resected in 47 patients. Seven tumor resections were performed at diagnosis. The remaining forty cases underwent preoperative chemotherapy. Resection was performed after three or four cycles of induction chemotherapy in 29 cases. In one patient, resection was carried out after two courses, the reason of which had not been reported. Definitive surgery was postponed until after HDC in ten cases, due to the local team’s decision that the primary tumor was unresectable after four cycles in at least four cases. Information on the extent of tumor resection was available in 45 cases. Complete resection was achieved in 32 patients (68%), > 90% tumor resection in ten (21.3%), and 50–90% tumor resection in three (6.4%). No surgery-related deaths were reported. Of the 43 patients for whom surgical details and outcomes were available, 26 experienced progression or recurrence. Among these, the site of the first progression / recurrence was locoregional in three patients, metastatic in 21 patients, and both locoregional and metastatic in two patients. The local recurrence rate (locoregional recurrence: n = 5/total cases: 43) was 11.6%. Nephrectomies were reported in eight patients. Substantial postoperative complications included two chylous ascites and one wound infection.
Next, we assessed the effect of radical surgery on the timing of restarting postoperative chemotherapy. Of the 29 patients who underwent radical surgery after three or four courses of chemotherapy, the average interval between the start of the last chemotherapy course and surgery was 36.0 days (range 23–49 days; protocol limit: 56 days). The average interval between surgery and restarting the next course was 12.9 days (range 6–28 days; protocol limit: 14 days). In five patients, postoperative chemotherapy was delayed beyond the protocol limit (15, 16, 17, 21, and 28 days).
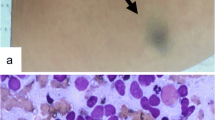
Array CGH analysis
An array CGH of tumor DNA was conducted in forty-five patients with available tissue. According to the pattern of the genomic signatures previously defined by Ohira et al. [8,9,10], all cases were classified into three genomic groups (GGs): a group with infrequent chromosomal events (silent, GGS); a group with partial chromosomal gains/losses (GGP); and a group of whole chromosomal gains/ losses (GGW). Thirty-nine tumors showed a GGP pattern, four showed a GGW pattern, and two showed a silent GGS pattern, although both of these had MYCN amplification.
Prognostic factors
Univariate analysis of previously reported prognostic factors was done by comparing the survival curve for each variable using the log-rank test. The results are shown in Table 2. Contrary to expectations, age under 18 months was identified as a significant predictor of poor prognosis, although this result may be biased by the small sample size of this group (n = 3). All three had MYCN-amplified tumors. Other than in age, there was no significant difference among the indicated subgroups. Notably, the PFS of patients with MYCN amplification was not inferior to that of patients without MYCN amplification (3-year PFS 45.0 vs 29.1%; Fig. 3). The three-year PFS of GGW (0.0%) was poorer than that of GGP (42.9%), although the difference was not statistically significant. The three-year OS of GGW (25%) was significantly worse than that of GGP (74.1%). Of note, the four GGW cases had unusual genomic features that distinguished them from the typical infant GGW tumors: Two had MYCN amplification and remaining others also had additional unique genomic alterations described below.
Discussion
This is a report of the first nation-wide phase II clinical trial conducted by JNBSG, which found an improvement in survival unlike the previous studies conducted in Japan. The results were reasonable, considering the fact that the patients did not receive post-transplant treatment including immunotherapy and isotretinoin. Other studies consisting of induction chemotherapy followed by consolidation with HDC using melphalan, etoposide, and carboplatin resulted in comparable outcomes. A randomized phase III trial conducted by Children’s Cancer Group (CCG) published in 1999 demonstrated that HDC with autologous bone marrow rescue resulted in significantly better PFS (34% at 3 years) than nonmyeloablative chemotherapy [7]. Recent studies have shown further improvement in patient survival. The COG ANBL0032 study reported that immunotherapy consisting of anti-GD2 antibody with GM-CSF and interleukin-2 combined with isotretinoin therapy was more effective in improving the survival rate of children with high-risk neuroblastomas which were in remission after HDC than isotretinoin alone [11]. The SIOPEN group reported that patients treated with HDC using busulfan and melphalan had a better outcome compared to those treated with melphalan, carboplatin or etoposide [12]. These novel approaches will be validated using Japanese cohorts in ongoing and future trials by JCCG.
A considerable number of patients experienced severe treatment-related toxicities, including three deaths resulting from treatment with the 07MEC HDC regimen in which etoposide and carboplatin were infused on days − 7, − 6, − 5 and − 4, while melphalan was infused on days − 5 and − 4. Since the combination of the three drugs itself is widely used for HDC [7, 13], we speculated that administration of melphalan on the last 2 days of 07MEC, the timing of which differed from that in the COG study, could have induced severe toxicity. We modified the regimen by infusing melphalan prior to etoposide and carboplatin (09MEC) as in the German NB97 protocol [13]. As a result, the incidence of severe toxicity dramatically decreased, suggesting that the risk of life-threatening complications could be reduced by avoiding simultaneous use of melphalan and the other two drugs.
There is as yet no consensus on the impact of aggressive surgery on the survival of high-risk neuroblastomas [14,15,16,17,18]. In our study, we found no significant difference in the PFS or OS of patients treated with different degrees of resection. Gross residual disease at the end of treatment did not necessarily lead to local failure. Boost radiotherapy of 10.8 Gy may have played a role in these cases. Simon demonstrated that the extent of best operation did not impact PFS or OS [18]. In their protocol, they recommend radiation therapy of 40 Gy for unresectable residual diseases. Their results, along with ours, suggest that local control may be achieved by optimizing the combination of surgery and local radiotherapy. Severe surgical complications may occasionally interfere with the seamless deployment of multimodal treatment and indirectly affect the long-term outcome of the patient. In the present study, postoperative chemotherapy was delayed in a number of patients after radical surgery. Currently, we are conducting a trial in which radical surgical resection is intentionally delayed until the completion of all chemotherapy courses including HDC with the aim of shortening the interval between each chemotherapy course and subsequently strengthening the time-dose intensity of the entire treatment.
The array CGH study revealed that there were four patients in the high-risk neuroblastoma cohort that showed a GGW pattern. These had a worse prognosis than patients with GGP pattern tumors. In general, tumors showing a GGW pattern typically occur in infants, have a single copy of the MYCN gene, are hyperdiploid, and have a very favorable outcome in contrast to GGP tumors, which typically occur in high-risk neuroblastomas [8,9,10, 19,20,21]. GGW cases in our cohort had rare but distinct genomic features that distinguished them from the typical infant GGW tumors: two had MYCN amplification, one had amplification of the 12q region, and one showed a local rearrangement pattern in chromosome 11 that resembled chromothripsis [22]. Although we might speculate that such aberrations could have played a critical role in the acquisition of the aggressive behavior of these tumors, further investigation with a larger cohort is required to obtain conclusive results.
MYCN has proven to be a powerful predictor of poor prognosis in general and in patients with localized neuroblastoma [23,24,25]. However, in contrast to previous findings reporting MYCN amplification as a predictor of poor prognosis in high-risk neuroblastoma [4, 13], MYCN amplification lacked prognostic impact in the present study in line with the results of other recent reports in which patients were treated with similar strategies [12, 26], suggesting that among high-risk patients treated with aggressive multimodal therapy, MYCN may cease to be a prognostic factor.
There are several limitations for the interpretation of the results of our study. First, the sample size is relatively small, particularly that of patients who have completed the protocol treatment, and might have affected the statistical analysis. Second, there were amendments in the timing of surgery and the overall treatment course was not uniform among the cases. Third, the amendment in the order of drug administration in HDC may have had impact on the prognosis, although we did confirm that the EFS did not differ between 07MEC and 09MEC (5-year EFS 26.8% vs 30.0%).
In conclusion, an improvement was seen in the outcome of patients treated with the JN-H-07 protocol in contrast to the previous studies conducted in Japan, particularly those dealing with MYCN-amplified tumors. Further analyses using a larger cohort are warranted to verify our findings.
Change history
04 August 2020
In the October 2018 issue of International Journal of Clinical Oncology.
References
Bolande RP (1974) The neurocristopathies: a unifying concept of disease arising in neural crest maldevelopment. Hum Pathol 5:409–429
Kreissman SG, Seeger RC, Matthay KK et al (2013) Purged versus non-purged peripheral blood stem-cell transplantation for high-risk neuroblastoma (COG A3973): a randomised phase 3 trial. Lancet Oncol 14:999–1008. https://doi.org/10.1016/S1470-2045(13)70309-7
Pearson AD, Pinkerton CR, Lewis IJ et al (2008) High-dose rapid and standard induction chemotherapy for patients aged over 1 year with stage 4 neuroblastoma: a randomised trial. Lancet Oncol 9:247–256
Kaneko M, Tsuchida Y, Uchino J et al (1999) Treatment results of advanced neuroblastoma with the first Japanese study group protocol. Study Group of Japan for Treatment of Advanced Neuroblastoma. J Pediatr Hematol Oncol 21:190–197
Kaneko M, Tsuchida Y, Mugishima H et al (2002) Intensified chemotherapy increases the survival rates in patients with stage 4 neuroblastoma with MYCN amplification. J Pediatr Hematol Oncol 24:613–621
Therasse P, Arbuck SG, Eisenhauer EA et al (2000) New guidelines to evaluate the response to treatment in solid tumors. J Natl Cancer Inst 92:205–216
Matthay KK, Villablanca JG, Seeger RC et al (1999) Treatment of high-risk neuroblastoma with intensive chemotherapy, radiotherapy, autologous bone marrow transplantation, and 13-cis-retinoic acid. Children’s Cancer Group. N Engl J Med 341:1165–1173
Ohira M, Nakagawara A (2010) Global genomic and RNA profiles for novel risk stratification of neuroblastoma. Cancer Sci 101:2295–2301
Tomioka N, Oba S, Ohira M et al (2008) Novel risk stratification of patients with neuroblastoma by genomic signature, which is independent of molecular signature. Oncogene 27:441–449
Nakazawa A, Haga C, Ohira M et al (2015) Correlation between the International Neuroblastoma Pathology Classification and genomic signature in neuroblastoma. Cancer Sci 106:766–771
Yu AL, Gilman AL, Ozkaynak MF et al (2010) Anti-GD2 antibody with GM-CSF, interleukin-2, and isotretinoin for neuroblastoma. N Engl J Med 363:1324–1334
Ladenstein R, Pötschger U, Pearson AD et al (2017) Busulfan and melphalan versus carboplatin, etoposide, and melphalan as high-dose chemotherapy for high-risk neuroblastoma (HR-NBL1/SIOPEN): an international, randomised, multi-arm, open-label, phase 3 trial. Lancet Oncol 18:500–514
Berthold F, Boos J, Burdach S et al (2005) Myeloablative megatherapy with autologous stem-cell rescue versus oral maintenance chemotherapy as consolidation treatment in patients with high-risk neuroblastoma: A randomised controlled trial. Lancet Oncol 6:649–658
von Allmen D, Davidoff AM, London WB et al (2017) Impact of extent of resection on local control andsurvival in patients from the COG A3973 Study With High-Risk Neuroblastoma. J Clin Oncol 35:208–216
von Allmen D, Grupp S, Diller L et al (2005) Aggressive surgical therapy and radiotherapy for patients with high-risk neuroblastoma treated with rapid sequence tandem transplant. J Pediatr Surg 40:936–941
Koh CC, Sheu JC, Liang DC et al (2005) Complete surgical resection plus chemotherapy prolongs survival in children with stage 4 neuroblastoma. Pediatr Surg Int 21:69–72
Holmes K, Sarnacki S, Pötschger U et al (2014) Presented at Advances in Neuroblastoma Research (ANR) 2014, Cologne, Germany, May 13–16, 2014. ANR 2014 congress information book, p 107
Simon T, Häberle B, Hero B et al (2013) Role of surgery in the treatment of patients with stage 4 neuroblastoma age 18 months or older at diagnosis. J Clin Oncol 31:752–758
Vandesompele J, Speleman F, Van Roy N et al (2001) Multicentre analysis of patterns of DNA gains and losses in 204 neuroblastoma tumors: how many genetic subgroups are there? Med Pediatr Oncol 36:5–10
Janoueix-Lerosey I, Schleiermacher G, Michels E et al (2009) Overall genomic pattern is a predictor of outcome in neuroblastoma. J Clin Oncol 27:1026–1033
Guimier A, Ferrand S, Pierron G et al (2014) Clinical characteristics and outcome of patients with neuroblastoma presenting genomic amplification of loci other than MYCN. PLoS One 9:e101990. https://doi.org/10.1371/journal.pone.0101990 2014.
Stephens PJ, Greenman CD, Fu B et al (2011) Massive genomic rearrangement acquired in a single catastrophic event during cancer development. Cell 144:27–40. https://doi.org/10.1016/j.cell.2010.11.055
Seeger RC, Brodeur GM, Sather H et al (1985) Association of multiple copies of the N-myc oncogene with rapid progression of neuroblastomas. N Engl J Med 313:1111–1116
Bagatell R, Beck-Popovic M, London WB et al (2009) International Neuroblastoma Risk Group. Significance of MYCN amplification in international neuroblastoma staging system stage 1 and 2 neuroblastoma: a report from the International Neuroblastoma Risk Group database. J Clin Oncol 27:365–370. https://doi.org/10.1200/JCO.2008.17.9184
Meany HJ, London WB, Ambros PF et al (2014) Significance of clinical and biologic features in Stage 3 neuroblastoma: a report from the International Neuroblastoma Risk Group project. Pediatr Blood Cancer 61:1932–1939. https://doi.org/10.1002/pbc.25134
Park JR, Scott JR, Stewart CF et al (2011) Pilot induction regimen incorporating pharmacokinetically guided topotecan for treatment of newly diagnosed high-risk neuroblastoma: a Children’s Oncology Group study. J Clin Oncol 29:4351–4357. https://doi.org/10.1200/JCO.2010.34.3293
Acknowledgements
This research was supported in part by the Practical Research for Innovative Cancer Control from the Japan Agency for Medical Research (AMED; #16ck0106070h0003, #16ck0106130h0003). We thank all physicians at the participating institutions for enrolling the cases, filling case report forms, and providing follow-up data.
Author information
Authors and Affiliations
Consortia
Corresponding author
Ethics declarations
Conflict of interest
The authors have no conflicts of interest directly relevant to the content of this article.
About this article
Cite this article
Hishiki, T., Matsumoto, K., Ohira, M. et al. Results of a phase II trial for high-risk neuroblastoma treatment protocol JN-H-07: a report from the Japan Childhood Cancer Group Neuroblastoma Committee (JNBSG). Int J Clin Oncol 23, 965–973 (2018). https://doi.org/10.1007/s10147-018-1281-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10147-018-1281-8