Abstract
Charged particle therapy (proton beam therapy and carbon ion therapy) is a form of radiotherapy which has the unique characteristic of superior depth dose distribution, and has been used for the treatment of hepatocellular carcinoma (HCC) in a limited number of patients, especially in Japan. We undertook a systematic review to define the clinical utility of charged particle therapy for patients with HCC. We searched the MEDLINE database from 1983 to June 2016 to identify clinical studies on charged particle therapy for HCC. Primary outcomes of interest were local control, overall survival, and late radiation morbidities. A total of 13 cohorts from 11 papers were selected from an initial dataset of 78 papers. They included a randomized controlled trial comparing proton beam therapy with transarterial chemoembolization, 9 phase I or II trials and 2 retrospective studies. The reported actuarial local control rates ranged from 71.4–95% at 3 years, and the overall survival rates ranged from 25–42.3% at 5 years. Late severe radiation morbidities were uncommon, and a total of 18 patients with grade ≥3 late adverse events were reported among the 787 patients included in this analysis. Charged particle therapy for HCC was associated with good local control with limited probability of severe morbidities. The cost-effectiveness and the distinctive clinical advantages of charged particle therapies should be clarified in order to become a socially accepted treatment modality for HCC.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Hepatocellular carcinoma (HCC) is the second leading cause of cancer death and the age-adjusted incidence of HCC is still increasing worldwide [1, 2]. HCC is mostly attributable to persistent infection by hepatitis B or C viruses with intercurrent liver cirrhosis, which limits the treatment options.
Recent progress in radiation oncology has enabled the concentration of higher radiation doses of photon beams to HCC lesions surrounded by relatively radiosensitive normal liver tissue, using stereotactic body radiotherapy (SBRT) or stereotactic ablative body radiotherapy, and this has now become one of the ablative treatment options for HCC [3]. Charged particle therapy (CPT) is a form of radiotherapy with superior depth dose distribution compared to photon radiotherapy. This superiority in depth dose distribution is attained by the energy-dependent specific range of the charged particles within the tissues and the sharp peak of the energy deposit just before stopping the particle, which is called Bragg peak. Consequently, tumors can be treated more effectively with less toxicity by charged particles than by photons on theoretical grounds, even in the cirrhotic liver with limited hepatic functional reserve (Fig. 1). Recently, CPT facilities are increasing worldwide owing to the development of compact accelerators and the lowered cost of facility construction.
Typical dose distributions of proton beam therapy (a) and stereotactic body radiotherapy (b). Both modalities can achieve highly conformal dose distribution, but the middle- to low-dose region of the normal liver can be minimized by charged particle therapy owing to Bragg peak. Accordingly, treatment of larger tumors (i.e., maximum diameter >5 cm) is more suitable for charged particle therapy
With the increase in CPT facilities, the number of HCC patients who are treated by CPT is also increasing (Fig. 2). However, the scarcity of clinical trials comparing CPT with other treatment modalities and the limited number of the facilities where CPT can be used, seem to hamper the prevalence of CPT for HCC. Here, we systematically reviewed the treatment results of CPT (proton beam therapy [PBT] and carbon ion therapy) for HCC in order to confirm the safety and efficacy of this treatment modality. We also summarized the findings from these and other related papers.
Materials and methods
A systematic review of publications was performed using the MEDLINE database from 1983 to June 2016 as a part of the work for the revision of the Japanese Clinical Practice Guidelines for Hepatocellular Carcinoma, although the review protocol was not registered in advance [4, 5].
The search strategy was developed to obtain literature on CPT with or without systemic therapy for human HCC, excluding review articles. The search methods were implemented by skilled librarians of the International Medical Information Center (Tokyo, Japan), with input from the authors. A literature search was limited to English language papers and carried out in February 2012 for the period from 1983 to 2011, and in October 2016 for the period from 2012 to June 2016. The detailed search queries are described in the Clinical Practice Guidelines for Hepatocellular Carcinoma—The Japan Society of Hepatology 2013 update for the search carried out in 2012, and will be described on the web page of the Japan Society of Hepatology (https://www.jsh.or.jp/) for the search carried out in 2016 [4, 5].
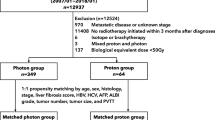
The inclusion criteria were reports of clinical results after CPT for HCC with data on survival and local control. Retrospective studies as well as prospective clinical trials were also included. Only papers published in English were selected. The number of participants was not used for inclusion criteria, but single-case reports were excluded. Retrospective studies which were reported from institutions that had already published the results of their own prospective clinical trials were excluded in order to avoid possible duplicate publication; some retrospective studies might include patients who had been treated in a prospective clinical trial. The first selection was conducted through a review of the titles and abstracts of the records from the database search by two of the authors (HI and HS) independently. We then performed a second selection through a full-text review of the papers adopted in the previous step by the authors (MM, TO, HI, and HS). The search flow diagram during our selection procedure is presented in Fig. 3. Our methodology was guided by the PRISMA statement [6], which provides an evidence-based process for conducting systematic reviews.
Results
Literature search
A total of 78 papers were identified from the database search. After the first and second selection through screening and review, 11 papers with 13 cohorts met the inclusion/exclusion criteria (Fig. 3) [7,8,9,10,11,12,13,14,15,16,17]. A review paper was included because it contained the summary results of two prospective studies which were not reported elsewhere [17]. Table 1 lists a summary of these studies.
Among the 13 cohorts included in this analysis, 10 and 3 were prospective and retrospective studies, respectively. Ten prospective studies comprised 9 phase I or II trials and a randomized controlled trial which compared PBT with transarterial chemoembolization (TACE). The results of the randomized controlled trial were based on an interim analysis [8]. Thirteen cohorts included 9 PBT cohorts and 4 carbon ion cohorts.
There was only one study which had a comparative treatment arm of TACE in a randomized controlled study [8], and one retrospective study which compared the two cohorts of PBT and carbon ion therapy [15]. All the other cohorts were single-arm studies of PBT or carbon ion therapy. As a result, comparative evidence was at a high risk of bias, and as well as selection bias. Assessment of publication bias was not performed, because we evaluated only published literature in the MEDLINE database.
Clinical results
Each prospective study included 15–76 patients, and 27 and 353 patients were eligible in the two retrospective studies. Most prospective studies included unresectable tumors. Dose fractionations differed among the studies, and the crude and actuarial local control rates ranged from 67–93% and 71.4–95% at 3 years, respectively. In addition, overall survival rates ranged from 25−42.3% among those who reported 5-year results. The overall survival rate after PBT was not significantly different from that after TACE, with a rate of 59% for the entire group at 2 years, according to the interim report of the randomized controlled trial [8].
Late severe radiation morbidities were uncommon. There was a total of 18 grade ≥3 late adverse events including 8 patients from prospective studies and 12 patients from retrospective data among the 787 patients included in this analysis, but most cohorts had no severe morbidities. Some patients with post-treatment hepatic insufficiency or Child–Pugh score deterioration were reported in some papers [9, 13, 14]. On the other hand, some patients with improvement in Child–Pugh score after treatment were reported in these papers [9, 14]. Kawashima et al. [13] reported a relatively high rate of hepatic insufficiencies with 8 of 30 patients treated by PBT, but they found two risk factors predicting the tendency of hepatic insufficiency—the retention rate of indocyanine green at 15 min (ICG R15) and the percentage of hepatic noncancerous portions receiving ≥30 Gy (RBE) (V30%). Here, Gy (RBE) is the unit of relative biological effectiveness (RBE)-weighted absorbed dose in PBT, recommended by the International Commission on Radiation Units and Measurements (ICRU) [18]. All studies affirmed the safety of CPT for HCC under adequate patient selection.
Discussion
Summary of findings
The findings from our systematic review suggested high efficacy of CPT on local tumor control, resulting from the theoretical benefit of concentrated radiation dose to the tumor by Bragg peak.
Survival rates depend on patient characteristics such as hepatic functional reserve and number of tumors. However, reported survival rates were promising because most cohorts had inclusion criteria of unresectable HCCs, although comparative evidence and patient selection were at a high risk of bias in this systematic review as shown above. Kato et al. [12] reported an overall survival rate of 50% at 5 years in 6 patients without previous treatment, as a subgroup analysis of their prospective study, which was comparable to the results after surgery. Chiba et al. [19] also reported an excellent survival rate of 53.5% in 50 patients with favorable prognostic factors of Child–Pugh class A and solitary tumor from their retrospective analysis, which was not included in this systematic review because of the potential overlap of patients.
Severe adverse events were limited within the analyzed studies. Only 2.3% (18/787 patients) of grade ≥3 late adverse events were reported. A randomized controlled study also suggested less toxicity after PBT compared with TACE, from the data on days of hospitalization within 30 days of the treatment course (4.6 days and 0.73 days per patient after TACE and PBT, respectively, p < 0.001). There were some patients with post-treatment hepatic insufficiency or Child–Pugh score deterioration in some papers [9, 13, 14]. However, it is difficult to differentiate between the natural clinical course of liver cirrhosis and post-treatment sequelae only by Child–Pugh score deterioration. Some patients with an improvement in Child–Pugh score after treatment were also reported in these papers [9, 14].
From these findings, the Committee for the Revision of the Clinical Practice Guidelines for Hepatocellular Carcinoma of the Japan Society of Hepatology issued a recommendation to the Japanese Clinical Practice Guidelines for Hepatocellular Carcinoma (2017) that particle radiotherapy [PBT and heavy particle (carbon ion) radiotherapy] can be performed for HCC that is difficult to treat with other local therapies (weak recommendation) (authors’ translation) [5].
PBT
HCC treatment by PBT was initiated in 1983 at the High Energy Accelerator Research Organization (KEK) in Japan. Prior to that, PBT was indicated mainly to head and neck lesions such as uveal melanomas, cerebral arteriovenous malformations, pituitary adenomas, and chordomas. However, KEK and the University of Tsukuba proposed the use of PBT to truncal tumors including HCC, and the first clinical trial of PBT for HCC was started. A good local control rate of almost 100% with no severe adverse event was reported with the early clinical experience of PBT for HCC [20,21,22]. Encouraged by this success, PBT for HCC gradually prevailed throughout the world. To date, >50 facilities are in operation worldwide and the number of facilities is still increasing [23]. Many facilities are now treating HCC patients with proton beams.
So far, the largest prospective study of PBT for HCC was reported from the Loma Linda University Medical Center [7, 24], which has the first hospital-based PBT system [25, 26]. Seventy-six patients were included in the trial and treated with a proton dose of 63 Gy (RBE) in 15 fractions between 1998 and 2006. At the last follow-up, 15 patients (20%) had experienced local treatment failure. The median progression-free survival was 36 months (95% CI 30–42 months). Alpha-fetoprotein (AFP) levels decreased significantly after PBT. Among the first 27 patients with an elevated pretreatment AFP level, the mean AFP value decreased from 1405 to 35 ng/mL. No acute toxicity that required treatment interruption of PBT was observed. Five patients experienced grade 2 toxicities of gastrointestinal bleeding or ulcerations near the irradiated area, but these gastrointestinal toxicities were observed only in the patients treated in the earlier period. After the experience of these patients with gastrointestinal toxicities, greater attention was paid to reduce the field margins adjacent to the bowel, and no more grade 2 gastrointestinal toxicities were reported. They also evaluated radiation-induced liver disease via clinical and laboratory evaluation, but no significant overall change was observed in aspartate aminotransferase, alanine aminotransferase, alkaline phosphatase, bilirubin, or albumin levels or prothrombin time after PBT. Albumin levels were slightly decreased down to 2.8 g/dL at 1 month after PBT from the baseline average level of 3.3 g/dL, but recovered to the pretreatment level by 6 months.
Hong et al. [11] reported clinical results of a multi-institutional phase II study from the United States. They enrolled 49 HCC and 43 intrahepatic cholangiocarcinoma (ICC) patients with localized unresectable liver tumors at the Massachusetts General Hospital, MD Anderson Cancer Center, and the University of Pennsylvania. The proton dose was 67.5 Gy (RBE) and 58.05 Gy (RBE) in 15 fractions for peripheral and central tumors, respectively, in general, but dose de-escalation was permitted to keep the dose constraints. After a median follow-up period of 19.5 months, the local control rate was 94.4% (95% CI 87.2–98.2%) at 2 years for all the patients. The rates were similar for HCC and ICC (94.8 vs 94.1%), and no local recurrence was reported among the patients who received ≥60 Gy (RBE). The median progression- survival free and overall survival rates were 13.9 months (95% CI 8.6–49.9 months) and 49.9 months (95% CI 17.8 months for lower bound, but not reached for upper bound), respectively, for HCC patients. Of the 83 patients analyzed, four patients (4.8%) experienced grade 3 radiation-induced toxicity of hepatic functions or gastrointestinal ulcers; however, no grade 4 or grade 5 toxicities were reported. In their analyses, the sum of the longest tumor diameters and the existence of tumor vascular thrombosis did not affect overall survival for HCC patients after PBT.
Bush et al. [8] conducted a prospective randomized clinical trial comparing PBT with TACE, and the results of the interim analysis were reported recently. In this randomized trial, a total of 70 patients who were candidates for both PBT and TACE were enrolled, and 33 patients were assigned to PBT. Local control and progression-free survival rates at 2 years were 88 and 48%, respectively, for the patients in the proton arm, which were better than those of 45 and 31% for the TACE patients; however, the differences between the treatment arms were not statistically significant. In addition, the 2-year overall survival rate was 59% with no difference between the treatment arms. Moreover, the total number of hospitalization days was significantly shorter in the proton arm (24 vs 166 days, p < 0.001). They concluded that PBT might have a role in the treatment of newly diagnosed HCC in some patients.
A retrospective review of the entire clinical experiences of PBT for HCC at the University of Tsukuba was reported [19, 27]. From their entire experience of 162 patients, overall survival and local control rates at 5 years were 23.5% and 86.9%, respectively [19]. Good hepatic function of Child–Pugh class A and solitary tumor were better prognostic factors for survival, and patients with both these two prognostic factors had an overall survival rate of 53.5% at 5 years.
Major possible adverse events after PBT for HCC are gastrointestinal toxicities (bleeding or ulceration) and hepatic insufficiencies. The probability of gastrointestinal toxicities can be decreased by cautious field arrangement of proton beams, as already mentioned above [7]. With regard to hepatic insufficiency after PBT, Kawashima et al. analyzed the dose-volume histogram (DVH) of 60 patients with HCC treated by PBT, and reported ICG R15 and V30% as useful predictors, as is the case with photon radiotherapy [13, 28,29,30,31]. For 20 patients with ICG R15 <20%, there was no hepatic insufficiency after PBT, but 6 of 8 patients with ICG R15 ≥50% died of hepatic insufficiency. In these 8 patients, there was no obvious relationship between the development of hepatic insufficiency and the liver DVH. Among the 32 patients with ICG R15 values of 20–49.9%, none of the 21 patients whose liver V30% was <25% experienced hepatic insufficiency, but 5 of 11 patients (45%) whose liver V30% was ≥25% developed hepatic insufficiency (p = 0.037).
PBT has been used for several challenging disease statuses of HCC. One of the major conditions where treatment options are limited is portal vein tumor thrombosis (PVTT). However, excellent local tumor control can be expected even for tumors with invasion to the main trunk of the portal vein. Sugahara et al. [32] reported a local progression-free rate of 91% at 2 years after PBT for HCC with PVTT. Overall survival rates have also been reported to range from 33.3–57% at 2 years, without treatment-related severe late complications [16, 32, 33]. Another challenging condition is proximity of the tumor to the alimentary tract. Kim et al. proposed a risk-adapted simultaneous integrated boost technique to HCCs to avoid gastrointestinal toxicities [34]. When the planning target volume (PTV) overlaps the planning organ at risk volume (PRV) of the gastrointestinal tract, they prescribed 50–60 Gy (RBE) in 10 fractions to the PTVs minus the overlapping volumes, whereas the dose to the overlapping volumes was restricted to 30 Gy (RBE) in 10 fractions. They treated HCC with tumor vascular thrombosis using PBT, with local recurrence in only 12.2% of patients during the follow-up period, and no isolated local recurrence or severe gastrointestinal toxicity was reported [34]. Mizumoto et al. also reported a risk-adapted selection scheme of the dose fractionation schedules to maintain high local control rates without increasing the risk of late complications. They adopted a small fraction dose schedule of 77 Gy (RBE) in 35 fractions with gastrointestinal tract avoidance as far as possible after 40–50 Gy (RBE) for tumors proximal to the alimentary tract with a reduced risk of gastrointestinal toxicities [35]. In addition, decent local control rates can be expected for HCC patients with large tumors (87% at 2 years for tumors >10 cm), or portal tumors (86% at 3 years), and elderly patients (100% at 3 years for patients aged ≥80 years) [36,37,38]. Even for recurrent tumors after PBT, repeated PBT can be safely delivered with a good local control rate of 87.8% at 5 years [39]. An overview of these treatment results indicates that PBT appears to be useful even in cases with limited treatment options.
Carbon ion therapy
Carbon ion therapy for HCC was first started in Japan in 1995 at the National Institute of Radiological Sciences (NIRS) in expectation that the biological benefit of high RBE and high linear energy transfer (LET) of carbon ion beam can yield better treatment efficacy than photon or proton therapy [12, 17].
Kato et al. [12] published the first clinical results of carbon ion therapy for HCC in 2004 from the NIRS. They enrolled 24 patients and conducted a phase I/II study by dose escalation with a total dose of 49.5–79.5 Gy (RBE) in 15 fractions. The cumulative local control and overall survival rates were 81 and 50% at 3 years, respectively. The overall survival rate of the 6 patients without previous treatment for HCC was 83 and 50% at 3 years and 5 years, respectively, which was higher than that of patients with previous treatment (p = 0.04). There was no local recurrence among the 6 patients whose total dose was 72.0 Gy (RBE) or higher. No severe adverse events were observed at any dose level. They proved the safety and effectiveness of carbon ion therapy for HCC, and their recommended total dose was 72.0 Gy (RBE) in 15 fractions.
To date, NIRS researchers have conducted several other clinical trials for HCC with short-course irradiation regimens [17]. The superiority of short-course hypofractionated regimens was proved by biological experiments which demonstrated that the RBE values of the carbon ion beam for both tumor and normal tissues were lowered when the fraction dose increased, and the decrease in the RBE value for normal tissues was steeper than that for tumors [40, 41]. A four-fraction regimen with a total dose of 52.8 Gy (RBE) also yielded a high local control rate of 94% at 3 years [17]. Local control rates for porta hepatis lesions were slightly worse than those for non-porta hepatis lesions, but the difference was not statistically significant (87.8 vs 95.7%, p = 0.306) [42]. Two-fracion regimens are now being adopted and have treated >110 patients, with minor adverse events only [43]. The mature data of their clinical results are not available yet.
A phase I dose escalation study (the PROMETHEUS-01 trial) was also carried out in Germany [44]. The total dose was escalated from 40 Gy (RBE) up to 56 Gy (RBE) in 4 fractions. Their early experiences with six patients treated with a 4 × 10 Gy (RBE) scheme were retrospectively reviewed [45]. With a median follow-up period of 11 months, all 7 irradiated tumors were locally controlled, and no severe adverse events occurred. The results of longer follow-up and dose escalation will be reported in the future.
Comparison between proton beam and carbon ion
To date, the Hyogo Ion Beam Medical Center (HIBMC) is the only facility in the world where treatment results of HCC by both proton beam and carbon ion therapies are available. Komatsu et al. [15] evaluated the clinical outcome of 343 consecutive HCC patients with 386 tumors, including 242 patients with 278 tumors treated by PBT and 101 patients with 108 tumors treated by carbon ion therapy at the HIBMC. They selected a better suited beam by direct comparison of the dose distribution of two beam types. Local control rates for proton beam and carbon ion were 90.2 and 93%, respectively, at 5 years after various dose fractionation schemes [15]. Tumor size was an independent risk factor for local control in multivariate analysis, and local control rates of tumors <50 mm, 50–100 mm, and >100 mm were 95.3, 84.4, and 42.2%, respectively, at 5 years. For tumors <50 mm, local control rates were equivalent for both beam types (95.5 and 94.5% for proton beam and carbon ion, respectively, at 5 years), but for larger tumors, local control rates after PBT appear slightly lower than those for carbon ion therapy, although the number of patients with tumors >100 mm is very small (84.1 and 90.9% for tumors of 50–100 mm, and 43.4 and 80% for tumors >100 mm for proton beam and carbon ion, respectively, at 5 years).
Future prospects for CPT
Recent progress in particle therapy technology is remarkable, especially for the spot-scanning technique [46,47,48]. Spot-scanning irradiation uses a number of pencil beams of charged particles with a certain single energy for highly conformal sophisticated dose distribution by changing the irradiation point and its beam energy adequately according to the shape of the tumor. With this advanced technique, uninvolved liver tissues can be spared from higher dose radiation, and morbidities after CPT will be decreased. In addition, contamination of secondary neutrons can be reduced because the spot-scanning system does not use collimators, compensators, and scattering foil [49]. It generally takes longer for irradiation by spot scanning compared to the conventional passive scattering technique and the dose distributions are susceptible to target movement, known as the ‘interplay’ effect. However, with the recent systems using high-speed response and accurate control of the beam position, these drawbacks are gradually being resolved, and the irradiation time by the spot-scanning technique is becoming equivalent to that by conventional techniques, even for moving targets like HCCs [50]. More sophisticated future systems are expected to overcome these problems completely.
The efficacy of CPT is increasingly being recognized worldwide, as treatment results are being accumulated. However, it is extremely difficult to conduct randomized phase III trials of direct comparison with other treatment modalities by the conventional method of evidence-based medicine. This is because of the limited number of CPT facilities and the fact that the therapy is far less invasive compared to other treatment modalities for HCC. In spite of these difficulties, some phase III trials are ongoing or have been planned in order to directly compare CPT with TACE or radiofrequency ablation [8, 51, 52]. A direct comparison between CPT and surgery for HCC appears to be the most difficult, but the Japanese Clinical Oncology Group is now planning a non-randomized prospective concurrent control study between surgery and PBT for HCC. In this study, HCC patients who are candidates for both surgery and PBT will undergo either treatment at the patient’s discretion and the primary endpoint of this study is overall survival. The study is expected to cover a 10-year period, but the significance of PBT for HCC will be established when the results are revealed.
In addition, the American Society for Radiation Oncology (ASTRO) issued a Model Policy on PBT in 2014 [53], and PBT for HCC is now covered by medical insurance in the United States. In Japan, PBT and carbon ion therapy are covered only for pediatric tumors and bone and soft tissue tumors, respectively, and are not yet covered for HCC by the Japanese national health insurance. The Japanese Clinical Study Group of Particle Therapy (JCPT), the Japanese Society for Radiation Oncology (JASTRO), the Japanese Radiation Oncology Study Group (JROSG) and other groups are now conducting multi-institutional prospective clinical trials in order to obtain approval for national health insurance for HCC and other cancers. CPT or PBT is regarded as a possible treatment option in some clinical practice guidelines from the Japan Society of Hepatology and the National Comprehensive Cancer Network (NCCN) [3, 4, 54]. The NCCN guidelines recommend that PBT may be appropriate in specific situations [3]. In the Japanese guidelines, CPT can be considered for HCCs that are difficult to treat with other local therapies, especially for therapeutically intractable tumors such as those with portal vein or inferior vena cava tumor thrombus and large lesions [4, 5]. The Korean Liver Cancer Study Group also mentioned the efficacy of PBT in the commentary text within their guidelines [55, 56]. There are many other practice guidelines for HCC where there is no report of CPT [57,58,59,60,61,62,63]. However, the Japan, Korean, and NCCN guidelines for HCC will have an influence on the pattern of clinical practice in other countries or societies, because these guidelines are often referred to throughout the world.
As a result of the recent circumstances concerning CPT for HCC, it is hoped that further excellent clinical results after CPT will be accumulated worldwide, and that CPT will be applied much more often for the treatment of HCC in the coming decade.
Limitations
The results of our systematic review process indicated some limitations of this study.
There was only one study which compared PBT with another treatment modality [8], and this was also a report of an interim analysis. All other reports included in our analysis were studies with a single-arm treatment of CPT. Therefore, our results were difficult to compare with other treatment modalities, although most studies were prospective except for two. In particular, overall survival rate depends on patient characteristics such as hepatic functional reserve and the number and size of the tumor.
There were many retrospective reports from the University of Tsukuba [27, 32, 33, 36,37,38,39, 64,65,66,67]. These retrospective studies were excluded from our systematic review process because of the potential overlap of patients. Their experience of PBT for HCC with a total of 318 patients [27], tumors located adjacent to the alimentary tract [35, 64] or to the porta hepatis [37], tumors associated with portal vein tumor thrombosis [32, 33] or with inferior vena cava tumor thrombus [65], and large tumors [38] were excluded. Their experience of patients with severe cirrhosis [66], patients for whom other treatment modalities either were contraindicative or were unfeasible [67], elderly patients [36], or repeated treatment [39] were not included in this systematic review. However, these excluded reports were extremely important and might represent the true efficacy of PBT, because many of the patients with limited treatment options other than CPT were successfully treated by PBT. Indeed, a wider range of HCC patients can be treated by CPT than by other ablative treatment modalities for HCC. Most prospective trials included patients with tumors invading the portal vein or tumors >5 cm [7,8,9,10,11,12,13,14,15,16]. In addition, retrospective studies suggested that CPT can be indicated irrespective of tumor location, and even larger tumors (>10 cm) can be treated effectively by PBT [35, 38]. Child–Pugh class C patients are difficult to treat even by CPT, but there is almost no other contraindication of CPT for HCC. Repeated treatment can also be considered if the tumor is located in the peripheral region of the liver with good hepatic function with minimal side-effects [39, 68].
Conclusions
CPT for HCC was associated with good local control with limited probability of severe morbidities, because charged particles have superiority in depth dose distribution compared to photons. Accordingly, CPT might be more beneficial than SBRT for the treatment of HCC which is usually surrounded by cirrhotic liver with high radiation-sensitive tissues. This is gradually being recognized worldwide through reports of high local control rates after CPT. Survival rates after CPT are also promising, and comparative data collections are now ongoing. Although it is very difficult to conduct randomized controlled trials of CPT, evidence of CPT for HCC is slowly and steadily being compiled.
The next step is to clarify the cost-effectiveness of CPT. In addition, the distinctive clinical advantages of PBT and carbon ion therapy should also be revealed. Through these efforts, CPT for HCC will become a socially accepted treatment modality for HCC.
References
Petrick JL, Braunlin M, Laversanne M et al (2016) International trends in liver cancer incidence, overall and by histologic subtype, 1978–2007. Int J Cancer 139(7):1534–1545. doi:10.1002/ijc.30211
Zhang Y, Ren JS, Shi JF et al (2015) International trends in primary liver cancer incidence from 1973 to 2007. BMC Cancer 15:94. doi:10.1186/s12885-015-1113-4
Natinal Comprehensive Cancer Network (2017) Hepatobiliary cancers. In: NCCN clinical practice guidelines in oncology. https://www.nccn.org/professionals/physician_gls/pdf/hepatobiliary.pdf. Accessed Mar. 2017
Japan Society of Hepatology (2013) Evidence-based clinical practice guidelines for hepatocellular carcinoma, 3rd edn. Kanehara Shuppan, Tokyo
Japan Society of Hepatology (in press) Clinical practice guidelines for hepatocellular carcinoma, 4th edn. Kanehara Shuppan, Tokyo
Moher D, Liberati A, Tetzlaff J et al (2009) Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. BMJ 339:b2535. doi:10.1136/bmj.b2535
Bush DA, Kayali Z, Grove R et al (2011) The safety and efficacy of high-dose proton beam radiotherapy for hepatocellular carcinoma: a phase 2 prospective trial. Cancer 117(13):3053–3059. doi:10.1002/cncr.25809
Bush DA, Smith JC, Slater JD et al (2016) Randomized clinical trial comparing proton beam radiation therapy with transarterial chemoembolization for hepatocellular carcinoma: results of an interim analysis. Int J Radiat Oncol Biol Phys 95(1):477–482. doi:10.1016/j.ijrobp.2016.02.027
Fukumitsu N, Sugahara S, Nakayama H et al (2009) A prospective study of hypofractionated proton beam therapy for patients with hepatocellular carcinoma. Int J Radiat Oncol Biol Phys 74(3):831–836. doi:10.1016/j.ijrobp.2008.10.073
Hong TS, DeLaney TF, Mamon HJ et al (2014) A prospective feasibility study of respiratory-gated proton beam therapy for liver tumors. Pract Radiat Oncol 4(5):316–322. doi:10.1016/j.prro.2013.10.002
Hong TS, Wo JY, Yeap BY et al (2016) Multi-institutional phase II study of high-dose hypofractionated proton beam therapy in patients with localized, unresectable hepatocellular carcinoma and intrahepatic cholangiocarcinoma. J Clin Oncol 34(5):460–468. doi:10.1200/JCO.2015.64.2710
Kato H, Tsujii H, Miyamoto T et al (2004) Results of the first prospective study of carbon ion radiotherapy for hepatocellular carcinoma with liver cirrhosis. Int J Radiat Oncol Biol Phys 59(5):1468–1476. doi:10.1016/j.ijrobp.2004.01.032
Kawashima M, Furuse J, Nishio T et al (2005) Phase II study of radiotherapy employing proton beam for hepatocellular carcinoma. J Clin Oncol 23(9):1839–1846. doi:10.1200/JCO.2005.00.620
Kim TH, Park JW, Kim YJ et al (2015) Phase I dose-escalation study of proton beam therapy for inoperable hepatocellular carcinoma. Cancer Res Treat 47(1):34–45. doi:10.4143/crt.2013.218
Komatsu S, Fukumoto T, Demizu Y et al (2011) Clinical results and risk factors of proton and carbon ion therapy for hepatocellular carcinoma. Cancer 117(21):4890–4904. doi:10.1002/cncr.26134
Lee SU, Park JW, Kim TH et al (2014) Effectiveness and safety of proton beam therapy for advanced hepatocellular carcinoma with portal vein tumor thrombosis. Strahlenther Onkol 190(9):806–814. doi:10.1007/s00066-014-0604-6
Tsujii H, Mizoe J, Kamada T et al (2007) Clinical results of carbon ion radiotherapy at NIRS. J Radiat Res 48(Suppl A):A1–A13
ICRU (2007) Prescribing, recording, and reporting proton-beam therapy
Chiba T, Tokuuye K, Matsuzaki Y et al (2005) Proton beam therapy for hepatocellular carcinoma: a retrospective review of 162 patients. Clin Cancer Res 11(10):3799–3805. doi:10.1158/1078-0432.CCR-04-1350
Matsuzaki Y, Osuga T, Chiba T et al (1995) New, effective treatment using proton irradiation for unresectable hepatocellular carcinoma. Intern Med 34(4):302–304
Matsuzaki Y, Osuga T, Saito Y et al (1994) A new, effective, and safe therapeutic option using proton irradiation for hepatocellular carcinoma. Gastroenterology 106(4):1032–1041
Tanaka N, Matsuzaki Y, Chuganji Y et al (1992) Proton irradiation for hepatocellular carcinoma. Lancet 340(8831):1358
Particle Therapy Co-operative Group (2017) Particle therapy facilities in operation. https://www.ptcog.ch/index.php/facilities-in-operation. Accessed Mar 2017
Bush DA, Hillebrand DJ, Slater JM et al (2004) High-dose proton beam radiotherapy of hepatocellular carcinoma: preliminary results of a phase II trial. Gastroenterology 127(5 Suppl 1):S189–S193
Slater JM, Miller DW, Archambeau JO (1988) Development of a hospital-based proton beam treatment center. Int J Radiat Oncol Biol Phys 14(4):761–775
Coutrakon G, Hubbard J, Johanning J et al (1994) A performance study of the Loma Linda proton medical accelerator. Med Phys 21(11):1691–1701. doi:10.1118/1.597270
Nakayama H, Sugahara S, Tokita M et al (2009) Proton beam therapy for hepatocellular carcinoma: the University of Tsukuba experience. Cancer 115(23):5499–5506. doi:10.1002/cncr.24619
Pan CC, Kavanagh BD, Dawson LA et al (2010) Radiation-associated liver injury. Int J Radiat Oncol Biol Phys 76(3 Suppl):S94–S100. doi:10.1016/j.ijrobp.2009.06.092
Kawashima M, Kohno R, Nakachi K et al (2011) Dose-volume histogram analysis of the safety of proton beam therapy for unresectable hepatocellular carcinoma. Int J Radiat Oncol Biol Phys 79(5):1479–1486. doi:10.1016/j.ijrobp.2009.12.048
Yoon HI, Koom WS, Lee IJ et al (2012) The significance of ICG-R15 in predicting hepatic toxicity in patients receiving radiotherapy for hepatocellular carcinoma. Liver Int 32(7):1165–1171. doi:10.1111/j.1478-3231.2012.02784.x
Mizumoto M, Oshiro Y, Okumura T et al (2014) Association between pretreatment retention rate of indocyanine green 15 min after administration and life prognosis in patients with HCC treated by proton beam therapy. Radiother Oncol 113(1):54–59. doi:10.1016/j.radonc.2014.08.015
Sugahara S, Nakayama H, Fukuda K et al (2009) Proton-beam therapy for hepatocellular carcinoma associated with portal vein tumor thrombosis. Strahlenther Onkol 185(12):782–788. doi:10.1007/s00066-009-2020-x
Hata M, Tokuuye K, Sugahara S et al (2005) Proton beam therapy for hepatocellular carcinoma with portal vein tumor thrombus. Cancer 104(4):794–801. doi:10.1002/cncr.21237
Kim DY, Park JW, Kim TH et al (2017) Risk-adapted simultaneous integrated boost-proton beam therapy (SIB-PBT) for advanced hepatocellular carcinoma with tumour vascular thrombosis. Radiother Oncol 122(1):122–129. doi:10.1016/j.radonc.2016.12.014
Mizumoto M, Okumura T, Hashimoto T et al (2011) Proton beam therapy for hepatocellular carcinoma: a comparison of three treatment protocols. Int J Radiat Oncol Biol Phys 81(4):1039–1045. doi:10.1016/j.ijrobp.2010.07.015
Hata M, Tokuuye K, Sugahara S et al (2007) Proton beam therapy for aged patients with hepatocellular carcinoma. Int J Radiat Oncol Biol Phys 69(3):805–812. doi:10.1016/j.ijrobp.2007.04.016
Mizumoto M, Tokuuye K, Sugahara S et al (2008) Proton beam therapy for hepatocellular carcinoma adjacent to the porta hepatis. Int J Radiat Oncol Biol Phys 71(2):462–467. doi:10.1016/j.ijrobp.2007.09.056
Sugahara S, Oshiro Y, Nakayama H et al (2010) Proton beam therapy for large hepatocellular carcinoma. Int J Radiat Oncol Biol Phys 76(2):460–466. doi:10.1016/j.ijrobp.2009.02.030
Hashimoto T, Tokuuye K, Fukumitsu N et al (2006) Repeated proton beam therapy for hepatocellular carcinoma. Int J Radiat Oncol Biol Phys 65(1):196–202. doi:10.1016/j.ijrobp.2005.11.043
Koike S, Ando K, Uzawa A et al (2002) Significance of fractionated irradiation for the biological therapeutic gain of carbon ions. Radiat Prot Dosimetry 99(1–4):405–408
Ando K, Koike S, Uzawa A et al (2005) Biological gain of carbon-ion radiotherapy for the early response of tumor growth delay and against early response of skin reaction in mice. J Radiat Res 46(1):51–57
Imada H, Kato H, Yasuda S et al (2010) Comparison of efficacy and toxicity of short-course carbon ion radiotherapy for hepatocellular carcinoma depending on their proximity to the porta hepatis. Radiother Oncol 96(2):231–235. doi:10.1016/j.radonc.2010.05.019
Kamada T, Tsujii H, Blakely EA et al (2015) Carbon ion radiotherapy in Japan: an assessment of 20 years of clinical experience. Lancet Oncol 16(2):e93–e100. doi:10.1016/S1470-2045(14)70412-7
Combs SE, Habermehl D, Ganten T et al (2011) Phase i study evaluating the treatment of patients with hepatocellular carcinoma (HCC) with carbon ion radiotherapy: the PROMETHEUS-01 trial. BMC Cancer 11:67. doi:10.1186/1471-2407-11-67
Habermehl D, Debus J, Ganten T et al (2013) Hypofractionated carbon ion therapy delivered with scanned ion beams for patients with hepatocellular carcinoma—feasibility and clinical response. Radiat Oncol 8:59. doi:10.1186/1748-717X-8-59
Pedroni E, Bacher R, Blattmann H et al (1995) The 200-MeV proton therapy project at the Paul Scherrer Institute: conceptual design and practical realization. Med Phys 22(1):37–53. doi:10.1118/1.597522
Gillin MT, Sahoo N, Bues M et al (2010) Commissioning of the discrete spot scanning proton beam delivery system at the University of Texas M.D. Anderson Cancer Center, Proton Therapy Center, Houston. Med Phys 37(1):154–163. doi:10.1118/1.3259742
Shimizu S, Miyamoto N, Matsuura T et al (2014) A proton beam therapy system dedicated to spot-scanning increases accuracy with moving tumors by real-time imaging and gating and reduces equipment size. PLoS One 9(4):e94971. doi:10.1371/journal.pone.0094971
Schneider U, Agosteo S, Pedroni E et al (2002) Secondary neutron dose during proton therapy using spot scanning. Int J Radiat Oncol Biol Phys 53(1):244–251
Furukawa T, Inaniwa T, Sato S et al (2010) Performance of the NIRS fast scanning system for heavy-ion radiotherapy. Med Phys 37(11):5672–5682. doi:10.1118/1.3501313
United States National Institute of Health (2009) Transarterial chemoembolization versus proton beam radiotherapy for the treatment of hepatocellular carcinoma. In: ClinicalTrails.gov. https://clinicaltrials.gov/ct2/show/NCT00857805. Accessed Mar 2017
United States National Institute of Health (2013) Comparison between radiofrequency ablation and hypofractionated proton beam radiation for recurrent/residual HCC. In: ClinicalTrails.gov. https://clinicaltrials.gov/ct2/show/NCT01963429. Accessed Mar. 2017
American Society for Radiation Oncology (2014) Proton beam therapy model policy issued by ASTRO. https://www.astro.org/News-and-Publications/News-and-Media-Center/News-Releases/2014/Proton-Beam-Therapy-Model-Policy-issued-by-ASTRO/. Accessed Mar 2017
Kokudo N, Hasegawa K, Akahane M et al (2015) Evidence-based clinical practice guidelines for hepatocellular carcinoma: the Japan Society of Hepatology 2013 update (3rd JSH-HCC Guidelines). Hepatol Res 45(2):123–127. doi:10.1111/hepr.12464
Korean Liver Cancer Study Group, National Cancer Center Korea (2015) 2014 KLCSG-NCC Korea practice guideline for the management of hepatocellular carcinoma. Gut Liver 9(3):267–317. doi:10.5009/gnl14460
Korean Liver Cancer Study Group, National Cancer Center Korea (2015) 2014 Korean Liver Cancer Study Group-National Cancer Center Korea practice guideline for the management of hepatocellular carcinoma. Korean J Radiol 16(3):465–522. doi:10.3348/kjr.2015.16.3.465
Ryder SD, British Society of Gastroenterology (2003) Guidelines for the diagnosis and treatment of hepatocellular carcinoma (HCC) in adults. Gut 52(Suppl 3):iii1–iii8
Ferenci P, Fried M, Labrecque D et al (2010) Hepatocellular carcinoma (HCC): a global perspective. J Clin Gastroenterol 44(4):239–245. doi:10.1097/MCG.0b013e3181d46ef2
Omata M, Lesmana LA, Tateishi R et al (2010) Asian Pacific Association for the Study of the Liver consensus recommendations on hepatocellular carcinoma. Hepatol Int 4(2):439–474. doi:10.1007/s12072-010-9165-7
Abdo AA, Hassanain M, AlJumah A et al (2012) Saudi guidelines for the diagnosis and management of hepatocellular carcinoma: technical review and practice guidelines. Ann Saudi Med 32(2):174–199
European Association for Study of Liver, European Organisation for Research and Treatment of Cancer (2012) EASL-EORTC clinical practice guidelines: management of hepatocellular carcinoma. Eur J Cancer 48(5):599–641. doi:10.1016/j.ejca.2011.12.021
Verslype C, Rosmorduc O, Rougier P et al (2012) Hepatocellular carcinoma: ESMO-ESDO Clinical Practice Guidelines for diagnosis, treatment and follow-up. Ann Oncol 23(Suppl 7):41–48. doi:10.1093/annonc/mds225
Carrillo FJ, Mattos AA, Vianey AF et al (2015) Brazilian society of hepatology recommendations for the diagnosis and treatment of hepatocellular carcinoma. Arq Gastroenterol 52(Suppl 1):2–14. doi:10.1590/S0004-28032015000500001
Nakayama H, Sugahara S, Fukuda K et al (2011) Proton beam therapy for hepatocellular carcinoma located adjacent to the alimentary tract. Int J Radiat Oncol Biol Phys 80(4):992–995. doi:10.1016/j.ijrobp.2010.03.015
Mizumoto M, Tokuuye K, Sugahara S et al (2007) Proton beam therapy for hepatocellular carcinoma with inferior vena cava tumor thrombus: report of three cases. Jpn J Clin Oncol 37(6):459–462. doi:10.1093/jjco/hym038
Hata M, Tokuuye K, Sugahara S et al (2006) Proton beam therapy for hepatocellular carcinoma patients with severe cirrhosis. Strahlenther Onkol 182(12):713–720. doi:10.1007/s00066-006-1564-2
Hata M, Tokuuye K, Sugahara S et al (2006) Proton beam therapy for hepatocellular carcinoma with limited treatment options. Cancer 107(3):591–598. doi:10.1002/cncr.22039
Mayahara H, Oda Y, Kawaguchi A et al (2005) A case of hepatocellular carcinoma initially treated by carbon ions, followed by protons for marginal recurrence with portal thrombus. Radiat Med 23(7):513–519
Acknowledgements
The authors would like to thank the following foundation and individuals for their assistance in developing this report. The general incorporated foundation of the Japan Society of Hepatology (Tokyo, Japan) developed and implemented the search strategy and conducted a literature search. Dr. Atsuya Takeda (Ofuna Chuo Hospital) and Dr. Ken Harada (Tokai University) helped with screening and retrieval of the literature review. This study was supported in part by JSPS KAKENHI [Grant numbers 16K10410 (Grant recipient: HI), 15H04901 (Grant recipient: HS), 16K10383 (Grant recipient: TO)].
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
About this article
Cite this article
Igaki, H., Mizumoto, M., Okumura, T. et al. A systematic review of publications on charged particle therapy for hepatocellular carcinoma. Int J Clin Oncol 23, 423–433 (2018). https://doi.org/10.1007/s10147-017-1190-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10147-017-1190-2