Abstract
Background
Esophagectomy following neoadjuvant chemotherapy (NAC) is a standard treatment for resectable advanced esophageal cancer in Japan. However, approximately 10 % of patients with resectable advanced esophageal cancer experience recurrence within 6 months.
Methods
One hundred twenty-eight patients with resectable advanced esophageal cancer underwent NAC between October 2008 and July 2015 in Kumamoto University Hospital. Among them, 82 patients with esophageal squamous cell carcinoma (SCC), who underwent curative esophagectomy without adjuvant treatment, were eligible. Clinicopathological factors correlated with early recurrence were retrospectively analyzed.
Results
Of 82 patients, 14 (17 %) recurred within 6 months after surgery. The logistic regression analysis suggested that CRP before NAC ≥ 0.5 mg/dl [hazard ratio (HR) 33.8, 95 % confidence interval (CI) 2.767–413.9; p = 0.006), presence of poorly differentiated SCC component (HR 138, 95 % CI 5.339–3576; p = 0.003), and pathological vessel invasion (HR 16.3, 95 % CI 1.960–136.1; p = 0.010) were candidates for independent risk factors of early recurrence. Patients with at least two factors frequently recurred (82 %). Of 14 patients with early recurrence, 13 (93 %) had a distant metastasis.
Conclusions
Patients with resectable advanced esophageal cancer with at least two factors of CRP before NAC ≥ 0.5 mg/dl, presence of poorly differentiated SCC component, and pathological vessel invasion might be at high risk for early recurrence after esophagectomy following NAC. These patients might be considered for additional treatment and should be meticulously followed up after treatment.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Although esophageal cancer remains a refractory neoplasm, treatment results have been improving in the recent decade [1]. Regarding resectable advanced esophageal cancer, the 5-year overall survival (OS) rate was reported to be 17–52 % when treated with surgery alone [2–4]. Recent randomized controlled trials (RCTs) proved that additional treatment with esophagectomy significantly improved the 5-year OS compared with those after surgery alone [2–5]. The standard treatment for resectable advanced esophageal cancer differs between Western and Eastern countries. In Western countries, neoadjuvant chemoradiotherapy (CRT) is common. However, in Japan, neoadjuvant chemotherapy (NAC) is usually considered before esophagectomy [6].
In patients with resectable advanced esophageal cancer, early recurrence sometimes occurs after these standard treatments. In previous studies on NAC, approximately 10 % of patients with resectable advanced esophageal cancer were noted to recur within 6 months after surgery [6–9]. Although these patients might require further treatment or meticulous follow-up after surgery, it is unclear as to which cohort might recur in such an early period. Although there are several studies on the risk factors of early recurrence after surgery alone or neoadjuvant treatment including CRT [10–13], to our knowledge, the risk factors of early recurrence after only NAC for resectable advanced esophageal cancer have never been investigated.
In the present study, we retrospectively examined the clinicopathological factors in patients with resectable advanced esophageal cancer, which correlate with early recurrence within 6 months after esophagectomy following NAC. In addition, we also investigated the pattern of early recurrences to estimate the ideal additional treatment.
Materials and methods
Patients
Between October 2008 and July 2015, 128 patients with resectable advanced esophageal cancer received NAC, which consisted of docetaxel, cisplatin, and 5-FU (DCF), or 5-fluorouracil (FU) and cisplatin (FP), followed by surgery at the Department of Gastroenterological Surgery, Kumamoto University. Among these patients, 6 who underwent surgery other than subtotal esophagectomy, 4 who had remnant cancer after esophagectomy, 6 who were followed up not more than 6 months after surgery, and 8 who had a cancer histologically different from squamous cell carcinoma (SCC) were excluded from this study. Moreover, 22 patients who received additional treatment after surgery were also excluded because such treatments certainly affect the timing of recurrence. Consequently, 82 patients were eligible for this study. Clinical, surgical, and pathological data were collected from among the prospectively entered data in the clinical database. The pretreatment tumor stage was classified according to the Union for International Cancer Control (UICC) TNM staging, version 7 [14]. Our institutional ethics committee approved this study (Registry No. 1067). Documented comprehensive consent was obtained from all the patients.
Treatment strategy
The treatment strategy for esophageal cancer was as follows: for patients with T1, node-negative tumors, we performed esophagectomy without preoperative treatment. For patients with T2/T3, node-negative tumors, or non-T4, node-positive tumors, which indicate resectable advanced esophageal cancer, NAC was administered before esophagectomy. For patients with T4 tumors, induction CRT was indicated. Definitive CRT was considered when patients preferred nonsurgical treatment, regardless of the tumor stage. When the use of CRT failed to locally control the carcinoma, we recommended salvage esophagectomy.
Neoadjuvant chemotherapy
The applied DCF regimen consisted of docetaxel (60 mg/m2), administered intravenously (IV) on day 1, followed by cisplatin (6 mg/m2), administered IV on days 1–5, and 5-FU (350 mg/m2), administered continuously IV on days 1–5. This regimen cycle was repeated every 3 weeks [15]. The applied FP regimen consisted of cisplatin (80 mg/m2), administered IV on day 1, followed by 5-FU (800 mg/m2), administered continuously IV on days 1–5. This regimen cycle was repeated every 4 weeks. Although DCF was principally administered, FP was considered when patients had an allergy to docetaxel. Most patients received two cycles of each regimen and underwent elective subtotal esophagectomy at 3–4 weeks after the last round of NAC.
Subtotal esophagectomy
Esophagectomy in this study was defined as a subtotal esophagectomy with two- or three-field regional lymph node dissection that required three incisional manipulations (neck, chest, and abdomen). When tumors were located in the upper or middle thoracic esophagus, three-field lymph node dissection was performed. For lower esophageal tumors, dissection of the cervical lymph nodes was omitted when tumor depth could be classified as within clinical stage T1. Minimally invasive esophagectomy (MIE) was defined as surgery performed using only thoracoscopy, regardless of the use of laparoscopy in the abdomen. MIE for clinical T1 and T2 cases was adopted after May 2011.
Definition of morbidities
We applied the definitions of risk-adjusted morbidity and mortality for esophagectomy for cancer in accordance with the Society of Thoracic Surgeons General Thoracic Surgery Database guidelines [16]. Pulmonary morbidity was defined as the presence of one or more of the following postoperative conditions: initial ventilatory support for more than 48 h or reintubation for respiratory failure, need for tracheostomy, and pneumonia. Pneumonia was defined as the presence of new infiltrates as seen on chest radiographs and a positive culture result from bronchoalveolar lavage. Furthermore, any pulmonary morbidity requiring intervention or surgical treatment was included. Surgical site infection (SSI) was defined as an infection that occurred within 30 days of surgery in the area of the body affected by the surgery, including superficial incisional, deep incisional, and organ/space SSIs. Anastomotic leak was defined based on signs of clinical leakage such as rubefaction, skin edema, emission of digestive fluid or pus from the wound or drain, or a radiographically apparent leak confirmed by using esophagography or computed tomography (CT). Cardiovascular morbidity was defined as the presence of any cardiac disorders such as arrhythmia, ischemic heart disease, and pericardial fluid collection requiring pharmacological, electrical, or interventional treatment, as well as the presence of any thrombosis in accordance with the Common Terminology Criteria for Adverse Events, version 4.03 [17]. Morbidity was defined as morbidity with a Clavien–Dindo classification (CDc) ≥II [18]. Severe morbidity was defined as morbidity with a CDc ≥IIIb, which indicates the need for surgical, endoscopic, or radiological intervention under general anesthesia.
Follow-up evaluation
The patients were followed up at 3-month intervals. Recurrence was confirmed by performing clinical examinations, including CT and endoscopy. Tumor marker levels were measured every 3 months until 5 years after surgery. CT scanning from the neck to the upper abdomen was performed at least twice a year for 3 years after surgery. When recurrence was strongly suggested as observed on CT, [18F]-fluorodeoxyglucose–positron emission tomography CT (FDG-PET CT) was considered. Patients who had recurrence within 6 months after esophagectomy were defined as having early recurrence in this study.
Statistical analyses
Statistical analyses were performed by using the software program StatView version 5.0 (Abacus Concepts, Berkeley, CA, USA). Statistical comparisons between the groups were performed by using the chi-square test. When the matrix contained fewer than five patients, Fisher’s exact test was used. The Mann–Whitney U test was used for unpaired samples. Linear regression analysis between two variables was carried out using a simple regression method. The following clinical factors were adopted for analyses of risk factors of early recurrence: age, sex, performance status, American Society of Anesthesiologists Performance status, Brinkman index, body mass index (BMI), tumor location, clinical T, clinical N, number of lymph node metastases, type of NAC regimen, effect of NAC, presence of diabetes mellitus, respiratory comorbidity, cardiovascular comorbidity, pretreatment and preoperative value of albumin, C-reactive protein (CRP), SCC, width of dissection field, use of MIE, incidence of any morbidity, pneumonia, pulmonary morbidity, leak, surgical site infection, cardiovascular morbidity, severe morbidity, reoperation, presence of poorly SCC component, pathological T, pathological N, number of pathological lymph node metastases, presence of lymphatic invasion, and vessel invasion. BMI was divided into two groups (<18.5 kg/m2, or ≥18.5 kg/m2) according to the BMI as recommended by the World Health Organization [19]. Number of lymph node metastases was divided into two groups (0–2, ≥3) according to the median value. Pretreatment and preoperative value of albumin and CRP were divided in two groups (<3.5 g/dl, ≥3.5 g/dl, and <0.5 mg/dl, ≥0.5 mg/dl) based on each standard value. Clinical response (effect of NAC) was evaluated according to the Response Evaluation Criteria in Solid Tumors (RECIST) v 1.1 [20]. Valuables with a probability level ≤0.1 (clinical T, albumin before NAC, CRP before NAC, reoperation, presence of poorly SCC component, pathological T, number of pathological lymph node metastases, lymphatic invasion, and vessel invasion) were considered to be possibly associated with early recurrence and adopted for the subsequent multivariate analysis. However, if clinical T and pathological T were closely associated with each other, we deleted clinical T according to the hazard ratio in univariate analysis. In the logistic regression analysis, factors for which the p value was <0.05 were considered to be independent risk factors.
Results
A total of 82 patients received NAC with the DCF (74 patients) or FP (8 patients) regimen and subsequent esophagectomy. Of these patients, 14 patients (17 %) recurred within 6 months after esophagectomy following NAC. Of 14 recurrences, 5 were detected by planned CT at 6 months. Six recurrences with metastasis in the skin or cervical LN or bone or local recurrence were discovered by CT or PET CT for examination of patient symptoms from postoperative day (POD) 58 to POD 140. Two recurrences of dissemination or abdominal LN was detected by PET CT to scrutinize the cause of elevation of tumor marker at 3 months. One recurrence of mediastinal LN was discovered by CT at the time of two-stage surgery for reconstruction in POD 70. Of 82 patients, 11 patients received only one cycle of NAC because of adverse events (enteritis, 2 patients; ischemic colitis, 1; diverticulitis, 1; pleurisy, 1; aneurysmal inflammation, 1 patient) or patient refusal to undergo the next cycle (5 patients). Patient backgrounds are listed in Table 1. Patients with early recurrence had significantly more advanced clinical T stage. Albumin level before NAC was significantly lower and CRP level before NAC was significantly higher in patients with early recurrence.
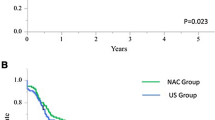
Surgical outcomes are listed in Table 2. Any postoperative morbidity did not affect the incidence of early recurrence within 6 months. Reoperation was considered possibly relevant to early recurrence. Pathological outcomes are shown in Table 3. Presence of poorly differentiated SCC component, advanced T stage (T3, T4), three or more lymph node metastases, and presence of vessel invasion were significantly associated with early recurrence. Lymphatic invasion was also considered possibly relevant to early recurrence. Pathological response grade did not correlate with early recurrence (data not shown). The logistic regression analysis suggested that CRP before NAC at ≥0.5 mg/dl [hazard ratio (HR) 33.8, 95 % confidence interval (CI) 2.767–413.9; p = 0.006], presence of poorly differentiated SCC component (HR 138, 95 % CI 5.339–3576; p = 0.003), and presence of pathological vessel invasion (HR 16.3, 95 % CI 1.960–136.1; p = 0.010) have the possibility of becoming independent risk factors of early recurrence (Table 4). As for these potential risk factors, 28 % of patients with one factor recurred within 6 months after esophagectomy. On the other hand, patients with at least two factors frequently recurred, with an incidence of 82 % (9/11).
Table 5 shows the pattern of early recurrence. Thirteen patients (93 %) had a distant metastasis; only 1 patient had a local recurrence.
Discussion
We retrospectively analyzed the clinicopathological factors of patients with resectable advanced esophageal cancer who had an early recurrence within 6 months after esophagectomy following NAC. In this study, 17 % of patients recurred during this early period. This rate is slightly higher than that seen in the JCOG 9907 study [6], which might be caused by the differences in cancer stage and NAC regimen. This study included cases of more advanced esophageal cancer, which consisted of 53 % of clinical stage III and 10 % of stage IVA, whereas the patients in the JCOG 9907 study consisted of 50 % in clinical stage III and none in stage IVA (6th UICC). Moreover, although several studies reported that the response rate of NAC with DCF is higher than that of NAC with FP, the long-term outcome is still unclear [21].
As for the difference in chemotherapy regimen, the incidence of early recurrence was same between DCF and FP. Relapse-free survival (RFS) was also same (data not shown). Nomura et al. reported the same results on RFS after NAC with DCF and FP [9]. Unfortunately, this study did not contain a sufficient number of patients to clarify the definitive difference between DCF and FP.
The current analyses contained multiple variables of different time phases. It is unclear which timing is best to predict those patients who would recur such an early period, before initial treatment or after NAC just before surgery or after surgery. We believe that we should select those patients after surgery for two reasons. One reason is that pathological findings are certainly integral for prediction of prognosis. The other reason is that at least, as of now, patients with resectable advanced esophageal cancer should be treated with the best strategy currently performed (NAC and subsequent surgery). Therefore, we conducted multivariate analysis with multiple variables of different phases that could be obtained after surgery.
In this study, CRP before NAC ≥0.5 mg/dl, presence of poorly differentiated SCC component, and pathological vessel invasion were associated with early recurrence. To date, several retrospective studies have been conducted to confirm risk factors of early death within 1 year after surgery for esophageal cancer. Kosugi et al. reported that the presence of intramural metastasis was the only risk factor of early death after extended radical esophagectomy [11]. Zhu et al. and Davies et al. reported that grade of differentiation and number of lymph node metastases were valuable prognostic factors predicting early death [12, 13]. Zhu et al. also suggested that depth of invasion, lymph node metastasis, and marginal status of specimen resected become prognostic factors. However, these studies included patients without NAC, total or partial. There was only one study of early cancer-related mortality after neoadjuvant therapy [10]. In this article, Stiles et al. suggested that performance status, poor tumor differentiation, and clinical response of NAC were independent risk factors of early mortality within 1 year. Additionally, they also reported that 29 % of patients with at least two of these risk factors would die within 1 year after surgery. However this study also contained 31 % of neoadjuvant CRT. To date, studies of early recurrence for patients who underwent surgery following only NAC were not available.
In this study, pathological factors associated with early recurrence were consistent with those in previous studies. Common in most studies, poorly differentiated SCC was a strong risk factor for poor prognosis. Several key enzymes, such as fatty acid synthase and pyruvate kinase M2, were reported to correlate with the differentiation of esophageal SCC, and these were also associated with the prognosis of esophageal cancer [22, 23]. It is already confirmed that vessel invasion of esophageal SCC correlated with poor prognosis because of the high incidence of metastasis [24, 25]. Elevated CRP is established as a risk factor of poor prognosis of advanced or inoperable esophageal SCC [26–28]. The Glasgow Prognostic Score (GPS) or novel inflammation-based prognostic score, which includes CRP level as a parameter, could also predict the prognosis of esophageal SCC [29–31]. In this study, because albumin <3.5 g/dl before NAC was close to being the independent risk factor of early recurrence with a probability level of 0.084, we also examined the usefulness of GPS and modified GPS as the indicator for early recurrence. Consequently, both scores could also be the predictive indicator (data not shown) in this cohort. Production of CRP is induced by interleukin (IL)-6, IL-1, tumor necrosis factor-α, and transforming growth factor-β [32]. These cytokines could induce tumor progression or invasion and are correlated with poor prognosis in esophageal cancer [33–36]. Moreover, cancer cells could also produce CRP by themselves; positive findings of tumoral CRP expression in immunohistochemistry are reported to be associated with a poor outcome in esophageal SCC [37].
Among these three risk factors in this study, patients with at least two factors frequently recurred, with an incidence of 82 %. Such patients should certainly be considered for additional treatment and should be followed up carefully. Regarding additional treatment, systemic chemotherapy might be appropriate, as most of the recurrences were distant metastases (Table 5) as in a previous report [38]. However, an optimal treatment regimen for such patients was not established. We believe that both the development of novel agents and advance in treatment strategy are necessary for patients at high risk of early recurrence. In addition, a reliable method to predict such patients before treatment should be established to avoid unprofitable treatment, especially highly invasive esophagectomy.
This study has certain limitations. This is a retrospective study that was conducted at a single institute. Moreover, the sample size was not sufficiently large. Therefore, the present results remain undefined. We believe that a multicenter study with a larger cohort is desirable to establish definitive risk factors of early recurrence after surgery following NAC for resectable advanced esophageal cancer.
In conclusion, for resectable advanced esophageal cancer, CRP before NAC ≥0.5 mg/dl, presence of poorly differentiated SCC component, and pathological vessel invasion might be correlated with early recurrence within 6 months after esophagectomy following NAC. Particularly, for patients with at least two factors, additional treatment and cautious follow-up might be necessary after surgery.
References
Zacherl J (2014) The current evidence in support of multimodal treatment of locally advanced, potentially resectable esophageal cancer. Dig Dis 32:171–175
van Hagen P, Hulshof MC, van Lanschot JJ et al (2012) Preoperative chemoradiotherapy for esophageal or junctional cancer. N Engl J Med 366:2074–2084
Allum WH, Stenning SP, Bancewicz J et al (2009) Long-term results of a randomized trial of surgery with or without preoperative chemotherapy in esophageal cancer. J Clin Oncol 27:5062–5067
Ando N, Iizuka T, Ide H et al (2003) Surgery plus chemotherapy compared with surgery alone for localized squamous cell carcinoma of the thoracic esophagus: a Japan Clinical Oncology Group Study–JCOG9204. J Clin Oncol 21:4592–4596
Boonstra JJ, Kok TC, Wijnhoven BP et al (2011) Chemotherapy followed by surgery versus surgery alone in patients with resectable oesophageal squamous cell carcinoma: long-term results of a randomized controlled trial. BMC Cancer 19(11):181
Ando N, Kato H, Igaki H et al (2012) A randomized trial comparing postoperative adjuvant chemotherapy with cisplatin and 5-fluorouracil versus preoperative chemotherapy for localized advanced squamous cell carcinoma of the thoracic esophagus (JCOG9907). Ann Surg Oncol 19:68–74
Kelsen DP, Winter KA, Gunderson LL et al (2007) Long-term results of RTOG trial 8911 (USA Intergroup 113): a random assignment trial comparison of chemotherapy followed by surgery compared with surgery alone for esophageal cancer. J Clin Oncol 25:3719–3725
Allum WH, Stenning SP, Bancewicz J et al (2009) Long-term results of a randomized trial of surgery with or without preoperative chemotherapy in esophageal cancer. J Clin Oncol 27:5062–5067
Nomura M, Oze I, Abe T et al (2015) Impact of docetaxel in addition to cisplatin and fluorouracil as neoadjuvant treatment for resectable stage III or T3 esophageal cancer: a propensity score-matched analysis. Cancer Chemother Pharmacol 76:357–363
Stiles BM, Salzler GG, Nasar A et al (2015) Clinical predictors of early cancer-related mortality following neoadjuvant therapy and oesophagectomy. Eur J Cardiothorac Surg 48:455–460
Kosugi S, Kanda T, Yajima K et al (2011) Risk factors that influence early death due to cancer recurrence after extended radical esophagectomy with three-field lymph node dissection. Ann Surg Oncol 18:2961–2967
Zhu ZJ, Hu Y, Zhao YF et al (2011) Early recurrence and death after esophagectomy in patients with esophageal squamous cell carcinoma. Ann Thorac Surg 91:1502–1508
Davies AR, Pillai A, Sinha P et al (2014) Factors associated with early recurrence and death after esophagectomy for cancer. J Surg Oncol 109:459–464
Edge SB, Byrd DR, Compton CC et al (2009) AJCC Cancer Staging Manual, 7th edn. Springer, New York
Watanabe M, Nagai Y, Kinoshita K et al (2011) Induction chemotherapy with docetaxel/cisplatin/5-fluorouracil for patients with node-positive esophageal cancer. Digestion 83:146–152
Society of Thoracic Surgeons (2013) Risk-Adjusted Morbidity and Mortality for Esophagectomy for Cancer. Available: http://www.sts.org/quality-research-patient-safety/quality/quality-performance-measures [accessed Feb 28, 2016]
National Cancer Institute (2010) Common Terminology Criteria for Adverse Events (CTCAE). United States Department of Health and Human Services. Available: http://evs.nci.nih.gov/ftp1/CTCAE/CTCAE_4.03_2010-06-14_QuickReference_5x7.pdf#search=‘http%3A%2F%2Fevs.nci.nih.gov%2Fftp1%2FCTCAE%2F+CTCAE_4.03_20100614_QuickReference_57.pdf [accessed Feb. 28, 2016]
Dindo D, Demartines N, Clavien PA (2004) Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg 240:205–213
Murata N, Soga Y, Iida O et al (2015) Complex relationship of body mass index with mortality in patients with critical limb ischemia undergoing endovascular treatment. Eur J Vasc Endovasc Surg 49:297–305
Eisenhauer EA, Therasse P, Bogaerts J et al (2009) New response evaluation criteria in solid tumours: revised RECIST guideline (version 1.1). Eur J Cancer 45:228–247
Watanabe M, Baba Y, Yoshida N et al (2014) Outcomes of preoperative chemotherapy with docetaxel, cisplatin, and 5-fluorouracil followed by esophagectomy in patients with resectable node-positive esophageal cancer. Ann Surg Oncol 21:2838–2844
Wu D, Xu J, Yu G et al (2013) Expression status of fatty acid synthase (FAS) but not HER2 is correlated with the differentiation grade and prognosis of esophageal carcinoma. Hepatogastroenterology 60:99–106
Zhan C, Shi Y, Lu C, Wang Q (2013) Pyruvate kinase M2 is highly correlated with the differentiation and the prognosis of esophageal squamous cell cancer. Dis Esophagus 26:746–753
Imamura Y, Watanabe M, Nagai Y et al (2012) Lymphatic vessel invasion detected by the D2-40 monoclonal antibody is an independent prognostic factor in node-negative esophageal squamous cell carcinoma. J Surg Oncol 105:277–283
Bai B, Ma W, Wang K et al (2013) Detection of D2-40 monoclonal antibody-labeled lymphatic vessel invasion in esophageal squamous cell carcinoma and its clinicopathologic significance. Cancer Biol Med 10:81–85
Fujiwara H, Suchi K, Okamura S et al (2011) Elevated serum CRP levels after induction chemoradiotherapy reflect poor treatment response in association with IL-6 in serum and local tumor site in patients with advanced esophageal cancer. J Surg Oncol 103:62–68
Lindenmann J, Fink-Neuboeck N, Koesslbacher M et al (2014) The influence of elevated levels of C-reactive protein and hypoalbuminemia on survival in patients with advanced inoperable esophageal cancer undergoing palliative treatment. J Surg Oncol 110:645–650
Wang CY, Hsieh MJ, Chiu YC et al (2009) Higher serum C-reactive protein concentration and hypoalbuminemia are poor prognostic indicators in patients with esophageal cancer undergoing radiotherapy. Radiother Oncol 92:270–275
Ohira M, Kubo N, Masuda G et al (2015) Glasgow Prognostic Score as a prognostic clinical marker in T4 esophageal squamous cell carcinoma. Anticancer Res 35:4897–4901
Xu XL, Yu HQ, Hu W et al (2015) A novel inflammation-based prognostic score, the C-reactive protein/albumin ratio predicts the prognosis of patients with operable esophageal squamous cell carcinoma. PLoS One 10:e0138657
Hirahara N, Matsubara T, Hayashi H et al (2015) Impact of inflammation-based prognostic score on survival after curative thoracoscopic esophagectomy for esophageal cancer. Eur J Surg Oncol 41:1308–1315
Groblewska M, Mroczko B, Sosnowska D et al (2012) Interleukin 6 and C-reactive protein in esophageal cancer. Clin Chim Acta 413:1583–1590
Chen MF, Kuan FC, Yen TC et al (2014) IL-6-stimulated CD11b + CD14 + HLA-DR-myeloid-derived suppressor cells are associated with progression and poor prognosis in squamous cell carcinoma of the esophagus. Oncotarget 5:8716–8728
Le Bras GF, Taylor C, Koumangoye RB et al (2015) TGFβ loss activates ADAMTS-1-mediated EGF-dependent invasion in a model of esophageal cell invasion. Exp Cell Res 330:29–42
Chen MF, Lu MS, Chen PT et al (2012) Role of interleukin 1 beta in esophageal squamous cell carcinoma. J Mol Med 90:89–100
Szlosarek P, Charles KA, Balkwill FR (2006) Tumour necrosis factor-alpha as a tumour promoter. Eur J Cancer 42:745–750
Nakatsu T, Motoyama S, Maruyama K et al (2012) Tumoral CRP expression in thoracic esophageal squamous cell cancers is associated with poor outcomes. Surg Today 42:652–658
Sudarshan M, Alcindor T, Ades S et al (2015) Survival and recurrence patterns after neoadjuvant docetaxel, cisplatin, and 5-fluorouracil (DCF) for locally advanced esophagogastric adenocarcinoma. Ann Surg Oncol 22:324–330
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Naoya Yoshida and coauthors have no conflict of interest in relation to this article.
About this article
Cite this article
Yoshida, N., Baba, Y., Shigaki, H. et al. Risk factors of early recurrence within 6 months after esophagectomy following neoadjuvant chemotherapy for resectable advanced esophageal squamous cell carcinoma. Int J Clin Oncol 21, 1071–1078 (2016). https://doi.org/10.1007/s10147-016-0994-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10147-016-0994-9