Abstract
Background
This retrospective single-center study assessed the feasibility, outcomes, and side-effects of high-dose methotrexate (HD-MTX) plus procarbazine in the treatment of immunocompetent patients with primary central nervous system lymphoma (PCNSL).
Methods
Ninety-one patients diagnosed with PCNSL between January 2001 and December 2011 were treated with HD-MTX plus procarbazine. To reduce neurotoxicity in patients aged ≥60 years, only those not responding to chemotherapy and patients with relapse underwent whole-brain irradiation.
Results
All 91 consecutive patients were scheduled to receive HD-MTX. Their median age was 66 years (range 32–88 years) and their median Karnofsky performance score was 40 (range 20–100). While 56 patients (61.5 %) completed 3 cycles of HD-MTX chemotherapy and 48 (52.7 %) showed a complete response, treatment was stopped in 11 patients (12.1 %) due to toxicity. The median overall survival and progression-free survival were 40.6 and 11.7 months, respectively. Overall survival was significantly improved in patients who completed 3 cycles of chemotherapy compared with those did not (56.4 vs 24.0 months; p = 0.013 by univariate and p = 0.022 by multivariate analysis).
Conclusions
Initial treatment with HD-MTX plus procarbazine was effective in patients with PCNSL. Completion of 3 cycles of HD-MTX chemotherapy was a significant independent prognostic factor for patient survival.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Primary central nervous system lymphoma (PCNSL) is highly aggressive, and accounts for 3–4 % of all intracranial malignancies [1]. While the standard treatment, whole-brain radiotherapy (WBRT) alone, has been demonstrated to produce a complete response in up to 70 % of patients, their median survival is only 12–18 months and the 5-year survival rate is <5 % [2, 3]. The addition of high-dose methotrexate (HD-MTX)-based chemotherapy has been shown to substantially improve median survival in these patients [3–5]. However, long-term evaluation of patients treated with combined chemoradiotherapy has revealed a substantial risk of developing leukoencephalopathy with dementia, ataxia, gait disturbance, and incontinence [6]. The main risk factors for leukoencephalopathy are radiotherapy (RT), age ≥60 years, intrathecal therapy, and chemotherapy after WBRT [6–9].
Fliessbach et al. [10] reported that the preservation of neurocognitive function and quality of life were better in patients treated with chemotherapy alone than in those subjected to combined treatment. Illerhaus et al. [11] found that in patients aged >65 years, using an MCP regimen consisting of HD-MTX plus the oral alkylating agents lomustine and procarbazine, omitting intrathecal chemotherapy, and restricting WBRT to patients not responding to chemotherapy, was feasible, effective, and resulted in a low rate of leukoencephalopathy.
Here, we present our experience in treating PCNSL with HD-MTX plus procarbazine and deferring RT in patients aged ≥60 years.
Materials and methods
Our study included 91 newly diagnosed immunocompetent PCNSL patients. PCNSL was histologically confirmed by biopsy or resection. To diagnose B-cell lymphoma, we performed immunohistochemical analysis for cluster of differentiation (CD) 20 expression. After routine deparaffinization, rehydration, and blocking of endogenous peroxidase activity we performed microwave-enhanced antigen retrieval. Slide-mounted sections immersed in 0.01 M sodium citrate buffer (pH 6.0) were placed for 3 and 15 min in 700-W and 200-W microwave ovens, respectively, at maximum power. CD20 immunostaining was performed using an anti-CD20 antibody (1:100; internal clone L26, DAKO, Carpinteria, CA, USA). For T-cell lymphoma, immunostaining with an anti-CD45RO antibody (1:100; internal clone UCHL1, DAKO) was performed.
To exclude patients with systemic lymphoma, positron emission tomography (PET) or whole-body computed tomography studies that included the chest, abdomen, and pelvis were performed for all patients. Other enrollment criteria included age >20 years, negative human immunodeficiency virus serology, Karnofsky performance status (KPS) ≥20, adequate bone marrow (absolute neutrophil count ≥1,500/mm3, hemoglobin ≥8.0 g/dL, platelets ≥100,000/mm3), and renal (creatinine clearance ≥60 mL/min), heart (ejection fraction ≥50 %), and hepatic function (aspartate aminotransferase/alanine aminotransferase ≤2 times upper limit of normal).
Between January 2001 and December 2011, we enrolled 91 patients in our study. All patients provided written informed consent prior to receiving the treatment protocol.
Induction therapy consisted of a cycle of high-dose MTX (3.5 g/m2) delivered intravenously over 3 h on days 1, 22, and 43. Leucovorine rescue (15 mg) was initiated 24 h after the start of MTX infusion, and administered 9 times every 3 h, followed by 5 times every 6 h, and was continued until MTX clearance (<0.1 µM). Procarbazine (60 mg/m2) was administered orally on days 1–7, 22–28, and 43–49. The initial betamethasone treatment dose was tapered from 16 to 2 mg every 4 days.
We administered RT after induction chemotherapy in all patients aged <60 years. Patients with complete remission (CR) underwent whole-brain RT (30 Gy in 15 daily fractions). The schedule for patients manifesting a partial response (PR) or progressive disease (PD) during or after induction chemotherapy was 40 Gy in 20 fractions to the whole brain plus a 14 Gy boost by the three-dimensional conformal technique. In the boost treatment, delineation of the planning target volume was performed by adding a 2-cm margin to the gross tumor volume, which consisted of the residual tumors. The boost dose was 14 Gy in seven fractions at the isocenter (Fig. 1).
Baseline magnetic resonance imaging (MRI) was performed in all patients before induction chemotherapy. The results were assessed before the second and third cycle of chemotherapy, at the end of treatment, and during the follow-up period. We evaluated all patients every 3 months for the first 2 years and every 6 months thereafter. Changes in tumor size were assessed on gadolinium-enhanced MR images of the brain. Remission on enhanced MR images was defined according to International PCNSL Collaborative Group criteria [12]. CR was defined as the disappearance of all contrast enhancement on MR images in the absence of corticosteroids, PR was defined as a ≥50 % reduction in tumor size compared with that seen on baseline MR images, and PD as a ≥25 % increase in tumor size or the appearance of any new lesion. All other findings were recorded as stable disease (SD). Toxicity was graded according to the common toxicity criteria (CTC) version 3.0.
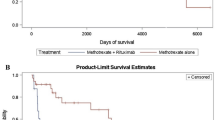
The primary end-points of this study were overall survival (OS) and progression-free survival (PFS). OS was defined as the time from initial diagnosis to death from any cause, and PFS as the time from diagnosis to disease progression or death due to any cause. Patients who did not experience the event of interest with respect to OS or PFS during the study period were considered censored observations, with the time from the first diagnosis to the last follow-up visit as the censoring time. For patients in CR, the response duration was defined as the time from the first observation of a response to the time progression was first observed or death. In patients without progression and in survivors, it was censored at the time of the last follow-up examination. The Kaplan–Meier method was used to estimate survival and response duration probabilities and their 95 % confidence intervals (CIs) using GraphPad Prism software (GraphPad Software, Inc. San Diego, USA). The Mantel–Cox log-rank test was applied to assess the strength of association between OS and PFS. The analyzed variables included patient age and sex, the KPS at the time of admission, tumor location, and completion of 3 cycles of HD-MTX treatment. In addition, the Memorial Sloan-Kettering Cancer Center (MSKCC) prognosis score, based on age and KPS, was validated. Statistical analysis was performed using Stat Mate III software (version III for Macintosh; ATOMS, Tokyo, Japan), and p values <0.05 were considered statistically significant.
Results
Patient characteristics
As shown in Table 1, 51 out of the 91 patients were male (56.0 %), the median age was 66 years (range 32–88 years), and the median KPS was 40 (range 20–100). The diagnosis of PCNSL was based on tumor biopsy (n = 88) and resection (n = 2), and the pathological diagnoses were diffuse large B-cell and T-cell lymphoma in 87 and 3 patients, respectively. All patients with T-cell lymphoma showed negative human T-cell lymphotropic virus type 1 serology. One patient was diagnosed based on MRI and PET findings.
Treatment
First cycle
Of the 91 patients, 79 completed the first cycle of treatment and proceeded to the second cycle. The remaining 12 patients did not proceed due the development of adverse events, including nonketotic hyperosmolar coma (n = 1), hematopoietic insufficiency grade 4 or 2 (n = 1 each), prolonged MTX clearance followed by pneumonia (n = 1), and renal failure (n = 1), or due to disease progression (n = 7).
Second cycle
Among the 79 patients proceeding to the second cycle, 56 completed the cycle and proceeded to the third cycle. The other 23 did not proceed due to acute heart failure (n = 1), pneumonia (n = 3), prolonged MTX clearance followed by renal failure grade 4 (n = 1), hematopoietic insufficiency grade 3 (n = 1), and disease progression (n = 17).
Treatment response and survival
The treatment response was evaluated on contrast-enhanced MR images acquired within 3 weeks of MTX treatment. Progression was observed in 7 and 17 patients after the first and second cycles, respectively. In 48 of the 91 patients (52.7 %) CR was noted after the third cycle (Fig. 2).
The median OS and PFS were 40.6 months (95 % CI, 28.9–51.3 months) and 11.7 months (95 % CI, 1.0–21.5 months), respectively (Figs. 3, 4). Among the 48 patients classified as CR, disease progression was later observed in 36 patients. The median time to progression was 12.6 months (range 0.4–88.2 months). In patients aged ≥60 years, the median OS and PFS were 31.3 and 6.8 months, respectively (Table 2), whereas in patients aged <60 years, the corresponding times were 78.7 and 22.6 months, respectively. Although there were no significant differences between the two groups (p = 0.061 and p = 0.081 for OS and PFS, respectively), a trend was observed, with patients aged <60 years having a more favorable survival outcome. Moreover, patients who completed three cycles experienced significantly longer OS (56.4 vs 24.0 months; p = 0.013 by univariate and p = 0.022 by multivariate analysis; Tables 2 and 3).
Since patient age and performance status are the two variables that have been consistently identified as independent prognostic factors, we analyzed our data based on the MSKCC classification (class 1, age <50 years; class 2, age ≥50, KPS ≥70; class 3, age ≥50, KPS <70). The median OS was 51.1, 59.9, and 31.8 months for patients classified as class 1 (n = 15), 2 (n = 16), and 3 (n = 60), respectively. The median PFS was 24.0, 15.9, and 5.5 months, respectively. No significant differences were detected among the groups with respect to OS (p = 0.26) and PFS (p = 0.35).
Long-term survivors (>90 months)
At the last follow-up visit, 6 patients (5 male and 1 female) had survived for >90 months. Their median age at the time of diagnosis was 65.5 years (range 41–83 years) and their median KPS at the time of admission was 55 (range 20–100). Of these, 5 patients had completed three cycles of HD-MTX treatment and 2 had undergone whole-brain irradiation as part of their initial treatment. In one patient, we had to stop treatment after the first cycle because of toxicity. Accordingly, he did not receive additional treatment, but was instead regularly followed up.
Five of these patients experienced disease recurrence at a median time of 72.5 months (range 19.4–90.5) after the initial diagnosis. Among them, one patient experienced systemic disease recurrence at 62.5 months but prolonged survival (106.4 months) after salvage high-dose chemotherapy with autologous peripheral blood stem cell transplantation. An 83-year-old female manifested local recurrence at 19.4 months, but was treated with temozolomide and survived for 94.9 months without mental deterioration. Three patients died of disease progression. Only one patient survived without recurrence after the initial HD-MTX treatment plus WBRT (102 months). He worked normally and his KPS was 100 without mental deterioration.
Acute toxicity
Treatment-related toxicity was observed in 60 (65.9 %) patients. CTC grades I/II, III, and IV toxicities occurred in 34 (37.4 %), 15 (16.5 %), and 10 (11.0 %) patients, respectively. One (1.1 %) patient with T-cell lymphoma died of hemophagocytic syndrome after the first cycle of HD-MTX treatment. Gastrointestinal disturbances, including mucositis, were observed in 11 patients (12.1 %). Of these, 2 manifested grade III toxicities and 9 experienced hyperglycemia (grade III/IV, n = 5). Others developed hematologic complications (n = 8; grade III/IV, n = 5), pneumonia (n = 7; grade III/IV, n = 5), liver dysfunction (n = 6; grade III, n = 1), and renal dysfunction (n = 2; grade IV, n = 2). In 11 patients, HD-MTX treatment was discontinued due to toxicity.
Late toxicity
At the most recent follow-up examination, 38 patients (41.8 %) were alive. Updated clinical data were not available from 13 patients, resulting in 25 patients being included in the final survival analysis. In these 25 patients (13 male and 12 female; median age 64 years; range 41–83 years), the median follow-up duration was 51.8 months (range 2.8–106.4 months), median initial KPS was 40 (range 20–90), and median KPS at the last follow-up examination was 50 (range 30–100). We did not assess neurotoxicity by serial neurocognitive function tests. Radiological signs of neurotoxicity such as brain atrophy and/or diffuse hyperintensity lesions on fluid-attenuated inversion recovery images were detected on the most recent MRI studies in 11 of these patients, with 9 patients manifesting neurocognitive dysfunction [median KPS 40 (range 30–50)]. Of these 9 patients, 7 received WBRT initially or during the course of the disease.
Discussion
We report a consecutive series of PCNSL patients who were treated uniformly based on our response-based strategy of reduced or deferred irradiation in patients with CR after induction with MTX-based chemotherapy.
The patient’s age and PS strongly affect therapeutic decisions in PCNSL and have been suggested as prognostic factors. According to Abrey et al. [13], who proposed the MSKCC prognostic model, patients aged <50 years have a better prognosis with respect to both OS and PFS. Therefore, we analyzed our data using the MSKCC score but could not find any significant differences between the patient groups. The median OS in our class 3 patients (age ≥50 years, KPS <70) was 31.8 months, which is better than the previously reported OS for class 3 patients (1.1 year and 5.2 months [13, 14]).
Analysis of the survival data in our class 3 patients showed that 12 out of 60 patients survived for >60 months, a finding that may have contributed to the favorable survival outcomes of this group.
It has been reported that the initial treatment response affects the prognosis. Kiewe et al. [14] showed in their study that the response to first-line MTX-based treatments as well as a younger age were associated with improved survival, with the median OS for patients responding to first-line treatment (45 months) being significantly better than for patients with no response (18 months; p = 0.04). In our series of 91 patients, 56 (61.5 %) completed 3 cycles of HD-MTX chemotherapy, and 48 (52.7 %) obtained CR. The median OS in patients who completed chemotherapy was better than in those who did not (56.4 vs 24.0 months; p = 0.013). Moreover, six patients survived for >90 months, including 5 who completed 3 cycles of chemotherapy (chemotherapy only, n = 4; chemotherapy followed by WBRT, n = 2). The observation that these 5 patients experienced disease recurrence after a median of 72.5 months suggests that the response to first-line chemotherapy has a prognostic impact.
Phase II studies conducted during the last decade have shown that the addition of HD-MTX-based chemotherapy to RT improves survival compared with RT alone. However, these combined treatments expose long-term survivors, especially elderly patients, to severe delayed neurotoxicities [7]. Accordingly, it has been suggested that chemoradiotherapy is associated with significant cognitive impairment and that radiographic abnormalities such as white matter changes or cortical atrophy, are correlated with cognitive functions [10, 15].
Treatment trials using chemotherapy alone have been conducted to avoid severe long-term neurotoxicity [11, 16, 17]. The reported CR rates after HD-MTX monotherapy are 30–65 %, and the reported median PFS is 13–17 months [17–19]. In our study, the CR rate after 3 cycles of HD-MTX was 52.7 % and the median PFS was 11.7 months. Other studies [4, 20] have reported CR in 82–88 % of patients treated with HD-MTX followed by WBRT and a median PFS of 32–40 months. However, it remains unclear whether the relatively short PFS is related to deferred RT or the use of single-agent regimens rather than a combination of drugs. In our opinion, the advisability of RT as a systematic consolidation treatment in patients with CR after chemotherapy is debatable. Reni and Ferreri [21] suggested that WBRT consolidation against microscopic residual disease is preferable to RT delivered at the time of relapse in patients with more bulky disease. Although this is a basic principle of oncology, the prognosis remains poor in patients with PCNSL and treatment must attempt to preserve good quality of life during the disease-free stage in patients with CR.
Furthermore, others [22, 23] have reported that WBRT is effective as salvage therapy in PCNSL patients who failed to respond to initial HD-MTX treatment. The reported response rates to salvage WBRT are 74–79 %, with a reported median survival of 10.9–16 months. These observations suggest that it might be reasonable to defer WBRT, as it retains its efficacy as salvage treatment.
Due to the availability of effective salvage therapy, the high rate of initial treatment failure did not translate into inferior survival in this study. We have previously reported the effectiveness of temozolomide in refractory or relapsed PCNSL [24]. In this previous study, although some patients were elderly and were heavily pre-treated, temozolomide treatment resulted in a CR in 29 % and PR in 18 % of patients, and was found to be well tolerated without eliciting any major toxicity.
In conclusion, we found that HD-MTX chemotherapy with procarbazine was effective in patients with PCNSL, especially in those who completed 3 cycles of initial treatment. The relatively short PFS and lower CR observed in our study compared with those in other studies might reflect our use of mild therapy regimens as the first-line treatment and the deferral of RT. To improve treatment outcomes, multi-agent regimens using non-cross-resistant drugs should be considered to treat patients with aggressive systemic non-Hodgkin’s lymphoma.
References
Nakamura H, Makino K, Yano S et al (2011) Epidemiological study of primary intracranial tumors: a regional survey in Kumamoto prefecture in southern Japan––20-year study. Int J Clin Oncol 16:314–321
Nelson DF, Martz KL, Bonner H et al (1992) Non-Hodgkin’s lymphoma of the brain: can high dose, large volume radiation therapy improve survival? Report on a prospective trial by the Radiation Therapy Oncology Group (RTOG): RTOG 8315. Int J Radiat Oncol Biol Phys 23:9–17
DeAngelis LM, Seiferheld W, Schold SC et al (2002) Combination chemotherapy and radiotherapy for primary central nervous system lymphoma: radiation Therapy Oncology Group Study 93-10. J Clin Oncol 20:4643–4648
O’Brien P, Roos D, Pratt G et al (2000) Phase II multicenter study of brief single-agent methotrexate followed by irradiation in primary CNS lymphoma. J Clin Oncol 18:519–526
Hiraga S, Arita N, Ohnishi T et al (1999) Rapid infusion of high-dose methotrexate resulting in enhanced penetration into cerebrospinal fluid and intensified tumor response in primary central nervous system lymphomas. J Neurosurg 91:221–230
Filley CM, Kleinschmidt-DeMasters BK (2001) Toxic leukoencephalopathy. N Engl J Med 345:425–432
Abrey LE, DeAngelis LM, Yahalom J (1998) Long-term survival in primary CNS lymphoma. J Clin Oncol 16:859–863
Correa DD, DeAngelis LM, Shi W et al (2004) Cognitive functions in survivors of primary central nervous system lymphoma. Neurology 62:548–555
Omuro AM, Ben-Porat LS, Panageas KS et al (2005) Delayed neurotoxicity in primary central nervous system lymphoma. Arch Neurol 62:1595–1600
Fliessbach K, Helmstaedter C, Urbach H et al (2005) Neuropsychological outcome after chemotherapy for primary CNS lymphoma: a prospective study. Neurology 64:1184–1188
Illerhaus G, Marks R, Muller F et al (2009) High-dose methotrexate combined with procarbazine and CCNU for primary CNS lymphoma in the elderly: results of a prospective pilot and phase II study. Ann Oncol 20:319–325
Abrey LE, Batchelor TT, Ferreri AJ et al (2005) Report of an international workshop to standardize baseline evaluation and response criteria for primary CNS lymphoma. J Clin Oncol 23:5034–5043
Abrey LE, Ben-Porat L, Panageas KS et al (2006) Primary central nervous system lymphoma: the Memorial Sloan-Kettering Cancer Center prognostic model. J Clin Oncol 24:5711–5715
Kiewe P, Fischer L, Martus P et al (2008) Primary central nervous system lymphoma: monocenter, long-term, intent-to-treat analysis. Cancer 112:1812–1820
Neuwelt EA, Guastadisegni PE, Varallyay P et al (2005) Imaging changes and cognitive outcome in primary CNS lymphoma after enhanced chemotherapy delivery. Am J Neuroradiol 26:258–265
Hoang-Xuan K, Taillandier L, Chinot O et al (2003) Chemotherapy alone as initial treatment for primary CNS lymphoma in patients older than 60 years: a multicenter phase II study (26952) of the European Organization for Research and Treatment of Cancer Brain Tumor Group. J Clin Oncol 21:2726–2731
Batchelor T, Carson K, O’Neill A et al (2003) Treatment of primary CNS lymphoma with methotrexate and deferred radiotherapy: a report of NABTT 96-07. J Clin Oncol 21:1044–1049
Guha-Thakurta N, Damek D, Pollack C et al (1999) Intravenous methotrexate as initial treatment for primary central nervous system lymphoma: response to therapy and quality of life of patients. J Neurooncol 43:259–268
Herrlinger U, Schabet M, Brugger W et al (2002) German Cancer Society Neuro-Oncology Working Group NOA-03 multicenter trial of single-agent high-dose methotrexate for primary central nervous system lymphoma. Ann Neurol 51:247–252
Glass J, Gruber ML, Cher L et al (1994) Preirradiation methotrexate chemotherapy of primary central nervous system lymphoma: long-term outcome. J Neurosurg 81:188–195
Reni M, Ferreri AJ (2004) Is withdrawal of consolidation radiotherapy an evidence-based strategy in primary central nervous system lymphomas? J Clin Oncol 22:1165–1167 (author reply 1167–1168)
Hottinger AF, DeAngelis LM, Yahalom J et al (2007) Salvage whole brain radiotherapy for recurrent or refractory primary CNS lymphoma. Neurology 69:1178–1182
Nguyen PL, Chakravarti A, Finkelstein DM et al (2005) Results of whole-brain radiation as salvage of methotrexate failure for immunocompetent patients with primary CNS lymphoma. J Clin Oncol 23:1507–1513
Makino K, Nakamura H, Hide T et al (2012) Salvage treatment with temozolomide in refractory or relapsed primary central nervous system lymphoma and assessment of the MGMT status. J Neurooncol 106:155–160
Conflict of interest
The authors declare that they have no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
About this article
Cite this article
Makino, K., Nakamura, H., Hide, Ti. et al. Prognostic impact of completion of initial high-dose methotrexate therapy on primary central nervous system lymphoma: a single institution experience. Int J Clin Oncol 20, 29–34 (2015). https://doi.org/10.1007/s10147-014-0692-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10147-014-0692-4