Abstract
Background
We aimed to evaluate the association of preoperative plasma fibrinogen levels with the clinicopathological parameters, disease-free survival, and overall survival in patients with renal cell carcinoma.
Methods
We retrospectively studied 286 patients with renal cell carcinoma who underwent radical nephrectomy from 2000 to 2003 at one center. The plasma fibrinogen was routinely determined before operation in all patients. The correlation of preoperative plasma fibrinogen levels with clinicopathological findings was evaluated by t-test or analysis of variance (ANOVA) methods. As well, univariate and multivariate analyses were used to determine the association between the preoperative level of plasma fibrinogen and survival duration.
Results
An elevated level of plasma fibrinogen was positively related to the Fuhrman grade (P < 0.001), tumor size (P < 0.001), and T stage (P < 0.001), but it was negatively related to histologic type (P = 0.266). Univariate analysis showed that the Fuhrman grade, tumor size, T stage, hemoglobin, corrected calcium, lactate dehydrogenase, and plasma fibrinogen level were significantly correlated with disease-free survival (P < 0.001, P < 0.001, P < 0.001, P < 0.001, P = 0.001, P < 0.001, and P < 0.001, respectively) and overall survival (P < 0.001, P = 0.001, P < 0.001, P < 0.001, P = 0.002, P = 0.001, and P < 0.001). Multivariate analysis showed that the plasma fibrinogen level remained as an independent prognostic factor for disease-free survival (P = 0.021) and overall survival (P < 0.001).
Conclusions
A high preoperative plasma fibrinogen level is an independent predictor of distant metastasis and survival prognosis after radical nephrectomy in patients with renal cell carcinoma.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Renal cell carcinoma (RCC) is the most common cancer of the kidney. Despite improvements in medical imaging for early diagnosis, over 40 % of patients with kidney cancer remain incurable. To identify the patients with a high risk of metastasis would be helpful for active surveillance or adjuvant therapy after primary surgery. Related clinical parameters such as the tumor-node-metastasis (TNM) stage, pathologic Fuhrman’s grade, and performance status have been well established to predict the patient’s outcome. However, we have been working on finding available biomarkers from body fluid to make the prognostic prediction of RCC more accurate.
It has been well demonstrated that coagulation pathways are often activated during the progression of cancers. About 50 % of all patients, and up to 95 % of those with metastatic lesions have abnormality of hemostatic parameters [1]. A persuasive body of evidence shows that hemostatic factors can interact with cancer cells and be involved in tumor growth, progression, and metastasis [2]. Most solid tumors in humans and experimental animals contain considerable amounts of fibrinogen-related products, mostly cross-linked fibrin, suggesting that fibrinogen plays an important role during the process of tumor stroma formation [3, 4].
Fibrinogen is a glycoprotein synthesized by hepatocytes and it is converted to fibrin by activated thrombin [5]. Fibrinogen is a key protein in the coagulation pathway, clot formation, and wound healing, and it supports platelet aggregation, which represents the final step of the coagulation cascade [6, 7]. Fibrin matrices promote the migration of a substantial number of distinct cell types, including transformed cells, endothelial cells, macrophages, and fibroblasts [4, 8, 9]. Fibrin matrices also promote neovascularization, and they facilitate tumor stroma formation by a mechanism which is analogous to wound repair [10]. Fibrin degradation products (FDPs) have also been shown to display powerful chemotactic, immune-modulatory, and angiogenic properties [11–13]. The role of fibrinogen in carcinogenesis has been suggested previously in several tumor types [14–16]. The incidence of lung metastasis in fibrinogen-deficient mice intravenously transplanted with Lewis lung carcinoma (LLC) [15] or B16 melanoma [17] was significantly reduced when compared with that in wild-type mice. Also, when LLC was subcutaneously inoculated in these transgenic mice the number of metastases in regional lymph nodes and the lungs was markedly reduced compared with the number in wild-type mice [15]. These results raised the possibility that hyperfibrinogenemia might function to enhance metastasis formation, as compared with a low fibrinogen level. Interestingly, there was no marked difference in the growth of subcutaneously transplanted tumors between the fibrinogen-deficient and wild-type mice, indicating that fibrinogen plays a major role in the development of metastases but not in the growth of the primary tumor [15]. It has been suggested that the formation of platelet–fibrin-oncocyte aggregates may be causally related to endothelial adhesion and metastatic potential [18–20]. Furthermore, fibrin/fibrinogen deposition induces fibrinolytic activity resulting in the degradation of the extracellular matrix, providing fertile ground for tumor cell planting; as well, fibrin/fibrinogen deposition has a direct mitogenic effect [14, 21, 22]. Taken together, the substantial lines of indirect evidence point to an important role for fibrinogen in tumor progression.
Recent studies in humans have shown that elevated fibrinogen plasma levels are a useful prognostic parameter for several human malignancies, such as gastric cancer, [23] cervical cancer, [24], and ovarian cancer [25]. The purpose of this study was to evaluate the association of preoperative plasma fibrinogen levels with clinicopathological parameters, disease-free survival (DFS), and overall survival (OS) in patients after nephrectomy for RCC.
Patients and methods
Patients
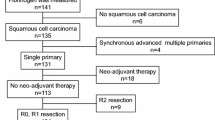
In total, 286 consecutive patients with histopathologically verified RCC who underwent radical nephrectomy at the Department of Genitourinary Oncology, Tianjin Medical University Cancer Institute and Hospital, from January 2000 to December 2003, were enrolled in the present study. Patients with a history of other types of malignant tumor, preoperatively existing distant metastasis, lymph node involvement, or venous tumor thrombus, and patients with inflammatory disorders were excluded. All patients were treated with surgery alone. Clinical data were extracted from patient files.
Of these 286 patients, 185 were male and 101 were female. Ages ranged between 28 and 77 years, with an average of 55.72 years. Disease-free survival (DFS) and cancer-specific survival durations were calculated from the date of surgery. The median DFS duration for the 59 patients with postoperative distant metastasis was 36.6 months, and the DFS for the 227 patients without distant metastasis was 96.5 months. The median follow-up period for the 56 patients who died of an RCC-related cause was 34.6 months, and this period for the 230 survivors was 94.5 months. The clinicopathological staging for each patient at the time of surgery was determined by using the 1997 International Union Against Cancer (UICC) TNM classification of malignant tumors. All tissue sections were reevaluated by one pathologist according to the 2004 WHO classification of kidney cancer and the Fuhrman grading system. The distribution of pathological subtypes postoperatively was as follows: 238 patients had clear cell RCC and 48 had non-clear cell RCC (papillary, chromophobe, collecting duct, and unclassified RCC).
After nephrectomy, follow up of all patients was carried out every 3 months for 2 years, then every 6 months thereafter or until death. The check-up items included physical examination, ultrasound, chest X-ray, and computed tomographic scan.
Fibrinogen measurement
Peripheral blood samples were collected 48–72 h before the operation, and plasma fibrinogen was measured by the Clauss clotting method using DADE Thrombin Reagent™ and a Sysmex CA-7000 automated coagulometer (Sysmex, Kobe, Japan). Plasma fibrinogen levels between 200 and 400 mg/dl were considered to be normal.
Statistical analysis
Preoperative plasma fibrinogen values are expressed as means (±SD). The correlation between preoperative plasma fibrinogen and clinicopathological factors was evaluated by unpaired t-test, and one-way analysis of variance (ANOVA) with the least significant difference (LSD) multiple comparison, where appropriate.
The DFS rate and 5-year survival rate were calculated by the Kaplan–Meier method, and differences between groups were tested with the log-rank test. Disease-free survival (DFS) times and cancer-specific survival times of patients were censored at the last follow-up date. Factors examined in the univariate analysis were: sex (male vs. female), age (<50 vs. 50–60 vs. >60 years), histological type (clear cell vs. non-clear cell), tumor size (<4 vs. 4–7 vs. 8–10 vs. >10 cm), T stage (T1 vs. T2 vs. T3 vs. T4), Fuhrman grade (I vs. II vs. III vs. IV), hemoglobin (≥ lower limit of normal [LLN] vs. <LLN), corrected calcium (≤11 mg/dl vs. >11 mg/dl), lactate dehydrogenase (LDH, ≤1.5 × upper limit of normal [ULN] vs. >1.5 × ULN), and the preoperative plasma fibrinogen level (per 100 U). LLN and ULN were the lower and upper limits, respectively, of the laboratory’s normal range. Univariate analyses were performed to identify variables associated with 5-year DFS and 5-year OS. Variables in the univariate analysis that had a P value of <0.05 were included in the multivariate analysis, which was performed by the Cox proportional hazard model using a forward LR stepwise procedure for variable selection. All laboratory variables and tumor size were treated as continuous variables in the multivariate analysis. The hazard ratios (HRs) and the corresponding 95 % confidence intervals (CIs) were obtained, and statistical significance was set at P < 0.05. Statistical analyses and graphics were performed with the SPSS 13.0 statistical software package (SPSS, Chicago, IL, USA).
Results
Correlation analysis
The mean (±SD) preoperative plasma fibrinogen level was 314.4 ± 85.9 mg/dl. The clinicopathological parameters evaluated included sex, age, Fuhrman grade, histological type, tumor size, T stage, and the preoperative plasma fibrinogen level. Correlations between preoperative plasma fibrinogen levels and clinicopathological parameters are given in Table 1. Elevated plasma fibrinogen levels were associated with age (P = 0.02), tumor size (P < 0.001), Fuhrman grade (P < 0.001), and T stage (P < 0.001), but not with histological type (P = 0.243). Patients who had distant metastasis during follow up had higher preoperative plasma fibrinogen levels.
Univariate analysis
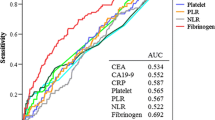
The 5-year DFS rate was 77.1 % for all 286 patients. In the univariate analysis, the significant prognostic factors were tumor size (P < 0.001), Fuhrman grade (P < 0.001), T stage (P < 0.001), hemoglobin (P < 0.001), corrected calcium (P < 0.001), LDH (P < 0.001), and preoperative plasma fibrinogen levels (P < 0.001), as shown in Table 2. Kaplan–Meier curves for DFS, stratified for different plasma fibrinogen levels, are shown in Fig. 1.
The 5-year survival rate was 82.4 % for all 286 patients. In the univariate analysis, the significant prognostic factors were tumor size (P < 0.001), Fuhrman grade (P < 0.001), T stage (P < 0.001), hemoglobin (P < 0.001), corrected calcium (P = 0.002), LDH (P = 0.001), and preoperative plasma fibrinogen levels (P < 0.001) (Table 3). Kaplan–Meier curves for OS, stratified by different plasma fibrinogen levels, are shown in Fig. 2. In addition, Kaplan–Meier curves for OS, stratified by different plasma fibrinogen levels, in patients who developed distant metastasis, are shown in Fig. 3.
Multivariate analysis
In the multivariate analysis by the Cox proportional hazard model, preoperative plasma fibrinogen levels were an independent prognostic factor for both DFS (HR = 1.423, P = 0.021) and OS (HR = 1.997, P < 0.001). In addition, the Fuhrman grade, T stage, hemoglobin, corrected calcium, and LDH were independent prognostic factors for DFS. The T stage, hemoglobin, corrected calcium, and LDH were independent prognostic factors for OS (Table 4).
Discussion
Renal cell carcinoma (RCC) is an oncological disease with a biologically heterogeneous phenotype. Wide survival estimates exist for a given stage of disease even with putatively clinically localized disease. Of the 50,000 patients diagnosed with RCC every year, approximately 70 % will present with localized disease. Although nephrectomy is potentially curative, metastases will nonetheless develop in 30 % of those with localized disease. Metastases reduce overall 5-year survival from greater than 90 % to less than 10 % and decrease median overall survival (OS) to less than 1 year. Based on this dramatically decreased survival, in addition to the classic TNM system, we sought prognostic markers of DFS and OS, including serum markers such as hemoglobin, corrected calcium, and LDH.
In the present study, our main findings were as follows: (1) elevated preoperative plasma fibrinogen levels were associated with the Fuhrman grade, tumor size, and T stage. (2) Elevated preoperative plasma fibrinogen levels were a risk factor for postoperative distant metastasis after nephrectomy for RCC. (3) Preoperative plasma fibrinogen levels were an independent prognostic factor for the patients with localized RCC.
Recent studies have shown that thrombin might also be an important modulator of cancer metastasis in vivo [26]. In the present study, prothrombin time (PT) and activated partial thromboplastin time (APTT) were examined in each patient, but no significant associations with postoperative distant metastasis, T stage, or plasma fibrinogen levels were found (data not shown). Of note, Kerlin and co-workers [27] recently demonstrated that elevated fibrinogen levels in hyperfibrinogenemia transgenic mice with suppressed thrombin activity did not alter the incidence or extent of thrombus formation. Their findings suggested that hyperfibrinogenemia is more than a by-product of cardiovascular disease, but may—in a positive or negative manner—determine the severity and/or progression of vascular disease. It therefore seems that high fibrinogen levels are not associated with systemic thrombin activation and subsequent enhancement of fibrin formation. This is in accordance with previous findings in patients with gastric cancer [23].
In our study, the plasma fibrinogen level was a clinically relevant event related to Fuhrman grade, advanced T stage, and postoperative distant metastasis, and our results strongly suggest that fibrinogen is involved in the progression of RCC during the later phase of the disease. This is in accordance with previously published data in patients with other malignancies [23–25], reflecting the fact that the plasma fibrinogen level seems to rise with tumor progression and metastasis.
Fibrinogen may enhance metastasis through several possible mechanisms. Firstly, the soluble form of fibrinogen could serve as a bridging molecule between tumor cells and host cells. Fibrinogen is a dimeric molecule with multiple integrin and non-integrin binding motifs, and malignant cells often express high levels of fibrinogen receptors, such as α5β1 and αvβ3 integrins or intercellular adhesion molecule 1 (ICAM-1). In addition, tumor cells and platelets can form large aggregates through the binding of fibrinogen, because platelet αIIbβ3 integrin receptors have a high affinity for fibrinogen. These aggregates effectively form microemboli in target organs, which can protect tumor cells from the innate immune system [28, 29]. A study by Palumbo and colleagues [17] found that the number of tumor cells located in the lung was markedly decreased in fibrinogen-deficient mice 4–24 h after tumor inoculation, but at no earlier time points. This suggests that fibrinogen is essential for the sustained adherence of tumor cells to the endothelia of target organs [17].
Although there is sufficient evidence to suggest that elevated fibrinogen levels might aid the development of metastatic lesions, we cannot ignore the possibility that this elevation is simply the result of the tumor mass spreading. Fibrinogen, which is one of the major acute phase proteins produced by the liver, is greatly enhanced in response to infection or other inflammatory disorders. Indeed, in our study, the fibrinogen levels in all of the patients with preoperative acute inflammatory disorders were high. Inflammatory proteins, such as interleukin (IL)-6 and C-reactive protein (CRP), are reported to be higher in cancer patients than in non-cancer patients. It has already been reported that the CRP level did not show an independent association with lymphatic metastasis, although the plasma fibrinogen level did [30], suggesting that hyperfibrinogenemia, different from high serum CRP, may not be a simple by-product of the inflammatory response caused by tumor progression but might have some etiologic relevance to tumor metastasis. In addition, elevated fibrinogen could also be the result of hypercoagulation and/or a hypoxic status caused by tumor growth, through the production of fibrinogen by the tumor cells themselves. In the present retrospective study, however, we could not show a precise causal relationship between hyperfibrinogenemia and cancer metastasis.
Our results have shown that an elevated preoperative plasma fibrinogen level is an independent risk factor for DFS time and OS in patients with RCC in a multivariate analysis. This is in accordance with findings in other malignancies [23–25]. This finding supports the assumption that elevated fibrinogen plasma levels are derived from tumor cells and their microenvironment that exhibit tumor-promoting effects, rather than being signs of a host-versus-tumor response.
Conclusions
The present study suggests that the plasma fibrinogen level is an independent predictor of advanced tumor stage, postoperative distant metastasis, DFS time, and OS time after nephrectomy for RCC. The value of monitoring plasma fibrinogen levels for detecting recurrent disease after nephrectomy needs to be elucidated in the future.
Abbreviations
- RCC:
-
Renal cell carcinoma
- DFS:
-
Disease-free survival
- OS:
-
Overall survival
- CRP:
-
C-reactive protein
- LDH:
-
Lactate dehydrogenase
References
Rickles FR, Edwards RL (1983) Activation of blood coagulation in cancer: Trousseau’s syndrome revisited. Blood 62:14–31
Wang X, Wang E, Kavanagh JJ et al (2005) Ovarian cancer, the coagulation pathway, and inflammation. J Transl Med 3:25
Bardos H, Molnar P, Csecsei G et al (1996) Fibrin deposition in primary and metastatic human brain tumours. Blood Coagul Fibrinolysis 7:536–548
Dvorak HF, Nagy JA, Berse B et al (1992) Vascular permeability factor, fibrin, and the pathogenesis of tumor stroma formation. Ann N Y Acad Sci 667:101–111
Tennent GA, Brennan SO, Stangou AJ et al (2007) Human plasma fibrinogen is synthesized in the liver. Blood 109:1971–1974
Collen D, Tytgat GN, Claeys H et al (1972) Metabolism and distribution of fibrinogen. I. Fibrinogen turnover in physiological conditions in humans. Br J Haematol 22:681–700
Koenig W (2003) Fibrin(ogen) in cardiovascular disease: an update. Thromb Haemost 89:601–609
Altieri DC, Mannucci PM, Capitanio AM (1986) Binding of fibrinogen to human monocytes. J Clin Invest 78:968–976
Dejana E, Languino LR, Polentarutti N et al (1985) Interaction between fibrinogen and cultured endothelial cells. Induction of migration and specific binding. J Clin Invest 75:11–18
Dvorak HF, Harvey VS, Estrella P et al (1987) Fibrin containing gels induce angiogenesis. Implications for tumor stroma generation and wound healing. Lab Invest 57:673–686
Gross TJ, Leavell KJ, Peterson MW (1997) CD11b/CD18 mediates the neutrophil chemotactic activity of fibrin degradation product D domain. Thromb Haemost 77:894–900
Languino LR, Duperray A, Joganic KJ et al (1995) Regulation of leukocyte–endothelium interaction and leukocyte transendothelial migration by intercellular adhesion molecule 1-fibrinogen recognition. Proc Natl Acad Sci USA 92:1505–1509
Robson SC, Saunders R, Purves LR et al (1993) Fibrin and fibrinogen degradation products with an intact D-domain C-terminal gamma chain inhibit an early step in accessory cell-dependent lymphocyte mitogenesis. Blood 81:3006–3014
Gerner C, Steinkellner W, Holzmann K et al (2001) Elevated plasma levels of crosslinked fibrinogen gamma-chain dimer indicate cancer-related fibrin deposition and fibrinolysis. Thromb Haemost 85:494–501
Palumbo JS, Potter JM, Kaplan LS et al (2002) Spontaneous hematogenous and lymphatic metastasis, but not primary tumor growth or angiogenesis, is diminished in fibrinogen-deficient mice. Cancer Res 62:6966–6972
Palumbo JS, Talmage KE, Massari JV et al (2005) Platelets and fibrin(ogen) increase metastatic potential by impeding natural killer cell-mediated elimination of tumor cells. Blood 105:178–185
Palumbo JS, Kombrinck KW, Drew AF et al (2000) Fibrinogen is an important determinant of the metastatic potential of circulating tumor cells. Blood 96:3302–3309
Cavanaugh PG, Sloane BF, Honn KV (1988) Role of the coagulation system in tumor-cell-induced platelet aggregation and metastasis. Haemostasis 18:37–46
Chew EC, Wallace AC (1976) Demonstration of fibrin in early stages of experimental metastases. Cancer Res 36:1904–1909
Crissman JD, Hatfield JS, Menter DG et al (1988) Morphological study of the interaction of intravascular tumor cells with endothelial cells and subendothelial matrix. Cancer Res 48:4065–4072
Hatzfeld JA, Hatzfeld A, Maigne J (1982) Fibrinogen and its fragment D stimulate proliferation of human hemopoietic cells in vitro. Proc Natl Acad Sci USA 79:6280–6284
Pollanen J, Stephens RW, Vaheri A (1991) Directed plasminogen activation at the surface of normal and malignant cells. Adv Cancer Res 57:273–328
Yamashita H, Kitayama J, Kanno N et al (2006) Hyperfibrinogenemia is associated with lymphatic as well as hematogenous metastasis and worse clinical outcome in T2 gastric cancer. BMC Cancer 6:147
Polterauer S, Seebacher V, Hefler-Frischmuth K et al (2009) Fibrinogen plasma levels are an independent prognostic parameter in patients with cervical cancer. Am J Obstet Gynecol 200(647):e641–e647
Polterauer S, Grimm C, Seebacher V et al (2009) Plasma fibrinogen levels and prognosis in patients with ovarian cancer: a multicenter study. Oncologist 14:979–985
Lopez Y, Paloma MJ, Rifon J et al (1999) Measurement of prethrombotic markers in the assessment of acquired hypercoagulable states. Thromb Res 93:71–78
Kerlin B, Cooley BC, Isermann BH et al (2004) Cause-effect relation between hyperfibrinogenemia and vascular disease. Blood 103:1728–1734
Nieswandt B, Hafner M, Echtenacher B et al (1999) Lysis of tumor cells by natural killer cells in mice is impeded by platelets. Cancer Res 59:1295–1300
Yano HJ, Hatano K, Tsuno N et al (2001) Clustered cancer cells show a distinct adhesion behavior from single cell form under physiological shear conditions. J Exp Clin Cancer Res 20:407–412
Yamashita H, Kitayama J, Nagawa H (2005) Hyperfibrinogenemia is a useful predictor for lymphatic metastasis in human gastric cancer. Jpn J Clin Oncol 35:595–600
Acknowledgments
This work was supported by a Grant from the National Natural Science Foundation of China, No. 81072090.
Conflict of interest
We have no conflicts of interest to declare.
Author information
Authors and Affiliations
Corresponding author
Additional information
J. Du and J.-H. Zheng contributed equally to this work.
About this article
Cite this article
Du, J., Zheng, JH., Chen, XS. et al. High preoperative plasma fibrinogen is an independent predictor of distant metastasis and poor prognosis in renal cell carcinoma. Int J Clin Oncol 18, 517–523 (2013). https://doi.org/10.1007/s10147-012-0412-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10147-012-0412-x