Abstract
Three-column osteotomy (3-CO) is a powerful technique in adult deformity surgery, and pedicle subtraction osteotomy (PSO) is the workhorse to correct severe kyphotic spinal deformities. Aging of the population, increasing cases of iatrogenic flat back deformities and understanding the importance of sagittal balance have led to a dramatic increase of this surgical technique. Surgery, however, is demanding and associated with high complication rates so that every step of the procedure requires meticulous technique. Particularly, osteotomy closure is associated with risks like secondary fracture, translation, or iatrogenic stenosis. This step is traditionally performed by compression or a cantilever maneuver with sometimes excessive forces on the screws or instrumentation. Implant loosening or abrupt subluxation resulting in construct failure and/or neurological deficits can result. The aim of this prospective registry study was to assess the efficacy and safety of our surgical PSO technique as well as the osteotomy closure by flexing a hinge-powered OR table. In a series of 84 consecutive lumbosacral 3-CO, a standardized surgical technique with special focus on closure of the osteotomy was prospectively evaluated. The surgical steps with the patients positioned prone on a soft frame are detailed. Osteotomy closure was achieved by remote controlled bending of a standard OR table without compressive or cantilever forces in all 84 cases. This technique carries a number of advantages, particularly the reversibility and the slow speed of closure with minimum force. There was not a single mechanical intraoperative complication such as vertebral body fracture, subluxation, or adjacent implant loosening during osteotomy closure, compared to external cohorts using the cantilever technique (p = 0.130). The feasibility of controlled 3-CO closure by flexing a standard OR table is demonstrated. This technique enables a safe, gentle closure of the osteotomy site with minimal risk of implant failure or accidental neurological injury.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The three-column osteotomy (3-CO) is a powerful technique to correct sagittal and coronal imbalance in adult deformity surgery. Pedicle subtraction osteotomy (PSO) is the workhorse to correct kyphotic spinal deformities [29]. It is a closed wedge osteotomy with shortening of the dorsal structures, by resecting the lamina, facet joints, and pedicles at the index level. In case of a PSOplus, the adjacent disc is removed as well to achieve more correction. In the presence of severe deformities, vertebral column resection (VCR) may be required. In recent years, usage of three-column osteotomies (3-CO) has increased almost exponentially to particularly treat the increasing number of iatrogenic flat back syndromes due to a better understanding of the concept of sagittal balance. Several authors have demonstrated improved health-related quality of life (HRQL) by restoring sagittal alignment [5, 19, 20]. PSO and Smith-Peterson osteotomy (SPO) are well known procedures to correct sagittal plane deformity [28]. The type of osteotomy depends on the degree of deformity. Schwab et al. introduced a classification (grade 1–6) regarding the amount of bone resection, potential instability, and the possibility of a large corrective move [25]. To summarize the classification, grades 1 and 2 consist of a partial or complete facet joint resection, grades 3 and 4 are so-called pedicle subtraction osteotomies with or without the resection of the adjacent disc (PSOplus), whereas grades 5 and 6 describe a vertebral column resection (VCR) performed at one or two segments [7]. To correct extensive sagittal plane deformities (> 25°), we propose a PSO (grade 3) or PSOplus (grade 4), if needed in combination with additional osteotomies (SPO) at further levels [7].
Adult deformity surgery, however, is demanding and associated with high complication rates so that every step of the procedure requires meticulous technique. Particularly, osteotomy closure is associated with risks like secondary fracture, translation, or iatrogenic stenosis. This step is traditionally performed by compression or a cantilever maneuver with sometimes excessive forces on the adjacent screws or instrumentation. Implant loosening or abrupt subluxation resulting in construct failure and/or neurological deficits can result, varying from 2 to 15% in literature [2, 3, 9, 10, 12, 15, 17, 24].
With the dramatic increase in spinal instrumentation, spine surgeons face more and more effects of fusion such as adjacent segment disease and iatrogenic kyphoscoliosis recently [12, 22, 27]. Many spine centers aim at introducing 3-CO, which automatically comes with a learning curve and associated complications. The scope of this manuscript is to detail the surgical steps of our PSO technique with special emphasis on osteotomy site closure and to present intraoperative results in a large consecutive series.
Materials and methods
A standardized step-wise surgical technique for 3-CO has been developed at our center and applied continuously since 2011. After obtaining approval by the institutional ethics committee, 84 consecutive patients, who underwent lumbosacral 3-CO with osteotomy site closure by bending a standard OR table (††) and use of a special osteotomy set (*), were analyzed. Surgical details, construct length, duration of surgery, and hardware failure were collected prospectively. The particular focus of this study was to evaluate the efficacy and safety of osteotomy closure by remotely bending a standard OR table without any compression or cantilever forces on the instrumentation under fluoroscopic control. This method of using the operating table provides limited ability to adjust the position of the head, which must be carefully secured by anesthesia during the maneuver.
Preoperative planning is essential to determine the amount of correction needed and requires an in-depth analysis of spinopelvic parameters and Roussouly types.8 Compensatory mechanisms have to be taken into consideration when calculating the amount of required correction [7, 21]. This article, however, focuses on the intraoperative, not preoperative steps.
Statistical analysis was performed using SPSS Statistics 27 (IBM, Armonk, New York, USA). Chi-square and Fisher exact test were used for dichotomous data analysis depending on the number of subjects involved. A p value of less than 0.05 was considered statistically significant. The Wilson test was applied for binominal confidence interval calculation. Data entry in an electronic database was performed in a pseudonymized form. Data was stored according to local regulations in a database.
Step-wise surgical technique
-
Place the patient in prone position under general anesthesia on a standard OR table (††). A soft cushion frame supports the thorax and the pelvis leaving the abdomen decompressed. The level of osteotomy should be exactly at the hinge of the table (Fig. 1A).
-
Perform standard posterior exposure with meticulous hemostasis, exposure of all posterior bony structures: lamina, isthmus, facet joints, and transverse processes.
-
Implant pedicle screws at least two adjacent levels above or below the osteotomy with/without navigation, free-hand or under fluoroscopy.
-
Perform SPOs and TLIFs at additional levels if necessary, according to the preoperative plan.
-
Resect the base of the transverse processes with a drill or Kerrison Rongeurs. Dissect the paravertebral muscles and segmental artery from the lateral part of the vertebral body, and apply a folded hemostatic sponge (^).
-
Resect the inferior facets of the upper vertebra, the superior isthmus, the inferior facets, and the entire lamina of the index vertebra, and extensively decompress the nerve roots laterally, above and below the index level. In some cases, temporary distraction devices (**) may be helpful to prevent early partial closure after bony resection (Fig. 1B).
-
Use a special PSO osteotomy set (*) for the following steps.
-
Open and hollow the pedicles by using several specific dilators consecutively (Fig. 2A and B).
-
Create a hollow space in front of the posterior vertebral wall, and progressively push the cancellous bone anteriorly to create a solid anterior fusion mass (Fig. 2C and D).
-
Resect the pedicles with specifically shaped osteotomes (Fig. 3 A and B; Fig. 4C).
-
Remove the adjacent superior disc (in case of PSOplus).
-
Remove two thirds of the lateral cortical wall in a wedge-shaped manner and chisel to the anterior third of the vertebra to minimize the risk of superior endplate fracture (Fig. 3C and D).
-
Resect the posterior vertebral wall in two steps with a special posterior wall impactor* (Fig. 4A).
-
Remove the posterior anulus with a Kerrison Rongeurs underneath the dural sac, if the adjacent superior disc is also resected.
-
Apply the gentle osteotomy closure technique by adjusting the OR table hinge (remotely controlled) (††) (Fig. 5B) under continuous visualization of the dural sac and nerve roots without stress to the implants under fluoroscopic surveillance.
-
Finalize the construct by rod implantation (Fig. 4D).
(A) Position the patient in prone position on a standard OR table on top of a soft cushion frame, with the level of osteotomy at the hinge of the table (red arrow). (B) Perform a standard midline posterior approach with meticulous hemostasis. Instrumentation spanning at least two levels above and below the index level. Sufficiently decompress the nerve root laterally, above and below the index pedicle. Use a distraction device to prevent partial osteotomy closure
*: PSO Osteotomy Set Medtronic ®, Medtronic plc, Dublin, Ireland.
**: TLIF poly screw distractor ®, DePuy Synthes Spine, Johnson & Johnson, Medical Devices Companies, Raynham, MA 02,767, USA.
^: Spongostan®, Ethicon, Johnson & Johnson; New Brunswick, NJ, USA.
††: Maquet 1150 ®, Maquet Gmbh; Germany, 76,437 Rastatt/Germany.
Results
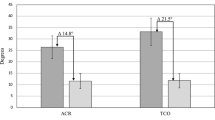
Our cohort represents a typical patient population of adult deformity with female predominance and a mean age of 65.6 ± 10.1 years (range: 32–83). The average PI-LL mismatch was 31° with a mean PI of 55° and preoperative lumbar lordosis averaging 24°. Osteotomies were primarily performed in the lumbar spine, especially at the levels of L4 and L3. Fifty-seven patients (67.9%) were treated with a short construct, spanning between 5 and 7 motion segments and instrumentation at least two levels above and below. Forty-two patients (50.0%) received a PSO, 38 (45.2%) a PSOplus, whereas 4 patients (4.8%) were treated with a VCR. The mean operation time was 384 ± 102 min. It has to be noted, however, that the longest surgical step in our cohort consisted of decompression and adhesiolysis, as the majority of patients (73.8%) had several prior surgeries (Table 1).
Prospective analysis of this series of 84 consecutive patients who underwent lumbosacral 3-CO with our gentle osteotomy closing technique did not reveal a single intraoperative mechanical complication due to the maneuver such as implant loosening or abrupt vertebral body subluxation. Lumbar lordosis improved significantly after 3-CO (24.1 ± 17.8° vs. 51.3 ± 10.6°; p < 0.001).
No perioperative hardware failure was noted following the gentle osteotomy closure with the assistance of a flexible hinge-powered operating table (n = 0 (0.0%); p = 0.130; CI95, 0.000–0.0437; Wilson), compared to external cohorts. Two patients showed postoperative neurologic deficits (n = 2 (2.4%); p = 0.032*; CI95, 0.0066–0.0827) [2, 3, 8, 11, 12].
Discussion
Our standardized step-wise surgical technique for 3-CO with special focus on closure of the osteotomy site was able to completely prevent intraoperative mechanical complications in a large prospective series. Gentle closure by using a remotely controlled hinge-powered standard OR table obviates the application of high compressive or cantilever forces on the implants, which carry the risk of uncontrolled subluxation, fracture, or stenosis. Flexing the OR table exactly at the level of the osteotomy seems to be a safe and advantageous alternative to applying excessive force on the instrumentation.
Many variants of spinal osteotomies have been described in the literature, and it is well accepted that 3-CO is a demanding procedure which should be performed in specialized spine centers by experienced surgical and anesthesiological teams [1, 3, 6, 8, 14, 16, 25, 28].
Posterior subperiostal exposure, meticulous hemostasis, and placement of pedicle screws in free-hand or navigated technique with complete laminectomy and far lateral decompression of the upper and lower nerve roots followed by the resection of both transverse processes at the index level have been rather standardized. However, there are different osteotomy techniques which apply osteotomes or chisels to resect the pedicles and the adjacent bone above and below. As a final step, the posterior vertebral wall anterior to the dural sac is removed by upwards angled pituitary Rongeurs or decancellation techniques like the eggshell procedure. Osteotomy of cancellous bone is often associated with significant bleeding, and a significant risk of pseudarthrosis at the osteotomy level has been described repeatedly with these techniques [6, 13, 23].
In our case series, we applied a specific osteotomy set *, which compacts the cancellous bone via a transpedicular route and pushes the bone forward. Bone compaction minimizes blood loss and creates a solid fusion mass anteriorly. As many patients are osteoporotic, this may prevent pseudarthrosis, and we have not seen a case of pseudarthrosis at the osteotomy site in the reported 84 patients. The last step prior to closure is the resection of the posterior wall with a specific impactor after dissection of the posterior longitudinal ligament.
Traditionally, the surgical step of osteotomy closure is performed by compression or cantilever maneuvers with sometimes excessive forces on the adjacent implants and bony structures or in combination with patient repositioning on the table with extension of the hips joints and elevation of the trunk [3, 6, 8, 12].
This can lead to loosening or abrupt subluxation especially in osteoporotic patients resulting in intra- or postoperative implant failure or neurological deficit [2, 18].
The 3-CO is an obviously destabilizing procedure that carries a high risk of secondary neurological deficits caused by fracture, translation, or iatrogenic stenosis following closure of the osteotomy.
Despite being a known complication, exact numbers of perioperative hardware failure and screw loosening are rarely published. We, however, were able to introduce a safe osteotomy site closure technique without any perioperative hardware failure. Furthermore, this technique enables the reopening of the osteotomy site in case of dural kinking or suspected nerve root entrapment. This technical advantage resulted in a significant reduced number of patients with associated neurologic deficits (p = 0.032) [2, 3, 8, 11, 12].
Several authors have described their technical aspects to perform osteotomies. Osteotomy closure is generally achieved by compression or cantilever maneuvers, sometimes with specially designed instruments connected to the pedicle screws. Only a single case report has described the use of a flexible hinge-powered operating table for controlled PSO site closure [3, 7, 9, 12, 24].
The reported technique enables a safe, gentle closure of the osteotomy with no or a very low risk of implant failure or accidental injury of nervous structures. By simple use of a standard OR table in combination with a soft cushion frame, stable patient positioning even in presence of severe fixed kyphotic deformity with flexed hips is possible (Fig. 5A and B; Fig. 6), which might be cumbersome with other positioning devices. Furthermore, the table can be moved back and forth on top of its base to enable AP views during instrumentation.
Pre- and postoperative full spine standing X-rays and computed tomography of the lumbar spine of an 84-year-old female patient with a fixed kyphotic deformity and sagittal imbalance. The massive lumbar kyphosis of 65° resulted from interspinous implants at the levels L2/3, L3/4, and L4/5 and an osteoporotic fracture of L3. The patient was immobilized due to severe low back pain (VAS 10). After instrumentation of L1 to the ilium and VCR of L3 gentle closure of the osteotomy site using the hinge-powered OR table obviated the need to put any stress on the implants. Outcome was excellent at 2 years with minimal low back pain (VAS 3) and a walking distance of 200 m
An additional crucial advantage of the applied closure technique is the fact that the osteotomy can be reopened and closed degree by degree to check for inadvertent nerve root or dural sac compression or allow additional resection of bony structures in case of residual stenosis. Once the rods are inserted and the osteotomy is secured, the table is brought back into the original position for wound closure.
Tips and pearls
-
For lumbar osteotomies, no temporary rod is required [3].
-
Meticulous adhesiolysis is mandatory to remove dural scarring in case of prior surgery to avoid dural kinking during osteotomy closure.
-
Beware of stenosis of the dural sac during osteotomy closure. Our technique allows gentle reopening and closure of the osteotomy without stress on pedicle screws and bony structures to optimize the maneuver and potentially extend dural sac decompression.
-
Any abnormal resistance during osteotomy closure is highly indicative of insufficient bony resection and/or persistent cortical bone, in particular of the lateral and/or the posterior wall of the vertebral body [3].
-
Cobalt chromium rods are possible to increase the strength of the construct and reduce the risk of rod fracture. Currently, however, the use of one or two satellite rods to span the osteotomy connected with side to side connectors in a titanium construct seems ideal, as it provides high rigidity at the level of the osteotomy and more flexibility at the ends of the construct [4, 26].
-
Autografts augmented with bone substitutes were put on the surface of the posterior bony elements to enhance fusion.
-
Intraoperative monitoring of MEP/SSEP is mandatory for osteotomies performed in the thoracic spine, but not required below the level of the conus medullaris [3].
-
Postoperative orthoses are not standardized required.
The metal components of the table, however, limit intraoperative imaging, which would be possibly with carbon fiber OR tables. Spinal navigation is thus more challenging. Internationally, many patients are treated on a standard Jackson table, which often, despite its advantages, does not allow bending. However, with some new models, flexion at a hinge is possible and therefore allows the adaption of the above-mentioned osteotomy closure technique [16].
Conclusion
This study of 84 consecutive patients undergoing lumbosacral 3-CO demonstrates the feasibility of using a flexible hinge-powered operating table for controlled osteotomy closure without any mechanical intraoperative complication. This technique eliminates application of massive force to the instrumentation and bony structures and thereby minimizes the risk of vertebral body fracture or translation and consecutive neurological impairment.
Data availability
The datasets used and/or analyzed during the current study available from the corresponding author on reasonable request.
Code availability
Not applicable.
References
Ames CP, Barry JJ, Keshavarzi S, Dede O, Weber MH, Deviren V (2013) Perioperative outcomes and complications of pedicle subtraction osteotomy in cases with single versus two attending surgeons. Spine Deform 1(1):51–58
Auerbach JD, Lenke LG, Bridwell KH et al (2012) Major complications and comparison between 3-column osteotomy techniques in 105 consecutive spinal deformity procedures. Spine 37(14):1198–1210
Barrey C, Perrin G, Michel F, Vital J-M, Obeid I (2014) Pedicle subtraction osteotomy in the lumbar spine: indications, technical aspects, results and complications. Eur J Orthop Surg Traumatol 24(S1):21–30
Birkenmaier C (2018) Pseudarthrose und Konstruktversagen nach lumbaler Pedikelsubtraktionsosteotomie: Einflüsse von Biomechanik, Operationstechnik Biologie und Vermeidungsstrategien. Orthopäde 47(4):310–319
Boissière L, Takemoto M, Bourghli A et al (2017) Global tilt and lumbar lordosis index: two parameters correlating with health-related quality of life scores—but how do they truly impact disability? Spine J 17(4):480–488
Bourghli A, Cawley D, Novoa F, Rey M, Alzakri A, Larrieu D, Vital J-M, Gille O, Boissiere L, Obeid I (2018) 102 lumbar pedicle subtraction osteotomies: one surgeon’s learning curve. Eur Spine J 27(3):652–660
Bridwell KH (2006) Decision making regarding Smith-Petersen vs. pedicle subtraction osteotomy vs. vertebral column resection for spinal deformity. Spine 31(19 Suppl):S171-178
Bridwell KH, Lewis SJ, Edwards C, Lenke LG, Iffrig TM, Berra A, Baldus C, Blanke K (2003) Complications and outcomes of pedicle subtraction osteotomies for fixed sagittal imbalance. Spine 28(18):2093–2101
Bridwell KH, Lewis SJ, Lenke LG, Baldus C, Blanke K (2003) Pedicle subtraction osteotomy for the treatment of fixed sagittal imbalance. J Bone Jt Surg 85-A(3):454–463
Buchowski JM, Bridwell KH, Lenke LG, Kuhns CA, Lehman RA, Kim YJ, Stewart D, Baldus C (2007) Neurologic complications of lumbar pedicle subtraction osteotomy: a 10-year assessment. Spine 32(20):2245–2252
Daubs MD, Brodke DS, Annis P, Lawrence BD (2016) Perioperative complications of pedicle subtraction osteotomy. Glob Spine J 6(7):630–635
Faundez A, Le Huec J-C, Hansen LV, Poh Ling F, Gehrchen M (2019) Optimizing pedicle subtraction osteotomy techniques: a new reduction plier to increase technical safety and angular reduction efficiency. Oper Neurosurg 16(3):383–388
Huec J-C, Aunoble S (2012) Pedicle subtraction osteotomy for sagittal imbalance. Eur Spine J 21(9):1896–1897
Hyun S-J (2013) Spinal pedicle subtraction osteotomy for fixed sagittal imbalance patients. World J Clin Cases 1(8):242
Ikenaga M, Shikata J, Takemoto M, Tanaka C (2007) Clinical outcomes and complications after pedicle subtraction osteotomy for correction of thoracolumbar kyphosis. J Neurosurg Spine 6(4):330–336
Jones KE, Hunt MA, Martin CT, Polly DW (2019) Controlled pedicle subtraction osteotomy site closure using flexible hinge-powered operating table. Oper Neurosurg 17(5):E214–E218
Kim K-T, Suk K-S, Cho Y-J, Hong G-P, Park B-J (2002) Clinical outcome results of pedicle subtraction osteotomy in ankylosing spondylitis with kyphotic deformity. Spine 27(6):612–618
Lau D, Dalle Ore CL, Reid P, Safaee MM, Deviren V, Smith JS, Shaffrey CI, Ames CP (2019) Utility of neuromonitoring during lumbar pedicle subtraction osteotomy for adult spinal deformity. J Neurosurg Spine 31(3):397–407
Le Huec JC, Cogniet A, Demezon H, Rigal J, Saddiki R, Aunoble S (2015) Insufficient restoration of lumbar lordosis and FBI index following pedicle subtraction osteotomy is an indicator of likely mechanical complication. Eur Spine J 24(S1):112–120
Le Huec J-C, Faundez A, Dominguez D, Hoffmeyer P, Aunoble S (2015) Evidence showing the relationship between sagittal balance and clinical outcomes in surgical treatment of degenerative spinal diseases: a literature review. Int Orthop 39(1):87–95
Le Huec JC, Thompson W, Mohsinaly Y, Barrey C, Faundez A (2019) Sagittal balance of the spine. Eur Spine J 28(9):1889–1905
Martin BI, Mirza SK, Spina N, Spiker WR, Lawrence B, Brodke DS (2019) Trends in lumbar fusion procedure rates and associated hospital costs for degenerative spinal diseases in the United States, 2004 to 2015. Spine 44(5):369–376
Murrey DB, Brigham CD, Kiebzak GM, Finger F, Chewning SJ (2002) Transpedicular decompression and pedicle subtraction osteotomy (eggshell procedure): a retrospective review of 59 patients. Spine 27(21):2338–2345
Obeid I, Boissière L, Vital J-M, Bourghli A (2015) Osteotomy of the spine for multifocal deformities. Eur Spine J 24(S1):83–92
Schwab F, Blondel B, Chay E et al (2014) The comprehensive anatomical spinal osteotomy classification. Neurosurgery 74(1):112–120
Seyed Vosoughi A, Joukar A, Kiapour A, Parajuli D, Agarwal AK, Goel VK, Zavatsky J (2019) Optimal satellite rod constructs to mitigate rod failure following pedicle subtraction osteotomy (PSO): a finite element study. Spine J 19(5):931–941
Sheikh SR, Thompson NR, Benzel E, Steinmetz M, Mroz T, Tomic D, Machado A, Jehi L (2020) Can we justify it? Trends in the utilization of spinal fusions and associated reimbursement. Neurosurgery 86(2):E193–E202
Smith-Petersen MN, Larson CB, Aufranc OE (1969) Osteotomy of the spine for correction of flexion deformity in rheumatoid arthritis. Clin Orthop 66:6–9
Thomasen E (1985) Vertebral osteotomy for correction of kyphosis in ankylosing spondylitis. Clin Orthop 194:142–152
Author information
Authors and Affiliations
Contributions
PPG is the first author. PPG, NK, and CT made substantial contributions to the conception. PPG, NK, SL, GM, and SH were actively involved in the acquisition as well as analysis and interpretation of data. PPG, NK, and CT drafted the paper, whereas all authors critically revised it. The final version was read by all authors, who gave the final approval of the version to be published. All authors are accountable for all aspects of the work. PPG should be approached in case of further questions as he is the first and corresponding author.
Corresponding author
Ethics declarations
Ethics approval
The research conducted has been performed in accordance with the Declaration of Helsinki and was approved by the local research ethics committee (AN2014-0234).
Consent to participate
Informed consent for study participation was obtained prior to surgery.
Consent for publication
Informed consent for publication was obtained along with the ICF.
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Girod, PP., Kögl, N., Molliqaj, G. et al. Flexing a standard hinge-powered operating table for lumbosacral three-column osteotomy (3-CO) site closure in 84 consecutive patients. Neurosurg Rev 45, 517–524 (2022). https://doi.org/10.1007/s10143-021-01559-5
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10143-021-01559-5