Abstract
Management options for newly diagnosed vestibular schwannoma (VS) include observation, surgery, or radiation. There are no randomized trials to guide management of patients with VS. This article is a short review of the role of stereotactic radiosurgery in management of newly diagnosed VS.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Vestibular schwannomas (VS) are slow-growing, benign tumors of the cerebellopontine angle that develop from the vestibular portion of the eighth cranial nerve. The most common presenting symptom is unilateral hearing loss. Patients may also experience vertigo, tinnitus, disequilibrium, headache, trigeminal, or facial nerve-related symptoms. In the absence of pathologic tissue, the diagnosis of VS is made radiographically using contrast-enhanced magnetic resonance imaging (MRI). Most VS have an intracanalicular component with widening of the porus acusticus [22]. Extracanalicular extension occurs as these tumors enlarge. VS are not staged but can be graded on the Koos grading scale. In the early twentieth century, surgical resection was the mainstay of treatment for newly diagnosed VS. However, in the current era of higher-quality MRI, VS are diagnosed earlier and potentially at a time when patients still have useful or normal hearing. This prompted a search for less invasive management strategies. In 1969, stereotactic radiosurgery (SRS) was described by Leksell and Noren as a potential alternative to surgical management [17]. Today, management options for newly diagnosed VS include observation, surgery, or radiation. The aim of this article is to provide a concise review of the role of SRS in management of newly diagnosed VS.
Materials and methods
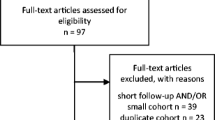
We searched relevant papers within the PUBMED database. All searches used the following keywords: vestibular schwannoma, acoustic neuroma, stereotactic radiosurgery, and management. A secondary search was performed using the bibliographies of the articles from the primary search. Only full-length, original communications were accepted. The search was limited to human subjects and English language publications. Articles were reviewed by title and abstract for potential relevance to this topic. The article itself was reviewed if the title and/or abstract did not clearly indicate degree of relevance.
Results
Our search found 352 papers. After selection, cross-reference checking, and review for clinical relevance, 36 studies met the inclusion criteria for this review. There were 4 prospective studies that analyzed adverse effects and quality of life after observation, SRS, or surgery [1, 3, 6, 27]. The remainder were retrospective studies evaluating dose, local control rates, and toxicity with SRS. Three studies evaluated fractionated SRS outcomes [10, 21, 35]. Other studies included for clinical relevance described growth patterns [12, 30] and radiographic features of VS for diagnosis [22]. There were three systematic literature reviews [24, 33, 36]. There were no randomized trials.
Discussion
Indications for intervention
Large tumors causing brainstem compression or symptoms of mass effect require intervention. Surgery is recommended for VS with significant mass effect if possible. Surgical intervention includes a range of approaches and varying degrees of resection depending on tumor and patient factors as well as surgical expertise [2, 9, 13, 14]. The management of small- to medium-sized VS (< 3 cm) remains controversial despite the significant volume of literature analyzing outcomes. Treatment options include observation with serial imaging, surgery, or radiotherapy [16]. In one series of patients managed with observation, the average growth rate of untreated VS was 0.7 ± 1.4 mm per year [12]. Another study reported a mean volumetric growth rate of 33.5% per year. Factors associated with greater likelihood of tumor growth included larger tumor size and presence of tinnitus at diagnosis. Tumor growth was reported as the most important factor for change in management from observation to intervention in one study [3]. Overall, the goal of observation to defer potential complications of treatment must be weighed against the potential for complication inherent to the natural progression of these tumors. Consideration of patient age and comorbidities may assist in making appropriate treatment decisions in this setting.
Treatment with SRS
The role of SRS in the treatment of VS depends on patient preference and surgical candidacy as well as the experience of the treating institution. Provider bias remains a strong factor dictating treatment decision-making. Typically, targets up to 3.0 cm in maximal diameter are considered appropriate for management with SRS [24]. The International Stereotactic Radiosurgery Society (ISRS) practice guideline considers observation and SRS reasonable treatment options for newly diagnosed small VS without significant mass effect, such as Koos grade I tumors [33]. A prospective cohort study by Breivik et al. looked at the course of VS following treatment with SRS compared with conservative management. After 5 years, there was a significant reduction in tumor volume in the SRS group and a lower incidence rate of future treatment in the SRS group compared with the observation group. Treatment with SRS did not significantly impact rates of hearing loss, symptoms, or quality of life compared with observation [1]. For growing small to moderate size VS without significant mass effect (Koos grades I–III tumors), the ISRS practice guideline considers SRS a reasonable treatment option [33].
SRS dose and tumor control
The ISRS practice guideline for VS recommends a dose of 11–14 Gy to the tumor margin for single-fraction SRS. Series of patients treated with marginal doses of 12–14 Gy reported 5-year control rates ranging from 90 to 99% [4, 5, 15, 19, 23, 26, 32]. It has been reported that a prescription dose of 12.5 Gy to the tumor margin provides an ideal balance of high tumor control with minimal complication [24, 29]. Institutions have seen success with a treatment dose of 11.5 Gy to the 50% isodose line [14]. Klijn S et al. reported a 5-year tumor control rate of 91.3% with similar complication rates to other contemporary series after treatment of 420 patients with gamma knife stereotactic radiosurgery (GKRS) with a median marginal dose of 11 Gy [14]. There is interest in fractionated SRS for tumor dose escalation and potential sparing of auditory and facial nerve functions [34]. Examples of dose fractionations reported in the literature include 4–5 Gy × 5, 3–4 Gy × 10, and 6 Gy × 3 daily. Five-year tumor control rates for fractionated SRS range from 96 to 100% [10, 21, 35]. No studies included in this review reported a difference in 5-year tumor control rates between single-fraction SRS and fractionated SRS.
Toxicity
Toxicity associated with SRS has decreased over the last 40 years in line with a trend towards dose de-escalation [7, 18]. In patients treated with a single-fraction marginal dose of 12–14 Gy, 5-year hearing preservation rates range from 41 to 79% [5, 8, 21, 24, 28]. There are many parameters that can influence the probability of functional hearing preservation after SRS, making evaluation of treatment effect alone difficult. Prognostic factors for hearing preservation after treatment include pretreatment limited hearing loss that is Gardner-Robertson class I and intracanalicular tumor location [12, 29]. Multiple studies have demonstrated a higher chance of hearing preservation when the dose to the cochlea is lower than 4 Gy. Yang et al. performed a systematic literature review of the results of hearing preservation after GKRS that included 45 articles and 4234 patients. Their analysis revealed that patients treated with less than 13 Gy were significantly more likely to have preserved hearing than patients who received larger doses of radiation [36]. Dose rate may impact functional outcomes, and a recent study reported significantly improved freedom from progressive symptomatic hearing loss and facial nerve dysfunction following SRS treatment with dose rates below 2.675 Gy/min [31].
The risk of facial or trigeminal nerve dysfunction after SRS is low [25]. In a study using MRI-based dose planning and a dose of 13 Gy to the tumor margin, the risk of new facial weakness was less than 1% and the risk of trigeminal sensory loss was 3.1% at 5 years. None of the patients who underwent SRS for intracanalicular tumors developed facial or trigeminal neuropathies at 5 years [20]. The Mayo Clinic prospectively compared surgery with SRS in patients with VS less than 3 cm and found that SRS had better facial nerve and hearing preservation than surgery, with similar tumor control [27]. In patients with large tumors that cannot be managed with radiosurgery alone, a facial-nerve sparing resection followed by SRS for significant regrowth is an option that can provide excellent facial nerve preservation rates [11].
Fractionated SRS is sometimes recommended for larger tumors (> 3–4 cm) and to spare normal structures like brainstem and cochlea if close in proximity. Series included in this review did not report statistically significant differences between single-fraction SRS and fractionated SRS in terms of hearing preservation. Trigeminal and facial nerve preservation rates reported for fractionated SRS were similar to those reported for single-fraction SRS [21, 35].
Conclusion
There are no randomized trials to guide management of patients with VS. SRS is an effective treatment option for small- to medium-sized VS without significant mass effect. Surgery and SRS have similar local control rates in appropriately selected patients and in some instances, SRS provides better functional outcomes. Fractionated SRS offers a theoretical radiobiological advantage compared with single-fraction SRS and may allow for improved sparing of normal structures. However, at this time, evidence for differences in toxicity outcome between fractionated and single-fraction SRS is limited.
References
Breivik CN, Nilsen RM, Myrseth E, Pedersen PH, Varughese JK, Chaudhry AA et al (2013) Conservative management or gamma knife radiosurgery for vestibular schwannoma: tumor growth, symptoms, and quality of life. Neurosurgery. 73(1):48–56 discussion 56-57
Carlson ML, Link MJ, Wanna GB, Driscoll CLW (2015) Management of sporadic vestibular schwannoma. Otolaryngol Clin N Am 48(3):407–422
Chao ST, Thakkar VV, Barnett GH, Vogelbaum MA, Angelov L, Weil RJ, Rasmussen P, Reuther AM, Jamison B, Neyman G, Suh JH (2012) Prospective study of the short-term adverse effects of gamma knife radiosurgery. Technol Cancer Res Treat 11(2):117–122
Chopra R, Kondziolka D, Niranjan A, Lunsford LD, Flickinger JC (2007) Long-term follow-up of acoustic schwannoma radiosurgery with marginal tumor doses of 12 to 13 Gy. Int J Radiat Oncol Biol Phys 68(3):845–851
Chung W-Y, Liu K-D, Shiau C-Y, Wu H-M, Wang L-W, Guo W-Y et al (2005) Gamma knife surgery for vestibular schwannoma: 10-year experience of 195 cases. J Neurosurg 102(Suppl):87–96
Di Maio S, Akagami R (2009) Prospective comparison of quality of life before and after observation, radiation, or surgery for vestibular schwannomas. JNS. 111(4):855–862
Foote KD, Friedman WA, Buatti JM, Meeks SL, Bova FJ, Kubilis PS (2001) Analysis of risk factors associated with radiosurgery for vestibular schwannoma. J Neurosurg 95(3):440–449
Golfinos JG, Hill TC, Rokosh R, Choudhry O, Shinseki M, Mansouri A et al (2016) A matched cohort comparison of clinical outcomes following microsurgical resection or stereotactic radiosurgery for patients with small- and medium-sized vestibular schwannomas. JNS. 125(6):1472–1482
Gormley WB, Sekhar LN, Wright DC, Kamerer D, Schessel D (1997) Acoustic neuromas: results of current surgical management. Neurosurgery. 41(1):50–58 discussion 58-60
Hansasuta A, Choi CYH, Gibbs IC, Soltys SG, Tse VCK, Lieberson RE, Hayden MG, Sakamoto GT, Harsh GR 4th, Adler JR Jr, Chang SD (2011) Multisession stereotactic radiosurgery for vestibular schwannomas: single-institution experience with 383 cases. Neurosurgery. 69(6):1200–1209
Haque R, Wojtasiewicz TJ, Gigante PR, Attiah MA, Huang B, Isaacson SR et al (2011) Efficacy of facial nerve–sparing approach in patients with vestibular schwannomas. JNS. 115(5):917–923
Kano H, Kondziolka D, Khan A, Flickinger JC, Lunsford LD (2009) Predictors of hearing preservation after stereotactic radiosurgery for acoustic neuroma. J Neurosurg 111(4):863–873
Kim K-M, Park C-K, Chung H-T, Paek SH, Jung H-W, Kim DG (2007) Long-term outcomes of gamma knife stereotactic radiosurgery of vestibular schwannomas. J Korean Neurosurg Soc 42(4):286–292
Klijn S, Verheul JB, Beute GN, Leenstra S, Mulder JJS, Kunst HPM, Hanssens PE (2016) Gamma knife radiosurgery for vestibular schwannomas: evaluation of tumor control and its predictors in a large patient cohort in the Netherlands. J Neurosurg 124(6):1619–1626
Kondziolka D, Lunsford LD, McLaughlin MR, Flickinger JC (1998) Long-term outcomes after radiosurgery for acoustic neuromas. N Engl J Med 339(20):1426–1433
Kondziolka D, Mousavi SH, Kano H, Flickinger JC, Lunsford LD (2012) The newly diagnosed vestibular schwannoma: radiosurgery, resection, or observation? Neurosurg Focus 33(3):E8
Leksell L (1971) A note on the treatment of acoustic tumours. Acta Chir Scand 137(8):763–765
Link MJ, Driscoll CLW, Foote RL, Pollock BE (2012) Radiation therapy and radiosurgery for vestibular schwannomas. Otolaryngol Clin N Am 45(2):353–366
Litvack ZN, Norén G, Chougule PB, Zheng Z (2003) Preservation of functional hearing after gamma knife surgery for VS. Neurosurg Focus 14(5):e3
Lunsford LD, Niranjan A, Flickinger JC et al (2005) Radiosurgery of vestibular schwannomas: summary of experience in 829 cases. J Neurosurg 102:195–199
Meijer OWM, Vandertop WP, Baayen JC, Slotman BJ (2003) Single-fraction vs. fractionated linac-based stereotactic radiosurgery for VS: a single-institution study. Int J Radiat Oncol Biol Phys 56(5):1390–1396
Mulkens TH, Parizel PM, Martin JJ, Degryse HR, Van de Heyning PH, Forton GE et al (1993) Acoustic schwannoma: MR findings in 84 tumors. Am J Roentgenol 160(2):395–398
Murphy ES, Barnett GH, Vogelbaum MA, Neyman G, Stevens GHJ, Cohen BH, Elson P, Vassil AD, Suh JH (2011) Long-term outcomes of gamma knife radiosurgery in patients with vestibular schwannomas. J Neurosurg 114(2):432–440
Muzevic D, Legcevic J, Splavski B, Cayé-Thomasen P (2014) Stereotactic radiotherapy for vestibular schwannoma. Cochrane ENT Group, editor. Cochrane Database Syst Rev [Internet] [cited 2019 Sept 25]; Available from: http://doi.wiley.com/10.1002/14651858.CD009897.pub2
Myrseth E, Møller P, Pedersen PH, Lund-Johansen M (2009) Vestibular schwannoma: surgery or gamma knife radiosurgery? A prospective, nonrandomized study. Neurosurgery 64(4):654–663
Pollock BE, Link MJ, Foote RL (2009) Failure rate of contemporary low-dose radiosurgical technique for vestibular schwannoma. J Neurosurg 111(4):840–844
Pollock BE, Driscoll CL, Foote RL et al (2006) Patient outcomes after vestibular schwannoma management: a prospective comparison of microsurgical resection and stereotactic radiosurgery. Neurosurgery. 59:77–85 discussion 77-85
Régis J, Tamura M, Delsanti C, Roche P-H, Pellet W, Thomassin J-M (2008) Hearing preservation in patients with unilateral vestibular schwannoma after gamma knife surgery. Prog Neurol Surg 21:142–151
Saadatmand HJ, Wu C-C, Wang TJC (2016) Interdisciplinary management of acoustic neuromas. Appl Radiat Oncol 5(1):5–16
Schnurman Z, Nakamura A, McQuinn MW, Golfinos JG, Roland JT, Kondziolka D (2019) Volumetric growth rates of untreated vestibular schwannomas. J Neurosurg 2:1–7
Smith DR, Saadatmand HJ, Wu C-C, Black PJ, Wuu Y-R, Lesser J, Horan M, Isaacson SR, Wang TJC, Sisti MB (2019) Treatment outcomes and dose rate effects following gamma knife stereotactic radiosurgery for vestibular schwannomas. Neurosurgery. 85(6):E1084–E1094
Timmer FCA, Hanssens PEJ, van Haren AE, van Overbeeke JJ, Mulder JJS, Cremers CWRJ, Graamans K (2011) Follow-up after gamma knife radiosurgery for vestibular schwannomas: volumetric and axial control rates. Laryngoscope. 121(7):1359–1366
Tsao MN, Sahgal A, Xu W, De Salles A, Hayashi M, Levivier M et al (2017) Stereotactic radiosurgery for vestibular schwannoma: International Stereotactic Radiosurgery Society (ISRS) practice guideline. J Radiosurg SBRT 5(1):5–24
Vulpe H, Save AV, Xu Y, Elliston CD, Garrett MD, Wu C-C et al (2019) Frameless stereotactic radiosurgery on the gamma knife icon: early experience from 100 patients. Neurosurgery https://doi.org/10.1093/neuros/nyz227
Williams JA (2002) Fractionated stereotactic radiotherapy for acoustic neuromas. Acta Neurochir 144(12):1249–1254 discussion 1254
Yang I, Sughrue ME, Han SJ, Aranda D, Pitts LH, Cheung SW et al (2010) A comprehensive analysis of hearing preservation after radiosurgery for vestibular schwannoma. J Neurosurg 112(4):851–859
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Dr. Wang reports personal fees and non-financial support from AbbVie, personal fees from AstraZeneca, personal fees from Cancer Panels, personal fees from Doximity, personal fees and non-financial support from Elekta, personal fees and non-financial support from Merck, personal fees and non-financial support from Novocure, personal fees and non-financial support from RTOG Foundation, personal fees from Rutgers, personal fees from University of Iowa, personal fees from Wolters Kluwer, outside the submitted work.
Ethical approval
Not applicable.
Informed consent
Not applicable.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Buss, E.J., Wang, T.J.C. & Sisti, M.B. Stereotactic radiosurgery for management of vestibular schwannoma: a short review. Neurosurg Rev 44, 901–904 (2021). https://doi.org/10.1007/s10143-020-01279-2
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10143-020-01279-2