Abstract
The lateral supraorbital (LSO) approach is a minimally invasive modification of the pterional approach. The authors assess the surgical indications and esthetic benefits of the LSO approach in comparison with the pterional approach for parachiasmal meningiomas. From April 2013 to May 2017, a total of 64 patients underwent surgery for parachiasmal meningiomas. Among them, tumor resection was performed with the LSO approach for 34 patients and pterional approach for 30 patients. A retrospective analysis was done on tumor characteristics, surgical outcome, approach-related morbidity, and esthetic outcome between the two approaches. Gross total resection was achieved in 33 of 34 patients (97.1%) with the LSO approach. There were no differences in tumor size, origin, consistency, internal carotid artery encasement, cranial nerve adhesion, and optic canal invasion between the two approaches. The most common tumor origin was the tuberculum sellae for both the LSO and pterional approaches. For tumors with preoperative visual compromise, immediate visual outcome improved or remained stable in 76% and 80.9% with the LSO and pterional approaches, respectively. Surgery time, surgical bleeding, hospital length of stay, and esthetic outcome were significantly shorter and superior with the LSO approach. There were no differences in surgical morbidity and brain retraction injury between the two approaches. The LSO approach can provide a safe, rapid, and minimally invasive exposure for parachiasmal meningiomas compared with the pterional approach. Surgeons must consider tumor size, origin, and extent in determining the resectability of the tumor rather than the extent of exposure.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The standard pterional approach is the most basic, familiar, and widely used approach to neurosurgeons. It offers a wide surgical field and access to vascular and neoplastic lesions in the parachiasmal region. However, the pterional approach for parachiasmal tumors can be extensive, invasive with a long surgery time, and postoperative cosmetic problems [6, 23,24,25]. Temporalis muscle atrophy and facial nerve dysfunction from extensive manipulation of the temporalis muscle have been suggested with the pterional approach [1, 3, 4, 12]. In the era of minimally invasive approaches, several surgical alternatives have been proposed to overcome these issues [2, 12, 13, 22, 31]. The lateral supraorbital (LSO) approach described by Hernesniemi et al. [14] is one such approach that is a less invasive modification of the pterional approach without the temporal extension. This modified technique can access vascular and neoplastic lesions located in the sellar, parasellar, suprasellar, and retrosellar regions. The approach has also shown its possibility as a reasonable alternative to the pterional approach for meningiomas with parachiasmal origin and location such as the tuberculum sellae, olfactory groove, planum sphenoidalis, and anterior clinoid process [23,24,25]. The main advantages of an LSO approach compared with a pterional approach would be in a shorter, less invasive skin incision that causes less trauma to the temporalis muscle and facial nerve. This, in turn, leads to a shorter surgery time and bleeding for the surgeon, and reduced hospital length of stay and incision scar for the patient [6, 19, 23,24,25, 27].
The purpose of this study was to assess the indications, surgical outcome, approach-related morbidity and esthetic outcome, and limitations of the LSO approach in comparison with the standard pterional approach for parachiasmal meningiomas.
Methods
Patient population
From April 2013 to May 2017, 64 consecutive patients underwent surgery for meningiomas with parachiasmal origin and location by two neurosurgeons (C.K.H and J.H.C) with extensive experience in the surgical management of meningiomas. The inclusion criteria of the patients enrolled in the study were as follows: (1) meningiomas with parachiasmal origin including the tuberculum sellae, anterior clinoid process (ACP), olfactory groove, planum sphenoidalis, frontal base, and the dorsum sellae, (2) parachiasmal meningiomas located anterior and above the Sylvian cistern without extension into the middle cranial fossa, (3) patients with a postoperative follow-up period of more than 12 months, and (4) patients with data regarding approach-related esthetic outcome, surgery time for approach, surgery time from skin-to-skin, surgical bleeding, and hospital length of stay. Thirty-four patients were underwent surgery with the LSO approach and 30 patients with the standard pterional approach. The LSO approach was first introduced to our institution in 2016. Before the advent of the LSO approach, parachiasmal meningiomas were resected by pterional or subfrontal interhemispheric approaches. Medical records and tumor registry of the patients were reviewed for demographic data, tumor characteristics, intraoperative surgical data, surgical outcome, approach-related esthetic outcome, preoperative and postoperative imaging, and postoperative morbidity. The data was analyzed retrospectively after obtaining informed consent from every patient. The study was approved by the institutional review board and conducted in accordance with the ethical guidelines of the Declaration of Helsinki.
Surgical technique and indication
Lateral supraorbital approach
The lateral supraorbital (LSO) approach was performed in the same manner as described by Hernesniemi et al. [14]. The patient is positioned in supine and the head fixed with a three-pin Mayfield head holder, elevated above the heart, and rotated to the contralateral side by 30–45°. The skin incision is located right behind the hair line, starting above the pinna and extending medially within the hairline towards a mid-point between the superior temporal line and midline (Fig. 1). After the skin incision, only a small portion of the superior and anterior temporalis muscle is cut and retracted to expose the bone. Then, a small burr hole is drilled on McCarty’s keyhole that simultaneously exposes the anterior cranial fossa floor and the orbit. The burr hole is extended posteriorly towards the sphenoid ridge with a match head drill tip. The posteroinferior margin of the bone flap does not extend beyond the sphenoid ridge. A small, semilunar shaped bone flap with the keyhole at the center of the inferior margin is made with a craniotome. The anteroinferior margin of the bone flap can be tailored according to the extent of surgical viewing required on the contralateral side, but does not extend beyond the supraorbital notch. After the craniotomy, the orbital roof is flattened with an acorn drill tip. Extradural anterior clinoidectomy can be performed as needed. The dura is opened in a semilunar shape and the Sylvian cistern can be opened for cerebrospinal fluid (CSF) drainage. For tumors with optic canal invasion, opening of the falciform ligament is done in every case to remove the tumor at the entrance of the optic canal. Unroofing of the optic canal is performed with a diamond drill, only when tumor extension into the optic canal is evident after opening the falciform ligament. Extradural anterior clinoidectomy is performed in selective cases to gain additional corridor into the carotid-optic space. After tumor resection, cranial mini-plates can be used to fix the bone flap back into its place with minimal craniectomy defect.
Step-by-step procedures of a left lateral supraorbital (LSO) approach. The skin incision of the LSO approach is shorter than the pterional approach and does not extend towards the midline or below the pinna. The incision is always hidden behind the hairline. The bone flap of the LSO approach has the McCarty’s keyhole (black dot) at the center of the inferior margin and does not extend beyond the sphenoid ridge (black triangle) (a). After the skin incision, only a small portion of the superior and anterior temporalis muscle is cut and retracted to expose the bone. Then, a small, semilunar shaped bone flap with the keyhole at the center of the inferior margin is made. The posteroinferior margin of the bone flap does not extend beyond the sphenoid ridge (b). After the craniotomy, the orbital roof is flattened with a drill to minimize brain retraction (c). The dura is also opened in a semilunar shape (d). To reduce further brain retraction, the Sylvian cistern can be opened for cerebrospinal fluid (CSF) drainage (e)
Indication of LSO approach
The range of microscopic surgical view of the LSO approach for normal anatomic structures is as follows: anteriorly, the olfactory groove, planum sphenoidalis, and tuberculum sellae; laterally, the ipsilateral internal carotid artery (ICA), optic nerve, and ACP, medially, the contralateral optic nerve, and posteriorly, the pituitary stalk (Fig. 2). The microscopic surgical window of the anterior cranial fossa with an LSO approach resembles the window of a pterional approach. In general, the LSO approach is a good candidate for (1) neoplastic lesions located anterior and above the Sylvian cistern, (2) parachiasmal meningiomas originating from the tuberculum sellae, olfactory groove, and ACP, (3) parachiasmal meningiomas without cavernous sinus (CS) invasion, and (4) pituitary stalk lesions requiring biopsy (Fig. 3) [6, 23,24,25,26]. The LSO approach is a reasonable alternative to the standard pterional approach for lesions located at the anterior cranial fossa without significant temporal extension.
A visual comparison of the microscopic operative view of a left LSO (a–d) and pterional approach (e–h) for a tuberculum sellae meningioma. The following normal anatomic structures can be seen after opening the Sylvian cistern (SC) for CSF drainage (a and e): Anteriorly, the olfactory groove (OG), planum sphenoidalis (PS), and tuberculum sellae (TS) (b and f). Laterally, the ipsilateral internal carotid artery (ICA), optic nerve (ON), and anterior clinoid process (ACP) (c and g). Medially, the contralateral optic nerve and posteriorly, the pituitary stalk (black arrow) (d and h)
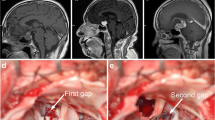
The surgical range (yellow circles) and maximal border (red dotted lines) of the LSO approach shown on T2 axial (a), sagittal (b), and coronal (c) magnetic resonance (MR) images. Preoperative and 1-year postoperative gadolinium-enhanced T1-weighted axial, sagittal, and coronal MR images: Simpson resection grade I was achieved with a left LSO approach for a tuberculum sellae meningioma with bilateral optic canal invasion and optic nerve adhesion (d–i). Simpson resection grade I was achieved with a left LSO approach for a large, olfactory groove meningioma with moderate consistency and bilateral olfactory nerve adhesion (j–o). Simpson resection grade I was achieved with a right LSO approach for an ACP meningioma with ipsilateral ICA encasement and optic canal invasion (p–u). All, three tumors did not extend beyond the Sylvian cistern
Data interpretation
All patients underwent a complete radiologic workup with thin-sectioned computed tomography (CT) and magnetic resonance imaging (MRI) scans including T2-weighted and gadolinium-enhanced T1-weighted axial, coronal, and sagittal images acquired at 3-mm or 1-mm intervals. The imaging studies were obtained before surgery, within 48 h after surgery, annually for the first 2 years, and every 2 to 3 years thereafter. All performed images were interpreted by two neuroradiologists who were blinded to patient information. Tumor size was defined as the largest diameter on an axial MR image. Extent of resection (EOR) was classified into gross total resection (GTR), subtotal resection (STR), and biopsy. GTR was defined as grossly complete tumor removal with no evidence of residual tumor on immediate postoperative MRI. STR was defined as the presence of residual tumor on immediate postoperative MRI. The intention of the surgery was GTR if the tumor was fully visible and under control by the surgeon. Intentional STRs were performed for tumors with CS invasion. Preoperative brain edema and postoperative brain retraction injury were determined by comparing the change of white matter signal intensity adjacent to the tumor on T2-weighted MR images. Surgery time for the approach was defined as the time from skin incision to dural opening and from dural closure to skin closure. Surgery time from skin-to-skin was defined as the time from skin incision to skin closure. Surgical bleeding included the total amount of blood lost by the patient during the entire surgery. Hospital length of stay was defined as the number of in-hospital days from the day of surgery to the day of discharge. For patients with preoperative visual compromise, visual outcome was interpreted as improved, stable, or aggravated depending on the change of visual acuity and visual field as previously described [21]. Approach-related esthetic outcome entailed an outpatient clinic survey on the patient’s incision site and mastication discomfort, supraorbital hypoesthesia, facial nerve palsy, temporalis muscle atrophy, bony defect, visible scar outside the hairline, and cosmetic satisfaction. The mean follow-up period was 24.1 months (range, 12.3–56.2 months).
Statistical analysis
Characteristics of the patients, tumors, and surgical outcome between the LSO and pterional approaches were compared by using Mann-Whitney U test. A Fischer’s exact test was used to compare categorical variables. Data analyses were performed using SPSS software version 18.0 for Windows (SAS Institute, Inc.). Two-tailed and p values of p ≤ 0.05 were considered statistically significant.
Results
Patient and tumor characteristics
There were 50 female (78.1%) and 14 male (21.9%) patients with a mean age of 53 years (range, 29–80 years). The most common presenting symptom was visual impairment (48.4%), followed by incidentally found on health check-up (26.6%). The mean largest diameter of the tumors was 2.7 cm (range, 1.0–5.5 cm). The local disease status at the time of surgery was primary in 62 patients (96.9%), recurrent after surgery in 1 patient (1.6%), and residual after surgery in 1 patient (1.6%). The most common meningioma histology was meningothelial (60.9%), followed by transitional (28.1%), psammomatous (4.7%), atypical (3.1%), and secretory (1.6%).
Tumor resection was performed with the LSO approach for 34 patients (53.1%) and with the standard pterional approach for 30 patients (46.9%). The most common tumor origin for the LSO approach was the tuberculum sellae (70.6%), followed by ACP (11.8%), olfactory groove (5.9%), planum sphenoidalis (5.9%), frontal base (2.9%), and dorsum sellae (2.9%). The tuberculum sellae (66.7%) and ACP (30%) were the most common tumor origin for the pterional approach. There were no differences in preoperative brain edema; CS invasion of the tumor; local disease status at the time of surgery, tumor size, origin, histology, and consistency; and ICA encasement, cranial nerve adhesion, and optic canal invasion of the tumor between the two approaches (Table 1).
Surgical outcome
The mean surgery time for the approach was significantly shorter with the LSO (106.9 min) compared with the pterional approach (147.6 min) (p < 0.01). This subsequently led to significant differences with the mean surgery time from skin-to-skin (274.9 min for the LSO and 390.6 min for the pterional approach) (p < 0.01), surgical bleeding (356 mL for the LSO and 537 mL for the pterional approach) (p = 0.014), and hospital length of stay (9.9 days for the LSO and 13.1 days for the pterional approach) (p < 0.01) between the two approaches. Gross total resection was achieved in 33 of 34 patients (97.1%) with the LSO approach and in 29 of 30 patients (96.7%) with the pterional approach. The Simpson resection grades were a mean 1.4 ± 0.8 and 1.5 ± 0.7 (median grade 1 with interquartile ranges of grade 1) for the LSO and pterional approaches, respectively. There were no differences in the GTR rate (p = 0.722) and the Simpson resection grade (p = 0.137) between the two approaches. For tumors with visual compromise, vision improved or remained stable before discharge in 76% and 80.9% of the patients with the LSO and pterional approaches, respectively (p = 0.722). There were no differences in brain retraction injury observed on postoperative T2-weighted MR images (p = 0.757) and surgical morbidity (p = 0.616) between the two approaches.
Transient surgical morbidity occurred in 3 patients (8.8%) with the LSO approach. All 3 patients had complications related to severe tumor adherence with the cranial nerves. One patient had anosmia from olfactory nerve dysfunction, another patient had bitemporal hemianopsia from optic nerve dysfunction, and the last patient had incomplete ptosis from occulomotor nerve dysfunction. All 3 patients recovered promptly after short-term administration of oral prednisolone. There was transient surgical morbidity in 2 patients (6.7%) with the pterional approach. One patient had CS invasion of the tumor with consequent occulomotor nerve palsy from the manipulation of the tumor inside CS. Another patient had incomplete ptosis from severe tumor adhesion with the occulomotor nerve. The 2 patients also recovered soon with short-term oral prednisolone administration. There were no tumor regrowth or recurrences, regardless of the surgical approach during the study period.
Approach-related morbidity and esthetic outcome
For approach-related morbidity, CSF leak, wound infection/dehiscence, supraorbital hypoesthesia, mastication discomfort, and facial nerve palsy occurred in none of the patients with the LSO approach and in 0%, 3.3%, 3.3%, 6.7%, and 0% of the patients with the pterional approach (Table 2). There was 1 patient (2.9%) in the LSO group with inadvertent frontal sinus opening and 2 patients (6.7%) in the pterional group. Incision site discomfort other than numbness occurred in 2 (5.9%) and 5 patients (16.7%) with the LSO and pterional approaches, respectively. For approach-related esthetic outcome, none of the patients with the LSO approach had temporalis muscle atrophy, bony defect, or visible scar outside the hairline and 94.1% of the patients were completely satisfied with their cosmetic outcome. There were mild, moderate, and pronounced temporalis muscle atrophy in 3 (10%), 2 (6.7%), and 1 patients (3.3%) with the pterional approach, respectively. Bony defect from skull depression and protrusion also occurred in 2 (6.7%) and 1 patients (3.3%) with the pterional approach, respectively. Twenty-five out of 30 patients (83.3%) in the pterional group had a visible scar outside the hairline, in front of the tragus. Consequently, only 66.7% of the patients with the pterional approach were fully satisfied with their esthetic outcome.
Discussion
The pterional approach was first described by Dandy [8, 9] in 1938, and later perfected and popularized by Yarsargil in 1984 [28,29,30]. The approach offers a wide surgical field and access to vascular and neoplastic lesions of the anterior and middle cranial fossa. It can also be modified and extended for various skull base approaches such as the orbitozygomatic and anterior petrosal approaches. The authors also used the pterional approach for various sellar, suprasellar, and retrosellar neoplastic lesions for over 20 years. However, the standard pterional approach for parachiasmal meningiomas limited in the anterior cranial fossa can be extensive and invasive with a long surgery time and postoperative cosmetic problems [6, 23,24,25]. Temporalis muscle atrophy, dysfunction of the temporal branch of the facial nerve, and tedious reconstruction of the temporal base are also drawbacks of the approach related to the exposure of the temporal lobe [1, 3, 4, 12]. In the era of minimally invasive surgery, supraorbital approach [22, 31], extended endoscopic endonasal approach [16, 17], mini-pterional approach [12], and LSO approach [6, 23,24,25,26] can be reasonable alternatives for parachiasmal tumors limited in the anterior cranial fossa. Unfortunately, the supraorbital approach has a narrow corridor requiring specially designed tube-shaft instruments with the risk of a postoperative scar on the face and damage to the facial nerve [29]. The extended endoscopic endonasal approach is becoming very popular, but requires a dedicated learning period to get used to an endoscope and the burden of a postoperative CSF leak [18, 20]. The skin incision of mini-pterional approach is similar to the LSO approach, but the bone flap is centered around the sphenoid ridge and smaller than the LSO approach [22]. On the contrary, the LSO approach is easy and can be done by any neurosurgeon with the knowledge and instruments adequate for the pterional approach. Among several minimally invasive approaches for parachiasmal meningiomas, the authors focused on the surgical indications, strengths, and weakness of the LSO approach in comparison with the standard pterional approach.
The main benefits of the LSO approach over the standard pterional approach are in the shorter surgery time and less intraoperative blood loss. It took the authors a mean 106.9 min from skin incision to dural opening and from dural closure to skin closure with the LSO approach, compared with a mean 147.6 min with the pterional approach. In capable hands, surgery time excluding tumor resection has been reported to take less than 30 min [23,24,25]. A shorter skin incision within the hairline and a smaller bone flap of the LSO approach not only help reduce surgery time, but also reduce intraoperative blood loss by more than one-thirds of the pterional approach. This, in turn, contributes to a significantly faster recovery, shorter hospital length of stay and satisfactory cosmetic results as shown by the results of this study [6, 19, 23,24,25, 27]. None of the patients with the LSO approach had an approach-related morbidity such as CSF leak, wound infection/dehiscence, supraorbital hypoesthesia, and mastication discomfort. Other than the 2 patients with mild incision site discomfort, 94.1% of the patients with the LSO approach were satisfied with their esthetic outcome without any temporalis muscle atrophy, bony defect, or visible scar outside the hairline. On the other hand, a small number of patients with the pterional approach had approach-related morbidities that consequently led to a lower cosmetic satisfaction rate of 66.7%. A longer skin incision that extends outside the hairline, in front of the tragus, temporalis muscle manipulation, bigger bone flap, and sphenoid ridge drilling were the procedures that contributed to a lower functional and esthetic satisfaction. The temporalis muscle can sustain injury during muscle manipulation and split which can lead to direct muscle fiber injury, denervation, and vascular disruption [1, 3, 4, 12]. Consequent injury results in mastication discomfort, facial nerve palsy, delayed temporalis muscle atrophy, and unsatisfactory cosmetic results. Various surgical tips had been proposed to avoid temporalis muscle injury, which have significantly reduced the incidence of facial nerve palsy [1, 5, 7, 10,11,12, 15]. However, even in capable hands, mild to pronounced temporalis muscle atrophy occurred in up to 20% of our patients with the pterional approach [27]. Significant temporalis muscle manipulation is inevitable with the pterional approach, whereas the LSO approach reduces the risk of muscle atrophy by only splitting the superior and anterior part of the muscle, preserving the nerve and vascular supply.
Then, aside from a shorter surgery time, less intraoperative blood loss, and satisfactory cosmetic results, what are the indications of the LSO approach? Experienced surgeons know that tumor-related factors are crucial in determining the resectability of the tumor rather than the extent of exposure. In this series, there were no differences in the local disease status at the time of surgery, tumor origin, histology, and consistency, and ICA encasement, cranial nerve adhesion, and optic canal invasion of the tumor between the LSO and pterional approaches. And yet, no differences could be found in postoperative brain retraction injury, surgical morbidity, and visual outcome for tumors with visual compromise between the two approaches. Excessive brain retraction could be anticipated with a smaller bone flap and surgical window, but there was no difference between the two approaches. The authors believe that the LSO approach can enhance its benefits when it is used accordingly. In general, the LSO approach is a good candidate for (1) neoplastic lesions located anterior and above the Sylvian cistern, (2) parachiasmal meningiomas originating from the tuberculum sellae, olfactory groove, and ACP, (3) parachiasmal meningiomas without CS invasion, and (4) pituitary stalk lesions requiring biopsy. The surgical field of the LSO approach provides access to the olfactory groove, planum sphenoidalis, and tuberculum sellae, anteriorly; the ipsilateral ICA, optic nerve, and ACP, laterally; the contralateral optic nerve, medially; and the pituitary stalk and dorsum sellae, posteriorly. For tumors with optic canal invasion, the LSO approach did not hinder performing surgical procedures such as unroofing of the optic canal or extradural anterior clinoidectomy. The GTR rate was comparable between the LSO (97.1%) and pterional approach (96.7%). The LSO approach showed its possibility as a reasonable alternative to the pterional approach for parachiasmal meningiomas excluding those, in which the intention of the surgery was STR from CS invasion of the tumor. The microscopic surgical window and resectability of an LSO approach for parachiasmal meningiomas was feasible as a pterional approach without the need for temporal lobe or middle cranial fossa exposure.
It is true that the simple observation of an anatomic structure does not correlate with the resectability and maneuverability on the same structure. According to a study with cadavers, the volume and shape of the surgical exposure were more favorable to the extent of resection with the pterional approach than the LSO approach [26]. There are even more factors to consider such as tumor characteristics and surgeon’s ability when it comes to in vivo operability. Among tumor-related factors, tumor origin and extent were the most important aspects in deciding whether the LSO approach could be used. Tumors originating or extending lateral or beneath the Sylvian cistern and tumors with CS invasion were not good candidates for the LSO approach. With tumor size, it was not easy to define an indication for the LSO approach. In this study, there was no difference in tumor size between the LSO and pterional approaches. A tumor with the largest diameter of 5.5 cm could be resected completely with the LSO approach. The cisterns can be opened for CSF drainage to minimize brain retraction in large tumors with preoperative brain edema. However, the Sylvian exposure of the LSO approach after opening the dura is limited only to the level of limen insula which requires gentle retraction of the frontal lobe at the beginning. The suprachiasmatic and carotid cisterns need even more frontal lobe retraction which could be difficult for large tumors with significant preoperative brain edema.
For tumors with visual compromise, there was no difference in visual outcome before discharge between the LSO and pterional approaches. However, it is still disturbing to find that visual field and acuity aggravated among 24% and 19% of the patients with the LSO and pterional approaches, respectively. The authors have found out that abnormal and thin preoperative retinal nerve fiber layer thickness induced by compressive optic neuropathy in parachiasmal meningiomas was responsible for the postoperative visual deterioration in all of these patients, and not the approach itself [21].
There were 3 patients with transient surgical morbidity after tumor resection with the LSO approach. Each deficit was related to severe tumor adherence with olfactory, optic, and occulomotor cranial nerves. The authors feel that olfactory and optic nerve dysfunctions would have been the same, regardless of the surgical approach, but different for occulomotor dysfunction. The LSO approach can access the optico-carotid corridor as equally as the pterional approach, but not so with the carotid-occulomotor corridor [26]. The LSO approach has a cylindrical work space with a surgical access directed more anteriorly compared with a pyramidal work space of the pterional approach with a more lateral surgical trajectory. In addition, the pterional approach has a larger working space, increased operability, and early access to the Sylvian and carotid cisterns than the LSO approach. Nevertheless, an LSO approach can have a reasonable operative view and resectability as a pterional approach without unnecessary temporal lobe exposure and temporalis muscle manipulation if it is used according to appropriate surgical indications.
Limitations
The limitations of this study are in the small number of patients which makes it difficult to draw a definitive surgical indication for the LSO approach. In addition, the follow-up period of the patients may not have been long enough to seek the difference in surgical outcome between the two approaches. There are also several clinical papers and cadaveric studies [26] in literature highlighting the advantages of the LSO approach over the standard pterional approach for anterior circulation aneurysms [19, 27] and parachiasmal tumors [6, 23,24,25]. These papers provide valuable data on what, when, how, and why the LSO should be used. However, none of reported studies directly compare the surgical outcome, approach-related morbidity, and esthetic outcome between the LSO and pterional approaches for parachiasmal meningiomas. The main purpose of this study was to find out if the LSO approach could be an alternative to the pterional approach without the esthetic compromise for parachiasmal meningiomas. The strengths and weaknesses of the two approaches were explored through an apples-to-apples comparison to summarize and suggest the tumor-related factors that can influence the selection of the surgical approach. The authors believe that one surgical approach cannot be superior to another. Instead, a surgical approach should be tailored and selected according to the characteristics of the tumor. The ability to choose the LSO approach appropriately will only be established after exploring the surgical indications and limitations of the approach.
Conclusion
The LSO approach can provide a safe, rapid, and minimally invasive exposure for parachiasmal meningiomas. It can be a reasonable alternative to the pterional approach for neoplastic lesions located anterior and above the Sylvian cistern without CS invasion. Instead of using a “one size fits all” craniotomy, surgeons must consider tumor-related factors in determining the resectability of the tumor rather than the extent of exposure.
References
Ammirati M, Spallone A, Ma J, Cheatham M, Becker D (1994) Preservation of the temporal branch of the facial nerve in pterional-transzygomatic craniotomy. Acta Neurochir 128:163–165
Andaluz N, Romano A, Reddy LV, Zuccarello M (2008) Eyelid approach to the anterior cranial base. J Neurosurg 109:341–346
Aydin IH, Takci E, Kadioglu HH, Kayaoglu CR, Tuzun Y (1995) Pitfalls in the pterional approach to the parasellar area. Minim Invasive Neurosurg 38:146–152
Badie B (1996) Cosmetic reconstruction of temporal defect following pterional craniotomy. Surg Neurol 45:383–384
Barone CM, Jimenez DF, Boschert MT (2001) Temporalis muscle resuspension using titanium miniplates and screws: technical note. Neurosurgery 48:450–451
Chen G, Wang Z, Zhou D (2013) Lateral supraorbital approach applied to sellar tumors in 23 consecutive patients: the Suzhou experience from China. World J Surg Oncol 21:11–41
Coscarella E, Vishteh AG, Spetzler RF, Seoane E, Zabramski JM (2000) Subfascial and submuscular methods of temporal muscle dissection and their relationship to the frontal branch of the facial nerve. Technical note. J Neurosurg 92:877–880
Dandy W (1938) Hirnchirurgie. Springer, Germany
Dandy W (1938) Intracranial aneurysm of the internal carotid artery. Cured by operation. Ann Surg 107:654–659
de Andrade FC Jr, de Andrade FC, de Araujo Filho CM, Filho JC (1998) Dysfuntion of the temporalis muscle after pterional craniotomy for intracranial aneurysms. Comparative, prospective and randomized study of one flap versus two flaps dieresis. Arq Neuropsiquiatr 56:200–205
Figueiredo EG, Deshmukh P, Zabramski JM, Preul MC, Crawford NR, Spetzler RF (2006) The pterional-transsylvian approach: an analytical study. Neurosurgery 59(4 Suppl 2):ONS263–ONS269
Figueiredo EG, Deshmukh P, Nakaji P, Crusius MU, Crawford N, Spetzler RF, Preul MC (2007) The minipterional craniotomy: technical description and anatomic assessment. Neurosurgery 61:256–264
Harland SP, Hussein A, Gullan RW (1996) Modification of the standard pterional approach for aneurysms of the anterior circle of Willis. Br J Neurosurg 10:149–153
Hernesniemi J, Ishii K, Niemela M, Smrcka M, Kivipelto L, Fikiki M, Shen H (2005) Lateral supraorbital approach as an alternative to the classical pterional approach. Acta Neurochir Suppl 94:17–21
Hwang SW, Abozed MM, Antoniou AJ, Malek AM, Heilman CB (2010) Postoperative temporalis muscle atrophy and the use of electrocautery: a volumetric MRI comparison. Skull Base 20:321–326
Komotar RJ, Starke RM, Raper DM, Anand VK, Schwartz TH (2012) Endoscopic endonasal versus open transcranial resection of anterior midline skull base meningiomas. World Neurosurg 77:713–724
Koutourousiou M, Fernandez-Miranda JC, Stefko ST, Wang EW, Snyderman CH, Gardner PA (2014) Endoscopic endonasal surgery for suprasellar meningiomas: experience with 75 patients. J Neurosurg 120:1326–1339
Kulwin C, Schwartz TH, Cohen-Gadol AA (2013) Endoscopic extended transsphenoidal resection of tuberculum sellae meningiomas: nuances of neurosurgical technique. Neurosurg Focus 35(6):E6
La Rocca G, Della Pepa GM, Sturiale CL, Sabatino G, Auricchio AM, Puca A, Olivi A, Marchese E, Albanese A (2018) Lateral supraorbital versus pterional approach: analysis of surgical, functional, and patient-oriented outcomes. World Neurosurg 119:e192–e199
Liu JK, Christiano LD, Patel SK, Tubbs RS, Eloy JA (2011) Surgical nuances for removal of olfactory groove meningiomas using the endoscopic endonasal transcribriform approach. Neurosurg Focus 30(5):E3
Park HH, Oh MC, Kim EH, Kim CY, Kim SH, Lee KS, Chang JH (2015) Use of optical coherence tomography to predict visual outcome in parachiasmal meningioma. J Neurosurg 123:1489–1499
Reisch R, Perneczky A, Filippi R (2003) Surgical technique of the supraorbital key-hole craniotomy. Surg Neurol 59:223–227
Romani R, Lehecka M, Gaal E, Toninelli S, Celik O, Niemela M, Porras M, Jaaskelainen J, Hernesniemi J (2009) Lateral supraorbital approach applied to olfactory groove meningiomas: experience with 66 consecutive patients. Neurosurgery 65:39–52
Romani R, Laakso A, Kangasniemi M, Lehecka M, Hernesniemi J (2011) Lateral supraorbital approach applied to anterior clinoidal meningiomas: experience with 73 consecutive patients. Neurosurgery 68:1632–1647
Romani R, Laakso A, Kangasniemi M, Niemelä M, Hernesniemi J (2012) Lateral supraorbital approach applied to tuberculum sellae meningiomas: experience with 52 consecutive patients. Neurosurgery 70:1504–1518
Salma A, Alkandari A, Sammet S, Ammirati M (2011) Lateral supraorbital approach vs pterional approach: an anatomic qualitative and quantitative evaluation. Neurosurgery 68:364–372
Welling LC, Figueiredo EG, Wen HT, Gomes MQ, Bor-Seng-Shu E, Casarolli C, Guirado VM, Teixeira MJ (2015) Prospective randomized study comparing clinical, functional, and aesthetis results of minipterional and class pterional craniotomies. J Neurosurg 122:1012–1019
Yasargil MG (1984) General operative techniques, in Yasargil MG (ed): microneurosurgery. New York. NY: Thieme-Stratton 1:208–233
Yasargil MG (1996) Meningiomas. In: Yasargil MG (ed) Microneurosurgery, vol 4B. Thieme, New York, pp 134–185
Yasargil MG (1996) Surgical approaches. In: Yasargil MG (ed) Microneurosurgery, vol 4B. Thieme, New York, pp 29–68
Zumofen DW, Rychen J, Roethlisberger M, Taub E, Kalbermatten D, Nossek E, Potts M, Guzman R, Riina HA, Mariani L (2017) A review of the literature on the transciliary supraorbital keyhole approach. World Neurosurg 98:614–624
Acknowledgments
The authors would like to thank Dong-Su Jang, MFA, (Medical Illustrator, Medical Research Support Section, Yonsei University College of Medicine, Seoul, Korea) for his help with the illustrations.
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
The study was approved by the institutional review board and conducted in accordance with the ethical guidelines of the Declaration of Helsinki.
Informed consent
The data was analyzed retrospectively after obtaining informed consent from every patient.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Park, H.H., Sung, K.S., Moon, J.H. et al. Lateral supraorbital versus pterional approach for parachiasmal meningiomas: surgical indications and esthetic benefits. Neurosurg Rev 43, 313–322 (2020). https://doi.org/10.1007/s10143-019-01147-8
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10143-019-01147-8