Abstract
Craniotomy surgical site infections are an inherent risk and dreaded complication for the elective brain tumor patient. Sequelae can include delays in resumption in adjuvant treatments for multiple surgeries if staged cranioplasty is pursued. Here, the authors review their experience in operative debridement of surgical site infections with single-stage reimplantation of the salvaged craniotomy bone flap. A prospectively maintained database of a single surgeon’s neuro-oncology patients from 2009 to 2017 (JRF) was queried to identify 11 patients with surgical site infection after craniotomy for tumor resection. All patients underwent a protocol of aggressive operative debridement including drilling the bone edges and intraoperative flap sterilization with single-stage reimplantation, followed by tailored-antibiotic therapy. Ten of the 11 patients with frankly contaminated bone flaps from surgical site infection were able to be salvaged in a single-stage procedure. Five of these patients underwent adjuvant chemotherapy and/or radiation without secondary complication. There was one treatment failure in a delayed fashion which required additional surgery for craniectomy; however, this occurred after adjuvant treatment was administered. Surgical debridement and bone flap salvage is safe and cost-effective in managing acute surgical site infections after craniotomy for tumors. Additionally, this practice is likely beneficial in expediting the resumption of cancer therapy.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Craniotomy surgical site infections are an inherent risk and dreaded complication for the neurosurgeon. Estimates of incidence of infection in non-emergent craniotomies range from 2.4 to 8% [8, 16, 21]. Despite a significant decrease in surgical site infections concurrent with surgical antibiotic prophylaxis, there remain certain high-risk populations [16]. Risk factors identified for craniotomy wound infection include radiation therapy, re-operations, prolonged operative times, CSF leak, and sinus contamination [8]. The neuro-oncological patient usually satisfies one or more of these criteria.
In cases of post-craniotomy infection, the surgeon then must decide what, if any, are options for salvage of the bone flap. Historically, the standard of care for the post-craniotomy bone flap infection was operative debridement and explantation of the bone flap. Reasons for cranioplasty include protection against trauma, restoration of appearance, and prevention of the syndrome of the trephined [2]. Options for cranioplasty include reconstructions utilizing titanium mesh, polyetheetherketone (PEEK), or complex autologous grafts [13, 17, 19].
Several authors have challenged this paradigm. Series have demonstrated bone flap salvage with aggressive operative debridement [4, 24]. Different iterations of irrigation systems have shown adjuvant efficacy as well [1, 8, 11]. Published salvage rates range from 40 to 100%, and if series from 1985 and earlier are excluded, preservation improves to 67–100%.
Here, the authors wish to share their procedure for decontamination and single-stage reimplantation in high-risk patients, sometimes undergoing further oncological treatments.
Material and methods
Inclusion criteria
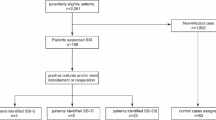
A single surgeon’s practice (JRF) was reviewed from 2009 to 2017. A practice database has been prospectively generated since 2009. This database is maintained in accordance with the ethical standards of our institution. The database was queried for incision and drainage of postoperative wound infection (CPT code 10180), debridement (CPT codes 11043 and 11044), and exploratory craniotomy (CPT codes 61304 and 61305). Forty-seven unique patients were identified. Inclusion criteria into the study included craniotomy for tumor excision and acute bacterial infection. Eleven patients met the inclusion criteria. Nine hundred sixty patients underwent craniotomy for tumor excision during this time, generating and having an infection rate of about 1.1%. Table 1 lists the patients and demographics.
Bone flap sterilization protocol
Early operative intervention of cranial wound infection is critical with bone flap salvage procedures. At the first identification of an erythematous or draining wound, the patient goes for urgent surgical debridement (Fig. 1). Oral antibiotic trials are avoided so as to prevent resistant species or sub-therapeutic dosing. The wound is widely opened and aggressively debrided of all necrotic and non-viable-appearing tissue including superficial scalp, sub-dermal adipose tissue, temporalis muscle, and early fibrinous scar tissue, which are sent to microbiology for culture (Fig. 2). All foreign materials such as synthetic dural grafts, cranial plates, and sealants are removed and also sent to microbiology for culture. The bone flap is removed and begins our sterilization protocol. During this time, the wound is irrigated with at least 3 L of saline or lactated ringers and soft tissue debridement continues. At this point, empiric antibiotics are started.
Once the bone flap is removed, it is grossly debrided with scrubbing and removal of fibrinous material. The cutting burr is then used to drill out porous areas of bone circumferentially, as well as on the superficial and deep side of the flap as this can be a refuge for bacterial concealment (Fig. 3). The bone is then soaked in peroxide followed by Betadine for 10 min each and repeated for a total soak time of 40 min. During this time, the native edges of the calvarial defect are carefully drilled until healthy-appearing, bleeding cancellous bone is encountered. The bone flap is closely reapposed to the bleeding calvarial edge with at least 25% of the flap in direct contact with the healthy skull (Fig. 4). Titanium plates and mini screws are used to secure the flap, attempting to minimize the amount of hardware used. A single 10-F subgaleal drain is left in the subgaleal space to prevent seroma, and typically removed the morning after surgery. The patient is changed from empiric antibiotics to culture-directed therapy as microbiological results return.
Antibiotic treatment
Empiric therapy begins after cultures are obtained intraoperatively. In general, the regimen has included vancomycin, cefepime, and metronidazole at meningitis-treatment doses. Bacterial sensitivities are typically finalized by the third day after cultures are obtained, though methicillin-resistant Staphylococcus aureus is detected within 24 h based on PCR testing for all gram-positive cocci at our institution. At this point, the inpatient infectious disease service is consulted to establish culture-directed therapy and duration. Patients also typically have short-interval follow-up in infectious disease clinic to determine if an oral suppressive regimen is indicated.
Results
All 11 patients had culture-positive acute bacterial infection with at most two species susceptible to antibiotic therapy. Notable risk factors for infection in this group included diabetes in two patients, prior craniotomy, prior whole brain radiation, obesity, and chronic steroid use related to rheumatoid arthritis. Six patients grew gram-positive bacterial species consisting of Staphylococcus species in four cases and Propionibacterium in three. The other four grew gram-negative rods consisting of Enterobacter species in two cases, Serratia marcescens, and Pseudomonas (see Table 2 for culture and antibiotic therapy details). Antibiotics were tailored once susceptibilities were established under the guidance of infectious disease consultation. All 11 patients initially received intravenous antibiotics (range 2–6 weeks). Five patients received an additional oral regimen after the completion of intravenous therapy, dependent on the species and sensitivities of the infection.
Ten patients appropriately cleared their infection after completion of antibiotics. One patient suffered from acute colitis from Clostridium difficile, attributed to the antibiotic use. This patient required change of antibiotics as well as oral metronidazole and vancomycin.
There was one treatment failure. This patient was a poorly controlled diabetic who underwent washout and attempted bone flap salvage 12 days after her initial surgery for glioblastoma multiforme. Because she had to obtain emergency insurance coverage, her adjuvant therapy started nearly 4 months after her washout. Rapid recurrence of the tumor was noted on imaging. On planned re-resection 2 months after completing adjuvant therapy, indolent infection of the incision and bone flap was noted. The patient underwent craniectomy, and restarted antibiotic therapy.
Mean follow-up in the series is 1126 days (range 87–2928). Five patients required adjuvant oncologic therapies and were able to receive such treatment. Upon disease progression, three patients underwent subsequent craniotomies and two had additional chemotherapy (see Table 3 for details of adjuvant therapy). One patient underwent treatment for disease progression nearly 18 months later.
Discussion
Utility of single-stage reimplantation in the neuro-oncological patient
Single-stage bone flap salvage is especially important to the neuro-oncological patient for several reasons. By avoiding a second operation, patients may proceed to planned adjuvant and complimentary therapies more quickly, avoiding delays in cancer treatment. Conversely, most oncological treatments are significantly caustic to the healing wound. Radiation therapy affects angiogenesis, fibroblast function, and other growth factors which can synergistically inhibit wound healing [9, 10, 23].
Newer chemotherapeutic agents have shown increased efficacy in treating high-grade gliomas, but also have a higher rate of wound-healing complications. Safety data from 900 patients treated with temozolomide and radiotherapy compared to that with bevacizumab, temozolomide, and radiotherapy showed wound-healing complications in 4.7 and 6.9% of patients respectively [22]. These risks were found to be even greater in one retrospective review on repeat craniotomies, with patients who received preoperative bevacizumab showing wound-healing complication rates increasing to 35% after second craniotomy and 33% after third [7]. This leads to the authors’ recommendation of delaying repeat craniotomies for recurrent glioblastoma to 28 days after the last administered dose of bevacizumab whenever possible. These studies support our hypothesis that avoiding a second cranioplasty operation after infection lowers the risk of further wound-healing complications. In this series, six patients underwent further treatment including radiation, temozolomide, and bevacizumab with one wound complication.
Decontamination methods
Data to support reimplantation of contaminated autologous bone flaps is accumulating. Bone flap decontamination techniques described in the case of dropped bone flaps have included soaking in Betadine and/or antibiotic solution, and autoclaving [14]. One center in Japan routinely employed bone flap autoclaving for autologous cranioplasty after deep-freezing without culture data. This practice was utilized similarly in a pediatric population with autoclaving before storage [15]. The adult population reported a 1 in 27 infection rate, while the pediatric population was of 3 in 14. This method has waned in popularity because of undesirable bone reabsorption in the process, and arguably low control rates.
The largest case series have been generated from autologous cranioplasty cases of positive intraoperative bone flap cultures without evidence of infection [5, 20]. With immediate culture of explanted bone flaps, the University of Washington and the University of Iowa groups found positive bacterial culture of bone flaps in 20 to 50% of cases. Historically discarded, both groups adopted a policy of reimplanting culture-positive autologous bone flaps over their observed time periods. Sterilization protocols included bacitracin soaking upon explantation and/or bacitracin and Betadine soaking of freezer-banked bone flaps before reimplantation. The University of Iowa group observed similar infection rates in culture-positive and culture-negative bone flaps—4.9 and 5.4% respectively. The University of Washington group observed an infection rate of culture-positive bone flaps statistically similar to culture-negative and synthetic cranioplasties—8, 7, and 5% respectively. While having invaluable contributions to their areas, the external validity to the frankly contaminated post-surgical bone flap is limited.
Bruce and Bruce published their series of 13 post-craniotomy wound infections [4]. Relying on aggressive debridement, removal of foreign material, and soaking of the bone flap in Betadine solution, they were able to demonstrate good results. Bone flaps were preserved in 11 of 13 patients (85%). Four patients required additional debridement (31%). Both patients requiring bone flap removal were anterior skull base cases with communication to the nasal sinuses. Their method does not include bone flap drilling, nor the use of drains.
A pediatric group in Denver published their experience of pus and free bone flaps in 14 patients in 2009 [24]. With aggressive debridement, they were able to preserve all bone flaps. However, only 2 of their 14 cases were tumor patients, and only 5 were postoperative infections. Half were related to primary bacterial infections (empyema and abscess). Additionally, three patients required additional minor procedures for wound debridement.
Irrigation systems have been employed in a variety of methods [1, 6, 8, 11]. Chou and colleagues demonstrated a 60% salvage rate in their series of 25 patients. The technique required 5 days of daily antibiotic suction-irrigation through subgaleal drains. Their case failures may have been due to lack of elevation nor debridement of the bone flaps. Auguste refined the method with operative debridement followed by a wash-in, wash-out antibiotic irrigation system. The clever system utilizes a total of four drains above and below the bone flap, and continually instills vancomycin solution typically for 5 days. Their method describes nursing evaluations every 2 h. Salvage was achieved in 11 of 12 patients, with the one failure being a patient undergoing adjuvant radiation. Delgado-Lopez and authors similarly reviewed a modest series of five patients with postoperative infections in a mixed population. Utilizing debridement, bone flap sterilization, and non-continuous wash-in, wash-out antibiotic irrigation, they were able to salvage all bone flaps. Their non-continuous irrigation system instilled smaller amounts of antibiotic solution and avoided the necessity of ICU observation for continuous irrigation.
Hyperbaric treatment has also shown promise treatment of cranial wounds [18]. Even in complicated neuro-oncologic patients, three of four bone flaps were able to be salvaged as opposed to three of six acrylic cranioplasties.
Our results combined with other recent, modern case series demonstrate that similar debridement methods without the utilization of the drainage system can show salvage rates that are non-inferior, without the associated costs of a prolonged ICU course as mentioned in the two studies conducted in the USA. It would be of interest to compare length of hospitalization in future investigations.
Causative organisms
Early recognition of surgical site infection with early debridement is most likely to yield culture data. Additionally, by minimizing the duration of empiric antibiotic therapy, the likelihood of antibiotic-resistant organisms should decrease [12]. Seven of our 11 patients had infections with typical skin flora, and none of the patients were infected with bacteria which demonstrated antibiotic resistance necessitating change to second-line or alternate antibiotic course.
Organisms found in culture vary by population. Bruce found Staphylococcus species in 5 of 13, and P. acnes in 4 of 13. Staphylococcus was isolated in all patients in Brazil. Common causative organisms in the Denver group were methicillin-sensitive S. aureus in 36% (including both tumor patients), and Streptococcus species in 29%. In series with duration-to-revision data, P. acnes was the most indolent infection: Bruce ranging 33–102 days and Auguste ranging 14–98 days. In a review of cranioplasty infections in a trauma population in Australia, they noted their delayed infections occurred with P. acnes—an average of 308 days to diagnosis in their three cases [3]. Similarly, the three P. acnes infections in this series had the three longest durations to presentation of average of 47 days.
Antibiotic therapy
Antibiotic treatment also lacks standardization in the literature. Auguste and McDermott instilled vancomycin solution via their drainage system concomitant with inpatient IV antibiotic treatment for 1 week, followed by 2 weeks of outpatient culture-directed IV antibiotic treatment, then 3 months of oral suppressive therapy [1]. The Delgado-Lopez group instilled vancomycin and cefotaxime via their irrigation and drainage system in addition to 2 weeks of broad-spectrum IV antibiotics followed by 4–8 weeks of culture-directed oral therapy [8]. Their oral antibiotic treatment endpoint was based on clinical healing. Widdel and Winston in their pediatric practice prescribe 6 weeks of culture-directed IV antibiotics [24]. Bruce and Bruce utilize culture-directed therapy as prescribed by infectious disease colleagues, typically 1 week of IV antibiotics followed by 2–4 weeks of oral therapy [4]. Use of broad-spectrum antibiotics in drainage systems and prolonged empiric treatment regimens may increase bacterial antibiotic resistance and increase risk of adverse medication effects though none were reported in these earlier series among small numbers. The variability in bacterial species and evolving resistance, variability of tissues involved, and practice differences within our collaborating infectious disease group make rote recommendations difficult. However, we guide our practice with avoidance of prolonged broad-spectrum antibiotic usage and early utilization of culture-directed therapy, along with the expertise of infectious disease specialists.
Limitations
This series is limited by its small sample size and lack of control. Just over half of the patients in this series required adjuvant therapy.
Conclusions
Surgical debridement and bone flap salvage is safe and cost-effective in managing acute surgical site infections after craniotomy for tumors. Additionally, this practice is likely beneficial in expediting the resumption of cancer therapy. Our method shortens ICU and hospital stays by avoiding the prolonged use of drains and avoids unnecessary broad-spectrum antibiotic treatment. Further prospective study will be important to demonstrate the long-term safety of the practice of bone flap salvage and identify patients at risk for treatment failure.
References
Auguste KI, McDermott MW (2006) Salvage of infected craniotomy bone flaps with the wash-in, wash-out indwelling antibiotic irrigation system: technical note and case series of 12 patients. J Neurosurg 105(4):640–644. https://doi.org/10.3171/jns.2006.105.4.640
Baumeister S, Peek A, Friedman A, Levin LS, Marcus JR (2008) Management of postneurosurgical bone flap loss caused by infection. Plast Reconstr Surg 122(6):195e–208e. https://doi.org/10.1097/PRS.0b013e3181858eee
Bhaskar IP, Inglis TJJ, Lee GYF (2014) Clinical, radiological, and microbiological profile of patients with autogenous cranioplasty infections. World Neurosurg 82(3-4):e531–e534. https://doi.org/10.1016/j.wneu.2013.01.013
Bruce JN, Bruce SS (2003) Preservation of bone flaps in patients with postcraniotomy infections. J Neurosurg 98(6):1203–1207. https://doi.org/10.3171/jns.2003.98.6.1203
Chiang H, Steelman VM, Pottinger JM, Schlueter AJ, Diekema DJ, Greenlee JDW, Howard MA, Herwaldt LA (2011) Clinical significance of positive cranial bone flap cultures and associated risk of surgical site infection after craniotomies or craniectomies. J Neurosurg 114(6):1746–1754. https://doi.org/10.3171/2011.1.JNS10782
Chou SN, Erickson DL (1976) Craniotomy infections. Clin Neurosurg 23(CN_suppl_1):357–362. https://doi.org/10.1093/neurosurgery/23.CN_suppl_1.357
Clark AJ, Butowski NA, Chang SM, Prados MD, Clarke J, Polley M-YC, Sughrue ME, McDermott MW, Parsa AT, Berger MS, Aghi MK (2011) Impact of bevacizumab chemotherapy on craniotomy wound healing. J Neurosurg 114(6):1609–1616. https://doi.org/10.3171/2010.10.JNS101042
Delgado-López PD, Martín-Velasco V, Castilla-Díez JM, Galacho-Harriero AM, Rodríguez-Salazar A (2009) Preservation of bone flap after craniotomy infection. Neurocir Astur Spain 20(2):124–131. https://doi.org/10.1016/S1130-1473(09)70179-4
Denham JW, Hauer-Jensen M (2002) The radiotherapeutic injury—a complex “wound”. Radiother Oncol J Eur Soc Ther Radiol Oncol 63(2):129–145. https://doi.org/10.1016/S0167-8140(02)00060-9
Dormand E-L, Banwell PE, Goodacre TEE (2005) Radiotherapy and wound healing. Int Wound J 2(2):112–127. https://doi.org/10.1111/j.1742-4801.2005.00079.x
Erickson DL, Seljeskog EL, Chou SN (1974) Suction-irrigation treatment of craniotomy infections. Tech Note J Neurosurg 41(2):265–267. https://doi.org/10.3171/jns.1974.41.2.0265
Goldmann DA, Weinstein RA, Wenzel RP, Tablan OC, Duma RJ, Gaynes RP, Schlosser J, Martone WJ (1996) Strategies to prevent and control the emergence and spread of antimicrobial-resistant microorganisms in hospitals. A challenge to hospital leadership. JAMA 275(3):234–240. https://doi.org/10.1001/jama.1996.03530270074035
Gordon CR, Fisher M, Liauw J, Lina I, Puvanesarajah V, Susarla S, Coon A, Lim M, Quinones-Hinojosa A, Weingart J, Colby G, Olivi A, Huang J (2014) Multidisciplinary approach for improved outcomes in secondary cranial reconstruction: introducing the pericranial-onlay cranioplasty technique. Neurosurgery 10(Suppl 2):179–189; discussion 189-190. https://doi.org/10.1227/NEU.0000000000000296
Jankowitz BT, Kondziolka DS (2006) When the bone flap hits the floor. Neurosurgery 59(3):585–590; discussion 585-590. https://doi.org/10.1227/01.NEU.0000231849.12751.B9
Josan VA, Sgouros S, Walsh AR, Dover MS, Nishikawa H, Hockley AD (2005) Cranioplasty in children. Childs Nerv Syst ChNS Off J Int Soc Pediatr Neurosurg 21(3):200–204. https://doi.org/10.1007/s00381-004-1068-2
Korinek A-M, Golmard J-L, Elcheick A, Bismuth R, van Effenterre R, Coriat P, Puybasset L (2005) Risk factors for neurosurgical site infections after craniotomy: a critical reappraisal of antibiotic prophylaxis on 4,578 patients. Br J Neurosurg 19(2):155–162. https://doi.org/10.1080/02688690500145639
Kshettry VR, Hardy S, Weil RJ, Angelov L, Barnett GH (2012) Immediate titanium cranioplasty after debridement and craniectomy for postcraniotomy surgical site infection. Neurosurgery 70:8–14; discussion 14-15. https://doi.org/10.1227/NEU.0b013e31822fef2c
Larsson A, Engström M, Uusijärvi J, Kihlström L, Lind F, Mathiesen T (2002) Hyperbaric oxygen treatment of postoperative neurosurgical infections. Neurosurgery 50:287–295; discussion 295-296
Morton RP, Abecassis IJ, Hanson JF, Barber J, Nerva JD, Emerson SN, Ene CI, Chowdhary MM, Levitt MR, Ko AL, Dellit TH, Chesnut RM (2016) Predictors of infection after 754 cranioplasty operations and the value of intraoperative cultures for cryopreserved bone flaps. J Neurosurg 125(3):766–770. https://doi.org/10.3171/2015.8.JNS151390
Morton RP, Josh Abecassis I, Hanson JF, Barber J, Nerva JD, Emerson SN, Ene CI, Chowdhary MM, Levitt MR, Ko AL, Dellit TH, Chesnut RM (2016) Predictors of infection after 754 cranioplasty operations and the value of intraoperative cultures for cryopreserved bone flaps. J Neurosurg 125(3):1–5. https://doi.org/10.3171/2015.8.JNS151390
O’Keeffe AB, Lawrence T, Bojanic S (2012) Oxford craniotomy infections database: a cost analysis of craniotomy infection. Br J Neurosurg 26(2):265–269. https://doi.org/10.3109/02688697.2011.626878
Saran F, Chinot OL, Henriksson R, Mason W, Wick W, Cloughesy T, Dhar S, Pozzi E, Garcia J, Nishikawa R (2016) Bevacizumab, temozolomide, and radiotherapy for newly diagnosed glioblastoma: comprehensive safety results during and after first-line therapy. Neuro-Oncol 18(7):991–1001. https://doi.org/10.1093/neuonc/nov300
Tibbs MK (1997) Wound healing following radiation therapy: a review. Radiother Oncol J Eur Soc Ther Radiol Oncol 42(2):99–106. https://doi.org/10.1016/S0167-8140(96)01880-4
Widdel L, Winston KR (2009) Pus and free bone flaps. J Neurosurg Pediatr 4(4):378–382. https://doi.org/10.3171/2009.5.PEDS0963
Acknowledgements
The authors wish to extend their gratitude to the support staff who aid in patient care and coordination, including Veronica Toudouze, PA and Lacinda Evans, NP.
Author information
Authors and Affiliations
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Statement of human rights
Informed consent was obtained from all individual participants and/or surrogates included in this study. Additional informed consent was obtained from the patient whose de-identified intraoperative photographs are used in the figures.
Statement on the welfare of animals
This article does not contain any studies with animals performed by any of the authors.
Rights and permissions
About this article
Cite this article
Wallace, D.J., McGinity, M.J. & Floyd, J.R. Bone flap salvage in acute surgical site infection after craniotomy for tumor resection. Neurosurg Rev 41, 1071–1077 (2018). https://doi.org/10.1007/s10143-018-0955-z
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10143-018-0955-z