Abstract
Subarachnoid hemorrhage (SAH) is usually caused by a ruptured intracranial aneurysm. However, in some patients, no source of hemorrhage might be detected despite repeated digital subtraction angiography (DSA). Our objective was to analyze factors influencing the clinical outcome in patients suffering from non-aneurysmal and non-perimesencephalic (NPM) SAH. Between 1999 and 2011, 68 of 1,188 patients with SAH (5.7 %) suffered from non-aneurysmal and NPM-SAH. Outcome was assessed according to the modified Rankin Scale (mRS) at 6 months (mRS 0–2 favorable vs. 3–6 unfavorable). In patients with angiogram-negative and NPM-SAH, favorable outcome was achieved in 56 patients (82.4 %). In the multivariate analysis, age <65 years and non-Fisher 3 bleeding pattern were significantly associated with favorable outcome. Angiogram-negative and NPM-SAH had good prognoses. Patients with non-Fisher-type 3 bleeding had excellent outcomes similar to patients with perimesencephalic SAH, but patients with Fisher-type 3 bleeding were at risk for poor outcome like aneurysmal SAH patients due to cerebral vasospasm and delayed cerebral ischemia. Age and bleeding type were detected as prognostic factors in the multivariate analysis.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Spontaneous subarachnoid hemorrhage (SAH) is usually caused by intracranial aneurysm rupture. However, in up to 20 % of the patients with SAH, cerebral angiography, computed tomography (CT) scans, and spinal magnetic resonance imaging (MRI) are negative for aneurysms or other vascular malformations [1–4]. In about 20 to 70 % of these patients with angiogram-negative SAH, the blood distribution is described either as perimesencephalic (PM), pretruncal, or prepontine [5].
The perimesencephalic SAH subgroup is considered to be associated with excellent outcome and low risk of rebleeding [5, 6]. Unfortunately, data on outcome in patients suffering from angiogram-negative and non-perimesencephalic (NPM) SAH are published often only in small case series [1, 7–14], and data is scarce for series with more than 50 patients [5, 15, 16].
We therefore analyzed patients suffering from angiographic-negative and NPM-SAH who had been admitted to our institution.
Methods
Between 1999 and 2011, 1,188 consecutive patients suffering from SAH have been admitted to our institution. SAH was diagnosed by CT scans or lumbar puncture. Patients with trauma-related SAH and patients in whom the bleeding sources were determined to be an aneurysm or vascular malformation were excluded from the study. Patient characteristics, treatments, radiological features, and outcomes were prospectively entered into our neurovascular database (SPSS, version 15, SPSS Inc.).
All patients underwent angiography and, since 2002, three-dimensional four-vessel digital subtraction angiography (DSA) to rule out intracranial bleeding sources. Patients with verified intracranial aneurysms were treated by surgical or endovascular aneurysm occlusion based on an interdisciplinary consensus [17]. In patients with angiogram-negative SAH, angiography was repeated approximately 14 days after the ictus. Additionally, spinal magnetic resonance imaging (MRI) was performed to rule out a spinal bleeding source.
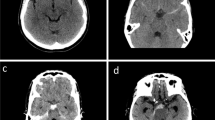
We defined a perimesencephalic hemorrhage, according to van Gijn et al. [6] and Rinkel et al. [18], if the hemorrhage was located in front of the brain stem, mainly in the interpendicular cistern, with or without extension to the ambient, chiasmatic, and horizontal part of the Sylvian cisterns. In non-perimesencephalic hemorrhages, blood was not located mainly in the interpendicular cistern, but in the Sylvian cistern, interhemispheric cistern, convexity or a CT-negative, and lumbar puncture-positive bleeding. Patients were further stratified according to the distribution of subarachnoid blood into Fisher 3 patterns (Fi3) or non-Fisher 3 patterns (non-Fi3) [19].
Our treatment protocol includes the application of nimodipine in all patients with SAH from the day of admission and has been described in detail previously [20, 21]. In patients with symptomatic vasospasm, hypertension was induced with catecholamines [22].
On admission, patients were divided into good grade (World Federation of Neurological Societies [WFNS] grades I–III) and poor grade (WFNS IV–V). Outcome was assessed according to the modified Rankin Scale (mRS) after 6 months and stratified into favorable (mRS score 0–2) and unfavorable (mRS score 3–6) outcome.
Statistical analysis
Data analyses were performed using the computer software package SPSS (version 15, SPSS, Inc.). Unpaired t tests were used for parametric statistics. Categorical variables were analyzed in contingency tables using the χ 2 test. Results with p < 0.05 were considered statistically significant.
In a second step, a multivariate analysis was performed to identify independent predictors of favorable outcome after 6 months and to find confounding effects between potentially independent predictors. Variables with significant p values on univariate analysis were considered as potentially independent variables in a multivariate analysis. A backward stepwise method was used to construct a multivariate logistic regression model in relation to favorable outcome as a dependent variable with an inclusion criterion of p < 0.05.
Results
Patient characteristics
One hundred fifty-two of the 1,188 patients (12.8 %) after diagnostic workup suffering from SAH had aneurysm-negative DSA with growing numbers in the last years. From July 1999 to June 2003, 32 patients presented with a non-aneurysmal SAH; in the following 4 years, 75 % more patients (n = 56) had a non-aneurysmal SAH and 100 % more patients (n = 64) from July 2007 to June 2011. Sixty-eight of the 1,188 patients (5.7 %) presented with angiogram-negative and NPM-SAH (Fig. 1). Overall, 56 of the 68 patients (82.4 %) suffering from angiogram-negative and NPM-SAH achieved favorable outcome.
Number of patients with non-aneurysmal SAH and percentage of patients using coagulation-affecting drugs. Not only the numbers of patients are increasing over the years but also the percentage of patients using drugs affecting the anticoagulation and/or platelet function increased over a period. Using coagulation-affecting drugs may be one reason for the growing numbers of patients with non-aneurysmal SAH
Patients’ characteristics, including age, sex, clinical status at admission, and clinical outcome are given in detail in Table 1.
Anticoagulation and platelet inhibition
From July 1999 to June 2003, 32 patients had a non-aneurysmal SAH and 6 % of the patients took anticoagulation-affective drugs. In the following period (July 2003 to June 2007), 75 % more patients had a non-aneurysmal SAH, and the use of drugs increased by 300 %. In the last period (July 2007 to June 2011), the number of SAH increased by 100 %, and the use of anticoagulation drugs or platelet-inhibiting drugs increased by 600 % compared to the first period (Fig. 1).
Neurological grading at admission
Fifty-seven patients (83.8 %) were in a good grade, whereas 11 patients (16.2 %) were in poor grade at admission. Favorable outcome was achieved in 51 of 56 good grade patients (91.1 %) and in 6 of 12 poor grade patients (50 %, p < 0.001).
Imaging results
Overall, in 14 of 166 patients (8.4 %), a bleeding source was detected by a second DSA (13 patients) or additionally performed spinal MRI (1 patient).
Subarachnoid blood distribution
Twenty-five of 68 patients (36.8 %) had Fi3 patterns, whereas 43 of 68 patients (63.2 %) had non-Fi3 patterns subarachnoid blood distribution. Patients with non-Fi3 blood patterns had a significant better admission status compared to patients with Fi3 patterns (p < 0.001; OR 28, 95 % CI 3.3–238). Favorable outcome was achieved in 16 patients with Fi3 (64.0 %) vs. 40 patients (93.0 %) with non-Fi3 (p < 0.01; OR 7.5, 95 % CI 1.8–31; Table 2).
Cerebral vasospasm and delayed cerebral ischemia
Thirty-one patients (20.4 %) with angiogram-negative DSA developed cerebral vasospasm (CVS). Eighteen patients with NPM-SAH vs. 13 patients with PM-SAH developed CVS over the course of treatment (26.5 vs. 15.5 %; p = 0.1). From 25 patients with a Fi3 patterns, 12 patients developed CVS vs. 6 of 43 patients with non-Fi3 patterns (48 vs. 14.0 %; p < 0.01; OR 5.7, 95 % CI 1.8–18). Considering the Vergouwen definitions [23], 21 patients developed a delayed cerebral ischemia (DCI), 13 patients with NPM-SAH vs. 8 patients with PM-SAH (19.1 vs. 9.5 %; p = 0.1). Ten patients with Fi3 patterns vs. 3 with non-Fi3 patterns showed DCI (40 vs. 7.0 %; p < 0.01; OR 8.9, 95 % CI 2.1–37).
Posthemorrhagic hydrocephalus
Overall, early hydrocephalus was detected in 19 of 68 patients (27.9 %). Fourteen patients with Fi3 patterns (56.0 %) vs. five patients (11.6 %) with non-Fi3 patterns suffered from early hydrocephalus (p < 0.001; OR 9.7, 95 % CI 2.8–33). Overall, 7 of 68 patients (10.3 %) developed a shunt-dependent hydrocephalus. Two patients with Fi3 patterns (8.0 %) vs. five patients with non-Fi3 patterns (11.6 %) developed a shunt-dependent hydrocephalus during follow-up (p = 0.66). Favorable outcome was significantly more often achieved in patients without early hydrocephalus compared to patients suffering from early hydrocephalus (21.4 vs. 58.3 %; p < 0.01; OR 5.1; 95 % CI 1.4–19).
Multivariate analysis
In the univariate analysis ‘age, hydrocephalus, bleeding type, and good admission status’ were significantly associated with favorable outcome in patients with angiographic-negative and NPM-SAH. Therefore, we performed a multivariate logistic regression analysis of those variables. The multivariate regression model did illustrate the variables “age <65 years” (p < 0.05; OR 6.1, 95 % CI 1.3–28.4) and “non-Fi3 blood pattern” (p < 0.01; OR 10.8, 95 % CI 2.2–52.6) as independent and significant predictors for favorable outcome in patients with angiographic-negative and NPM-SAH (Nagelkerke’s R 2 = 0.33), so the variables hydrocephalus and admission status were dependent variables from age and bleeding type and, therefore, not a significant predicting factor of patients’ outcome (Table 2).
Discussion
Subarachnoid hemorrhage without identification of a bleeding source is a rare entity [1, 3, 6, 18]. Our data shows growing numbers of this bleeding type (Fig. 1), but data on patients with angiogram-negative and NPM-SAH is not so often [1, 7, 8, 11, 12, 24–27] and scarce for series with more than 50 patients [5, 15, 16]. Therefore, our institutional data was analyzed, and 68 patients (5.7 %) suffering from angiogram-negative and NPM-SAH were identified. The present data indicates that patients with angiogram-negative and NPM-SAH might achieve favorable outcome. In the multivariate analysis, age <65 years and non-Fi3 blood pattern were significantly associated with favorable outcome.
Anticoagulation and platelet inhibition
We have significant increasing numbers of patients with non-aneurysmal SAH despite the technological improvements of DSA. One reason could be the increasing number of patients with systemic anticoagulation or platelet inhibition (Fig. 1). Data for perimesencephalic SAH and coagulation-influencing drugs is scarce, but describes higher blood amount and rebleeding rates [28–30]. In the literature, good and valid data for non-perimesencephalic SAH analyzing these is not only scarce, it is missing. Boswell et al. described a 4 % rehemorrhage rate (range 0–12.3 %) for perimesencephalic and non-perimesencephalic SAH in their meta-analysis [31], which is slightly higher than the one case (without taking coagulation-influencing drugs) in our series (1.5 %), but a high number of unreported or non-selected cases have to be assumed. Unfortunately, actually, a comparison of recurrent hemorrhages seems not be useful due to the very different hospital algorithms (some centers only perform a single DSA at admission), but after an extensive diagnostic workup, the risk of a rehemorrhage seems to be very low.
Incidence of non-aneurysmal NPM-SAH and neurological condition at admission
Up to 13 % of patients with spontaneous SAH and aneurysm-negative baseline DSA present with perimesencephalic or NPM-SAH pattern on initial CT scan [1, 5, 7, 8, 11, 12, 15, 16, 24, 25, 27].
In the present series, 5.7 % of patients presented with non-aneurysmal and NPM-SAH. Most of these patients were in a good clinical condition at admission (83.8 %). In the present series, favorable outcome was achieved in 82.4 % of the patients with angiogram-negative NPM-SAH.
Angiographic results
A recently published study reported a significantly lower rate of rebleeding in patients with perimesencephalic SAH compared to patients with NPM-SAH [31]. Therefore, rebleeding is the most important preventable cause of unfavorable outcome in patients suffering from spontaneous SAH [32]. Therefore, in patients with aneurysm-negative baseline DSA, repeat DSA is necessary in order to detect a potential bleeding source and to prevent rebleeding [27, 31, 33]. In the present series, 152 patients had a spontaneous angiogram-negative SAH after diagnostic workup. In our treatment protocol, all patients receive two DSA and MRI of the whole spine, resulting in only one rebleeding after this diagnostic workup. However, in 13 patients (7.8 %) with initial non-aneurysmal SAH, a source of hemorrhage was revealed in the second DSA. In one patient (0.6 %) with a repeated aneurysm-negative DSA, an additionally performed spinal MRI identified a spinal pathology as source of the hemorrhage. This rate is similar to other published data with series of more than 50 patients (7–18 %) [15, 33–35]. Some studies described lower rates, but repeated angiography was done in less than 50 patients [8, 36].
SAH pattern on initial CT scan
In patients suffering from non-aneurysmal and NPM-SAH, favorable outcome was significantly associated with SAH pattern on initial CT [16]. According to the multivariate analysis, favorable outcome was significantly more often achieved in patients without blood distribution according to Fisher score 3 (p < 0.01; Table 1 ).
Cerebral vasospasm and delayed cerebral ischemia
As previously reported, patients suffering from non-aneurysmal and NPM-SAH had significantly higher risk to develop angiographic CVS when compared to patients with PM-SAH [11]. In the present series, 15.5 % of patients with PM-SAH developed CVS compared to 26.5 % of patients with NPM-SAH (p = 0.1). Especially, the Fi3 group developed significant, more frequent CVS (48.0 %) and DCI (40.0 %) vs. non-Fi3 patients (CVS 14.0 %, p < 0.01; DCI 7.0 %, p < 0.01), which seems to be the reason for the worse outcome of the Fi3 group (64.0 %) compared to the non-Fi3 group (93.0 %; p < 0.01).
Posthemorrhagic hydrocephalus
Posthemorrhagic hydrocephalus is common in patients with spontaneous SAH [37]. Posthemorrhagic hydrocephalus occurred significantly more often in patients with NPM-SAH when compared to patients with PM-SAH [11]. In the present series, early hydrocephalus was found in 27.9 % of patients with NPM-SAH. Furthermore, up to 21 % of patients with aneurysm-negative baseline DSA and NPM-SAH have been reported to develop shunt-dependent hydrocephalus [33]. 10.3 % of the patients with NPM-SAH developed shunt-dependent hydrocephalus during long-term follow-up.
Comparison of outcome between the non-Fisher-type 3 subgroup of angiographic-negative NPM-SAH and perimesencephalic SAH
The non-Fi3 subgroup was compared with patients suffering from perimesencephalic SAH in our hospital (Table 3). Both groups were in a good status at admission (98 vs. 91 %, not significantly different). A favorable outcome was achieved in 93 % of the patients in the non-Fi3 group compared to 89 % in the perimesencephalic SAH group (not significantly different). Patients without bleeding in the basal cisterns seem to have an excellent outcome like patients with perimesencephalic SAH (Table 3).
Functional outcome
Several studies have reported that the majority of patients with non-aneurysmal and NPM-SAH might achieve favorable outcome [2, 4, 6, 18, 38]. Overall, 82.4 % of patients with non-aneurysmal and NPM-SAH achieved favorable outcome in the present series. In the present study, a DCI was only in 7.0 % of the patients with a non-Fi3 bleeding pattern observed, compared to 40.0 % in the Fi3 group. Therefore, an absence of vasospasm and cerebral infarctions seems to be the main reason for the excellent outcome of the non-Fi3 compared to aneurysmal SAH or the Fi3 group (p < 0.01; OR 8.9, 95 % CI 2.1–37).
In the present multivariate analysis, younger age (p < 0.05) and non-Fi3 blood pattern (p < 0.01) were independent predictors for favorable outcome in patients with non-aneurysmal and NPM-SAH.
Conclusion
Patients suffering from spontaneous NPM-SAH incline to achieve favorable outcome. However, occurrence of rebleeding, vasospasm, or hydrocephalus might impair clinical outcome. Therefore, careful individual decision-making, repeated DSA, and attentive clinical observation are necessary to maintain the potential for favorable outcome in this rare patient cohort. Especially, patients with a Fisher-type 3 blood patterns were at risk for a poor outcome due to CVS and DCI.
References
Gupta SK, Gupta R, Khosla VK, Mohindra S, Chhabra R, Khandelwal N, Gupta V, Mukherjee KK, Tewari MK, Pathak A, Mathuriya SN (2009) Nonaneurysmal nonperimesencephalic subarachnoid hemorrhage: is it a benign entity? Surg Neurol 71:566–571
Rinkel GJ, Wijdicks EF, Vermeulen M, Hasan D, Brouwers PJ, van Gijn J (1991) The clinical course of perimesencephalic nonaneurysmal subarachnoid hemorrhage. Ann Neurol 29:463–468
Schwartz TH, Solomon RA (1996) Perimesencephalic nonaneurysmal subarachnoid hemorrhage: review of the literature. Neurosurgery 39:433–440
van Gijn J, Rinkel GJ (2001) Subarachnoid haemorrhage: diagnosis, causes and management. Brain 124:249–278
Ildan F, Tuna M, Erman T, Gocer AI, Cetinalp E (2002) Prognosis and prognostic factors in nonaneurysmal perimesencephalic hemorrhage: a follow-up study in 29 patients. Surg Neurol 57:160–165
van Gijn J, van Dongen KJ, Vermeulen M, Hijdra A (1985) Perimesencephalic hemorrhage: a nonaneurysmal and benign form of subarachnoid hemorrhage. Neurology 35:493–497
Beseoglu K, Pannes S, Steiger HJ, Hanggi D (2010) Long-term outcome and quality of life after nonaneurysmal subarachnoid hemorrhage. Acta Neurochir (Wien) 152:409–416
Canhao P, Ferro JM, Pinto AN, Melo TP, Campos JG (1995) Perimesencephalic and nonperimesencephalic subarachnoid haemorrhages with negative angiograms. Acta Neurochir (Wien) 132:14–19
Fontanella M, Rainero I, Panciani PP, Schatlo B, Benevello C, Garbossa D, Carlino C, Valfre W, Griva F, Bradac GB, Ducati A (2011) Subarachnoid hemorrhage and negative angiography: clinical course and long-term follow-up. Neurosurg Rev 34:477–484
Hui FK, Tumialan LM, Tanaka T, Cawley CM, Zhang YJ (2009) Clinical differences between angiographically negative, diffuse subarachnoid hemorrhage and perimesencephalic subarachnoid hemorrhage. Neurocrit Care 11:64–70
Kang DH, Park J, Lee SH, Park SH, Kim YS, Hamm IS (2009) Does non-perimesencephalic type non-aneurysmal subarachnoid hemorrhage have a benign prognosis? J Clin Neurosci 16:904–908
Kumar S, Goddeau RP Jr, Selim MH, Thomas A, Schlaug G, Alhazzani A, Searls DE, Caplan LR (2010) Atraumatic convexal subarachnoid hemorrhage: clinical presentation, imaging patterns, and etiologies. Neurology 74:893–899
Nayak S, Kunz AB, Kieslinger K, Ladurner G, Killer M (2010) Classification of non-aneurysmal subarachnoid haemorrhage: CT correlation to the clinical outcome. Clin Radiol 65:623–628
Whiting J, Reavey-Cantwell J, Velat G, Fautheree G, Firment C, Lewis S, Hoh B (2009) Clinical course of nontraumatic, nonaneurysmal subarachnoid hemorrhage: a single-institution experience. Neurosurg Focus 26:E21
Maslehaty H, Petridis AK, Barth H, Mehdorn HM (2011) Diagnostic value of magnetic resonance imaging in perimesencephalic and nonperimesencephalic subarachnoid hemorrhage of unknown origin. J Neurosurg 114:1003–1007
Woznica M, Rosahl SK, Berlis A, Weyerbrock A (2010) Outcome correlates with blood distribution in subarachnoid hemorrhage of unknown origin. Acta Neurochir (Wien) 152:417–422
Schuss P, Konczalla J, Platz J, Vatter H, Seifert V, Güresir E (2013) Aneurysm-related subarachnoid hemorrhage and acute subdural hematoma: single-center series and systematic review. J Neurosurg
Rinkel GJ, Wijdicks EF, Hasan D, Kienstra GE, Franke CL, Hageman LM, Vermeulen M, van Gijn J (1991) Outcome in patients with subarachnoid haemorrhage and negative angiography according to pattern of haemorrhage on computed tomography. Lancet 338:964–968
Fisher CM, Kistler JP, Davis JM (1980) Relation of cerebral vasospasm to subarachnoid hemorrhage visualized by computerized tomographic scanning. Neurosurgery 6:1–9
Güresir E, Beck J, Vatter H, Setzer M, Gerlach R, Seifert V, Raabe A (2008) Subarachnoid hemorrhage and intracerebral hematoma: incidence, prognostic factors, and outcome. Neurosurgery 63:1088–1093
Güresir E, Raabe A, Setzer M, Vatter H, Gerlach R, Seifert V, Beck J (2009) Decompressive hemicraniectomy in subarachnoid haemorrhage: the influence of infarction, haemorrhage and brain swelling. J Neurol Neurosurg Psychiatry 80:799–801
Raabe A, Beck J, Keller M, Vatter H, Zimmermann M, Seifert V (2005) Relative importance of hypertension compared with hypervolemia for increasing cerebral oxygenation in patients with cerebral vasospasm after subarachnoid hemorrhage. J Neurosurg 103:974–981
Vergouwen MD, Vermeulen M, van Gijn J, Rinkel GJ, Wijdicks EF, Muizelaar JP, Mendelow AD, Juvela S, Yonas H, Terbrugge KG, Macdonald RL, Diringer MN, Broderick JP, Dreier JP, Roos YB (2010) Definition of delayed cerebral ischemia after aneurysmal subarachnoid hemorrhage as an outcome event in clinical trials and observational studies: proposal of a multidisciplinary research group. Stroke 41:2391–2395
Germans MR, Pennings FA, Sprengers ME, Vandertop WP (2008) Spinal vascular malformations in non-perimesencephalic subarachnoid hemorrhage. J Neurol 255:1910–1915
Kong Y, Zhang JH, Qin X (2011) Perimesencephalic subarachnoid hemorrhage: risk factors, clinical presentations, and outcome. Acta Neurochir Suppl 110:197–201
Van Calenbergh F, Plets C, Goffin J, Velghe L (1993) Nonaneurysmal subarachnoid hemorrhage: prevalence of perimesencephalic hemorrhage in a consecutive series. Surg Neurol 39:320–323
Yu DW, Jung YJ, Choi BY, Chang CH (2012) Subarachnoid hemorrhage with negative baseline digital subtraction angiography: is repeat digital subtraction angiography necessary? J Cerebrovasc Endovasc Neurosurg 14:210–215
Garcia-Rodriguez LA, Gaist D, Morton J, Cookson C, Gonzalez-Perez A (2013) Antithrombotic drugs and risk of hemorrhagic stroke in the general population. Neurology 81:566–574
Naidech AM, Rosenberg NF, Maas MB, Bendok BR, Batjer HH, Nemeth AJ (2012) Predictors of hemorrhage volume and disability after perimesencephalic subarachnoid hemorrhage. Neurology 78:811–815
van der Worp HB, Fonville S, Ramos LM, Rinkel GJ (2009) Recurrent perimesencephalic subarachnoid hemorrhage during antithrombotic therapy. Neurocrit Care 10:209–212
Boswell S, Thorell W, Gogela S, Lyden E, Surdell D (2013) Angiogram-negative subarachnoid hemorrhage: outcomes data and review of the literature. J Stroke Cerebrovasc Dis 22:750–757
Broderick JP, Brott TG, Duldner JE, Tomsick T, Leach A (1994) Initial and recurrent bleeding are the major causes of death following subarachnoid hemorrhage. Stroke 25:1342–1347
Dalyai R, Chalouhi N, Theofanis T, Jabbour PM, Dumont AS, Gonzalez LF, Gordon DS, Rosenwasser RH, Tjoumakaris SI (2013) Subarachnoid hemorrhage with negative initial catheter angiography: a review of 254 cases evaluating patient clinical outcome and efficacy of short- and long-term repeat angiography. Neurosurgery 72:646–652
Delgado Almandoz JE, Crandall BM, Fease JL, Scholz JM, Anderson RE, Kadkhodayan Y, Tubman DE (2013) Diagnostic yield of catheter angiography in patients with subarachnoid hemorrhage and negative initial noninvasive neurovascular examinations. AJNR Am J Neuroradiol 34:833–839
Jung JY, Kim YB, Lee JW, Huh SK, Lee KC (2006) Spontaneous subarachnoid haemorrhage with negative initial angiography: a review of 143 cases. J Clin Neurosci 13:1011–1017
Khan AA, Smith JD, Kirkman MA, Robertson FJ, Wong K, Dott C, Grieve JP, Watkins LD, Kitchen ND (2013) Angiogram negative subarachnoid haemorrhage: outcomes and the role of repeat angiography. Clin Neurol Neurosurg 115:1470–1475
de Oliveira JG, Beck J, Setzer M, Gerlach R, Vatter H, Seifert V, Raabe A (2007) Risk of shunt-dependent hydrocephalus after occlusion of ruptured intracranial aneurysms by surgical clipping or endovascular coiling: a single-institution series and meta-analysis. Neurosurgery 61:924–933
Alen JF, Lagares A, Lobato RD, Gomez PA, Rivas JJ, Ramos A (2003) Comparison between perimesencephalic nonaneurysmal subarachnoid hemorrhage and subarachnoid hemorrhage caused by posterior circulation aneurysms. J Neurosurg 98:529–535
Author information
Authors and Affiliations
Corresponding author
Additional information
Comments
Siamak Asgari, Ingolstadt, Germany
In a retrospective study, Konczalla et al. reported about 68 patients with non-perimesencephalic subarachnoid hemorrhage who did not show any kind of bleeding source. All of them underwent two cerebral angiographies and one MRI of the cerebrum/cervical spine. Eighty-two percent of the patients experienced favorable outcomes. Twenty-seven percent of the patients developed cerebral vasospasm and 19 % of the patients suffered from delayed cerebral ischemia. Ten percent of the patients needed insertion of a CSF shunt. The authors presented a multivariate analysis pointing out Fisher grade 3 and patient age over 65 years as negative prognostic factors. This paper is of significant value for the neurovascular-interested readers and well-prepared. The authors had a database of over 1,188 patients with spontaneous subarachnoid hemorrhage available. Personally, I estimate an increasing number of patients with spontaneous non-perimesencephalic hemorrhage without visualizing a bleeding source in the recent years. Some of these bleedings occurred under systemic anticoagulation or dual platelet inhibition. The authors re-evaluate their data showing both an increasing number of non-aneurysmal SAH and patients treated with systemic anticoagulation or platelet inhibition. However, the rehemorrhage rate in these patients was very low (1.5 %).
Nicholas C. Bambakidis, Cleveland, USA
The authors analyzed factors influencing the clinical outcome in 68 patients suffering from non-aneurysmal and non-perimesencephalic (NPM) subarachnoid hemorrhage (SAH). The authors demonstrated that angiogram-negative and NPM-SAH had good prognoses. Patients with Fisher-type 3 bleeding were at risk for poor outcome like aneurismal SAH patients due to cerebral vasospasm and delayed cerebral ischemia. This is a large case series of angiogram-negative and NPM-SAH. We routinely repeat cerebral angiography on these patients and do not rely on CTA or MRA. Additionally, it is important to image the cervical spine with MRI to rule out spinal vascular malformation or other hemorrhagic lesions. As the authors point out, patients with large amounts of SAH are at risk of developing all of the usual complications of aneurysmal SAH and must be monitored and treated closely.
Rights and permissions
About this article
Cite this article
Konczalla, J., Schuss, P., Platz, J. et al. Clinical outcome and prognostic factors of patients with angiogram-negative and non-perimesencephalic subarachnoid hemorrhage: benign prognosis like perimesencephalic SAH or same risk as aneurysmal SAH?. Neurosurg Rev 38, 121–127 (2015). https://doi.org/10.1007/s10143-014-0568-0
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10143-014-0568-0