Abstract
Detailed outcome data for the management of anterior skull base fractures associated with cerebrospinal fluid (CSF) leakage is lacking. We present detailed follow-up data of a single-center study using a predetermined algorithm for the management of CSF leakage secondary to traumatic fractures. A number of 138 consecutive patients were included in the analysis; all patients underwent high-resolution computed tomography (CT) scanning at time of admission with β2-transferrin testing used to confirm CSF leakage. Patients with acute surgical indications were operated as emergent; leaks were repaired at the time of initial surgery in patients with intracranial pressure < 15 cm H2O. The remainder of the study population was managed conservatively including use of prophylactic antibiotics; lumbar drainage (LD) catheters were placed in those patients with leakage persisting beyond 48 h. Leaks lasting longer than 5 days underwent microsurgical repair using an intradural bicoronal approach. One-year follow-up assessment included evaluation of neurological status, Glasgow Outcome Scale (GOS), and repeat head CT. Twenty eight patients (26.9%) underwent emergent surgery, 15 of whom had simultaneous CSF leak repair, whereas 76 patients (73.1%) underwent delayed CSF leak repair between days 5 and 14. Postoperative meningitis rate was low (1.9%). Postoperative CSF leak (1.9%) was managed by intradural or transnasal endoscopic operation. Comparable rates of anosmia and frontal lobe hypodensities were seen in the surgical and conservatively managed subgroups. The presented algorithm, utilizing prophylactic antibiotics, trial of LD, acute and/or delayed intradural microsurgery, yields favorable outcomes. Large randomized controlled trials are needed to better define the role of prophylactic antibiotics and to better characterize the optimal timing and approach of surgical repair.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Approximately 25% of all patients with head injuries are presented with fractures of the anterior skull base [20]. These fractures remain a multidisciplinary challenge with respect to both diagnosis and management [18, 21, 23, 25]. Of patients with anterior skull base fractures, 12–30% will develop a cerebrospinal fluid (CSF) leak [10, 28]. Indications, approach, and timing of surgery as well as the use of prophylactic antibiotics remain controversial [6, 7, 11, 20].
In addition to the standard microsurgical bifrontal intradural approach [10, 20, 23], the endoscopic transnasal approach [9] and the subfrontal extradural approach [24, 25] have been increasingly employed in recent years for posttraumatic CSF leak closure. However, studies often do not provide standardized outcome measures or use accepted fracture classifications [22], making comparison between study populations difficult, thereby limiting generalizability.
The timing of operative intervention is controversial. Several authors favor immediate CSF leak closure [14], purportedly in order to minimize the risk of infection, while others prefer delayed surgery, citing spontaneous (<7 days) resolution of the CSF leaks in up to 85% of patients [3]. The appropriate use of prophylactic antibiotics is also debated. Opponents argue prophylactic antibiotics are ineffective and promote the development of multidrug-resistant bacteria [25], while proponents cite reduced rates of meningitis [6].
Unfortunately, detailed long-term clinical and neuroradiological outcome data is lacking [2, 3, 6, 8–10, 20, 23, 24]. Detailed outcome analyses are necessary to provide better evidence of the therapeutic effectiveness of these practices.
By examining detailed clinical and neuroradiological follow-up, this single-center study aims to analyze the efficacy of a proposed management algorithm for CSF leak associated with anterior skull base fractures.
Patients and methods
Patients
All patients with anterior skull base fractures and β2-transferrin-confirmed CSF leak treated between the years 1995 and 2005 at the Neurosurgical Department of the Medical University of Vienna, Austria were enrolled into this retrospective single-center study. All patients were treated according to a predetermined algorithm (Fig. 1). The study was approved by the institution’s ethics committee.
Diagnostics
In addition to the initial trauma evaluation for additional life-threatening injuries, a detailed neurological examination comprising the Glasgow Coma Scale (GCS) and the traumatic brain injury (TBI) classification (mild, moderate, severe) was performed on admission [5]. Patients with moderate or severe TBI were immediately transferred to the intensive care unit (ICU). Conscious patients performed the Valsalva maneuver to assess for occult CSF leak. In patients unable to cooperate and without elevation of intracranial pressure (ICP), careful bilateral compression of the jugular veins was used to provoke CSF leakage. In those patients with spontaneous or provoked rhinorrhea, the presence of the “double-ring sign” was evaluated at the bedside. Confirmatory β2-transferrin analysis was performed in all cases.
All patients underwent high resolution noncontrast computed tomography (CT) imaging (1-mm-thick sections with multiplanar reconstructions utilizing a bone reconstruction algorithm) at time of admission. Fractures were categorized according to the classification schema of Sakas et al. [22]: briefly, they define four major types of fractures: I—cribiform, II—frontoethmoidal, III—lateral frontal, and IV—complex fractures. Fractures with a maximum bone displacement of more than 1 cm in any plane were classified as “large” and those less than 1 cm as “small.” The classification allows for a direct correlation of fracture location, in particular, proximity to midline (Types I and II), and size with infection risk.
We obtained magnetic resonance imaging (MRI) if CT scans and β2-transferrin analysis was insufficient or indeterminate for purposes of preoperative planning for repair of intermittent or occult CSF leaks. Intrathecal fluorescein testing was used only introperatively during cases undergoing endoscopic repair.
All patients received prophylactic broad-spectrum antibiotics (Cefuroxime 1,500 mg, three times per day, for at least 7 days) or appropriate therapy as based on the antibiotigram of their nasal tampons [6].
Surgical indication and timing
The decision regarding initial conservative or surgical management was made according to the neurological condition of the patient and the radiological findings (Fig. 1).
We classified the patients into three groups:
-
Subgroup 1.
Patients with acute surgical indications (space occupying epidural, subdural, intraparenchymal hemorrhages, bone fragments with sizes >1 cm or dislocation, intracranial hypertension >20 cm H2O refractory to medical therapy, pneumaocephalus >2 cc) were operated on immediately according to the Guidelines of the “Traumatic Brain Injury Author Group:” [4] Wide decompressive craniectomies were performed in patients with intracranial space-occupying hemorrhages or cerebral swelling refractory to medical therapy. Bone fragments were removed or repositioned. In cases of frontal sinus fractures, the sinus was cranialized. In cases of tension pneumocephalus, the air was released, followed by watertight closure of the dura. Whenever possible, we tried to avoid and/or minimize resection of brain tissue. Patients received an external ventricular drain (EVD) with an intraparenchymal pressure sensor (drip chamber initially positioned at the level of the nasion, titrated for removal of no more than 150–200 ml/24 h). In patients with elevated ICP (>15 cm H2O) and intraoperative brain swelling, a two-step procedure with initial acute decompression followed by subsequent CSF leak closure was performed in an effort to limit additional retractor-related brain damage.
-
Subgroup 2.
Patients with severe/moderate TBI (GCS ≤ 13) without acute surgical indications (diffuse brain edema, extensive contusions) [4] were initially managed conservatively. Patients needing sedation received an EVD to enable ICP monitoring. Patients with persistent CSF leak ≥ 5 days underwent surgery between days 5 and 14 after clinical stabilization and normalization of ICP (<15 cm H2O).
-
Subgroup 3.
Patients with mild TBI (GCS > 13) without acute surgical indications [4] remained under clinical observation for 5 days. During this period, beds were kept in an semiupright position and patients were instructed to avoid activities associated with ICP elevation (e.g., coughing, sneezing, nose blowing). Patients were placed on a bowel regimen, including laxatives and stool softeners, to avoid unnecessary straining. In cases of persistent CSF leak ≥ 5 days, patients were brought for surgery between days 5 and 14.
Patients of subgroups 2 and 3 with spontaneous CSF leak closure before 5 days, including patients presenting with modest pneumocephalus (<2 cc), were followed conservatively.
Lumbar drains
Surgically managed patients received lumbar drainages (LDs) postoperatively. Conservatively managed patients received LDs only in cases of persistent CSF leak >48 h. Exclusion criteria for LD were elevated ICP (>15 cm H2O) or EVD. The LD drip chamber was initially positioned at the lumbar spine level, titrated to achieve removal of 150–200 ml of CSF per 24-h period.
Surgical technique
In all patients, CSF leak closure was performed using a standard microsurgical intradural bicoronal approach. A standard endoscopic transnasal approach was performed in selected cases of persistent postoperative CSF leak.
One-year follow-up
Neurological examination was performed together with Glasgow Outcome Scale (GOS) scoring and a follow-up CT scan at the time of 1-year follow-up. Follow-up CT scans were compared with the corresponding admission scan (preoperative scan in surgical patients; second scan after admission in conservatively managed patients); specific attention was paid to develop of new hypodensities in the frontal distribution. Together with olfaction preservation, these parameters were felt to represent a possible marker of iatrogenic parenchymal injury.
Statistics
Statistical analysis was performed to enable comparison of posttherapeutic GOS scores, cranial nerve palsies, and CT hypodensities between the surgical and the conservatively managed subgroups. The Fisher’s exact test was used to compare nominal variables. Data are presented as mean ± SD. A P value < 0.05 was considered significant. SAS 8.02 (SAS Institute, Cary, NC) software was used for all statistical procedures.
Results
A total of 158 patients were enrolled in the study; 138 patients (114 male, 24 female; 87.3%) were evaluated at 1-year follow-up (mean time 13.2 months).
Diagnostics
The CT fracture classification according to Sakas et al. [22] is shown in Table 1.
In 124 cases (89.8%), the CSF leak could be diagnosed using at least one of several bedside testing methods. 78 patients (56.5%) had spontaneous CSF leak without provocation. The Valsalva maneuver was performed in all 84 (67.8%) conscious patients and was macroscopically positive in 74 patients (88.1%). Bilateral compression of the jugular vein was performed in 31 unconscious patients (22.4%) with 19 positive results (61.3%). Double-ring sign examination was performed in 93 patients (67.4%) with spontaneous or provoked macroscopic rhinorrhea. Positive results were observed in 48 patients (48.8%). β2-transferrin analysis was performed in all 138 patients and positive in 129 cases (92.0% sensitivity). In 14 cases (10.2%), the diagnosis relied solely on β2-transferrin analysis and/or MR scans. In these cases, the patients and nursing staff were instructed to collect any drop of clear, watery fluid running down the nose or pharynx. In five of these patients (3.6%) with multiple fractures, additional MR scans were used to verify the site of the CSF leak. The intrathecal fluorescein test was used in two cases of persistent postoperative leak (1.4%), followed by endoscopic repair in the same session.
Surgical indication and timing
Seventy four patients (53.6%) were initially treated in the ICU. 104 patients (75.4%) were taken for surgery including 19 patients (18.3%) requiring optic nerve decompression. The epidemiological baseline data of each subgroup is presented in Fig. 2. Gender and age distributions were similar in the subgroups. There was a statistically significant increase in severe TBI in the conservatively managed subgroup (P = 0.0352). In the surgical subgroup, there was a significant increase in midline fractures (Sakas Type 1 and 2; P = 0.0007). In conservatively managed patients, Type 3 and 4 fractures were more common (P = 0.0007).
Lumbar drains
Seventy four patients (53.6%) received LDs (54 surgical patients vs. 20 conservatively managed patients). One out of 34 conservatively managed patients (2.9%) developed meningitis.
Surgical technique
Persistent postoperative CSF leak was observed in two out of 104 surgical patients (1.9%), both with large Type I fractures. Due to unsealed fractures within the sphenoid sinus, those two patients required reoperation using a transnasal endoscopic approach which was successful in stopping the leak. Two patients (1.9%) required reoperation for epidural or subdural hemorrhage. Two patients (1.9%) developed postoperative meningitis (one each Type I and II). No postoperative brain abscess was observed in the present series.
One-year follow-up
The GOS scores were as follows (Fig. 2): 60.8% of the patients showed excellent recovery with GOS scores of 5 (72 surgical vs. 12 conservative patients; P = 0.09). 8.7% of the patients had GOS scores of 4 (4 surgical vs. 8 conservative patients; P = 0.004). 16.7% of the patients suffered from considerable deficits with GOS scores of 3 (21 surgical patients vs. 2 conservative patients; P = 0.10). Of all patients, 3.7% were severely disabled with GOS scores of 2 (5 surgical vs. 0 conservative; P = 0.34). There were 14 deaths (10.1% of the patients), all of whom had severe TBI (2 surgical vs. 12 conservative patients; P < 0.0001). The subgroup analysis of the GOS scores is shown in Fig. 2. Analyzing subgroup 1 regarding surgical timing, the comparison of one-step surgery vs. delayed two-step surgery did not show statistically significant differences with respect to excellent clinical outcomes (GOS 5, P = 0.151) or the endpoint death (GOS 1, P = 1.0).
The incidence of cranial nerve palsies and CT hypodensities of the surviving patients (surgery n = 102, conservative n = 22) is shown in Table 2: four patients had Type IV fractures; the remainder of the study population consisted of Type I or II fractures. Radiological follow-up demonstrated altogether 23 frontal lobe hypodensities: 14 in patients with severe TBI, seven in patients with moderate TBI, and two in patients with mild TBI.
Discussion
Diagnostics
Our data demonstrate the high clinical value of simple bedside tests with successful CSF leak detection in 89.8% of all cases. β2-transferrin analysis combined with CT scanning is helpful in cases of chronic, intermittent, or occult CSF leak. β2-transferrin offers a sensitivity and specificity approaching 98% [17]. In the present series, CSF leak diagnosis was based primarily on β2-transferrin in only 10.2% of patients. Therefore, it may not be obligatory for routine CSF leak screening.
The neuroradiologic gold standard for the detection and characterization of skull fractures is high-resolution CT. It provides a sensitivity of 88% for the visualization of the bony defects responsible for CSF leak [3] and also allows for fracture classification used for operative planning and risk assessment [1, 15, 16, 22]. Based on an analysis of 48 patients, Sakas et al. [22] introduced a fast and effective classification showing direct correlation of fracture location close to the midline (Type I and II) and size (large > 1 cm) with complication risks. Comparing our data to Sakas et al., we found considerably higher rates of midline Type I fractures (30.4% vs. 14.5%), complex Type IV fractures (42.1% vs. 33.3%), and large fracture displacements (60.4% vs. 69.5%) as well as minimized infection rates (31.3% vs. 2.1%). Our low meningitis rate despite a higher percentage of high risk/complex cases may be the result of our use of prophylactic antibiotics.
In addition to CT scans, MRI (particularly T2-weighted sequences), are useful for the diagnosis of delayed, intermittent or occult CSF leak, as well as complications such as meningitis or brain abscess [7]. A recent study of MRI cisternography showed 88% sensitivity for CSF leak detection [29]. It is therefore a valuable tool for noninvasive diagnosis in the subacute or chronic state. In the present series, it was used in five cases with multiple fracture lines to verify the site of leakage. The intrathecal fluorescein assay is a precise but highly invasive tool, with a sensitivity of approaching 97% [29]. Its major disadvantage is the potential of severe complications including seizures in up to 0.75%. Therefore, it should likely be reserved as a diagnostic tool of last resort [29]. We only utilized intraoperative fluorescin testing during endoscopic CSF leak repair in two cases with persistent postoperative CSF leak.
Surgical indication and timing
Surgical indications and timing are the subject of much debate as demonstrated by multiple recently published management strategies. (Table 3). Several authors suggest treating any CSF leak as soon as possible, with the rationale that early intervention may minimize the risk of subsequent infections [14]. Many others favor conservative management initially [3, 6, 7, 9–11, 20, 23, 25, 27, 28], citing a high rate (approximately 50%) of spontaneous CSF leak closure. Previous papers have not yet contained detailed clinical and radiological outcome data with standardized criteria for surgical timing. The present algorithm outlines an initial conservative approach and/or delayed CSF leak closure for patients without acute surgical indications and patients with acute surgical indications and high ICP.
As mentioned above, many authors also prefer direct closure of the CSF leak only if adequate intraoperative control of ICP and cerebral edema can be obtained. They do not favor a two-step strategy with initial acute operation followed by delayed fistula closure. Additionally, they do not discuss precise indications for such a staged management [6, 10, 23]. With our proposed cut-off ICP value (15 cm H2O), we have tried to introduce an objective criterion for a staged operative strategy. The rationale for that cut-off value was based on our clinical experience of more difficult and traumatic surgery when ICP exceeds 15 cm H2O. Unfortunately, we cannot as yet prove the superiority of this strategy as the skewed distribution of severe TBI in conservative vs. surgical subgroups may bias our evaluation. Statistically comparable clinical outcomes of the patient populations of subgroup 1 managed with one- or two-step surgery appear to show the safety of this staged management strategy without additional risks for the patients resulting from a second intervention.
A postulated disadvantage of delayed surgery is an exponentially higher infection rate after 1 week [20, 24, 25]. This evidence led to our rationale to limit the conservative treatment trial to 5 days. As already discussed, we may have overcome this drawback with our strategy of prophylactic antibiotics, finding a very low rate of meningitis (2.9% conservative vs. 1.9% surgical group), despite the high percentage of higher risk Type I and II fractures. However, the use of prophylactic antibiotics remains controversial. Opponents of this strategy argue that antibiotics are ineffective and widespread use increases the proliferation of multidrug-resistant bacteria. Many centers do not initiate antibiotic therapy unless the patient develops a clinically evident infection. Our experience would seem to compare favorably with the literature (prior published postoperative meningitis rates ranging as high as 31.1%) [6, 22]. Nonetheless, prospective randomized trials are needed to further clarify this controversial issue.
Surgical techniques
Microsurgical intradural bicoronal approach
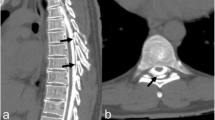
In addition to the continuing debate surrounding selection criteria and timing of surgery in this population, the ideal operative approach also engenders much discussion (Table 3). The microsurgical intradural bicoronal approach provides superb exposure of the entire anterior skull base extending from the lateral aspects of the sphenoid wings and the anterior clinoid processes to the sellar and parasellar regions (Fig. 3). Another advantage of the intradural approach is the ability to achieve hematoma evacuation and/or cerebral decompression while also attempting to seal the CSF leak within one surgical session. In the present study, the CSF leak was sealed within the same procedure in the majority of the acute patients (53.5% subgroup 1).
Microsurgical intradural bicoronal approach. After appropriate positioning, a bicoronal skin incision behind the hairline is performed (a). b The preparation of the vascularized galea-periosteal flap. The next step after the osteoplastic bilateral frontal craniotomy reaching the anterior skull base is the planned cranialization of the frontal sinus with complete removal of the sinus mucosa (c). Special attention is paid to the preservation of the olfactory nerves by microsurgical meticulous sharp dissection using a “no-touch” technique. Brain retraction is minimized. The microscopic localization of the bilateral CSF leaks (d, f) together with the corresponding bone window CT scan (e), with bilateral multiple anterior skull base fracture lines and pneumocephalus
Detractors of the intradural approach cite the potential of retractor-related brain damage and olfactory nerve damage. In our series, we aimed to minimize intraoperative brain damage by delaying CSF leak closure in patients with high initial ICP (>15 cm H2O). In those with nontraumatic lesions it is felt that olfaction can be preserved in nearly all patients [26].
In order to objectively assess for surgery and trauma-related olfactory nerve damage, we compared anosmia/hyposmia rates within the surgically and conservatively managed patients. Our nearly equivalent hyposmia rates (surgery 29.4% vs. conservative 27.3%; P = 0.26) weaken the argument that there is an increased risk of olfactory nerve damage with an intradural approach. We feel the similar rates of olfactory preservation further support our strategy of delayed CSF leak repair. Another main factor in olfaction preservation is our use of sharp dissection of both olfactory tracts within their arachnoid layer, avoiding the use of bipolar coagulation, in an effort to preserve the vascular supply. Any pressure or tension-related mass effect upon the olfactory tract should also be corrected during surgery.
Together with olfaction preservation, CT hypodensities within the frontal lobes may also serve as possible markers for retractor-related brain damage. Of course, other factors, such as late apoplexia or secondary axonal injury, limit the specificity of that parameter. In our study population, the 1-year follow-up CT scan showed a comparable rate of new frontal lobe hypodensities in surgical (3.9%) and conservatively managed patients (4.5%; P = 1.0). Therefore, we suspect that the comparable rates of hypodensities reflect resolving primary contusional injury of the frontal lobes and may have no significant relationship to the use of the microsurgical intradural bicoronal approach.
Our low rates of postoperative infection (1.9%) and postoperative persistent CSF leak (1.9%) are equivalent or even favorable when compared to the endoscopic or extradural approach.
Transnasal endoscopic approach
The transnasal endoscopic approach is widely used as the first-line approach for CSF leak closure. Recent series have shown success rates from 86% to 100% for nontraumatic CSF leak closure with a low rate of postinterventional meningitis (approximately 1%) [8, 13, 28]. Unfortunately, these studies did not give specific data on patient selection and postoperative anosmia rates. Indeed, nearly no follow-up data exists, which focuses on the success rates and outcomes of this approach for traumatic lesions alone.
In 2006, Basu et al. described the major limitation of the transnasal endoscopic approach [2]: far lateral lesions cannot be reached. Additional limitations include repair of CSF leaks >1 cm and compounding factors such as intracranial hypertension and patient obesity. Despite these shortcomings, this minimally invasive approach can be very useful in patients without acute surgical indications and low ICP presenting with small and/or delayed CSF leaks from Type I or II fractures located near midline. In the present study, the endoscopic approach was successfully used after incomplete intradural repair on small, persistent CSF leaks in two patients. Whereas most of the initial multiple, large and lateral fracture lines were sealed by first-line intradural repair, the residual leaks confined to the sphenoid sinus were well visualized by fluorescein and successfully sealed endoscopically.
Extradural subcranial approach
In patients without intracranial hypertension or intradural pathologies, the extradural subcranial approach is a reasonable alternative. Unfortunately, specific outcome data for the use of this approach in the management of traumatic lesions is limited [19, 24]. Postoperative meningitis rates are estimated at about 1%, with persistent CSF leaks occurring in about 2.8–3%. Before undertaking the present, consecutive series we frequently used this approach. However, in our experience, there are several limitations to the extradural approach, the most important of which may be that a one-step procedure for surgical repair of intradural lesions is not always feasible. During the operative approach, the dura mater may be torn, making identification of the “original” traumatic defect more difficult. Technically, the closure of the defect can be rather challenging, often necessitating increased brain retraction and resulting contusional-type injury. Additionally, this approach does not provide control over intradural complications, such as iatrogenic intraoperative hematoma, that are more common in the early posttraumatic period. Recently, a combination of the extradural and intradural approach was suggested for subacute patients [25].
Summarizing the data on operative approaches, there are clearly advantages and disadvantages of each one and likely several equivalent solutions (Table 3). The available data remains insufficient to justify general treatment recommendations. Prospective randomized studies are needed to answer these questions. In our opinion, the ideal approach depends mainly on the clinical state of the patient (acute, subacute, chronic) and the location and extent of the fracture. Fracture classification schema [22] should be applied more often as they may be help to tailor the approach on more selective basis.
Clinical outcome
Mortality and GOS
Our clinical outcome data also suggest the efficacy of the proposed management algorithm: in patients with moderate/mild TBI mortality was 0%, versus 15% mortality in this population seen in a recently published meta analysis [5]. Excellent clinical outcome (GOS 5) was observed in 36.5% of the patients with severe/moderate TBI. This compares favorably to the data reported in the literature which ranges from 12% to 35% [5]. This data is derived from large multicenter trials of TBI patients, irrespective of fracture location or CSF leakage, whereas the present study focused on a more well-defined patient subgroup. This of course limits direct comparison. Nevertheless, the authors believe that these considerable differences may not be entirely explained by differences in inclusion criteria.
Cranial nerve palsies
The present rates of posttraumatic visual deficits of 22.5% are similar to previously published data ranging from 16% to 30% [12]. The considerably higher percentage of visual deficits in the surgical subgroup is felt to be due to the increased numbers of extensive skull base fractures resulting in optic nerve compression necessitating operative repair of the skull base defects. Our incidence of oculomotor and abducens nerve palsies corroborate the findings of significantly higher occurrence of cranial nerve involvement in severe TBI [12]. Interestingly, nearly all cranial nerve palsies were observed in Type I and II fractures, i.e., fractures located in or around midline.
In conclusion, we present a single-center trial using a predetermined management algorithm for the management of CSF leakage associated with anterior skull base fractures, which utilizes acute and/or delayed intradural and endoscopic surgery, conservative treatment with or without LD, and prophylactic antibiotics. Our algorithm resulted in excellent clinical outcomes with respect to overall mortality, functional outcomes, cranial nerve palsies, and meningitis. Surgical and conservatively managed patients showed comparable rates of posttraumatic anosmia and CT-visualized frontal lobe hypodensities. Given the similar rates, we suspect the majority of these new hypodensities to be the result of evolving primary contusional injury and not retractor-related injury secondary to the intradural bicoronal approach. The management of anterior skull base fractures associated with CSF leak remains controversial. Debate continues around the role of prophylactic antibiotics, early identification of injury patterns unlikely to heal with conservative management, timing of CSF leak closure, and the ideal operative approach. These issues should be addressed by large, multicenter randomized controlled trials.
Limitations
There are many factors limiting the power of this study. It is a nonrandomized single-center crossover trial without a control group. The small sample size, especially the low number of cranial nerve palsies, limits the statistical power of this study. The surgical procedures were performed by different surgeons. The conservative and surgical subgroups were different with regard to the fracture locations and classification patterns and the severity of TBI. Additionally, while antiobiotics were used in all patients, therapy was tailored to the sensitivities of culture-documented organisms, possibly introducing additional bias.
References
Bächli H, Leiggener C, Gawelin P, Audige L, Enblad P, Zeilhofer H, Hirsch J, Buitrago-Tellez C (2009) Skull base and maxillofacial fractures: two centre study with correlation of clinical findings with a comprehensive craniofacial classification system. J Craniomaxillofac Surg 37:305–311
Basu D, Haughey B, Hartman J (2006) Determinants of success in endoscopic cerebrospinal fluid leak repair. Otolaryngol Head Neck Surg 135:769–773
Bell R, Dierks E, Horner L et al (2004) Management of cerebrospinal fluid leak associated with craniomaxillofacial trauma. J Oral Maxillofac Surg 62:676–684
Bullock M, Chesnut R, Ghajar J et al (2006) Surgical management of traumatic brain injury author group: guidelines for the surgical management of traumatic brain injury. Neurosurgery (Suppl march) 58:1–24
Chesnut R, Jamshid G, Maas A et al (2000) Glasgow coma scale score. In: Part II, Management and prognosis of severe traumatic brain injury. Brain trauma foundation. Available at: http://www2.braintrauma.org/guidelines/downloads/btf_guidelines_management.pdf
Friedman J, Ebersold M, Quast L (2001) Post-traumatic cerebrospinal fluid leakage. World J Surg 25:1062–66
Georgantopoulo A, Hodgkinson P, Gerber C (2003) Cranial-base surgery: a reconstructive algorithm. Br J Plast Surg 56:10–13
Hegazy H, Carrau R, Snyderman C et al (2000) Transnasal endoscopic repair of cerebrospinal fluid rhinorrhea: a meta-analysis. Laryngoscope 110:1166–1172
Katzen J, Jarrahy R, Eby J et al (2003) Craniofacial and skull base trauma. J Trauma 54:1026–1034
Kral T, Zentner J, Vieweg U et al (1997) Diagnosis and treatment of frontobasal skull fractures. Neurosurg Rev 20:19–23
Kruse J, Awasthi D (2006) Skull-base trauma: a neurosurgical perspective. J Craniomaxillofac Trauma 4:8–14
Kulkarni A, Aggarwal S, Kulkarni R et al (2005) Ocular manifestations of head injury: a clinical study. Eye 19:1257–1263
Locatelli D, Rampa F, Acchiardi I et al (2006) Endoscopic endonasal approaches for repair of cerebrospinal fluid leaks: nine-year experience. Neurosurg [ONS Suppl 2] 58:246–257
Loew F, Pertuiset B, Chaumier E et al (1984) Traumatic, spontaneous and postoperative CSF rhinorrhea. In: Symon L (ed) Advances and technical standard in Neurosurgery, vol 11. Springer, Wien, pp 169–207
Madhusudan G, SharmaR KN, Tewari M (2006) Nomenclature of frontobasal trauma: a new clinicoradiograpic classification. Plast Reconstr Surg 117:2382–2388
Manson P, Stanwix M, Yaremchuck M, Nam A, Hui-Cou RE (2009) Frontobasal fractures: anatomical classification and clinical significance. Plast Reconstr Surg 124:2096–2106
Oberascher G (1988) A modern concept of cerebrospinal fluid diagnosis in oto- and rhinorrhea. Rhinology 26:89–103
Probst C (1990) Neurosurgical treatment of traumatic frontobasal CSF fistulae in 300 patients. Acta Neurochir 106:37–47
Raveh J, Viullemin T (1988) The surgical one-stage management of combined cranio-maxillo-facial and frontobasal fractures. Advantages of the subcranial approach in 374 cases. J Cranio-Maxillofacial Surg 16:160–172
Rocchi G, Caroli E, Belli E et al (2005) Severe craniofacial fractures with frontobasal involvement and cerebrospinal fluid fistula: indications for surgical repair. Surg Neurol 63:559–563
Rousseaux P, Scherpereel B, Bernard M et al (1981) Fractures of the anterior skull base. Our therapeutical approach in 1254 cases in a series of 11200 head trauma cases [in French]. Neuro-Chirurgie 27:15–19
Sakas DE, Beale D, Whitwell H, Whittaker K, Krabs A, Abbasi K, Dias P (1998) Compound anterior cranial base fractures: classification using computerized tomography scanning as a basis for selection of patients for dural repair. J Neurosurg 88:471–477
Samii M, Tatagiba M (2002) Skull base trauma: diagnosis and management. Neurol Res 24:147–156
Schaller B (2005) Subcranial approach in the surgical treatment of anterior skull base trauma. Acta Neurochir 147:355–366
Scholsem M, Scholtes F, Collignon F et al (2008) Surgical management of anterior cranial base fractures with cerebrospinal fluid fistulae: a single-institution experience. Neurosurgerz 62:463–469
Sepehrnia A, Knopp U (1999) Preservation of the olfactorian tract in bifrontal craniotomy for various lesions of the anterior cranial fossa. Neurosurgery 44:198–206
Talamonti G, Fontana R, Villa F et al (1995) “High risk” anterior skull base fractures. Surgical treatment of 64 consecutive cases. J Neurosurg Sci 39:191–197
Wax M, Ramadan H, Ortiz O et al (1997) Contemporary management of cerebrospinal fluid rhinorrhea. Otolaryngol Head Neck Surg 116:442–449
Zaplac J, Marple B, Schwade N (2002) Skull base cerebrospinal fluid fistulas: a comprehensive diagnostic algorithm. Otolaryngol Head Neck Surg 126:669–676
Conflicts of Interest
None
Author information
Authors and Affiliations
Corresponding author
Additional information
Comments
Christopher Nimsky, Marburg, Germany
The management of anterior skull base fractures is still quite variable ranging from an aggressive approach to perform surgery in case of intracranial air inclusion without CSF leak up to more conservative approaches including the application of lumbar drainage in case of definitive CSF leakage. The authors have analyzed a large group of patients which were treated by a predefined algorithm. They could demonstrate a favorable outcome and their paper adds valuable information for the still controversial management of anterior skull base fractures. Whether late sequelae of anterior skull base fractures like meningitis and brain abscess are also rare are hopefully documented in an upcoming long follow-up study of these patients.
Peter S. Amenta, Jack I. Jallo, Philadelphia, USA
Sherif et al. present a detailed and methodical treatment algorithm for the management of cerebrospinal fluid (CSF) leaks associated with fractures of the anterior skull base. In doing so, the authors address the controversial topics of prophylactic antibiotics, the indications and timing of surgery, and the optimal surgical approach to these CSF leaks. The authors report excellent clinical outcomes including a low mortality rate, a final Glasgow Outcome Scale (GOS) of 5 in 36.5% of patients, a cranial nerve palsy incidence consistent with previously published data, and a low incidence of meningitis. Despite these exceptional outcomes, as the authors point out, a tremendous amount of uncertainty remains in regard to the appropriate management strategy for anterior skull base fractures and CSF leaks. As a result, we believe this study makes its greatest contribution to the literature because it details a systematic approach to a pathologic entity for which little standardization in management currently exists.
The management of anterior skull base fracture CSF leaks is largely dependent on the practice patterns of an individual institution and the familiarity of the surgeon with a particular procedure. Thus, it is difficult to compare results from multiple studies, as there is significant variability between management practices. Further complicating the interpretation of results is the wide spectrum of pathology and clinical presentations encountered in the traumatic brain injury population. CSF leaks associated with operative hematomas are more likely to be treated immediately during the initial emergent surgery than CSF leaks in patients with severe diffuse injury better suited to medical management.
As mentioned above, this paper represents an important addition to the literature because it lays the groundwork for a systematic approach to a problem for which there is little consensus. Additionally, it highlights the fact that there are multiple logical and legitimate approaches to managing these injuries. This finding was particularly evident in the equivalent incidences in frontal lobe hypodensities and hyposmia rates seen in the intradural and delayed repair groups. As always, the comfort level and surgical skill of the surgeon represent important variables. To further develop a consensus on the management of anterior cranial base fractures and associated CSF leaks, prospective multicenter trials including larger sample sizes of open surgical and endoscopically treated patients will be needed.
Raimund Firsching, Magdeburg, Germany
The authors Camillo et al. report their 10-year observations from a series of 138 patients with a frontobasal fracture and associated cerebrospinal fluid (CSF) leak. Their regimen is specified in detail and they conclude their results in terms of frequency of postoperative CSF leaks, meningitis, and anosmia reflect “favorable outcomes.”
The authors are to be congratulated, because they highlight most of the controversies that remain unresolved and in need of discussion. They based their clinical management on an algorithm that raises a number of questions:
• Patients with a Glasgow Coma Scale (GCS) sum score of <14 must be managed on the Intensive Care Unit (“obligatory”) in the authors’ view. This may involve patients who are fully conscious as this score may involve a number of neurological combinations. There must be generous resources to offer a place qualified for artificial respiration to these patients.
• The authors suggest to refrain from operating when the CSF leak is not noted after day 5 after the injury. This is a debatable view, because a CSF leak may persist without being apparent, as the CSF may pass down the pharynx not noted by the patient nor the doctor. As a late life-threatening meningitis may occur even many years later for the first time, there are strong arguments to expose and solidly seal the hole in the dura revealed by imaging that had caused the 5-day rhinorrhea. The assumption, a lumbar drainage will do the job, is another view not based on firm evidence and possibly not common practice of the majority of our colleagues.
• In patients with a low GCS sum score, the authors base their indication on the timing of surgical repair on the invasively recorded intracranial pressure (ICP) levels, which are to be lower than 15 mmHg to avoid too much pressure from the spatula on the frontal lobe during surgical repair of the hole in the dura. This is one way of solving this issue, a less invasive option were to decide timing on the neurological findings of the patient. When sedatives are not given prophylactically and not in a dosage causing coma but tailored to only ensure adequate ventilation and wake up tests are conducted regularly, it should be possible to note the emergence from coma in almost all cases. From experience, it is highly unlikely that the noncomatose patient will have ICPs elevated to a relevant level, and spatula will do no additional harm.
• The authors distinguish patients with small amounts of air of less than 2 cc (cm³) intradurally, in whom they see no need for surgical repair of the dura, from patients with larger amounts of air, in whom they recommend surgical repair. To the best of our knowledge, the amount of air has never been related to the occurrence of posttraumatic meningitis, and the assumption that small amounts of air were associated with spontaneous healing of the dura is not really evidence-based.
• The authors suggest endoscopic repair of the dura in patients with a persisting CSF leak after surgical repair. It is true that there are some authors recommending this endoscopic option. The long-term results of sealing with fibrin glue using an endoscopic approach, however, appear to be particularly scarce in the literature. The treacherous occurrence of late meningitis is occasionally seen by experienced neurosurgeons but hardly reported in the literature, and it cannot be ruled out by the experience gained from 138 patients.
Obviously there are many ways to fix frontobasal fractures associated with a CSF leak. We have to be grateful to the authors, who have presented this wide variety of options and unresolved controversies of this particular field of neurosurgery.
Rights and permissions
About this article
Cite this article
Sherif, C., Di Ieva, A., Gibson, D. et al. A management algorithm for cerebrospinal fluid leak associated with anterior skull base fractures: detailed clinical and radiological follow-up. Neurosurg Rev 35, 227–238 (2012). https://doi.org/10.1007/s10143-011-0352-3
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10143-011-0352-3