Abstract
Bow hunter's syndrome (BHS) is defined as symptomatic, vertebro-basilar insufficiency caused by mechanical occlusion of the vertebral artery (VA) at the atlanto-axial level during head rotation. In the literature, about 40 cases have been reported. However, due to the rarity of this pathology, there are no guidelines for diagnosis and treatment. Conservative, surgical, and endovascular concepts have been proposed. In order to work out an algorithm, we performed a systematic review of the literature and a retrospective analysis of patients, which have been treated in our institutions over the last decade. The clinical series was comprised of five patients. The symptoms ranged from transient vertigo to posterior circulation stroke. Diagnosis was established by dynamic angiography. In all patients, the VA was decompressed; one patient required additional fusion. The clinical and radiological results were good, and the treatment-related morbidity was low. The literature review demonstrated that Bow hunter's syndrome is a rare pathology but associated with a pathognomonic and serious clinical presentation. The gold standard of diagnosis is dynamic angiography, and patients were well managed with tailored vertebral artery decompression. By this management, clinical and radiological results were excellent and the treatment-related morbidity was low.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Bow hunter's syndrome (BHS) is defined as symptomatic, vertebro-basilar insufficiency caused by mechanical occlusion of the vertebral artery (VA) at the atlanto-axial level during head rotation. The term was coined by Sorensen in 1978 based on observations in a patient becoming symptomatic during archery [38]. In this patient, the management was conservative [38]. Meanwhile, about 40 similar cases have been reported in the literature [33]. However, due to the rarity of this pathology, there are no guidelines for diagnosis and treatment. Conservative, as well as surgical and, more recently, endovascular concepts have been suggested.
In the present paper, we report our experience with the surgical management of five patients treated over more than one decade. Additionally, and based on a thorough review of the literature, we carefully suggest a management algorithm.
Material and methods
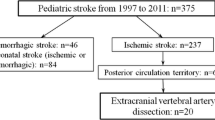
First, a retrospective analysis of patients with Bow hunter's syndrome who were treated over the last decade in two tertiary care centers with special interest in cerebro-vascular pathology was performed. The medical records and neuro-imaging data were analyzed. Second, an extensive review of the literature was conducted based on Medline. We searched for articles in English language but without time restriction and using the following key words: vertebral artery, compression, rotational/ positional occlusion, vertebro-basilar insufficiency, Bow hunter ('s) syndrome/ stroke.
Results
Our population was comprised of five patients. There were four men and one woman, with ages ranging from 8–46 years (mean age 24.2). The main symptoms were vertigo and visual blur during head rotation to one side. Extreme rotation regularly induced syncope. One patient presented with a posterior circulation infarction (patient #1). The patient's characteristics as well as treatment and outcome are summarized in Table 1.
Diagnosis was established in all patients by dynamic digital subtraction angiography (dDSA). This allowed assessment of the vertebral artery filling during defined head movements (rotation, flexion/ extension, and lateral bending). In all patients, an extrinsic VA compression could be documented for the head position, which induced the syncope. The compression site was always located at the atlanto-axial level. In all cases, the compressed VA was the dominant one, and head rotation towards the contra-lateral side provoked the occlusion. Furthermore, posterior communicating arteries were generally hypo- or aplastic providing no collateral flow from the anterior circulation. Four patients were operated on by an antero-lateral approach and decompression of the VA was realized; in one patient (#3), a bilateral approach was realized because of a complex combined vascular and bony malformation. One patient (#2) was decompressed via a posterior approach, and simultaneous occipito-cervical fusion (C0–C2) was performed because of a pre-existing instability. No serious complication was encountered. All patients improved clinically and became free of syncopes. Early control dDSA confirmed good permeability of the decompressed arteries even in extreme rotation.
Illustrative case (patient #5)
A 46-year-old female patient had progressive neck pain, vertigo, and visual symptoms. During head rotation to the right, she fainted. The diagnosis of Bow hunter's syndrome was established by dDSA. Vascular decompression was realized by a left antero-lateral approach. Postoperatively, the syncopes disappeared. The early control dDSA showed permeability of the decompressed VA (Fig. 1).
Computed tomography (a, c–e) and dynamic angiography (b, f). Pre-operative CT angiography (a) may localize the site of compression. Left vertebral angiogram (b) with the head rotated 90° to the right showing complete interruption of the flow at the atlanto-axial level. Postoperative CT, sagittal view, showing the course of the left VA (red dots) and the sites of decompression (c); note: decompression behind the massa lateralis of atlas (d1), partial transversectomy of atlas (d2), and axis (e3). Postoperative dynamic angiogram of the left VA with the head rotated to the right showing good patency (f)
Discussion
Etiology and pathophysiology
Based on the original description by Sorensen, Bow hunter's syndrome is defined as symptomatic vertebro-basilar insufficiency by mechanical occlusion of the vertebral artery at the atlanto-axial level during contra-lateral head rotation [38]. A similar clinical presentation may occur in case of a subaxial stenosis of the vertebral artery with ipsilateral head rotation [2, 8, 12, 17, 28, 32, 42]. Because pathogenesis and treatment strategy differ between these two entities, the latter were not the focus of the present article. However, for clear distinction, we suggest to introduce the terms atlanto-axial BHS and subaxial BHS. Finally, a mixed type may be distinguished, consisting of a bilateral VA stenosis, one at C1/C2, and the other at the subaxial level as in one case reported by Kimura et al. [25].
Numerous etiologies have been reported for VA compression at the atlanto-axial level, such as bony and/or vascular malformation [3, 26, 34, 36, 40], constriction at the dural entry point [1], instability [10], trauma (e.g., sport, accident, chiro-practice) [7], degeneration (e.g., spondylosis) [9], and systemic diseases (e.g., M. Paget, rheumatoid arthritis) [21]. In some cases, the etiology was supposed to be “idiopathic”; however, intra-operative exploration found “fibrous bands” constricting the VA [12, 19, 20, 26, 28, 30]. Those bands are thought to develop from fibrous transformation of small neck muscles or be part of thickened atlanto-axial membrane. Sometimes, they are the only pathological intra-operative findings such as in one patient of our series (patient #5).
Generally, VA compression due to congenital bony anomaly presents in the pediatric population. Other etiologies, which are acquired, may present later on.
The vascular pattern typically comprises a dominant VA which is compressed at the C1/C2 level by contra-lateral head rotation. Exceptionally, compression in a non-dominant VA ending as PICA has been reported [29]. Typically, in all cases, there is no collateral flow through the anterior circulation.
Management
Although symptoms of BHS are pathognomonic, all patients in our series had delayed diagnosis. Because untreated BHS may progress to posterior circulation infarction, even in children, such as in the youngest patient of our series (patient #1), preventive treatment is indicated [26, 37]. The presumed mechanisms are hemo-dynamic and/or thromboembolic because of endothelial damage by repetitive shear stress. Treatment options vary from conservative to surgical possibilities and more recently endovascular procedures [23, 39]. In order to schematize the management, we propose a simple algorithm (Fig. 2). Each part will be discussed in the next section.
Management algorithm for atlanto-axial Bow hunter's syndrome. The first line depicts the successive diagnostic steps (from left to right). First, Bow hunter's syndrome should be clinically diagnosed. Next non-invasive examinations should be realized. The golden standard of diagnosis is dynamic angiography. Depending on etiology and pathophysiology of the compression and operability (second line), different treatment options exist (third line). The algorithm is discussed in detail in the chapter “Discussion”
Diagnosis
Although clinical presentation of BHS is typical for vertebro-basilar insufficiency, the diagnosis may sometimes be delayed. The pathognomonic finding is that the symptoms occur during head rotation and extension and disappear when the head is turned back into neutral position.
Once BHS is clinically suspected, the mainstay of diagnosis is dDSA [3, 4, 26, 29]. A vertebral angiogram with the head turned into stress position (contra-lateral rotation and extension) will unequivocally prove the occlusion (Fig. 1b). A four-vessel cerebral angiography is important to assess anatomical variations, collateral flow, and eventually associated stenosis [13, 14, 23, 26]. This may be preceded by non-invasive examinations, such as magnetic resonance imaging (MRI) to document any ischemic event and computerized tomography (CT) and its variants (3D-CT and CT angiography). In our experience, CT angiography with reconstructions has given very precise information about compressing elements and the topographical relationships between artery and bone [31, 43, 44] (Fig. 1a). A dynamic cervical radiography may disclose any instability. Furthermore, pre-operative transcranial Doppler sonography (TCD) [24, 42] and electro-physiological examinations (brain stem auditory evoked response (BS-AER), motor-evoked potentials (MEP), somato-sensory-evoked potentials (SSEP)) may be valuable and serve as base-line for intra-operative monitoring [41].
Surgical treatment
Including the five patients of the present series and those of Netuka's review, 34 surgically treated cases of atlanto-axial BHS have been reported in the literature [33]. There were 11 fusions (32.4%), 17 decompressions from posterior (50%) and 6 from anterior or antero-lateral (17.6%) (Table 2).
Surgical decompression of the VA at the C1/C2 level has to be considered as the causal treatment of this pathology [26]. In the present series, an antero-lateral approach was realized in all, except one patient (Fig. 3). The surgical anatomy and further technical details may be found in previous reports [5, 14–16]. In brief, the atlanto-axial complex was approached antero-laterally. The VA was proximally and distally controlled. A partial transversectomy of C1, and if indicated, C2, were performed (Fig. 1c–e). Additionally, the decompression was tailored to the patient's specific anatomy to release any fibrous and/or bony compressive element. In patient #3, a bilateral antero-lateral approach was performed. This allowed treating a combined vascular/bony anomaly on one side and a bony anomaly on the other side. Intra-operatively, antero-lateral fibrous bands were found, which might have been missed via a posterior approach. We hypothesize that the presence of such antero-lateral fibrous bands, which are not identifiable on pre-operative imaging, may explain some surgical failures using a posterior midline approach as reported by Matsuyama et al. [30].
a–h Mechanism of vertebral artery compression at the atlanto-axial level. Artist's illustration showing the left VA with the head in neutral position (a, left); during head rotation to the right, the VA is physiologically stretched; however, in case of additional elements such as bony/vascular malformations or constricting fibrous bands, the artery may become externally compressed (a, right). Vertebral artery decompression by a left antero-lateral approach: the patient is positioned supine, Doppler monitoring is installed, and base-line values are recorded (b). Then, the head is slightly extended and turned to the contra-lateral side. The skin incision is at the anterior border of the sterno-cleidomastoid muscle (SCM) (c). The field between SCM and the Jugular vein is opened leading to the antero-lateral spine (d). Next, the tubercle of the atlas and the transverse process of the axis are identified as osseous landmarks (e). The vertebral artery is then identified and released of any muscle and fibrous elements between C1 and C2 (f). In order to achieve optimal decompression, partial transversectomy of C1 may be performed (g). In some cases, a partial transversectomy of C2 may be necessary. The second cervical nerve root may be sacrificed, if it appears to be compressive (green loop). The result of surgical release may be verified by visual inspection with the head being turned into the former stress position. The Doppler may help to indicate any residual compression. In our experience, this is sufficient and obviates the need for intra-operative angiography. If performed as described, no instability will be induced through this decompression. All along the surgery, special care has to be taken of the peri-vertebral venous plexus
In our experience, only one patient (#2) was treated by a posterior approach. The VA was decompressed, and simultaneously, an occipito-cervical fusion was realized because the patient harbored a pre-existing instability. The posterior route, which was used in 50% of the surgically treated cases in the literature, achieved very good results except for a 33.3% failure rate after 2–3 months reported by Matsuyama et al. [30, 33, 37]. The authors hypothesized that adhesion of the VA with surrounding soft tissues might be responsible of those failures. However, it is important to note that a peri-vascular scarring phenomenon was not observed in any other reported case of decompression. Maybe other reasons such as antero-lateral bands unreachable from a posterior approach—such as discussed above—may better explain such failures. These facts underline the tremendous importance of intra-operative or early postoperative control of surgical efficacy.
A completely different concept from vascular decompression is to perform atlanto-axial fusion. The rationale is to prevent extreme head rotation and consequent compression of the vertebral artery [9, 10, 30, 45]. This was first described in a case of BHS due to an odontoid defect inducing instability [10]. Later, Matsuyama et al. [30] fused another nine patients, even without instability because he had experienced failures after vascular decompression as discussed above. The fusion technique achieved excellent relief of the vascular compression syndrome; however, the restricted head mobility has been reported as bothersome and is therefore—according to our opinion— not the treatment of first choice.
Among others, we think that fusion should be reserved for cases, where atlanto-axial instability is the main factor of vertebral artery compression. Because of frequent VA anomalies in BHS patients, the perforation risk with screw techniques is expected to be higher in this population. Therefore, screw positioning as described by Harms and Melcher [22] seems safer than transarticular techniques. Alternatively, various screw-less techniques may be considered.
Independently of the surgical technique, the surgical efficacy has to be controlled by early dDSA (Fig. 1f). Some authors have reported the use of intra-operative Doppler sonography, angiography, or videoangiography with indo-cyanine green (ICG) as helpful [6, 41, 42]. In one patient, we used a transcranial Doppler in order to monitor the basilar artery flow throughout the operation. This allowed confirming the efficacy of the decompression of the VA during passive head rotation, intra-operatively.
Endovascular techniques
In case of bilateral vertebral artery stenosis, one at C1/C2 and the other at a subaxial level on the contra-lateral side, stenting of the latter was suggested [23, 39]. However, in those reports, the conclusions were conflicting. Whereas Horrowitz stated that their experience with stenting in this location has not been favorable, Sugiu reported a good result at the 6-month follow-up [23, 39]. At present, no conclusion, especially concerning long-term follow-up, may be drawn due to lacking data. Theoretically, vascular damage at the nondecompressed atlanto-axial level may further progress and ultimately result in cerebro-vascular stroke.
Conservative treatment
In a considerable number of reported BHS cases, the treatment was conservative. This included avoidance of head rotation, cervical collars and/or anticoagulation therapy [18, 23, 38, 43]. As no systematic follow-up has been reported, the long-term outcome cannot be assessed. One drawback of these options is a limitation of patient's quality of life.
As we lack exact data about the natural history of Bow hunter's syndrome, treatment recommendations have to be careful. However, as there is a potential life-threatening risk of posterior circulation infarction, we would generally recommend active treatment. We consider surgery as the treatment of choice, because it is a causal treatment. If performed in a center with competence in vascular and complex spinal procedures, the surgical risks appear to be acceptable. However, conservative options may be considered as alternative, if the patient is inoperable (age, co-morbidities) or not willing to accept surgery.
Conclusion
The present analysis based on a clinical series and a systematic review of the literature demonstrated that Bow hunter's syndrome is a rare pathology but associated with a pathognomonic and serious clinical presentation. The gold standard of diagnosis is dynamic angiography, and patients were well managed with tailored vertebral artery decompression. By this management, clinical and radiological results were excellent and the treatment-related morbidity was low.
References
Akar Z, Kafadar AM, Tanriover N, Dashti RS, Islak C, Kocer N, Kuday C (2000) Rotational compression of the vertebral artery at the point of dural penetration. Case report. J Neurosurg 93(2 Suppl):300–303
Bakay L, Leslie EV (1965) Surgical treatment of vertebral artery insufficiency caused by cervical spondylosis. J Neurosurg 23(6):596–602. doi:10.3171/jns.1965.23.6.0596
Barton JW, Margolis MT (1975) Rotational obstructions of the vertebral artery at the atlantoaxial joint. Neuroradiology 9(3):117–120
Bauer R, Sheehan S, Meyer JS (1961) Arteriographic study of cerebrovascular disease. II. Cerebral symptoms due to kinking, tortuosity, and compression of carotid and vertebral arteries in the neck. Arch Neurol 4:119–131
Bruneau M, Cornelius JF, George B (2006) Antero-lateral approach to the V3 segment of the vertebral artery. Neurosurgery 58(1 Suppl):ONS29–ONS35, discussion ONS29-35
Bruneau M, Sauvageau E, Nakaji P, Vandesteene A, Lubicz B, Chang SW, Baleriaux D, Brotchi J, De Witte O, Spetzler RF (2010) Preliminary personal experiences with the application of near-infrared indocyanine green videoangiography in extracranial vertebral artery surgery. Neurosurgery 66(2):305–311, discussion 311
Brunon J, Goutelle A (1974) Surgical treatment of vertebro-basilar insufficiency caused by extrinsic compression of the extracranial vertebral artery. Neurochirurgie 20(2):125–145
Bulsara KR, Velez DA, Villavicencio A (2006) Rotational vertebral artery insufficiency resulting from cervical spondylosis: case report and review of the literature. Surg Neurol 65(6):625–627
Chough CK, Cheng BC, Welch WC, Park CK (2010) Bow hunter's stroke caused by a severe facet hypertrophy of C1–2. J Korean Neurosurg Soc 47(2):134–136
Ford FR (1952) Syncope, vertigo and disturbances of vision resulting from intermittent obstruction of the vertebral arteries due to defect in the odontoid process and excessive mobility of the second cervical vertebra. Bull Johns Hopkins Hosp 91(3):168–173
Fox MW, Piepgras DG, Bartleson JD (1995) Anterolateral decompression of the atlantoaxial vertebral artery for symptomatic positional occlusion of the vertebral artery. Case report. J Neurosurg 83(4):737–740
George B (1993) Surgical treatment of extrinsic and neoplastic vertebral artery compression. Bull Acad Natl Med 177(1):99–111, discussion 111–112
George B, Carpentier A (2001) Compression of and by the vertebral artery. Oper Tech Neurosurg 4(4):202–218
George B, Cornelius JF (2001) Vertebral artery: surgical anatomy. Oper Tech Neurosurg 4(4):168–181
George B, Laurian C (1979) Surgical possibilities in the third portion of the vertebral artery (above C2). Anatomical study and report of a case of anastomosis between subclavian artery and vertebral artery at C1–C2 level. Acta Neurochir Suppl (Wien) 28(1):263–269
George B, Laurian C (1980) Surgical approach to the whole length of the vertebral artery with special reference to the third portion. Acta Neurochir (Wien) 51(3–4):259–272
George B, Laurian C (1989) Impairment of vertebral artery flow caused by extrinsic lesions. Neurosurgery 24(2):206–214
Grossmann RI, Davis KR (1982) Positional occlusion of the vertebral artery: a rare cause of embolic stroke. Neuroradiology 23(4):227–230
Hanakita J, Miyake H, Nagayasu S, Nishi S, Suzuki T (1988) Angiographic examination and surgical treatment of Bow hunter's stroke. Neurosurgery 23(2):228–232
Hardin CA, Poser CM (1963) Rotational obstruction of the vertebral artery due to redundancy and extraluminal cervical fascial bands. Ann Surg 158:133–137
Hardin CA, Williamson WP, Steegmann AT (1960) Vertebral artery insufficiency produced by cervical osteoarthritic spurs. Neurology 10:855–858
Harms J, Melcher RP (2001) Posterior C1–C2 fusion with polyaxial screw and rod fixation. Spine (Phila Pa 1976) 26(22):2467–2471
Horowitz M, Jovin T, Balzar J, Welch W, Kassam A (2002) Bow hunter's syndrome in the setting of contralateral vertebral artery stenosis: evaluation and treatment options. Spine (Phila Pa 1976) 27(23):E495–E498
Iguchi Y, Kimura K, Shibazaki K, Iwanaga T, Ueno Y, Inoue T (2006) Transcranial doppler and carotid duplex ultrasonography findings in Bow hunter's syndrome. J Neuroimaging 16(3):278–280
Kimura T, Sako K, Tohyama Y, Hodozuka A (1999) Bow Hunter's stroke caused by simultaneous occlusion of both vertebral arteries. Acta Neurochir (Wien) 141(8):895–896
Kuether TA, Nesbit GM, Clark WM, Barnwell SL (1997) Rotational vertebral artery occlusion: a mechanism of vertebrobasilar insufficiency. Neurosurgery 41(2):427–432, discussion 432–423
Lemole GM HJ, Spetzler RF, Zabramski JM. (2001) Bow hunter’s stroke. BNI Quaterly 2001 17:4–10
Mapstone T, Spetzler RF (1982) Vertebrobasilar insufficiency secondary to vertebral artery occlusion froma fibrous band. Case report. J Neurosurg 56(4):581–583
Matsuyama T, Morimoto T, Sakaki T (1997) Bow Hunter's stroke caused by a nondominant vertebral artery occlusion: case report. Neurosurgery 41(6):1393–1395
Matsuyama T, Morimoto T, Sakaki T (1997) Comparison of C1–2 posterior fusion and decompression of the vertebral artery in the treatment of bow hunter's stroke. J Neurosurg 86(4):619–623
Matsuyama T, Morimoto T, Sakaki T (1997) Usefulness of three-dimensional CT for bow hunter stroke. Acta Neurochir (Wien) 139(3):265–266
Miele VJ, France JC, Rosen CL (2008) Subaxial positional vertebral artery occlusion corrected by decompression and fusion. Spine (Phila Pa 1976) 33(11):E366–E370
Netuka D, Benes V, Mikulik R, Kuba R (2005) Symptomatic rotational occlusion of the vertebral artery—case report and review of the literature. Zentralbl Neurochir 66(4):217–222
Puca A, Scogna A, Rollo M (2000) Craniovertebral junction malformation and rotational occlusion of the vertebral artery. Br J Neurosurg 14(4):361–364
Seki T, Hida K, Akino M, Iwasaki Y (2001) Anterior decompression of the atlantoaxial vertebral artery to treat bow hunter's stroke: technical case report. Neurosurgery 49(6):1474–1476
Shimizu S, Yamada M, Takagi H, Fujii K, Kan S (1999) Bow hunter's stroke associated with an aberrant course of the vertebral artery—case report. Neurol Med Chir (Tokyo) 39(12):867–869
Shimizu T, Waga S, Kojima T, Niwa S (1988) Decompression of the vertebral artery for Bow-hunter's stroke. Case report. J Neurosurg 69(1):127–131
Sorensen BF (1978) Bow hunter's stroke. Neurosurgery 2(3):259–261
Sugiu K, Agari T, Tokunaga K, Nishida A, Date I (2009) Endovascular treatment for bow hunter's syndrome: case report. Minim Invasive Neurosurg 52(4):193–195
Tominaga T, Takahashi T, Shimizu H, Yoshimoto T (2002) Rotational vertebral artery occlusion from occipital bone anomaly: a rare cause of embolic stroke. Case report. J Neurosurg 97(6):1456–1459
Velat GJ, Reavey-Cantwell JF, Ulm AJ, Lewis SB (2006) Intraoperative dynamic angiography to detect resolution of Bow Hunter's syndrome: technical case report. Surg Neurol 66(4):420–423, discussion 423
Vilela MD, Goodkin R, Lundin DA, Newell DW (2005) Rotational vertebrobasilar ischemia: hemodynamic assessment and surgical treatment. Neurosurgery 56(1):36–43, discussion 43–35
Wakayama K, Murakami M, Suzuki M, Ono S, Shimizu N (2005) Ischemic symptoms induced by occlusion of the unilateral vertebral artery with head rotation together with contralateral vertebral artery dissection—case report. J Neurol Sci 236(1–2):87–90
Wang S, Wang C, Liu Y, Yan M, Zhou H (2009) Anomalous vertebral artery in craniovertebral junction with occipitalization of the atlas. Spine (Phila Pa 1976) 34(26):2838–2842
Yang PJ, Latack JT, Gabrielsen TO, Knake JE, Gebarski SS, Chandler WF (1985) Rotational vertebral artery occlusion at C1–C2. AJNR Am J Neuroradiol 6(1):96–100
Acknowledgements
We would like to thank Lili Laleva for the art work and Tad Dobrowolski for linguistic help.
Author information
Authors and Affiliations
Corresponding author
Additional information
Comments
Ernst Delwel, Rotterdam, The Netherlands
The authors have produced a well-written and educative article on the Bow Hunter's Syndrome (BHS). They performed a review of the literature and present the results of five patients which they have operated.
Typical for BHS is symptomatic compression of the (dominant) vertebral artery (VA) at the atlanto-axial level by contra-lateral rotation of the head. Dynamic DSA is indicated for the diagnosis and shows occlusion of the VA during contra-lateral rotation of the head. In all cases, there is insufficient collateral blood flow from the anterior circulation. The BHS might lead to thromboembolic complications, but the exact natural history of the syndrome is not well known. In literature, a total of 34 patients were identified who were operated for the BHS: 11 fusions, 17 posterior vascular decompressions, and 6 anterior vascular decompressions. The authors favor the anterolateral decompression as it offers the possibility to identify and subsequently cut fibrous bands which might add to the compression of the VA at the atlanto-axial level. In all five cases operated by the authors, the patients recovered uneventful and the syndrome was cured. The effect of vascular decompression was checked intra- or postoperatively.
As the natural history of the BHS is not exactly known and conservative therapy has been described in literature as a reasonable option, to my opinion, surgery should only be performed in a center with high competence in vascular and complex spinal procedures to minimize the surgical risks. If possible, intra-operative control of the decompression of the VA might be useful.
The authors are to be complimented with their very instructive article and excellent surgical results in their five cases of BHS.
Carlo Schaller, Geneva, Switzerland
The authors report on a very rare neurovascular problem: Bow hunter's syndrome. Symptomatology may be very vague, and thus, this syndrome may be overlooked easily in routine clinical practice. This may in part be due to the fact that occlusion of the VA is transient only due to temporary rotation of the head, and that this position may be normalized by the patients themselves without paying too much of attention. It is potentially dangerous, however, as it may cause brainstem infarction occasionally.
In addition to a review of existing literature on the matter, the authors report on their own five patients, and they provide a diagnostic algorithm for the evaluation of these patients. All except for one of their patients were treated via an anterolateral approach for decompression of the VA at the C1/C2 junction. They recommend to add a posterior approach plus internal fixation in case of instability in the C1/C2 joint. They stress the importance of detailed follow-up as there is evidence from the (scarce) literature of a high rate of failure, possibly due to postoperative scarring, or—in case of posterior approaches—due to missed anterolateral ligaments.
Their paper is enriched by clear illustrations concerning patient positioning, surgical approach, and technique of decompression. The potential role of endovascular stenting, especially in case of concomitant proximal VA stenosis is discussed as well. This underlines the importance that such patients should be treated in dedicated neurovascular centers with all the necessary experts and equipment to treat potential complications.
The authors are to be commended for their clear and comprehensive description of this rare clinico-pathological entity and for their excellent description of the surgical technique. It is hoped that this article will help to avoid missing such patients in the neurosurgical practice of the readership of this journal.
Rights and permissions
About this article
Cite this article
Cornelius, J.F., George, B., N’dri Oka, D. et al. Bow-hunter’s syndrome caused by dynamic vertebral artery stenosis at the cranio-cervical junction—a management algorithm based on a systematic review and a clinical series. Neurosurg Rev 35, 127–135 (2012). https://doi.org/10.1007/s10143-011-0343-4
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10143-011-0343-4