Abstract
Experience with dissection of the temporal bone is essential for training in skull-base surgery, but only a limited number of neurosurgical residents have the opportunity of cadaver dissection. A modification of a commercially available prototype three-dimensional (3D) temporal bone model is proposed to include artificial dura mater, venous sinuses, and cranial nerves for such surgical training. The base 3D temporal bone model incorporates the surface details and the inner ear structures and air cells. Model dural sinuses and dura mater made from silicone, cranial nerves made from rubber fibers, and internal carotid artery made from rubber tubes were added to the model. Posterior petrosectomy (transpetrosal approach) and transcondylar approach were performed on this model using a high-speed drill and ultrasonic bone curette under an operating microscope. The modified 3D temporal bone model provided good experience with the complicated 3D anatomy. The model could be dissected, and the dural sinuses and dura mater preserved by the eggshell peeling technique in almost the same way as real temporal bone. The modified 3D temporal bone model provides a good educational tool for training in skull-base surgery.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Skull-base surgery of the temporal bone requires high levels of surgical technique because of the complicated anatomy. Experience with cadaver dissection is essential to obtain the requisite knowledge, but neurosurgical residents have only limited opportunities to participate in such anatomical dissections. Therefore, a model method for training would be very useful.
A simulated three-dimensional (3D) model of human temporal bone has been manufactured by the rapid prototyping method based on the 3D computed tomography (CT) data [4] using the selective laser sintering (SLS) method [6, 7]. This temporal bone model includes both the surface details and the inner bony fine structures, such as the cochlea, semicircular canals, mastoid antrum, air cells, fallopian canal, and internal auditory canal. The model was made from polyamide nylon and glass beads, which can be dissected by a surgical drill in the same way as real bone [6, 7]. This model 3D temporal bone has been used in otolaryngology for anatomical study, surgical training, and surgical simulation [6, 7]. Otological surgery of the temporal bone is mostly limited to inside the bone. In contrast, neurosurgical skull-base surgery involves dissection of the dura mater and dural sinus, and the cranial nerves after opening the bony canals. Therefore, a bony model incorporating simulated dura mater, dural sinuses, and cranial nerves is ideal for training in skull-base surgery.
Here, we describe the modification of the temporal bone model with colored silicon added to the inner surface to simulate the sigmoid sinus, superior, and inferior petrosal sinuses, posterior condylar emissary vein, and dura mater, and rubber moulds of the cranial nerves and intrapetrous portion of the internal carotid artery. The modified temporal bone model was used for training in retrolabyrinthine posterior petrosectomy (transpetrosal approach) and the transcondylar approach to assess use as a model substitute for real temporal bone [2, 3, 5, 8].
Materials and methods
The 3D temporal bone model made from polyamide nylon and glass beads, and incorporating surface details and the inner ear structures and air cells, was purchased (OMeR model, Kezlex®; Ono & Co., Ltd., Tokyo, Japan). This model also incorporates the part of the occipital bone including the jugular foramen, hypoglossal canal, occipital condyle, condylar fossa, posterior condylar canal, and jugular tubercle. Figure 1 shows the lateral aspect view and the 3D CT image of the model, which visualizes the zygomatic process, articular tubercle, styloid process, external acoustic meatus, mastoid process, digastric groove, temporal line, supramastoid crest, Macewen’s triangle, and Henle’s spine. The bone density CT of this model revealed the external and internal auditory canals, auditory tube, tympanic cavity, malleus and incus, cochlea, vestibule, lateral, posterior, and superior semicircular canals, mastoid antrum, and mastoid air cells (Fig. 2).
Prototype temporal bone model. a Lateral surface view of the temporal bone model. b Three-dimensional computed tomography scan of the temporal bone model showing details of the bone surface. Z Zygomatic process, AT articular tubercle, SP styloid process, AM external acoustic meatus, M mastoid process, DG digastric groove, TL temporal line, SC supramastoid crest, MT Macewen’s triangle, HS Henle’s spine
Bone density computed tomography scans of the temporal bone model showing the fine structures in the temporal bone. EAC External auditory canal, IAC internal auditory canal, AT auditory tube, TC tympanic cavity, MI malleus and incus, C cochlea, V vestibule, LSC lateral semicircular canal, PSC posterior semicircular canal, SSC superior semicircular canal, MA mastoid antrum, MAC mastoid air cells
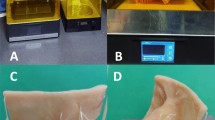
Blue hydrophilic vinyl polysiloxane impression material (Exafine® Regular Type; GC Corporation, Tokyo, Japan) was added to the inner surface of the temporal bone model to model the transverse, sigmoid, superior petrosal, and inferior petrosal sinuses, jugular vein, and posterior condylar emissary vein. The dura mater was modeled by painting brown hydrophilic vinyl polysiloxane impression material (Exafine® Injection Type; GC Corporation) onto the inner surface of the temporal bone model. The facial, cochlear, glossopharyngeal, vagal, accessory, and hypoglossal nerves were modeled with yellow rubber fibers positioned in the corresponding canals of the model. The intrapetrous portion of the internal carotid artery was formed from red rubber tube placed in the carotid canal (Fig. 3). The total cost was about 250$.
Prototype (left column) and modified (right column) temporal bone models. a Superior surface of the temporal bone, b posterior surface of the temporal bone, c inferior surface of the temporal bone. The dura mater was made from brown silicone. The dural sinuses (T transverse sinus, S sigmoid sinus, SPS superior petrosal sinus, IPS inferior petrosal sinus, JV jugular vein, EV posterior condylar emissary vein) were made from blue silicon. The facial (F), cochlear (C), glossopharyngeal (G), vagal (V), accessory (A), and hypoglossal nerves (H) were made from yellow rubber fibers. The intrapetrosal portion of the internal carotid artery (IC) was made from red rubber tube. AE Arcuate eminence, SS sigmoid sulcus, PR petrous ridge, JT jugular tubercle, FL foramen lacerum, HF hiatus facialis, DG digastric groove, M mastoid, SP styloid process, HC hypoglossal canal, JF jugular foramen, IAC internal acoustic canal, OC occipital condyle, PCC posterior condylar canal, CF condylar fossa, MF mandibular fossa, SMF stylomastoid foramen, CC carotid canal
The modified 3D temporal bone model was positioned in a temporal bone holder Sando-Davis (Nagashima Medical Instruments Co., Ltd., Tokyo, Japan) and fixed with Mayfield tri-pins. Temporal bone model dissection was performed using either a high-speed drill or an ultrasonic bone curette (Sonopet UST-2000; M&M Co., Ltd., Tokyo, Japan) under an operating microscope. The material of the model generates heat during drilling similarly to real bone. Irrigation suction was used to cool the model and aspirate the debris during drilling as in real surgery.
Results
Posterior transpetrosal approach
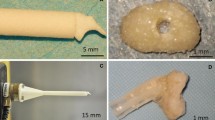
Decortication of the mastoid process was performed from the supramastoid crest to the mastoid tip using the high-speed drill with a cutting burr. The air cells behind Henle’s spine were drilled, and the mastoid antrum was opened (Fig. 4b). The feeling of drilling the cortical bone of the model with a cutting burr was almost the same as real bone. However, the inside of the mastoid antrum and air cells were packed with white material powder (polyamide nylon and glass beads) which had to be removed to disclose the antrum. Drilling the lateral bottom of the mastoid antrum using the high-speed drill with a diamond burr, the lateral semicircular canal was dissected out, together with the posterior and superior semicircular canals (Fig. 4c). The feeling of drilling the mastoid bony air cells (cancerous bone) of the model lacked the “crispy touch” of real bone drilling because the artificial bone made from synthetic resin material (polyamide nylon) had a “sticky touch” during drilling. Therefore, drilling out the semicircular canals from the mastoid air cells was more difficult in the model than in the real bone because of the sticky feeling of the artificial cancerous bone and the presence of powder material inside the air cells. After drilling out the digastric ridge, the fallopian canal surrounded by artificial cortical bone was opened using an ultrasonic bone curette (Fig. 4d). Artificial bone dissection was possible with the ultrasonic bone curette, but the device slightly lacked the power needed to drill the artificial bone material easily. The inside of the canal was also packed with powder material and the yellow rubber model facial nerve was placed in the canal after the removal of the power material. The posterior fossa dura and temporal fossa dura were disclosed. The bone over the transverse and sigmoid sinuses was thinned by either the diamond drill or ultrasonic curette until it resembled a transparent eggshell. The thinned bone was peeled from the surface of the venous sinus. The eggshell peeling technique could be realized using the model in almost the same way as real bone. Finally, Trautmann’s triangle, the superior petrosal sinus, and the presigmoid dura were disclosed using a micro-punch (Fig. 4e and f).
Posterior petrosectomy using the modified temporal bone model. a Lateral surface of the mastoid process and external auditory canal. The yellow rubber fiber represented the extracranial facial nerve. b After decortication of the mastoid process, the mastoida antrum was opened. c The transverse sinus and superior petrosal sinus were exposed. The semicircular canals were dissected out. d The fallopian canal was opened using an ultrasonic bone curette. e Trautmann’s triangle was opened using a micro-punch. f Appearance after posterior petrosectomy. The semicircular canals were colored with yellow paint. MT Mastoid tip, SP styloid process, AM external acoustic meatus, DG digastric groove, HS Henle’s spine, MA mastoid antrum, T transverse sinus, S sigmoid sinus, SPS superior petrosal sinus, TD temporal fossa dura, PD posterior fossa dura, PSD presigmoid dura, LSC lateral semicircular canal, PSC posterior semicircular canal, SSC superior semicircular canal, FN fallopian canal and facial nerve, DR digastric ridge
Transcondylar approach (Fig. 5)
The cortical bone covering the posterior third of the occipital condyle was removed with the high-speed drill using a cutting burr. The cancerous bone was drilled away with a diamond burr until the cortical bone of the hypoglossal canal was encountered. This process was achieved in the model in almost the same way as real bone except for the sticky feeling of the cancerous bone during drilling. The condylar fossa and condylar canal were drilled away and the posterior condylar emissary vein was trimmed. The hypoglossal canal was opened until the intracranial end of the canal was reached (Fig. 5b). The bone of the jugular tubercle situated above the hypoglossal canal was removed extradurally to the anterior portion of the tubercle using a diamond burr (Fig. 5c). The jugular bulb was exposed (Fig. 5d).
Transcondylar approach using the modified temporal bone model. a Posterior aspect of the condylar part of the occipital bone and the temporal bone. b Opening the hypoglossal canal. c Drilling of the jugular tubercle above the hypoglossal canal. d Decompressed jugular tubercle and exposed jugular bulb. JT Jugular tubercle, OC occipital condyle, CF condylar fossa, MT mastoid tip, DG digastric groove, S sigmoid sinus, EV posterior condylar emissary vein, HC hypoglossal canal, JB jugular bulb, VII facial nerve, VIII cochlear nerve, IX glossopharyngeal nerve, X vagal nerve, XI accessory nerve, XII hypoglossal nerve
Figure 6 shows the final appearances of the modified temporal bone model after the posterior petrosectomy and the resection of the posterior part of the occipital condyle. The complicated anatomical structures of the temporal bone including the bony structures, dura mater, dural sinuses, and cranial nerves were recognized stereoscopically from various angles.
Discussion
Artificial plastic petrous bone model created by the stereolithography method has been applied for surgical training [1], but was not suitable for dissection training using the high-speed drill or ultrasonic bone curette because the model was made from solid plastic [6, 7]. In contrast, the SLS method produces the 3D model by sintering powder layers and fusing with a laser. The present study used the temporal bone model (OMeR) produced by SLS, which reproduces the surface anatomical details and the fine bony structures inside the model. Furthermore, the OMeR model is suitable for surgical training because the constituent material (polyamide nylon and glass beads) can be drilled by a surgical burr [6, 7].
The present study verified that the model was dissected in almost the same way as real bone using the cutting burr of the high-speed drill. However, the feeling of drilling the cancerous bone of the model lacked the “crispy touch” of real bone because the artificial material (polyamide nylon) caused a “sticky touch” during drilling. Therefore, drilling out the semicircular canals from the mastoid air cells in the model was more difficult than the real bone because of the sticky feeling of the artificial cancerous bone and the presence of powder material inside the air cells. Better artificial bony material more closely resembling real bone and new technology to exclude the powder material from bony cavities will further improve this temporal bone model for surgical training.
Neurosurgical skull-base surgery involves drilling of the bony structures, but also manipulation of the dura mater, dural sinuses, cranial nerves, and major arteries. We added these structures to the temporal bone model by hand. This process facilitates better understanding of the stereoscopic anatomy of the temporal bone. The important procedures of skull-base surgery are to expose the dura mater and dural sinuses, and dissect out the cranial nerves. The temporal bone model including these vital structures is essential for training skull-base surgery. The present model could be dissected, and the dural sinuses and dura mater preserved by the eggshell peeling technique in almost the same way as real temporal bone. We propose use of this modified 3D temporal bone model as a good educational tool for training in skull-base surgery.
Summary and conclusion
A modification of a commercially available prototype three-dimensional (3D) temporal bone model is proposed to include artificial dura mater, venous sinuses, and cranial nerves for training in skull-base surgery. The present model could be dissected, and the dural sinuses and dura mater preserved by the eggshell peeling technique in almost the same way as real temporal bone. The modified 3D temporal bone model provides a good educational tool for training in skull-base surgery.
References
Begall K, Vorwerk U (1998) Artificial petrous bone produced by stereolithography for microsurgical dissecting exercises. ORL J Otorhinolaryngol Relat Spec 60:241–245
Bertalanffy H, Seeger W (1991) The dorsolateral, suboccipital, transcondylar approach to the lower clivus and anterior portion of the craniocervical junction. Neurosurgery 29:815–821
Hakuba A, Nishimura S, Inoue Y (1985) Transpetrosal–transtentorial approach and its application in the therapy of retrochiasmatic craniopharyngiomas. Surg Neurol 24:405–415
McAlea K, Forderhase P, Hejmadi U, Nelson C (1997) Materials and applications for the SLS selective laser sintering process. In: Chartoff R (ed) Proceedings of the 7th international conference on rapid prototyping. Dayton, University of Dayton, pp 23–33
Miller CG, van Loveren HR, Keller JT, Pensak M, el-Kalliny M, Tew JM Jr (1993) Transpetrosal approach: surgical anatomy and technique. Neurosurgery 33:461–469
Suzuki M, Ogawa Y, Kawano A, Hagiwara A, Yamaguchi H, Ono H (2004) Rapid prototyping of temporal bone for surgical training and medical education. Acta Otolaryngol 124:400–402
Suzuki M, Ogawa Y, Hagiwara A, Yamaguchi H, Ono H (2004) Rapidly prototyped temporal bone model for otological education. ORL J Otorhinolaryngol Relat Spec 66:62–64
Wen HT, Rhoton AL Jr, Katsuta T, de Oliveira E (1997) Microsurgical anatomy of the transcondylar, supracondylar, and paracondylar extensions of the far-lateral approach. J Neurosurg 87:555–585
Author information
Authors and Affiliations
Corresponding author
Additional information
Comments
Takeshi Mikami, Tomakomai, Japan
The training system for skull-base surgery is an indispensable tool allowing neurosurgeons to demonstrate an appropriate surgical strategy for a particular lesion. The temporal bone model can also be used as a teaching model for cranial anatomy. Unfortunately, it is not likely that this report constitutes a new approach to teaching cranial surgical techniques. However, the authors mentioned that the model could be dissected in almost the same way as real bone using a recently developed high-speed drill. The model bone might become increasingly realistic through recent advances in the model construction. The technological costs of the model bone construction should be reduced in the future so the surgical techniques can be attained more easily.
Continued use of the temporal bone model will be expected in the course of future development.
Takeshi Kawase, Tokyo, Japan
The artificial 3-D temporal bone (Kezlex), precisely manufactured resembling to the dried skull is beneficial to neurosurgeons who are not able to study it by cadaver dissection. The soft tissues such as cranial nerves, vessels and meninx are important to understand the anatomy; however, they have never been manufactured. The authors of this paper described the technique of manufacturing the soft tissues. If this model could be manufactured in a commercial base and sold with a reasonable price, it would be helpful for neurosurgeon’s education. However, the anatomical accuracy may be most important for the model and the manufacturer is requested to employ neurosurgeons as consultants, who are experts on microsurgical anatomy like the authors.
Imad N. Kanaan, Riyadh, Saudi Arabia
The best venues to teach clinical skills, sound judgment, and surgical dexterity as well as to conduct valued clinical research are the ward and operating theatre (laboratories of highest order) as correctly stated by William Halstead years ago. However, taking in consideration of patient’s safety, surgical outcome on one hand and the complexity of the intervention in the field of neurological, otological, and skull-base surgeries on the other hand, it is a prerequisite for training young surgeons to have a rehearsal or enhancement of their hand skills (Chirurg = hand, ergon = work) in an alternative set-up prior to live surgical experience. Options available are: use of navigation system, surgical simulator, attending cadaver workshops, microsurgical animal courses or using artificial models similar to the one described by the authors. In fact, a training course using well-prepared and treated cadaver samples by the masters in the field, if available and affordable, remains the best alternative option for real-time surgery considering the tactile tissue feed back the surgeon will adapt to or gain. The lack of available or adequate cadaver samples, soaring material costs and course fees have prompted the industry, with the help of modern technology, to seek a good alternative training models such as the one described by the authors; this will benefit the training of many young surgeons around the globe and, hopefully, with a drastic cut in costs.
Rights and permissions
About this article
Cite this article
Mori, K., Yamamoto, T., Oyama, K. et al. Modification of three-dimensional prototype temporal bone model for training in skull-base surgery. Neurosurg Rev 32, 233–239 (2009). https://doi.org/10.1007/s10143-008-0177-x
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10143-008-0177-x