Abstract
Magnesium has neuroprotective and antivasospastic properties in the presence of subarachnoid hemorrhage (SAH). The present study investigated the effect of intracisternal administration of magnesium on cerebral vasospasm in the experimental SAH rat model. The rat double-SAH model (0.2 mL autologous blood injected twice into the cisterna magna) was used. Normal saline (SAH group, N = 8) or 10 mmol/L magnesium sulfate in normal saline (SAH + MG group, N = 8) was infused into the cisterna magna at 1.5 μL/min for 30 min on day 5. Control rats without SAH also received intracisternal infusion of normal saline (control group, N = 6). Local cerebral blood flow (CBF) at 24 locations and the weighted average were quantitatively measured by the autoradiographic technique using [14C]iodoantipyrine during infusion. The weighted average CBF was significantly reduced (P < 0.01, Student’s t-test) in the SAH group (0.78 ± 0.16 mL g−1 min−1) compared to the control group (1.0 ± 0.15 mL g−1 min−1) and was significantly improved (P < 0.01, Student’s t-test) in the SAH + MG group (0.98 ± 0.18 mL g−1 min−1). Local CBF was significantly reduced (P < 0.05, unpaired t test) in 16 locations in the SAH group and significantly improved (P < 0.05, unpaired t test) in 12 locations in the SAH + MG group. Intracisternal infusion of magnesium sulfate significantly improved reduced CBF induced by experimental SAH in the rat.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Ruptured cerebral aneurysm can be successfully treated by clipping or intravascular surgery, but the incidence of angiographical vasospasm remains as high as 67%, and 25% to 30% of patients who survive the initial onset of subarachnoid hemorrhage (SAH) suffer from delayed cerebral ischemia manifesting on days 4 to 14 [6, 18]. Such delayed cerebral ischemia is still one of the major causes of morbidity and mortality in patients with SAH despite the availability of many therapies for cerebral vasospasm such as calcium channel blockers [1], hypervolemic hypertensive therapy [25], cisternal irrigation with urokinase or tissue plasminogen activator (t-PA) [7, 16], intra-arterial administration of papaverine hydrochloride [14], and transluminal balloon angioplasty [23]. Overall mortality rates for patients with ruptured aneurysm range from 30% to 70%, and 10% to 20% of the survivors suffer neurological disability caused by cerebral ischemia [12]. Therefore, a more potent therapeutic modality for cerebral vasospasm is required to prevent delayed cerebral ischemia after SAH [22].
Intravenous magnesium sulfate administration is used to treat pre-eclampsia and eclampsia during pregnancy, which share etiological similarities with the development of cerebral vasospasm after SAH [3, 10]. Magnesium ion (Mg2+) is considered to have both neuroprotective and vasodilatory effects. The neuroprotective effect may be mediated by inhibition of ischemia-induced glutamate release, which eventually causes excitotoxicity in the pathogenesis of ischemic neuronal death [17], inhibition of calcium influx into cells by blocking voltage-dependent and N-methyl-d-aspartate-activated calcium channels [20, 24], and blocking free radical production in the mitochondria [5, 34]. The vasodilation effect is considered to occur through blocking of Ca2+ influx and competitive inhibition of Ca2+ binding at calmodulin sites, which affect the myosin light chain kinase active form in the smooth muscles of cerebral blood vessels [34]. Magnesium also attenuates the effects on the cerebral arteries of endothelin-1 and oxyhemoglobin, which are considered to be important potent vasoconstrictors after SAH [15, 21].
Several in vitro and in vivo studies have shown the vasodilation effect of magnesium on spastic arteries in experimental SAH [26, 27]. Pilot clinical studies have demonstrated the safety and efficacy of magnesium therapy for SAH [4, 33, 36]. Recent prospective studies of continuous intravenous administration of magnesium sulfate in patients with aneurysmal SAH failed to show any vasodilatory effect on vasospasm detected by angiography and transcranial Doppler ultrasonography [29, 31]. The effect of continuous intravenous administration of Mg2+ on angiographic vasospasm was also examined using the monkey SAH model, but magnesium infusion failed to reverse the cerebral vasospasm after SAH [19]. In contrast, in vitro studies clearly show that increased extracellular Mg2+ concentration definitely causes vasodilation of both normal and contracted cerebral vessels in the presence of vasospasm-inducing chemicals [2, 21, 32]. However, the effect of increased Mg2+ concentration in the cerebrospinal fluid (CSF) on spastic cerebral arteries after SAH is only known through topical application of magnesium sulfate to the rat SAH model observed through a cranial window [27].
The present study examined the effects of intracisternal infusion of magnesium sulfate in the rat SAH model on the decreased cerebral blood flow (CBF) using a quantitative local CBF measuring technique in the awake state.
Materials and methods
All surgical procedures were performed according to the National Institutes of Health Guide for the Care and Use of Laboratory Animals and were approved by the Animal Care and Use Committee of Juntendo University.
Rat SAH model
The “double-hemorrhage model” in male Sprague–Dawley rats weighing 365 to 460 g was used to simulate delayed vasospasm. This model was proven to induce significant decreases in cerebral artery diameter and CBF on day 5 [35]. Briefly, the rat was lightly anesthetized with 1.0% to 1.5% halothane in 70% N2O/30% O2 and intraperitoneal injection of 25 mg/kg pentobarbital and then fixed in a rodent stereotaxic frame. Body temperature was strictly monitored with a rectal probe and maintained at 37°C with a thermal blanket or heating lamp. A suboccipital skin incision was made, and the atlanto-occipital membrane was exposed. A silastic catheter (0.012 in. inner diameter × 0.025 in. outer diameter, Read Plastic, Rockville, MD, USA) was implanted into the cisterna magna and fixed with glue, and then 0.2 mL autologous blood obtained from the tail vein was injected over 30 min using an infusion pump (EP-60; Eicom, Kyoto, Japan). The catheter was hidden beneath the skin, and the same procedure was repeated on the next day (day 2). The control rats underwent the same procedures, but 0.2 mL normal saline instead of blood was injected into the cisterna magna.
Quantitative CBF measurement
The animals were lightly anesthetized with halothane, and polyethylene catheters (PE50) were inserted into both femoral veins and one femoral artery, and the embedded cisternal catheter was pulled out on day 5. Loose-fitting plaster casts were then applied to the pelvic area and taped to an iron brick to prevent movement. The animal was then allowed to recover from the anesthesia for at least 4 h before starting intracisternal infusion and measurement of local CBF. Arterial blood pressure, hematocrit, and arterial blood gas were measured. Normal saline (SAH group, N = 8) or 10 mmol/L magnesium sulfate in normal saline (pH 7.410; SAH + MG group, N = 8) was infused into the cisterna magna at 1.5 μL/min using an infusion pump (EP-60) in the SAH model rats. Control rats without SAH received intracisternal infusion of normal saline (control group, N = 6). The infusion continued for 30 min before and during the 1-min period of CBF measurement [13].
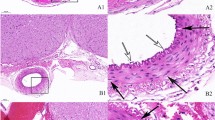
Local CBF at 24 locations and the weighted average were quantitatively determined by the autoradiographic technique using the [14C]iodoantipyrine method [28]. [14C]Iodoantipyrine of 50 μCi in 1 mL normal saline was continuously infused through the femoral vein catheter. The weights of the 13 to 16 arterial blood samples collected on filter papers were measured, and the 14C radioactivity was measured by a liquid scintillation counter (Packard Instruments, Downers Grove, IL, USA) to determine the time course of the arterial concentration of 14C. At 1 min after the infusion of [14C]iodoantipyrine, the animal was decapitated, and the brain was quickly removed and frozen in isopentane chilled to −60°C with dry ice and stored at −80°C. The frozen brain was cut into 20-μm-thick coronal sections for quantitative autoradiography and 10-μm-thick coronal sections for hematoxylin–eosin (HE) staining in a cryostat maintained at −20°C. The sections were thaw-mounted on glass coverslips, dried on a hot plate at 60°C, mounted on cardboard, and autoradiographed together with a set of calibrated 14C-labeled methylmethacrylate standards with Kodak BIOMAX MR films (Eastman Kodak, Rochester, NY, USA) in X-ray cassettes. The autoradiographs were digitized in an ES-2200 scanner (Seiko Epson, Nagano, Japan) and displayed on a computer monitor for densitometric analysis. The 24 local and weighted average values of CBF were calculated from the local tissue 14C concentrations and the time courses of the arterial blood 14C concentrations by the operational equation of the method and the computer program developed by G Mies (Max Planck Institut fur Neurologische Forschung, Koln, Germany) for the National Institutes of Health Image program (W Rasband, NIMH, Bethesda, MD, USA).
Statistics
The data are presented as means ± standard deviations. Statistical significances of differences were analyzed by one-way analysis of variance (ANOVA), two-way ANOVA, and Student’s t-test using the SPSS 7.5.1j software for Windows (SPSS Japan, Tokyo, Japan). P values less than 0.05 were considered statistically significant.
Results
Body weight, mean arterial blood pressure, body temperature, hematocrit, arterial PaO2, PaCO2, and pH at the time of measurement of local CBF were all within normal limits and not significantly different between the three experimental groups (Table 1). There was no clinical seizure observed during the CBF measurements.
The weighted average CBF was significantly reduced (P < 0.01, Student’s t-test) in the SAH group (0.78 ± 0.16 mL g−1 min−1) compared to that of the control group (1.0 ± 0.15 mL g−1 min−1) and was significantly improved (P < 0.01, Student’s t-test) in the SAH + MG group (0.98 ± 0.18 mL g−1 min−1) compared to that of the SAH group. Local CBF values in the 24 locations in the three experimental groups are listed in Table 2. The two-way ANOVA with two factors of group and location was performed to evaluate the difference in CBFs for the 24 locations and showed significant differences (P < 0.0001) between the control group and the SAH group and between the SAH group and the SAH + MG group (Table 3). Therefore, the unpaired t-test was applied to the separate locations, showing that local CBF was significantly reduced (P < 0.05) in 16 locations in the SAH group compared to the control group and that local CBF was significantly improved (P < 0.05) in 12 locations in the SAH + MG group compared to the SAH group, mostly in the posterior fossa and caudal structures (Table 2; Fig. 1). HE staining revealed no infarction lesions in the brains of any of the rats in the three experimental groups (data not shown). HE staining showed no other histological findings indicating the neurotoxic effects of magnesium infusion.
Digitized [14C]iodoantipyrine autoradiograms showing local cerebral blood flow (CBF) quantitatively encoded in color. Control rats received intracisternal infusion of normal saline (left column); subarachnoid hemorrhage (SAH) rats received intracisternal infusion of normal saline (center column); SAH + MG rats received intracisternal infusion of 10 mmol/L magnesium sulfate in normal saline (right column). SAH rats showed decreased CBF throughout the brain, which was improved in SAH + MG rats
To quantify the effect of MgSO4 infusion, the local CBF values of the SAH + MG group and the SAH group were standardized by dividing by the mean local CBF values of the SAH group for each of the 24 locations. Figure 2 compares the standardized CBF values of the SAH + MG group and SAH group and clearly shows the improvement in local CBF induced by MgSO4 infusion. Because MgSO4 was injected from the cisterna magna, the local CBF of the caudal area can be expected to improve more than the cranial area. To confirm this assumption, the differences in local CBF were evaluated by two-way ANOVA for the caudal area from the vestibular nucleus to the auditory cortex, the middle area from the superior colliculus to the hippocampus, and the cranial area from the barrel cortex to the genu of the corpus callosum. The P values were less than 0.001 for all three areas, but the F values suggested that improvement of local CBF was superior in the caudal area (F = 55.89), followed by the middle area (F = 30.46) and the cranial area (F = 14.72).
Comparison of standardized local CBF values in 24 local cerebral structures. Standardized CBF values were obtained as local CBF values measured in SAH + MG rats (solid circles) and SAH rats (open squares) divided by the mean local CBF values of the SAH group for the 24 brain structures. Points and bars represent the mean ± 2 standard errors. Differences in local CBF were evaluated by two-way ANOVA, showing F values of increasing in the order of cranial area (14.72), middle area (30.46), and caudal area (55.89) and indicating the more prominent effect of magnesium sulfate infusion in the caudal area
Discussion
The present study showed that intracisternal infusion of magnesium sulfate significantly improved the reduction in CBF induced by experimental SAH in the conscious rat. The vasodilation effect was more prominent in the caudal area than in the cranial area because the magnesium sulfate solution was infused from the cisterna magna. Therefore, the location of the tube used for intracisternal magnesium infusion may be critical to obtain the maximum dilatory effect on the spastic arteries. Furthermore, any subarachnoid blood clot, which may interfere with magnesium distribution in the subarachnoid space, should be dispersed as far as possible using urokinase or t-PA before initiation of magnesium sulfate infusion.
Extracellular Mg2+ is probably critical in the regulation of vasomotor tone. The normal serum Mg2+ concentration ranges from 0.7 to 0.96 mmol/L in humans and primates, and the CSF Mg2+ concentration is 30–40% higher (about 1.2 mmol/L) [8, 9, 11]. Increased Mg2+ concentration causes in vitro vasodilation of cerebral and coronary arteries suspended under isometric tension [2, 32]. The effect of changes in CSF Mg2+ concentration on cat normal arterioles was dose dependent and caused dilation in the range of 2.4 (1.2 mmol/L) to 9.6 mEq/L (4.8 mmol/L) [30]. The Mg2+ concentrations causing in vitro relaxation of arteries range from 4.8 to 12 mmol/L [2, 32]. Furthermore, topical application of 10 mEq/L (5 mmol/L) magnesium sulfate to the spastic basilar artery of the experimental SAH rat caused dramatic dilation of the artery [27]. Therefore, a CSF Mg2+ concentration of more than 5 mmol/L seems to be required to expect the vasodilation effect of Mg2+ on spastic cerebral arteries after SAH. The present study used the Mg2+ concentration of 10 mmol/L for intracisternal infusion based on the previous studies. Side effects such as bradycardia and hypotension can occur with serum Mg2+ concentration within the 2.2–3.1-mmol/L range, and serious side effects of respiratory suppression have been reported with levels above 3.1 mmol/L [34]. These facts suggest that the CSF Mg2+ concentrations required to ameliorate vasospasm are hard to achieve by intravenous administration of Mg2+ without clinical toxicity.
Clearly, reaching and maintaining the therapeutic concentration of Mg2+ in the CSF probably requires intracisternal continuous infusion of magnesium sulfate. Further study is required to assess the duration of the reversal effect of intracisternal magnesium infusion on reduced CBF after SAH before clinical application. Indeed more preclinical data is needed about the optimal concentration of magnesium sulfate, optimal timing to start and duration of the infusion, neurotoxicity of intracisternal injection, and so on. However, the present findings indicate that intracisternal infusion of magnesium sulfate is a promising vasodilation treatment to ameliorate cerebral vasospasm in patients with ruptured intracranial aneurysm.
References
Allen GS, Ahn HS, Preziosi TJ, Battye R, Boone SC, Boone SC, Cho SN, Kelly DL, Weir BK, Crabbe RA, Mellits DE, Rosenbloom SB, Dorsey FC, Ingram CR, Mellits DE, Bertsch LA, Boisvert DP, Hundley MB, Jonson RK, Strom JA, Transou CR (1983) Cerebral arterial spasm—a controlled trial of nimodipine in patients with subarachnoid hemorrhage. N Engl J Med 308:619–624
Altura BT, Altura BM (1980) Withdrawal of magnesium causes vasospasm while elevated magnesium produces relaxation of tone in cerebral arteries. Neurosci Lett 20:323–327
Belfort MA, Anthony J, Saadw GR, Allen JC Jr (2003) A comparison of magnesium sulfate and nimodipine for the prevention of eclampsia. N Engl J Med 348:304–311
Chia RY, Hughes RS, Morgan MK (2002) Magnesium: a useful adjunct in the prevention of cerebral vasospasm following aneurysmal subarachnoid haemorrhage. J Clin Neurosci 9:279–281
Dickens BF, Weglicki WB, Li YS, Mak IT (1992) Magnesium deficiency in vivo enhances free radical-induced intracellular oxidation and cytotoxicity in endothelial cells. FEBS Lett 311:187–191
Dorsch NW (2002) Therapeutic approaches to vasospasm in subarachnoid hemorrhage. Curr Opin Crit Care 8:128–133
Findlay JM, Kassell NF, Weir BK, Haley EC Jr, Kongable G, Germanson T, Truskowski L, Alves WM, Holness RO, Knuckey NW (1995) A randomized trial of intraoperative, intracisternal tissue plasminogen activator for the prevention of vasospasm. Neurosurgery 37:168–178
Fishman RA (1980) Cerebrospinal fluid in diseases of the nervous system. Saunders, Philadelphia, pp 220–222
Fong J, Gurewitsh ED, Volpe L, Wagner WE, Gomillion MC, August P (1995) Baseline serum and cerebrospinal fluid magnesium levels in normal pregnancy and preeclampsia. Obstet Gynecol 85:444–448
Greene MF (2003) Magnesium sulfate for preeclampsia. N Engl J Med 348:275–276
Hambleton P, Baskerville A, Wade JJ, Bailey NE (1981) Some normal clinical chemistry values for cerebrospinal fluid of the rhesus monkey (Macaca mulatta). Lab Anim 15:181–186
Hop JW, Rinkel GJ, Algra A, van Gijin J (1997) Case-fatality rates and functional outcome after subarachnoid hemorrhage: a systematic review. Stroke 28:660–664
Horinaka N, Kuang TY, Pak H, Wang R, Jehle J, Kennedy C, Sokoloff L (1999) Blockade of cerebral blood flow response to insulin-induced hypoglycemia by caffeine and glibenclamide in conscious rats. J Cereb Blood Flow Metab 17:1309–1318
Kassell NF, Helm G, Simmons N, Phillips CD, Cail WS (1992) Treatment of cerebral vasospasm with intra-arterial papaverine. J Neurosurg 77:848–852
Kemp PA, Gardiner SM, March JE, Rubin PC, Bennett T (1999) Assessment of the effects of endothelin-1 and magnesium sulfate on regional blood flows in conscious rats, by the coloured microsphere reference technique. Br J Pharmacol 126:621–626
Kodama N, Sasaki T, Kawakami M, Sato M, Asari J (2000) Cisternal irrigation therapy with urokinase and ascorbic acid for prevention of vasospasm after aneurysmal subarachnoid hemorrhage. Outcome in 217 patients. Surg Neurol 53:110–117
Lin JY, Chung SY, Lin MC, Cheng FC (2002) Effects of magnesium sulfate on energy metabolites and glutamate in the cortex during focal ischemia and reperfusion in the gerbil monitored by a dual-probe microdialysis technique. Life Sci 71:803–811
Macdonald RL, Weir B (1997) Cerebral vasospasm: prevention and treatment. In: Batjer HH, Caplan LR, Friberg L, Greenlee RG Jr, Kopitnik TA Jr, Young WL (eds) Cerebrovascular disease. Lippincott-Raven, Philadelphia, pp 1111–1121
Macdonald RL, Curry DJ, Aihara Y, Zhang ZD, Jahromi BS, Yassari R (2004) Magnesium and experimental vasospasm. J Neurosurg 100:106–110
Mayer ML, Westbrook GL, Guthrie PB (1984) Voltage-dependent block by Mg2+ of NMDA responses in spinal cord neurons. Nature 309:261–263
Miura K (1988) [Changes in Mg++ concentration of CSF after subarachnoid hemorrhage and Mg++—effect on the contractions of bovine cerebral artery]. No Shinkei Geka 16:1251–1259. (in Japanese)
Mocco J, Zacharia BE, Komotar RJ, Connolly ES Jr (2006) A review of current and future medical therapies for cerebral vasospasm following aneurysmal subarachnoid hemorrhage. Neurosurg Focus 21:E9
Newell DW, Eskridge JM, Aaslid R (2001) Current indications and results of cerebral angioplasty. Acta Neurochir Suppl 77:181–183
Nowak L, Bregestovski P, Ascher P, Herbet A, Prochiantz A (1984) Magnesium gates glutamate-activated channels in mouse central neurones. Nature 307:462–465
Origitano TC, Wascher TM, Reichman OH, Anderson DE (1990) Sustained increased cerebral blood flow with prophylactic hypertensive hypervolemic hemodilution (“triple-H” therapy) after subarachnoid hemorrhage. Neurosurgery 27:729–739
Pyne GJ, Cadoux-Hudson TA, Clark JF (2001) Magnesium protection against in vitro cerebral vasospasm after subarachnoid haemorrhage. Br J Neurosurg 15:409–415
Ram Z, Sadeh M, Shacked I, Sahar A, Hadani M (1991) Magnesium sulfate reverses experimental delayed cerebral vasospasm after subarachnoid hemorrhage in rats. Stroke 22:922–927
Sakurada O, Kennedy C, Jehle J, Brown JD, Carbin GL, Sokoloff L (1978) Measurement of local cerebral blood flow with iodo(14C)antipyrine. Am J Physiol 234:H59–H66
Schmid-Elsaesser R, Kunz M, Zausinger S, Prueckner S, Briegel J, Steiger HJ (2006) Intravenous magnesium versus nimodipine in the treatment of patients with aneurysmal subarachnoid hemorrhage: a randomized study. Neurosurgery 58:1054–1065
Seelig JM, Wei EP, Kontos HA, Choi SC, Becker DP (1983) Effect of changes in magnesium ion concentration on cat cerebral arterioles. Am J Physiol 245:H22–H26
Stippler M, Crago E, Levy EI, Kerr ME, Yonas H, Horowitz MB, Kassam A (2006) Magnesium infusion for vasospasm prophylaxis after subarachnoid hemorrhage. J Neurosurg 105:723–729
Turlapaty PD, Altura BM (1980) Magnesium deficiency produces spasms of coronary arteries: relationship to etiology of sudden death ischemic heart disease. Science 208:198–200
van den Bergh WM, Albrecht KW, Berkelbach van der Sprenkel JW, Rinkel GJ (2003) Magnesium therapy after aneurysmal subarachnoid haemorrhage a dose-finding study for long term treatment. Acta Neurochir (Wien) 145:195–199
van den Bergh WM, Dijkhuizen RM, Rinkel GJE (2004) Potentials of magnesium treatment in subarachnoid haemorrhage. Magnes Res 17:301–313
Vatter H, Weidauer S, Konczalla J, Dettmann E, Zimmermann M, Preibisch C, Zanella F, Seifert V (2006) Time course in the development of cerebral vasospasm after experimental subarachnoid hemorrhage: clinical and neuroradiological assessment of the rat double hemorrhage model. Neurosurgery 58:1190–1197
Veyna RS, Seyfried D, Burke DG, Zimmerman C, Mlynarek M, Nichols V, Marrocco A, Thomas AJ, Mitsias PD, Malik G (2002) Magnesium sulfate therapy after aneurysmal subarachnoid hemorrhage. J Neurosurg 96:510–514
Author information
Authors and Affiliations
Corresponding author
Additional information
Comments
Carl Muroi, Zürich, Switzerland
The potential prophylactic benefit of systemic magnesium sulfate (Mg) application has been evaluated in more than ten clinical trials with some remarkable results [1]. Less is known about the effect of topic Mg application. Mori et al. report a reverse of reduced cerebral blood flow (CBF) by intracisternal application of Mg in a rat subarachnoidal hemorrhage model. The reverse of vasospasm in terms of dilated spastic arteries by topic Mg application has already been documented in a rat model earlier [2]. However, in the present study, the improvement of (decreased) CBF is documented clearly, which was not done in previous studies. The shortcoming of the study is that the prophylactic aspect and the long-term effects have not been investigated.
References
1. Muroi C, Terzic A, Fortunati M, Yonekawa Y, Keller E (2008) Magnesium sulfate in the management of patients with aneurysmal subarachnoid hemorrhage: a randomized, placebo-controlled, dose-adapted trial. Surg Neurol 69:33–39
2. Ram Z, Sadeh M, Shacked I, Sahar A, Hadani M (1991) Magnesium sulfate reverses experimental delayed cerebral vasospasm after subarachnoid hemorrhage in rats. Stroke 22:922–927
Kazuhiko Nozaki, Kyoto, Japan
Cerebral vasospasm still strongly influences morbidity/mortality rates after subarachnoid hemorrhage, and new neuroprotective and anti-vasodilatory agents may improve a patient’s outcomes. Magnesium sulfate is one of the candidates against cerebral vasospasm because of its neuroprotective and vasodilatory effects, and the efficacy of its intravenous administration seems to be the same as that of nimodipine in a clinical study (Neurosurgery 58:1054–1065). In this paper, the authors focused on the effect of intracisternal infusion of magnesium sulfate on CBF using a rat double-hemorrhage model and found that 30 min of infusion on day 5 improved CBF reduction in almost all areas without any histological changes. The data provided seem to be promising, and because intracisternal thrombolysis may improve a patient’s outcome (Neurosurgery 54:326–334, 2004), the concentration of magnesium in irrigation solutions should also be adjusted for effective levels. However, further experimental studies should be performed before any clinical use. They should examine the duration of effectiveness and any side effects after continuous intracisternal infusion because cerebral vasospasm occurs and persist for 1 or 2 weeks.
Rights and permissions
About this article
Cite this article
Mori, K., Miyazaki, M., Iwata, J. et al. Intracisternal infusion of magnesium sulfate solution improved reduced cerebral blood flow induced by experimental subarachnoid hemorrhage in the rat. Neurosurg Rev 31, 197–203 (2008). https://doi.org/10.1007/s10143-008-0122-z
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10143-008-0122-z