Abstract
We report the surgical results in patients with acute cerebral main-trunk occlusion in the anterior circulation. Between April 2004 and March 2005, 26 patients were surgically treated within 24h after the onset. The occlusion occurred in the internal carotid artery in 10 patients, in the middle cerebral artery in 15, and in the anterior cerebral artery in 1. We investigated the clinical characteristics and surgical treatment and evaluated the outcome using the modified Rankin Scale (mRS). Nine patients underwent anastomosis, 14 had an embolectomy, and 3 had a carotid endarterectomy. In all the patients, revascularization was achieved, and neurological improvement was obtained. At 6months after the onset, eight (30.8%) patients showed a good recovery (defined as grade 1 on the mRS), seven (26.9%) were rated as grade 2, eight (30.8%) were grade 3, and three (11.5%) were grade 4. Manual muscle test on admission was significantly different between the good outcome and the poor outcome groups at 6months after onset. None of the patients experienced any complications related to the surgery. Early surgical revascularization can be an effective and safe treatment modality in appropriately selected patients with acute cerebral main-trunk occlusion in the anterior circulation.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
The symptoms of patients with acute cerebral main-trunk occlusion in the anterior circulation are severe and difficult to improve by any treatments; furthermore, the functional prognosis is poor, and the mortality rate is high. The revascularization rate of fibrinolysis is different in each occluded artery; it has been reported that it is approximately only 10–30% in the internal carotid artery (ICA) occlusions and 70–80% in the middle cerebral artery (MCA) occlusions [6, 11]. The National Institute of Neurological Disorders and Stroke (NINDS) reported that thrombolytic therapy by intravenous administration of a recombinant tissue plasminogen activator (t-PA) was effective in improving the prognosis of patients with acute cerebral infarction within 3h after the onset [12]. However, as cases with mild symptoms and small arterial occlusion such as lacunar stroke were included in the therapeutic subjects, cases of cerebral infarction due to main-trunk occlusion had a low revascularization rate and a poor prognosis [3, 8, 9]. In a study focusing on relatively severe cases within 6h after the onset, the efficacy has not been proven [4]. Since the prognosis is poor with conservative treatment for the acute main-trunk occlusion, we have actively performed emergency revascularization including fibrinolysis, embolectomy, and anastomosis, independently or in conjunction, on MCA occlusions, and carotid endarterectomy (CEA), embolectomy, anastomosis and stenting in ICA occlusions. There have been no reports investigating the long-term prognosis of cases in which revascularization was performed in the acute stage of the onset of cerebral infarction due to main-trunk occlusion. In this paper, we report the clinical characteristics, surgical treatment, and outcome at discharge and at 6months after the onset for patients in which surgical revascularization was performed in the cerebral ischemia due to main-trunk occlusion in the anterior circulation.
Patients and methods
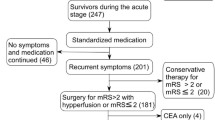
Treatment protocol
Our treatment protocol for acute cerebral main-trunk occlusion in the anterior circulation was as follows. A computed tomography (CT) scan was performed immediately after admission. If a CT scan disclosed no abnormalities or no new lesions and severe neurological deficits indicating a main-trunk occlusion were present, cerebral angiography was done. Intra-arterial fibrinolysis was performed using urokinase in patients with embolic occlusion in the main trunk of the MCA or anterior cerebral artery (ACA). If revascularization was not achieved in the patients undergoing intra-arterial fibrinolysis or if the diagnosis was an ICA occlusion, surgical revascularization would be conducted as soon as possible by confirming no new lesions on CT scans and magnetic resonance (MR) images after angiography. Patients with an occlusion of the intracranial ICA, MCA, or ACA would undergo either an embolectomy or anastomosis. Patients with an occlusion of the cervical ICA would be treated by either a CEA, anastomosis, or intravascular stent surgery.
Patients
Between April 1, 2004 and March 31, 2005, 654 patients with ischemic stroke were treated. Twenty-six consecutive patients underwent surgical treatment within 24h of the onset of acute cerebral stroke in the anterior circulation. Twelve with embolic MCA occlusion among 26 patients underwent intra-arterial fibrinolysis before surgical intervention that failed. Endovascular therapy was not performed on 14 patients because of ICA occlusion or not-embolic occlusion. Twenty-one patients were men and five were women. The mean age was 74.0 (range 56 to 88) years. All patients showed severe neurological deficits such as acute hemispheric symptoms on admission. ICA occlusion was evident in 10 patients, MCA occlusion was present in 15, and ACA occlusion was present in 1 (Table 1).
Outcomes
The outcome at discharge and 6months after the onset of the stroke was evaluated using the modified Rankin Scale (mRS). Grade 0 on the mRS was defined as the absence of symptoms. Grade 1 was defined as no significant disability despite some symptoms (the individual was able to carry out all his/her usual duties and activities). Grade 2 was the presence of a slight disability (the patient was unable to carry out all previous activities but was able to look after his/her own affairs without assistance). Grade 3 was considered to be moderate disability (the patient required some help but was able to walk without assistance). Grade 4 was moderately severe disability (the patient was unable to walk without assistance and cannot attend to his/her own physical needs without assistance). Grade 5 on the mRS was severe disability (the patient was bedridden, incontinent, and requires constant nursing care and attention). Grade 6 was equivalent to death.
Statistical analyses
A statistical analysis was performed based on the clinical characteristics between the good (grade 0 or 1 or 2 on the mRS) and the poor (grade 3 or 4 or 5 on the mRS) recovery groups at 6months after the onset of the stroke using Fisher’s exact probability test or the Mann–Whitney U test. A P value of less than 0.05 was regarded as statistically significant.
Results
Regarding the surgical treatment of cerebral ischemia in the acute stage, anastomosis was carried out in 9 patients, an embolectomy in 14, and a CEA in 3 (Table 1). Superficial temporal artery–middle cerebral artery (STA–MCA) anastomosis was performed in five patients with an ICA occlusion and three patients with an MCA occlusion. Superficial temporal artery (STA)–STA graft-ACA anastomosis was carried out in one patient with a left ACA occlusion. An embolectomy was performed in 2 patients with an intracranial ICA occlusion and 12 with an MCA occlusion. In all the patients, revascularization was intraoperatively confirmed by a Doppler flowmeter and postoperatively confirmed by angiography and/or echosonography. The mean time from onset to revascularization was 310.1min in 15 patients except for the patients with an unknown onset time or a gradual worsening of the symptoms. There were no complications related to surgery during the intraoperative and postoperative courses. No hemorrhagic complications were evident in any of the patients. Postoperatively, in all the patients neurological findings improved (Table 1 and Fig. 1). At discharge, the mRS was grade 1 in two patients (7.7%), grade 2 in seven (26.9%), grade 3 in five (19.2%), grade 4 in nine (34.6%), and grade 5 in three (11.5%) (Fig. 1). The average length of hospital stay in our hospital was 26 (range, 9–66) days. Three patients conducting all of their daily activities without assistance were discharged home, and 23 were transferred to in-patient rehabilitation services. The 6-month outcome after the onset according to the mRS was grade 1 in eight patients (30.8%), grade 2 in seven (26.9%), grade 3 in eight (30.8%), and grade 4 in three (11.5%; Fig. 1). None of the patients were classified as grade 5. All patients were alive after 6months. In addition, no patient experienced a recurrent cerebral infarction during 6months after the surgery.
With regard to prognostic factors between the good-outcome and the poor-outcome groups at 6months after onset, manual muscle test (MMT) on admission was significantly different. A statistical analysis of the clinical characteristics including sex, age, Glasgow Coma Scale (GCS) on admission, aphasia on admission, mRS on admission, side of the lesion, occluded artery, and time to recanalization showed no significant differences (Table 2).
Illustrative cases
Case 1
A 70-year-old man was admitted to our hospital with sudden onset of consciousness disturbance and left hemiparesis (MMT 2) and a conjugate deviation of the eyes to the right side. A CT scan and MR image showed no abnormal lesions except for an old watershed infarction (Fig. 2a). Angiography showed right ICA occlusion (Fig. 2b). CT scans taken immediately after angiography revealed no new lesions. Emergency STA–MCA anastomosis was performed. Revascularization in the right hemisphere was achieved approximately 310min after the onset. Postoperative MR perfusion studies demonstrated adequacy of perfusion of the right cerebral hemisphere through the STA (Fig. 2c).
Postoperative MR angiography showed an adequate perfusion of the right cerebral hemisphere through the STA (Fig. 2c). His symptoms improved after the operation, and he returned home 9days later with mild left hemiparesis (MMT 4). He was able to walk without a cane upon his discharge. At 6months after onset, he carried out all his usual duties and activities.
Case 9
A 75-year-old man had noticed a gradual worsening of mild right motor weakness. He was referred to our hospital and showed progressive deterioration of his symptoms, such as apathy, poor activity, right hemiparesis (MMT 1), and aphasia. CT scans revealed a cerebral infarction in the territory of the left ACA (Fig. 3a,b). Angiography showed an occlusion of the left ACA without collateral circulation (Fig. 3c,d). Initial endovascular therapy was not attempted. Emergency surgical revascularization, an STA–STA graft-A4 bonnet bypass, was conducted to improve his neurological deficits and prevent any further neurological deficits due to a complete cerebral infarction of the left ACA occlusion. Postoperative neuroimages revealed no fresh ischemic lesions. Neurological examinations showed the right motor weakness, and aphasia improved. Postoperative angiography revealed good perfusion of the left ACA area through the bypass (Fig. 3e–g). He was transferred to another hospital for rehabilitation 50days after the operation. At discharge, he had right motor weakness (MMT 3) and was not ambulant without assistance. At 6months after onset, however, he returned home ambulantly without assistance.
Case 9. A 75-year-old man. a, b CT scans showing low density area in the territory of the left anterior cerebral artery. c Right carotid angiogram (anteroposterior view) and d left carotid angiogram (anteroposterior view) showing occlusion of the left A2 without collateral circulation. e–g Left external carotid angiogram (e anteroposterior veiw and f, g lateral view) demonstrating left anterior cerebral artery from the anastomosis
Case 10
An 82-year-old woman having a history of arrhythmia was admitted to our hospital with a sudden onset of left hemiplegia, dysarthria, and conjugate deviation of the eyes to the right side. A CT scan and MR image disclosed no abnormalities (Fig. 4a). Cerebral angiography showed an embolic occlusion of the right ICA with a fair degree of collateralization (Fig. 4b,c). CT scans taken immediately after the angiography also revealed no new lesions. With an emergency embolectomy, revascularization in the right hemisphere was achieved approximately 230min after the onset of the stroke. Her symptoms gradually improved after the operation. Postoperative CT scans showed a small low-density area in the right globus pallidus. Postoperative angiography confirmed the right ICA revascularized (Fig. 4d,e). She was transferred to another hospital for rehabilitation 24days after onset. At discharge, she was able to walk without a cane, and her speech was normal. Six months after the onset, she returned to a homemaker and showed no motor weakness.
Case 10. A 82-year-old woman. a Axial diffusion weighted MRI showing no abnormalities. b Right carotid artery angiogram (lateral view) showing occlusion of the right internal carotid artery. c Left carotid artery angiogram (anteroposterior view) showing complete occlusion at the right A1 without collateral circulation. d, e Right carotid angiogram (d anteroposterior view and e lateral view) after embolectomy demonstrating recanalization of the occluded artery
Case 24
An 81-year-old man with a past history of cerebral infarction was admitted to our hospital due to a sudden onset of left hemiparesis (MMT 2), neglect to the left side, and conjugate deviation to the right. A CT scan showed no new lesions. Cerebral angiography revealed complete occlusion of the right cervical ICA (Fig. 5a,b). A CT scan taken immediately after the angiography revealed no abnormalities. An emergency CEA was performed; and revascularization in the right hemisphere was achieved approximately 5h after the onset. Postoperative MR images showed no major infarction except for a small cortical infarction in the right frontal lobe (Fig. 5c). Postoperative MR angiography revealed adequate perfusion in the right cervical ICA region (Fig. 5d). His symptoms gradually improved after the operation, and he was transferred to another hospital for rehabilitation 26days after the onset. At discharge, he had mild left motor weakness (MMT 4) and was ambulant with a cane. At 6months after the onset, he returned home carrying out all usual duties and activities.
Case 24. An 81-year-old man. a Right carotid angiogram (lateral view) showing a near occlusion of the right cervical ICA. b Left carotid angiogram (anteroposterior view showing fair collateral circulation. c Axial MRI showing a small cortical infarction. d Magnetic resonance angiogram after CEA demonstrating resolution of the right ICA occlusion
Discussion
In all patients with surgical intervention on cerebral main-trunk occlusions of the anterior circulation in the present study, revascularization was achieved followed by neurological improvement. There were no postoperative hemorrhages, no complications in the perioperative period, and no mortalities. Good results were obtained, with approximately 90% of patients able to walk 6months after the onset, and it is thus considered to be an effective treatment. They showed consciousness disturbance and severe hemiplegia, which were considered to be due to a hemodynamic mechanism in the cortical area. We then conducted surgery in order to improve the blood flow in the cortical area. A surgical intervention was performed after ensuring no cerebral infarction recognized on CT and/or magnetic resonance imaging (MRI). We have found that an excessive blood flow caused by revascularization can be prevented by controlling the blood pressure, and it rarely leads to hemorrhagic infarction. Our cases comprise therapeutic experiences before t-PA was approved in Japan (approval from October 2005). It is therefore necessary to investigate more cases in order to establish an effective treatment protocol in the future. We, however, consider that the prognosis can be improved in some cases by surgical treatment in the acute stage for main-trunk occlusion in the anterior circulation, which is generally considered resulting in a poor prognosis [3, 4, 8, 9]. On the other hand, we evaluate the patients using perfusion CT as the cerebral blood flow (CBF) study. Because a great amount of contrast agent needs to be used and it takes time in the acute stage, we did not perform cerebral blood flow measurements in our present study. However, we consider the necessity of cerebral blood flow measurement and will add it as a treatment protocol in the near future.
We have reported that an embolectomy for acute MCA occlusion is a treatment option [5]. In the present study, 10 (83%) out of 12 patients with MCA occlusion treated by embolectomy were able to walk without assistance at 6months after the onset. There are several authors reporting on the effectiveness of embolectomy for MCA occlusion [7, 13]. Because the revascularization rate of fibrinolysis is approximately 80% [11] and the main-trunk occlusion cases have a poor prognosis, an embolectomy is thus considered to be one of effective treatments for cases with MCA occlusion in which revascularization was not achieved or an improvement of symptoms was not obtained. In cases 10 and 11, an embolectomy was performed for the ICA occlusion. The former showed a good outcome, as the patient was independently ambulant at discharge; the latter demonstrated grade 4 at mRS at 6months from the onset but better than at onset. It is assumed that the differences between them might be due to the differences in the degree of collateral flow. As Touho et al. [13] reported that an embolectomy for occlusion of the ICA bifurcation was effective, it can be also effective for certain cases with carotid artery occlusion in the acute stage.
There have been reports in which STA–MCA anastomosis is effective for obtaining a neurological improvement in the acute stage [1, 15]. It is considered that postoperative hemorrhagic infarction can thus be avoided by intentionally selecting a low-flow bypass in the acute cerebral infarction [1, 15]. In our cases, not only was STA–MCA anastomosis effective in the acute MCA occlusion, but also in one case of ACA occlusion, and in five cases of carotid artery occlusion, STA–MCA anastomosis was effective. Even when performing thrombolytic therapy by either intravenous or regional arterial administration as a treatment for either intracranial or extracranial carotid artery occlusion, the revascularization rate is mostly low, and the prognosis is poor [3, 6, 11]. The risk of hemorrhage is high, even though it is revascularized, and no effective treatments have yet been established [6, 11]. From the findings of our investigation, there are cases of carotid artery occlusion in which STA–MCA anastomosis or an embolectomy is effective in the acute stage. When the efficacy and safety of thrombolytic therapy cannot be assured for the acute treatment of carotid artery occlusion, STA–MCA anastomosis or embolectomy can be an effective surgical treatment for preventing cerebral infarction. On the other hand, regarding the treatment for acute cervical carotid artery occlusive lesions, medical treatment such as anticoagulant therapy is currently a common treatment option [2]. There have been, however, reports of acute-staged non-medical revascularization being performed [2, 10, 14]. These include percutaneous revascularization and CEA, but due to the potential occurrence of hyperperfusion and embolus to the peripheral areas and reocclusion, the appropriateness of this treatment has not yet been determined. In our present study, three patients underwent CEA for cervical carotid artery occlusion, but in all of the patients the length of the stenotic section was unknown, and CEA was performed with the risk of inducing an embolus in the periphery.
There are various factors affecting the prognosis in the main-trunk occlusion cases: how much collateral circulation has developed, whether the lesion site is left or right, the conditions on admission (severity), and the period from the onset to revascularization. In our cases, no factors were observed significantly affecting outcome except for MMT on admission. There was a tendency, however, that maintained leptomeningeal anastomosis and earlier revascularization resulted in better outcome. In the previous case report, good outcome was obtained when revascularization was performed within 6h for acute cerebral infarction [7]; however, in our investigation, there are patients having a good outcome undergoing revascularization longer than 6h after the onset. In these cases, the collateral circulation was maintained to some degree but not adequate enough.
We have conducted various attempts to shorten the time from the onset to treatment (revascularization) as much as possible. To shorten the time to convey patients to a hospital, we have held educational lectures to the public and held seminars for emergency crews and healthcare professionals. In addition, at our hospital, once we have a call from an emergency crew, we immediately communicate with the emergency department, examination department, and nursing department to promptly make preparations to accept a patient and prepare for the ambulance to arrive. At our hospital, we have also established clinical paths and, therefore, after the arrival of a patient, we immediately proceed to make a diagnosis, examine, and start treatment according to the protocol. We therefore consider it is important to shorten the time from the onset to treatment in order to achieve successful revascularization to the greatest degree possible.
Conclusion
We reported that patients with cerebral ischemia due to cerebral main-trunk occlusion in the anterior circulation were successfully treated by emergency surgical intervention in the acute stage. Our current study indicates that neurological findings improved in all of the patients, and no major complication developed such as intracranial hemorrhage postoperatively. Emergency surgical recanalization can achieve good recovery even in patients with the main-trunk occlusion of the anterior circulation.
References
Batjer H, Mickey B, Samson D (1986) Potential roles for early revasculaization in patients with acute cerebral ischemia. Neurosurgery 18:283–291
Brandl R, Brauer RB, Maurer PC (2001) Urgent carotid endarterectomy for stroke in evolution. VASA 30:115–121
Derex L, Hermier M, Adeleine P, Pialat JB, Wiart M, Berthezene Y, Froment JC, Trouillas P, Nighoghossian N (2004) Influence of the site of arterial occlusion on multiple baseline hemodynamic MRI parameters and post-thrombolytic recanalization in acute stage. Neuroradiology 46:883–887
Hacke W, Kaste M, Fieschi C, von Kummer R, Davalos A, Meier D, Larrue V, Bluhmki E, Davis S, Donnan G, Schneider D, Diez-Tejedor E, Trouillas P (1998) Randomized double-blind placebo-controlled trial of thrombolytic therapy with intravenous alteplase in acute ischemic stroke (ECASS II). Second European-Australasian Acute Stroke Study Investigators. Lancet 352:1245–1251
Horiuchi T, Nitta J, Sakai K, Tanaka Y, Hongo K (2007) Emergency embolectomy for treatment of acute middle cerebral artery occlusion. J Neurosurg 106:257–262
Jansen O, von Kummer R, Forsting M, Hacke W, Sartor K (1995) Thrombolytic therapy in acute occlusion of the intracranial internal carotid artery bifurcation. Am J Neuroradiol 16:1977–1986
Kakinuma K, Ezuka I, Takai N, Yamamoto K, Sasaki O (1999) The simple indicator for revascularization of acute middle cerebral artery occusion using angiogram and ultra-early embolectomy. Surg Neurol 51:332–341
Kim YS, Garami Z, Mikulik R, Molina CA, Alexandrov AV (2005) Early recanalization rates and clinical outcomes in patients with tandem internal carotid artery/middle cerebral artery occlusion and isolated middle cerebral artery occlusion. Stroke 36:869–871
Linfante I, Llinas RH, Selim M, Chaves C, Kumar S, Parker RA, Caplan LR, Schlaug G (2002) Clinical and vascular outcome in internal carotid artery versus middle cerebral artery occlusions after intravenous tissue plasminogen activator. Stroke 33:2066–2071
McPherson CM, Woo D, Cohen PL, Pancioli AM, Kissela BM, Carrozzella JA, Tomsick TA, Zuccarello M (2001) Early carotid endarterectomy for critical carotid artery stenosis after thrombolysis therapy in acute ischemic stroke in the middle cerebral artery. Stroke 32:2075–2080
Sasaki O, Takeuchi S, Koike T, Koizumi T, Tanaka R (1995) Fibrinolytic therapy for acute embolic stroke: intravenous, intracarotid, and intra-arterial local approaches. Neurosurgery 36:246–253
The National Institute of Neurological Disorders and Stroke rt-PA Stroke Study Group (1995) Tissue plasminogen activator for acute ischemic stroke. N Engl J Med 333:1581–1587
Touho H, Morisako T, Hashimoto Y, Karasawa J (1999) Embolectomy for acute embolic occlusion of the internal carotid artery bifurcation. Surg Neurol 51:313–320
Walters BB, Ojemann RG, Heros RC (1987) Emergency carotid endarterectomy. J Neurosurg 66:817–823
Yoshimoto Y, Kwak S (1995) Superficial temporal artery – middle cerebral artery anastomosis for acute cerebral ischemia: The effect of small augmentation of blood flow. Acta Neurochir (Wien) 137:128–137
Author information
Authors and Affiliations
Corresponding author
Additional information
Comments
Michael Reinert, Bern, Switzerland
The authors have performed either a low-flow extracranial-to-intracranial (EC–IC) bypass, embolectomy, or CEA in patients with acute onset of neurological deficit due to vascular occlusion, in a time frame around the 6-h limit. Surgical intervention has been performed either if endovascular procedures failed or if it was deemed to fail from the beginning. Emergency revascularization is a safe procedure and should be considered by the stroke team in these situations, also in patients with maintained but insufficient leptomeningeal collateralization.
Rights and permissions
About this article
Cite this article
Sakai, K., Nitta, J., Horiuchi, T. et al. Emergency revascularization for acute main-trunk occlusion in the anterior circulation. Neurosurg Rev 31, 69–76 (2008). https://doi.org/10.1007/s10143-007-0116-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10143-007-0116-2