Abstract
Glial tumors are the most common tumors of the nervous system, affecting individuals at any age. Since understanding of the molecular pathologies underlying human gliomas is still very poor, the treatment and therefore prognosis of this malignancy could not yet be improved. In order to determine whether different glioblastoma-associated genomic aberrations may serve as prognostic markers in combination with histopathological findings, 20 primary glioblastoma multiforme tumors were screened by comparative genomic hybridization, and the results were compared with histopathological and clinical features. All tumors showed genomic copy aberrations detected by comparative genomic hybridization. Regional and numerical increases in chromosome 7 copy number were the most frequently seen abnormality (10/20 tumors), followed by loss of chromosome 10 (8/20). Both of these aberrations were associated with shorter surveillance time. Chromosome 12q amplification was detected in seven tumors. Loss of 17p, 1p, and 19q in combination was seen in three cases. One of them was a giant cell GBM, whereas the remaining two cases were still alive. Combination of chromosome 1p and 19q deletions was also seen in a case with long surveillance. According to the preliminary findings of this study, in addition to the EGFR gene, amplification of other genes on chromosome 7 and the deletion of PTEN gene and other cancer-related genes on chromosome 10 appeared important to the development of glioblastoma multiforme and were associated with poor prognosis, whereas the combination of chromosome 1p and 19q deletions seems to be an informative molecular marker for better prognosis. The clinical features and genetic alterations of primary and secondary glioblastoma multiforme should be compared in large series to clarify the effective prognostic markers; and further molecular analyses focused on chromosomes 7 and 10 will be very helpful for understanding the molecular mechanisms underlying the progression of glioblastoma.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Glioblastoma multiforme (GBM) is the most common and most malignant central nervous system malignancy. It affects individuals at any age but has a predilection for adults. Although visible progress has been made in its diagnosis, the prognosis remains very poor [1]. Genetic alterations such as amplification of oncogenes and deletion of tumor suppressor genes have been shown to accumulate during carcinogenesis of malignant tumors [2]. Our abilities to stratify and treat these malignancies effectively are still very limited, since their development and progression, particularly the underlying molecular genetic alterations, are poorly understood at present.
Tumor classification and grading are necessary tools in the practice of medicine but are neither static nor resistant to progress. Several classification and grading schemes have been reported for human neoplasms, and most have relied on histopathological and immunohistochemical results [3, 4]. However, during the past decade, by improving molecular genetic techniques, our knowledge of the genetic basis of human malignancies has increased greatly and, for many neoplasms, cytogenetic and molecular genetic profiles become definitive criteria for classification. Different classification schemes have been reported for astrocytic brain tumors, and glioblastoma has been at the center of these efforts [3].
Necrosis, thrombosis, microvascular proliferation, and increased proliferation have been established as typical histopathological features of GBM [5, 6]. However, recent studies have identified different genomic alterations in histologically defined GBMs. Well-known recurrent chromosomal aberrations include losses of chromosomes 1p, 9p, 10, 13q, 17p, 19q, and 22, mutations of tumor suppressor genes such as CDKN2, PTEN, DMBT1, and p53, gain and/or amplification on chromosomes 7 and 12, and amplification and/or overexpression of genes such as EGFR, myc-N, PDGFR, MDM 2, and GLI [7, 8, 9, 10, 11, 12, 13]. These results indicate that these genomic aberrations are likely to be associated with the development of GBM. However, differences in the frequency of distinct molecular alterations in clinically defined GBM subgroups have been established. For instance, primary glioblastomas are characterized by EGFR amplification and/or overexpression, PTEN mutations, p16 deletion, MDM 2 amplification and/or overexpression, and complete loss of chromosome 10. In contrast, secondary glioblastomas contain p53 mutations in approximately 60% of cases and are further characterized by 19q and 10q deletions [3, 14, 15].
Histopathologically, clear distinction of these subtypes has remained elusive, but their development seems to be based on different genetic pathways. Furthermore, the differences in prognosis and therapeutic responses to specific therapies of these subtypes remain to be shown. The present study was designed to answer the question of whether different glioblastoma-associated genomic aberrations may serve as prognostic markers in combination with histopathological findings. The clinical, histopathological, and genomic copy alterations were compared.
Materials and methods
Tumor material
Histopathological, immunohistopathological, and comparative genomic hybridization (CGH) analyses were performed in tumor specimens from 20 adult patients. The ratio of males to females was 15:5. Patient age ranged from 30 to 72 years, with a mean of 53.15±10.80. Tumor specimens were classified as GBM grade IV according to the World Health Organization (WHO) classification of tumors of the central nervous system [3]. All tumor samples were available as formalin-fixed and paraffin-embedded material. For each tumor, four serial sections were obtained. The first and last sections were stained with hematoxylene and eosin (H&E) for histopathological analysis to ensure that the most cellular and anaplastic areas were selected from each tumor for further analysis. The remaining two sections were used for immunohistochemical and CGH studies.
Histopathological and immunohistochemical analysis
Histopathological and immunohistochemical parameters were chosen according to Schmidt et al. [4]. For each tumor, the predominant cell type, other major cell types, and additional cell types were assessed. Cell proliferation was evaluated by counting mitoses and determining the fraction of Ki-67-positive nuclei (clone MB67) (Neomarkers, USA). Necroses, microvascular proliferation, sarcomatous growth, degree of lymphocytic infiltration, thromboses, and calcification status of each tumor were also determined. The expression of glial fibrillary acidic protein (GFAP) (clone GA-5) (Neomarkers) was examined and divided into three categories: single cells, groups of cells, and more than 30% of the tumor cells.
Comparative genomic hybridization
Identification of DNA sequence copy number changes was accomplished by CGH as described previously [16]. Tumor DNA isolated from 15-μm sections of formalin-fixed, paraffin-embedded glioma tissue and reference DNA from the peripheral blood of a karyotypically normal male were amplified and labeled with fluorochromes using two rounds of degenerate oligonucleotide primed polymerase chain reaction (DOP-PCR) with the primer 6 MW (5'-CCGACTCGAGNNNNNNATGTGG-3'). Test and normal DNA probes were generated in a secondary labeling DOP-PCR reaction by incorporation of spectrum green (Vysis, Downers Grove, Ill., USA) and spectrum red (Vysis) directly conjugated nucleotides, respectively.
Slides were viewed on an Axiophot fluorescence microscope (Zeiss, Oberkochen, Germany), and images were captured and stored using a photometrics CCD camera with MacProbe version 4.11 software (Perceptive Scientific International, Chester, UK). For each hybridization, at least ten high quality metaphases were analyzed, and average green-to-red fluorescence intensity ratio profiles were generated for each chromosome. Comparative genomic hybridization ratios of 1:20 and 0:80 were used as the upper and lower thresholds, respectively, for identifying chromosomal imbalances. Any shifts in the mean green:red ratio above 1:20 were considered to indicate gains in chromosomal material, and shifts below 0:80 indicated losses. The procedures in experiments on samples in this study were in accordance with the Helsinki Declaration of 1975.
Results
We studied a series of 20 primary GBMs from adult patients. Fifteen patients were male and five were female, reflecting the male predominance among GBM patients. Patient age ranged from 30 to 72 years, with a mean of 53.2±10.8 (females 52.8±17.3, males 53.3±8.5). Survival for all patients averaged 10.0±5.6 months, with means of 9.6±5.9 for females and 11.6±5.4 for males.
Preoperative functional status was evaluated according to the Karnofsky performance status (KPS) scale. Eleven cases scored 80–100, whereas nine scored 70 or less. Fourteen cases received fractionated radiotherapy, and the tumors were reoperated in 13 patients. The tumor locations were the frontal lobe in five patients, parietal in seven, temporal in six, and occipital in one.
Table 1 summarizes the histopathological findings of GBMs. Seventeen tumors were primary GBM, and giant cell GBM was diagnosed in three cases. During the histopathological examination, necrosis in extensive areas was detected in 12 tumors. No sarcomatous growth was seen, but focal growth was detected in 12 tumors (Table 1).
Comparative genomic hybridization showed all tumors to have genomic copy aberrations (Table 2, Fig. 1). The most commonly detected chromosomal mutation involved chromosome 7, for which increased fluorescence signal intensity was observed in ten tumors. Four of these ten had complete chromosome 7 gain or amplification, whereas the remaining six showed amplification localized to a narrow chromosomal region consistent with band 7p13. The second most common increased signal intensity was restricted to a specific band consistent with 12q13–q15. It was seen in seven tumors. The other increased fluorescence intensity, detected in three tumors, involved chromosome 1. Involvement of partial regions of this chromosome was not detected.
The increased copy number changes involved whole chromosome or chromosomal arms other than chromosomes 1 and 7, and 12 were revealed in individual tumors. These genomic aberrations were chromosomes 6, 9q, 15q, 17q, and 20p. The number of increased copying per tumor was 1.35 in the present study.
Signal reductions indicative of deletions were also observed, and the number of deletions per tumor was 1.60. Loss of the entire chromosome 10 was the most commonly seen genomic loss; it was seen in eight tumors. Loss of chromosomes 1p, 17p, and 19q were other frequently seen deletions and each was observed in four tumors. Chromosomes 9p and 19q and whole chromosome 22 deletions were detected in three cases each, and the remaining deletions including chromosomes 3p, 5p, 11p, 13q, 16p, and 21 were present in individual tumors.
Combined molecular aberrations
Combinations of chromosome 1p and 17p13-p14 and 19q deletions were detected in three patients. Two of them were still alive at the time of data compilation, whereas the survival time in the other case was 15 months, higher than the mean value. On the other hand, loss of 1p and 19q was seen together in the case with 13-month surveillance.
It was interesting that whole chromosome 10 deletions were the common abnormality among patients with shorter surveillance times (5.4±3.3 months). On the other hand, five GBMs with surveillance below the mean value (5.0±3.1 months) showed combined loss of chromosome 10 and amplification of whole chromosome 7/7p11–p13 gain/amplification. Chromosome 7 alterations without loss of chromosome 10 were seen in four cases, whereas it was lost in two.
Combined chromosome 9p deletion and 12q amplification were present in four cases with GBM. Amplification in the chromosome 12q13–q15 region without loss of chromosome 9p was seen in two cases. No tumor was present with 9p deletion but without 12q amplification.
Loss of chromosome 10 and gain/amplification in chromosome 7 were more frequently observed in tumors with microvascularization. Chromosome 10 deletion was also the common abnormality in five tumors with extensive lymphocytic infiltration.
Discussion
Although GBM is the most common and most malignant central nervous system malignancy, the ability to treat it effectively and improve prognosis are still very limited because of poor understanding of the underlying molecular mechanisms. Young age, preoperative Karnofsky score, tumor size, gross complete removal, tumor localization, and the presence of giant tumor cells and good differentiated areas have been reported as clinical and histopathological parameters involved in good prognosis [4, 17]. However genetic markers related to better prognosis of GBM patients could not be differentiated yet.
Younger age at diagnosis has been reported as one of the significant parameters of better prognosis [4, 17, 18]. This tendency was also detected in this study, reflected in survival time and clinical features. Numerous complete or partial chromosomal gains/amplifications and deletions were identified by CGH in our 20 GBMs. The most frequently seen aberrations were gain/amplification of whole or partial chromosome 7 and loss of chromosome 10, which were previously reported as frequent abnormalities in primary GBMs. Whole or partial amplification of chromosome 7 has been reported as the most striking microscopically detectable aberration, and the presence of this genomic alteration shows a preferential involvement of this chromosome, supporting the pivotal role on chromosome 7 sequences in the biology of human gliomas. The EGFR gene was localized in the 7p11.2 region, and its overexpression has been shown in about 60% of primary GBMs [3, 10,11, 12, 19, 20]. In our series, amplification in the chromosome 7p11–p13 region, corresponding to the EGFR gene, was detected in five of ten tumors. No additional amplified regions of chromosome 7 were seen in our series, in contrast to others.
Whole chromosome 7 gain/amplification detected by CGH indicates numerical abnormality in the tumors, and polysomy 7 detected by cytogenetics and molecular cytogenetics analysis has been frequently reported [10, 11]. Both regional and numerical increases in chromosome 7 copy number therefore appear to be important in the development of GBM. In addition to the EGFR gene, other yet unknown cellular oncogenes and genes involved in cancer progression might be localized in the other regions of chromosome 7.
According to the results of our series, loss of whole chromosome 10 was associated with poor prognosis. The importance of this chromosome aberration in the prognosis of GBM has been reported previously [4, 20, 21, 22, 23]. The PTEN gene (MMAC1) cloned at 10q23.3 is a tumor suppressor gene and was shown to be inactivated by deletion and mutation in about 30% of glioblastomas. Chromosome 10q25-qter deletion has been detected frequently during the progression of meningiomas [16] and, because of the inactivation of the PTEN gene or other yet unknown tumor suppressor genes, chromosome 10q aberrations have been regarded as important in tumor progression. Such an association has also been indicated in human gliomas [22, 23], and therefore further molecular studies focused on chromosome 10 might help in understanding the biological mechanism(s) underlying the gliomas.
In the present series, a tendency toward the combination of chromosome 7/7p amplification with chromosome 10 deletion was seen in the tumors with poor prognosis. If such a relationship is confirmed, this feature is in accordance with the molecular basis of cancer development. Many oncogenes and mutant tumor suppressor genes are involved during tumor progression, and finally multiple mutations of these cancer-related genes are present in high-grade tumors. Colorectal carcinomas, prostate cancer, and renal cell tumors are some of the clear examples of tumor initiation and progression during the development of common human malignancy [24].
Several studies have pointed to a higher frequency of chromosome 17 deletion and/or p53 mutations in secondary GBMs [3, 15, 22, 25, 26, 27], which contain p53 mutations in approximately 60% of cases. In the present study, the partial loss on chromosome 17p was seen in four cases, with a consensus region of 17p13-p14. Schmidt et al. [4] showed the importance of p53 mutations to good prognosis. Our results showed this tendency as well, but the possible importance of this gene mutation should be clarified by the comparison of primary and secondary GBM patients in large series.
Several studies have shown that p53 mutations rarely occur in combination with EGFR amplification. In the present one, no such combination could be detected. However, the combination of 1p, 17p13-p14, and 19q deletions was seen in three cases. Two of these patients were still alive during preparation of this study. One of them was the giant cell GBM case with a survival time of 15 months. The CGH analysis showed 1p and 19q deletions in the tumor sample of the case with 13-month surveillance time. No isolated loss of 1p or 19q was seen. The surveillance times of these cases were higher than the mean value.
In oligodendroglial tumors, LOH1p and LOH19q have been indicated in better survival and favorable response to chemotherapy [15, 28, 29, 30, 31]. These deletions have also been reported in GBMs but at lower frequencies [4]. In our series, such a tendency could be seen but, due to the relatively small number of patients, no firm conclusion can be drawn about patient survival.
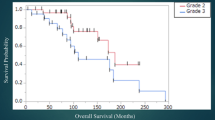
In summary, according to our preliminary findings, loss of chromosome 10 and chromosome 7/7p amplification are specific molecular markers associated with poor prognosis. Further molecular studies focusing on these chromosomes will be very helpful in understanding the underlying biological mechanisms of human gliomas. Moreover, the clinical and genetic alterations of primary and secondary GBMs should be compared in large series to clarify the effective prognostic markers (Fig. 1).
Summary of genetic copy number imbalances detected by CGH in 20 GBM cases. Losses are indicated by lines on the left of each chromosome ideogram, whereas lines on the right show gains. Chromosome regions to which amplification sites could be mapped and amplification of sequences in whole chromosome 7 are indicated by thick lines
References
Scott, JN, Rewcastle NB, Brasher PM, Fulton D, Hagen N, MacKinnon JA, Sutherland G, Cairncross JG, Forsyth P (1998) Long term glioblastoma multiforme survivors: a population based study. Can J Neurol Sci 25:197–201
Cooper GM (1997) The cell. Oxford University Press, New York
Kleihues P, Louis DN, Scheithauer BW, Rorke LB, Reifenberger G, Burger PC, Cavanee WK (2002) The WHO classification of tumors of the nervous system. J Neuropathol Exp Neurol 61:215–225
Schmidt MC, Antweiler S, Urban N, Mueller W, Kuklik A, Meyer-Puttlitz B, Wiestler OD, Louis DN, Fimmers R, Von Deimling A (2002) Impact of genotype and morphology on the prognosis of glioblastoma. J Neuropathol Exp Neurol 61:321–328
Burger PC, Vollmer RT (1980) Histologic factors of prognostic significance in the glioblastoma multiforme. Cancer 46:1179–1186
Burger PC, Vogel FS, Green SB, Strike TA (1985) Glioblastoma multiforme and anaplastic astrocytoma. Pathologic criteria and prognostic implications. Cancer 56:1106–1111
Jung V, Romeike FM, Henn W, Feiden W, Moringlane JR, Zang KD, Urbschat S (1999) Evidence of focal genetic microheterogenity in glioblastoma multiforme by area-specific CGH on microdissected tumor cells. J Neuropathol Exp Neurol 58:993–999
Rey JA, Bello MJ, de Campos JM, Kusak ME, Moreno S (1987) Chromosomal composition of a series of 22 human low-grade gliomas. Cancer Genet Cytogenet 29:223–237
Bigner SH, Mark J, Burger PC, Mahaley MS, Bullar DE, Muhlbaier LH, Bigner DD (1988) Specific chromosomal abnormalities in malignant human gliomas. Cancer Res 88:405–411
Brunner C, Jung V, Henn W, Zang KD, Urbschat S (2000) Comparative genomic hybridization reveals recurrent enhancements on chromosome 20 and in one case combined amplification sites on 15q24q26 and 20p11p12 in glioblastomas. Cancer Genet Cytogenet 121:124–127
Schröck E, Thiel G, Lozanova T, du Manoir S, Meffert M-C, Jauch A, Speicher MR, Nürnberg P, Vogel S, Janisch W, Donis-Keller H, Ried T, Witkowski R, Cremer T (1994) Comparative genomic hybridization of human malignant gliomas reveals multiple amplification sites and nonrandom chromosomal gains and losses. Am J Pathol 144:1203–1218
Weber R, Sommer C, Albert F, Kiessling M, Cremer T (1996) Clinically distinct subgroups of glioblastoma multiforme studied by comparative genomic hybridization. Lab Invest 74:108–119
Mao X, Hamoudi RA (2000) Molecular and cytogenetic analysis of glioblastoma multiforme. Cancer Genet Cytogenet 122:87–92
Maruno M, Yoshimine T, Ghulam Muhammad AKM, Ninomiya H, Kato A, Hayakawa T (1999) Chromosomal aberrations detected by comparative genomic hybridization (CGH) in human astrocytic tumors. Cancer Lett 135:61–66
Weber RG, Sabel M, Reifenberger J, Sommer C, Oberstrass J, Reifenberger G, Kiessling M, Cremer T (1996) Characterization of genomic alterations associated with glioma progression by comparative genomic hybridization. Oncogene 13:983–994
Arslantas A, Artan S, Oner U, Durmaz R, Muslumanoglu MH, Atasoy MA, Basaran N, Tel E (2002) Comparative genomic hybridization analysis of genomic alterations in benign, atypical and anaplastic meningiomas. Acta Neurol Belg 102:53–62
Durmaz R, Erken S, Arslantas A, Atasoy MA, Bal C, Tel E (1997) Management of glioblastoma multiforme: with special reference to recurrence. Clin Neurol Neurosurg 99:117–123
Obwegeser A, Ortler M, Seiwald M, Ulmer H, Kostron H (1995) Therapy of glioblastoma multiforme. A cumulative experience of 10 years. Acta Neurochir (Wien) 137:29–33
Romeike BFM, Jung V, Feiden W, Moringlane JR, Zang KD, Urbschat SM (2001) Distribution of epidermal growth factor receptor protein correlates with gain in chromosome 7 revealed by comparative genomic hybridization after microdissection in glioblastoma multiforme. Pathol Res Pract 197:427–431
Schlegel J, Scherthan H, Arens N, Stumm G, Kiessling M (1996) Detection of complex genetic alterations in human glioblastoma multiforme using comparative genomic hybridization. J Neuropathol Exp Neurol 55:81–87
Sano T, Lin H, Chen X, Langford LA, Koul D, Bondy ML, Hess KR, Myers JN, Hong K, Yung WK, Steck PA (1999) Differential expression of MMAC/PTEN in glioblastoma multiforme: relationship to localization and prognosis. Cancer Res 59:1820–1824
Leenstra S, Bijlsma EK, Troost D, Oosting J, Wesrerveld A, Bosch DA, Hulsebos TJM (1994) Allele loss on chromosome 10 and 17p and epidermal growth factor receptor amplification in human malignant astrocytoma related to prognosis. Br J Cancer 70:684–689
Balesaria S, Brock C, Bower M, Clark J, Nicholson SK, Lewis P, de Sanctis S, Evans H, Peterson D, Mendoza N, Glaser MG, Newlands ES, Fisher RA (1999) Loss of chromosome 10 is an independent prognostic factor in high-grade gliomas. Br J Cancer 81:1371–1377
Teich NM (1998) Oncogenes and cancer. In: Franks LM, Teich NM (eds) Cellular and molecular biology of cancer. Oxford University Press, NewYork, pp 169–201
Lang FF, Miller DC, Koslow M, Newcomb EW (1994) Pathways leading to glioblastoma multiforme: a molecular analysis of genetic alterations in 65 astrocytic tumors. J Neurosurg 81:427–436
Watanabe K, Tachibana O, Sato K, Yonekawa Y, Kleihues P, Ohgaki H (1996) Overexpression of the EGF receptor and p53 mutations are mutually exclusive in the evolution of primary and secondary glioblastomas. Brain Pathol 6:217–223
Reifenberger J, Reifenberger G, Liu L, James CD, Wechsler W, Collins VP (1994) Molecular genetic analysis of oligodendroglial tumors shows preferential allelic deletions on 19q and 1p. Am J Pathol 145:1175–1190
Bigner SH, Matthews MR, Rasheed BKA, Wiltshire RN, Friedman HS, Friedman AH, Stenzel TT, Dawes DM, McLendon RE, Bigner DD (1999) Molecular genetic aspects of oligodendrogliomas including analysis by comparative genomic hybridization. Am J Pathol 155:375–386
Cairncross JG, Ueki K, Zlatescu MC, Lisle DK, Finkelstein DM, Hammond RR, Silver JS, Stark PC, Macdonald DR, Ino Y, Ramsay DA, Louis DN (1998) Specific genetic predictors of chemotherapeutic response and survival in patients with anaplastic oligodendrogliomas. J Natl Cancer Inst 90:1473–1479
Ino Y, Betensky RA, Zlatescu MC, Sasaki H, Macdonald DR, Stemmer-Rachamimov AO, Ramsay DA, Cairncross JG, Louis DN (2001) Molecular subtypes of anaplastic oligodendroglioma: implications for patient management at diagnosis. Clin Cancer Res 7:839–845
Smith JS, Perry A, Borell TJ, Lee HK, O'Fallon J, Hosek SM, Kimmel D, Yates A, Burger PC, Scheithauer BW, Jenkins RB (2000) Alterations of chromosome arms 1p and 19q as predictors of survival in oligodendrogliomas, astrocytomas and mixed oligoastrocytomas. J Clin Oncol 18:636–645
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Arslantas, A., Artan, S., Öner, Ü. et al. The importance of genomic copy number changes in the prognosis of glioblastoma multiforme. Neurosurg Rev 27, 58–64 (2004). https://doi.org/10.1007/s10143-003-0279-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10143-003-0279-4